ABSTRACT
Background
The optimal macronutrient composition of the diet is controversial and many adults attempt to regulate the intake of specific macronutrients for various health-related reasons.
Objective
The objective was to compare stability and ranges of intakes of different macronutrients across diverse adult populations in the USA and globally.
Methods
US dietary intake data from NHANES 2009–2014 were used to determine macronutrient intake as a percentage of total energy intake. Variability in macronutrient intake was estimated by calculating the difference between 75th and 25th percentile (Q3–Q1) IQRs of macronutrient intake distributions. In addition, intake data from 13 other countries with per capita gross domestic product (GDP) over $10,000 US dollars (USD) were used to assess variability of intake internationally since there are large differences in types of foods consumed in different countries.
Results
Protein, carbohydrate, and fat intake (NHANES 2009–2014) was 15.7 ± 0.1, 48.1 ± 0.1, and 32.9 ± 0.1% kcal, respectively, in US adults. The IQR of protein intake distribution (3.73 ± 0.11% kcal) was 41% of carbohydrate intake distribution (9.18 ± 0.20% kcal) and 58% of fat intake distribution (6.40 ± 0.14% kcal). The IQRs of carbohydrate and fat intake distributions were significantly (P <0.01) influenced by age and race; however, the IQR of protein intake was not associated with demographic and lifestyle factors including sex, race, income, physical activity, and body weight. International mean protein intake was 16.3 ± 0.2% kcal, similar to US intake, and there was less variation in protein than carbohydrate or fat intake.
Conclusion
Protein intake of the US population and multiple international populations, regardless of demographic and lifestyle factors, was consistently ∼16% of total energy, suggesting biological control mechanism(s) tightly regulate protein intake and, consequently, influence intake of other macronutrients and food constituents. Substantial differences in intake of the other macronutrients observed in US and international populations had little influence on protein intake. This trial was registered at the ISRCTN registry as ISRCTN46157745 (https://www.isrctn.com/ISRCTN4615774).
Keywords: optimal diet, macronutrients, usual intake, intake distribution, interquartile ranges, NHANES, global, multicultural, dietary preferences
Introduction
The optimal macronutrient composition of the diet is a controversial topic. Many individuals attempt to modify the intake of specific macronutrients based on their perception of nutritional recommendations, such as reducing fat or carbohydrate or increasing protein intake. Radical shifts in macronutrient intake are the cornerstone of many popular fad diets, including the Atkins diet (low carbohydrate), the paleo diet (high protein, low grain), and ketogenic diet (high fat, low carbohydrate), that lack adequate scientific evidence for their efficacy and do not appear to be successful on a long-term basis due to a variety of factors, including compliance (1–6). When free-living adults are medically advised to modify their macronutrient intake and supervised by healthcare providers in large clinical trials, dietary compliance is low and attrition high (7–14).
Since macronutrients are acquired from a variety of foods and typically present in complex food matrices, consciously selecting a diet consisting of a specific macronutrient mix is a complex task. However, despite the inherent difficulty of consciously regulating macronutrient intake, humans and other animals effectively and unconsciously regulate the composition of their diet when adequate and varied foods are available (15, 16). Some of the regulatory mechanisms underlying these capabilities have been identified for protein and other macronutrients (15–21). For example, rodents avoid very high- or low-protein diets and, when given the opportunity, select a diet that contains adequate protein (15, 17, 22). The hypothesized biological constraints on protein ingestion, termed the “protein leverage theory,” suggest protein is prioritized over fat and carbohydrate intake, which may influence total caloric intake and limit dietary modification (16, 23, 24).
One objective of the current study was to evaluate protein, fat, and carbohydrate intake as a percentage of calories in US adults by age, sex, race-ethnicity, socioeconomic status, body weight status, and physical activity level. In addition, macronutrient intake was evaluated in adults from 14 countries (including the USA) with both accessible dietary intake data, to compare geographically and culturally diverse population groups, and gross domestic product (GDP) over $10,000 USD, to exclude countries where food availability might be restricted by economic factors. We hypothesized the distribution of protein intake as a percentage of calories would be more tightly regulated (i.e., less variation), as assessed by SD and IQR, than that of carbohydrate and fat intake in US adults and independent of demographic characteristics. We also hypothesized adults from other countries would have similar protein intake, as a percentage of total calories, as US adults, despite substantial geographic and cultural differences in dietary preferences, intake patterns, and food supply.
Methods
US macronutrient intake methods
Macronutrient intakes as a percentage of energy consumed per day by US adults were estimated using the 24-h dietary recall data collected from the dietary interview component of NHANES (25). NHANES is a continuous series of cross-sectional surveys that uses a complex, stratified multistage probability sample of a nationally representative, civilian noninstitutionalized US population identified from specified household clusters. A detailed description of NHANES study design and methods is available elsewhere (25).
Adult data from NHANES 2009 to 2010, 2011 to 2012, and 2013 to 2014 were combined to estimate recent macronutrient intake (n = 15,774). Data from all adults aged 19 y and older, excluding pregnant or lactating females and those with incomplete records, were used (Supplementary Figure 1). All participants or proxies provided written informed consent and the Research Ethics Review Board at the National Center for Health Statistics approved the protocol.
Statistical analyses were carried out with SAS 9.2 (SAS Institute Inc) using PROCSURVEY means. Appropriate weighting factors were used to adjust for oversampling of selected groups, survey nonresponse of some individuals, and day of the week when the interview was conducted. Individual usual intake (UI, habitual intake) of macronutrients was determined using the National Cancer Institute (NCI) method for a single dietary component (26) using both days of 24-h recall and day 1 sample weights. Covariates used in the UI estimations were day of the week of the 24-h recall [coded as weekend (Friday to Sunday) or weekday (Monday to Thursday)] and sequence of dietary recall (first or second). Percent kcal from protein, carbohydrates, and fat were analyzed separately by age/sex group, race-ethnicity, income quartile, physical activity level, and weight status. SDs and CIs for these distribution measures were also generated. IQRs of macronutrient intake distribution were calculated as the difference between the 75th and 25th intake percentile (Q3–Q1) as a measure of variability of intake. SAS PROC SGPLOT was used to output figures of intake distributions. To avoid considering very small differences to be statistically significant given the large number of observations used in these analyses, significance was set at P ≤0.01 and t tests were used to assess differences in intakes based on various demographic characteristics.
International macronutrient intake methods
Macronutrient intake (% kcal) from international populations was obtained from peer-reviewed published literature identified via PubMed and other databases or from publicly available national government reports. The following inclusion criteria were used to select data: macronutrient intake information was reported by sex; information was provided separately for adults aged between 18 and 70 y; and alcohol intake was either not legal in the country or calories from alcohol were separately provided. In addition, the survey methods used to determine macronutrient intake had to be based on either >1 dietary recall record, self-recorded dietary recall, diet history, or a scan of purchased foods. If the macronutrient intake in percent kcal was not reported directly in the publications, these values were calculated from data presented as kcal/d or g/d using conversion factors of 4 kcal/g for protein and carbohydrate, 9 kcal/g for fat, and 7 kcal/g for alcohol. If the caloric contribution of alcohol was not reported in the publications, it was estimated by recalculating the relative contributions of macronutrients. To eliminate countries where ad libitum selection of foods by a significant portion of the population could be limited for purely economic reasons, only countries with a GDP over $10,000 USD were considered (25, 27–40). Macronutrient intakes were plotted against their per capita GDP in US dollars and linear regression equations generated for males and females separately.
Results
Variability of US macronutrient intake
Recent (NHANES 2009–2014) macronutrient intake distributions as a percentage of calories are presented in Figure 1. The protein intake distribution range was the narrowest of the macronutrients, the carbohydrate intake range was the widest, and the intake range for fat was intermediate. The range of intake between 2 SD above and below the mean intake (calculated by subtracting the value of the left 2 SD tail from the right 2 SD tail) was the lowest for protein (11.2%) compared with carbohydrate and fat (27.3% and 18.9%, respectively) (Table 1). Quartile 1 and quartile 4 intakes were <13.7 and >17.4% kcal for protein; <43.6 and >52.8% kcal for carbohydrate; and <29.8 and >36.1% kcal for fat, with mean intakes being 15.7 ± 0.1, 48.1 ± 0.1 and 32.9 ± 0.1% kcal for protein, carbohydrate, and fat, respectively. The IQR intake distribution was the smallest (3.73 ± 0.11 percentage units) for protein intake and was 41% of the IQR of the carbohydrate intake distribution (9.18 ± 0.20 percentage units) and 58% of the IQR of the fat intake distribution (6.40 ± 0.14 percentage units) (Table 2). Excess kurtosis (kurtosis-3), an indicator of a narrower and steeper peak of a distribution compared with other distributions, was highest for the protein distribution with nonoverlapping CIs compared with carbohydrate and fat intake distributions (Table 2).
FIGURE 1.
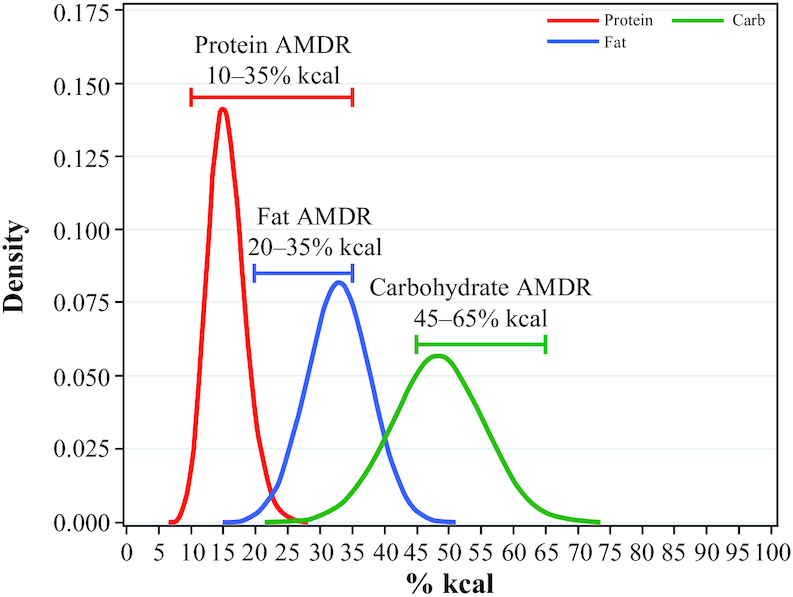
Distribution of usual macronutrient intake among adults aged 19+ y, NHANES 2009–2014 (n = 15,774). The narrower and steeper peak, and smaller tails, of the protein distribution compared with the fat and carbohydrate distributions are readily apparent and verified by the various statistical comparisons provided in the text. The Acceptable Macronutrient Distribution Range brackets indicate percentage of total energy and are 45–65% for carbohydrate, 20–35% for fat, and 10–35% for protein (45). AMDR, Acceptable Macronutrient Distribution Range.
TABLE 1.
Usual intake of macronutrients (% kcal) among adults aged 19+ y, NHANES 2009–2014 (n = 15,774)
| Protein | Carbohydrate | Fat | |
|---|---|---|---|
| 1 SD—left tail % of population | 12.9 ± 0.09 | 41.3 ± 0.24 | 28.2 ± 0.16 |
| 2 SD—left tail % of population | 10.1 ± 0.15 | 34.5 ± 0.38 | 23.5 ± 0.25 |
| 1 SD—right tail % of population | 18.5 ± 0.14 | 55.0 ± 0.17 | 37.7 ± 0.15 |
| 2 SD—right tail % of population | 21.3 ± 0.22 | 61.8 ± 0.29 | 42.4 ± 0.23 |
Data presented as estimated mean  SE of estimated mean.
SE of estimated mean.
TABLE 2.
Usual intake of macronutrients (% kcal) among adults aged 19+ y, NHANES 2009–2014 (n = 15,774)
| Protein | Carbohydrate | Fat | |
|---|---|---|---|
| Mean intake | 15.7 ± 0.1 | 48.1 ± 0.1 | 32.9 ± 0.1 |
| Intake quartile 1 | <13.7 | <43.6 | <29.8 |
| Intake quartile 2 | 13.7–15.5 | 43.6–48.2 | 29.8–33.0 |
| Intake quartile 3 | 15.6–17.4 | 48.3–52.8 | 29.9–36.1 |
| Intake quartile 4 | >17.4 | >52.8 | >36.1 |
| IQR | 3.73 ± 0.11 | 9.18 ± 0.20 | 6.40 ± 0.14 |
| Excess kurtosis (95th CI) | 0.32 (0.18, 0.45) | 0.05 (−0.02, 0.12) | 0.07 (−0.02, 0.16) |
Data presented as estimated mean  SE of estimated mean.
SE of estimated mean.
In the NHANES 2009–2014 data, mean intakes of macronutrients as a percentage of calories were not influenced by various demographic factors (Table 3). Protein intake as a percentage of calories, although statistically significant (P ≤0.01), was only 0.5 percentage units lower in female than in male adults. Carbohydrate intake was 2.3 percentage units higher in females than males (P ≤0.01). Protein intake was not affected by age (P >0.01), whereas older adults (≥71 y) consumed more carbohydrate than adults aged 31–50 and 51–70 y, and adults 51–70 y consumed more fat as a percentage of calories than adults aged 19–30 and 31–50 y. Protein intake was highest among Asians, followed by Hispanics and was lowest among non-Hispanic (NH)-whites and NH-blacks, but the widest difference in protein intake in these groups was only 1.8 percentage units. Carbohydrate intake was higher and fat intake lower for Asians and Hispanics than for NH-whites and NH-blacks. Adults in lower income groups [poverty income ratio (PIR) <1.35] consumed less protein (but only 0.4 percentage units) and fat, and more carbohydrate as a percentage of calories than adults in higher income groups (PIR >1.85). Intake of protein or fat as a percentage of calories was not affected by physical activity. However, sedentary adults consumed more carbohydrate as a percentage of calories than those in the vigorous activity group. Adults with normal body weight consumed less protein (but only 0.6 percentage units) and fat, and more carbohydrate as a percentage of calories than overweight or obese adults.
TABLE 3.
Mean usual intake of macronutrients (% kcal) among adults aged 19+ y in various demographic groups, NHANES 2009–2014 (n = 15,774)
| Demographic groups | Protein | Carbohydrate | Fat |
|---|---|---|---|
| Sex | |||
| Male | 15.9 ± 0.1a | 47.0 ± 0.2a | 33.0 ± 0.2 |
| Female | 15.4 ± 0.1b | 49.3 ± 0.2b | 32.9 ± 0.2 |
| Age groups | |||
| 19–30 y | 15.4 ± 0.2 | 48.9 ± 0.2ac | 32.5 ± 0.2a |
| 31–50 y | 15.7 ± 0.1 | 48.2 ± 0.2a | 32.5 ± 0.2a |
| 51–70 y | 15.8 ± 0.1 | 47.2 ± 0.2b | 33.6 ± 0.2b |
| 71+ y | 15.7 ± 0.2 | 49.2 ± 0.3c | 33.2 ± 0.2ab |
| Ethnicity | |||
| Hispanic | 16.4 ± 0.1a | 49.8 ± 0.3ad | 31.8 ± 0.2a |
| Non-Hispanic white | 15.5 ± 0.1b | 47.4 ± 0.2b | 33.4 ± 0.2b |
| Non-Hispanic black | 15.3 ± 0.1b | 48.6 ± 0.2c | 33.2 ± 0.3b |
| Asian | 17.2 ± 0.2c | 50.3 ± 0.5d | 30.4 ± 0.4c |
| Poverty income ratio | |||
| <1.35 | 15.4 ± 0.1a | 50.0 ± 0.2a | 32.1 ± 0.2a |
| 1.35–1.85 | 15.4 ± 0.2ab | 49.2 ± 0.3a | 33.1 ± 0.3b |
| >1.85 | 15.8 ± 0.1b | 47.1 ± 0.2b | 33.3 ± 0.2b |
| Physical activity level | |||
| Sedentary | 15.5 ± 0.1 | 49.1 ± 0.3a | 33.3 ± 0.2 |
| Moderate | 15.6 ± 0.1 | 48.2 ± 0.3ab | 33.1 ± 0.2 |
| Vigorous | 15.9 ± 0.1 | 47.6 ± 0.2b | 32.6 ± 0.2 |
| Body weight status | |||
| Normal weight | 15.3 ± 0.1a | 49.0 ± 0.2a | 32.0 ± 0.2a |
| Overweight | 15.8 ± 0.1b | 47.5 ± 0.2b | 33.1 ± 0.2b |
| Obese | 15.9 ± 0.1b | 48.0 ± 0.2b | 33.6 ± 0.2b |
| Overweight or obese | 15.9 ± 0.1b | 47.7 ± 0.2b | 33.3 ± 0.1b |
Data presented as estimated mean  SE of estimated mean. a-dValues with different superscripts are significantly different for a nutrient within a demographic group at P <0.01 via t tests.
SE of estimated mean. a-dValues with different superscripts are significantly different for a nutrient within a demographic group at P <0.01 via t tests.
In US adults, protein intake distribution (i.e., IQR for UI) was not affected (P >0.01) by any demographic or lifestyle factors including sex, race, income, physical activity, and body weight status (Table 4). IQRs for carbohydrate and fat intake distribution were significantly influenced by age and race-ethnicity. The IQR for carbohydrate intake was greater for adults aged 31–50 and 51–70 y than adults ≥71 y, as well as for NH-white adults compared with NH-black and Hispanic adults. The IQR for fat intake was higher for adults aged 51–70 y than 19–30 y, as well as for Asian adults than NH-black and Hispanic adults. Other demographic and lifestyle factors did not affect the IQR of carbohydrate or fat intake. It should also be noted that mean intakes of protein, carbohydrate, and fat have not changed significantly over the last decade among the US population (41).
TABLE 4.
IQR of usual intake of macronutrients (% kcal) among adults aged 19+ y by various demographic groups, NHANES 2009–2014 (n = 15,774)
| Demographic groups | Protein | Carbohydrate | Fat |
|---|---|---|---|
| Sex | |||
| Male | 3.73 ± 0.16 | 9.41 ± 0.32 | 6.58 ± 0.27 |
| Female | 3.70 ± 0.13 | 8.81 ± 0.25 | 6.20 ± 0.21 |
| Age groups | |||
| 19–30 y | 3.94 ± 0.20 | 8.39 ± 0.45ab | 5.80 ± 0.35a |
| 31–50 y | 3.68 ± 0.17 | 9.74 ± 0.30a | 6.20 ± 0.25ab |
| 51–70 y | 3.60 ± 0.20 | 9.33 ± 0.25a | 7.00 ± 0.30b |
| 71 + y | 3.59 ± 0.18 | 8.01 ± 0.34b | 5.85 ± 0.36ab |
| Ethnicity | |||
| Hispanic | 3.83 ± 0.20 | 8.07 ± 0.36a | 5.87 ± 0.25a |
| Non-Hispanic white | 3.68 ± 0.13 | 9.46 ± 0.28b | 6.47 ± 0.21ab |
| Non-Hispanic black | 3.45 ± 0.19 | 8.14 ± 0.26a | 5.73 ± 0.28a |
| Asian | 4.02 ± 0.44 | 8.96 ± 0.62ab | 7.27 ± 0.45b |
| Poverty income ratio | |||
| <1.35 | 3.81 ± 0.13 | 8.62 ± 0.34 | 6.30 ± 0.20 |
| 1.35–1.85 | 3.58 ± 0.40 | 8.12 ± 0.51 | 6.29 ± 0.51 |
| >1.85 | 3.60 ± 0.13 | 9.21 ± 0.24 | 6.26 ± 0.19 |
| Physical activity level | |||
| Sedentary | 3.70 ± 0.20 | 8.93 ± 0.32 | 6.64 ± 0.32 |
| Moderate | 3.43 ± 0.17 | 9.25 ± 0.35 | 6.29 ± 0.20 |
| Vigorous | 4.00 ± 0.17 | 9.21 ± 0.21 | 6.28 ± 0.26 |
| Body weight status | |||
| Normal weight | 3.74 ± 0.19 | 8.81 ± 0.34 | 5.89 ± 0.34 |
| Overweight | 3.41 ± 0.16 | 9.58 ± 0.32 | 6.74 ± 0.26 |
| Obese | 3.90 ± 0.16 | 9.16 ± 0.34 | 6.37 ± 0.26 |
| Overweight or obese | 3.70 ± 0.13 | 9.37 ± 0.28 | 6.54 ± 0.18 |
Data presented as estimated mean  SE of estimated mean. a-bValues with different superscripts are significantly different for a nutrient within a demographic group at P <0.01 via t tests.
SE of estimated mean. a-bValues with different superscripts are significantly different for a nutrient within a demographic group at P <0.01 via t tests.
Variability of international macronutrient intake
Per capita GDP in the international populations examined varied from slightly over  12,000 USD in Poland to over $71,000 USD in Norway (Table 5). The range of protein intake in the 14 international populations (including the USA) was narrower than for carbohydrate and fat as a percentage of calories. Protein intake ranged from 13.6% kcal for Japanese males to ∼18.5% kcal for Australian females, whereas carbohydrate intake ranged from 42.9% kcal for males of the Czech Republic to 68.0% kcal for Korean females, and fat intake ranged from 17.6% kcal for Korean females to 38.0% kcal for females from the Netherlands (Table 5). For each country, macronutrient intake data were plotted against per capita GDP in US dollars and the slopes for each macronutrient were similar for males and females. Intake of protein did not change substantially with per capita GDP, whereas the intake of carbohydrate decreased, and intake of fat increased with GDP (Figure 2). The steepness of the slopes of the regression lines for protein intake were 88–90% less than carbohydrate and 75–82% less than that of fat.
12,000 USD in Poland to over $71,000 USD in Norway (Table 5). The range of protein intake in the 14 international populations (including the USA) was narrower than for carbohydrate and fat as a percentage of calories. Protein intake ranged from 13.6% kcal for Japanese males to ∼18.5% kcal for Australian females, whereas carbohydrate intake ranged from 42.9% kcal for males of the Czech Republic to 68.0% kcal for Korean females, and fat intake ranged from 17.6% kcal for Korean females to 38.0% kcal for females from the Netherlands (Table 5). For each country, macronutrient intake data were plotted against per capita GDP in US dollars and the slopes for each macronutrient were similar for males and females. Intake of protein did not change substantially with per capita GDP, whereas the intake of carbohydrate decreased, and intake of fat increased with GDP (Figure 2). The steepness of the slopes of the regression lines for protein intake were 88–90% less than carbohydrate and 75–82% less than that of fat.
TABLE 5.
Macronutrient intake (% kcal) and per capita gross domestic product in multiple international populations. Data adapted from various national surveys
| Per capita GDP (US dollars)1 | Macronutrient intake (% kcal) for males/females | |||||
|---|---|---|---|---|---|---|
| Country | Sample year | Protein | Carbohydrate | Fat | References | |
| Australia | 51,592 | 2011–12 | 18.3/18.5 | 43.2/43.5 | 30.4/31.1 | (27) |
| Canada | 42,319 | 2004 | 15.9/15.5 | 47.3/50.0 | 31.3/30.9 | (28) |
| Czech Republic | 18,326 | 2002–05 | 17.2/16.8 | 42.9/47.1 | 35.7/35.1 | (29) |
| Finland | 43,492 | 2007 | 16.8/17.2 | 47.1/50.2 | 33.1/31.2 | (30) |
| France | 38,537 | 2006–07 | 16.2/17.1 | 43.5/44.6 | 35.2/37.1 | (31) |
| Germany | 42,326 | 2005–07 | 13.9/13.9 | 43.3/45.1 | 36.7/36.3 | (32) |
| Ireland | 65,871 | 2008–10 | 16.6/16.6 | 44.1/46.4 | 34.3/35.4 | (33) |
| Japan | 37,304 | 2012–132 | 13.6/15.9 | 55.0/58.9 | 23.5/24.4 | (34, 35) |
| Korea | 27,633 | 2007–09 | 15.0/14.3 | 63.0/68.0 | 18.0/17.6 | (36) |
| Netherlands | 45,210 | 1987–98 | 14.5/15.5 | 43.0/43.5 | 37.0/38.0 | (37) |
| Norway | 71,497 | 2010–11 | 18.0/18.0 | 43.0/44.0 | 34.0/34.0 | (38) |
| Poland | 12,309 | 2002–05 | 17.6/17.4 | 45.1/48.2 | 36.1/34.1 | (29) |
| United Kingdom | 40,411 | 2008–12 | 16.4/16.6 | 45.1/46.3 | 32.8/33.0 | (39) |
| United States | 57,294 | 2011–14 | 16.1/15.6 | 47.4/49.6 | 33.6/33.7 | (25) |
Sample year was 1990 for females.
GDP, gross domestic product.
FIGURE 2.
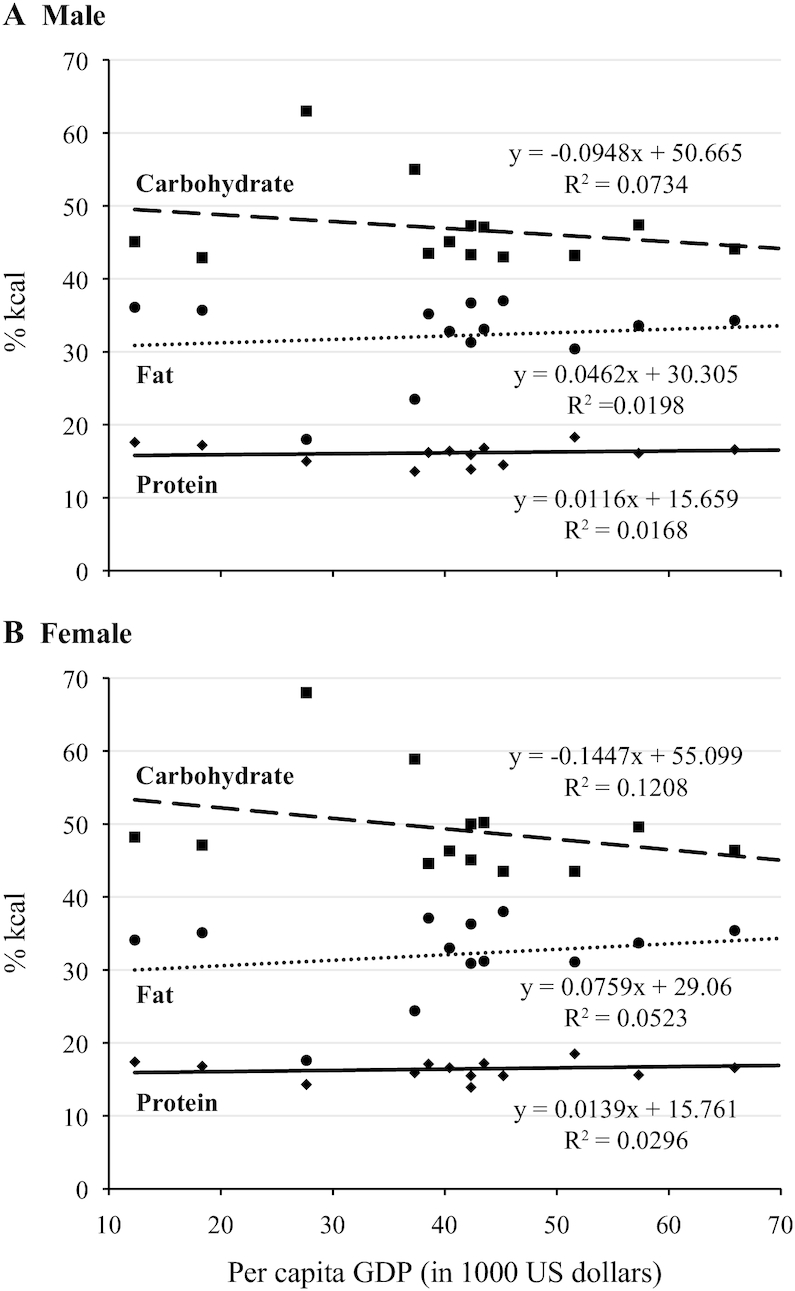
Protein, carbohydrate, and fat intake (% kcal) in 14 populations by per capita gross domestic product. Data adapted from various national surveys (25, 27–39). Squares represent carbohydrate intake, circles represent fat intake, and diamonds represent protein intake. Panel A for males and panel B for females. GDP, gross domestic product.
Discussion
In the USA, protein intake varies substantially less than carbohydrate and fat intake as assessed by the distribution of intake, SD, and IQR, standard measures of variability (Figure 1; Tables 1 and 2). These data support that, on a population level, protein intake is less variable than carbohydrate or fat. Differences in macronutrient intake associated with a variety of demographic variables were minimal but were greater for carbohydrate and fat (3% or less) compared with protein (2% or less) (Table 3). The IQR of protein intake in US adults was unaffected by age, ethnicity, income, physical activity, and weight status; however, carbohydrate and fat intake did vary significantly across age and ethnicity (Table 4).
The international macronutrient intake data presented from 13 countries with per capita GDP of over $10,000 USD and the USA also support the hypothesis that protein is the most tightly regulated macronutrient (Table 5). In countries with very different staple foods and cuisines, variation in protein intake was much less than either carbohydrate or fat. Furthermore, differences in per capita GDP had substantially less impact on protein intake than intake of the other macronutrients (Figure 2), even though foods with higher protein content, such as lean meats and dairy, generally have a greater energy cost than those that contain greater amounts of carbohydrates and fats, such as grains, sweets, butter, and oil (42, 43). The trend of decreased carbohydrate intake and increased fat consumption with increased per capita income in the international populations examined here is consistent with the literature on this issue (40). The stability in the proportion of protein intake in the human diet is consistent with a great deal of experimental data from humans and other mammals. For example, a very large, carefully controlled clinical trial comparing weight loss diets was conducted to examine the effects of varying protein intake from 15% to 25% of total caloric intake. However, in 2 y, when the study was complete, the actual variation in protein intake consumed by the different treatment groups was only 1.6 percentage units, demonstrating the difficulty of intentionally intervening to alter protein intake (7).
In aggregate, protein intake as a percentage of calories of the diet is tightly regulated and largely independent of a variety of factors including sex, age, socioeconomic status, ethnicity, physical activity, and body weight. In addition, despite cultural differences in dietary preferences, intake patterns, and food availability internationally, protein intake, relative to the other macronutrients, is remarkably stable. The data presented here indicate protein intake is more tightly regulated than carbohydrate and fat, consistent with prior studies (for examples see 16, 23, 24). Furthermore, the substantial variability in fat and carbohydrate intake observed, compared with protein, indicates intake of these macronutrients has relatively little influence on protein consumption.
There were a number of limitations in this study. Intake data from NHANES are self-reported, and although the best procedures were used to assess dietary intake, self-reported dietary data rely on memory and the ability of subjects to accurately report the foods and amounts of foods consumed, and are subject to reporting bias (44). Another limitation was the variability in methods used to collect the international macronutrient data. Although we restricted our selection of international data to the most accurate methods, there is undoubtedly added variability in the data reported here attributable to methodical differences in collecting and analyzing such complex data across such diverse populations. This type of measurement error may have created greater differences in estimates of macronutrient intake than would have been observed if identical procedures were used across all the nations studied. Major strengths of our study were use of a large nationally representative, population-based sample of adults to obtain US intake data and data from multiple international populations.
In conclusion, in US and international populations, converging evidence suggests protein intake is more tightly regulated than intake of the other macronutrients. The lack of substantial variation in protein intake across a variety of demographic variables in the US population and in 14 nations (including the USA) supports this finding and lends credence to the protein leverage hypothesis. A better understanding of the biological constraints on protein ingestion may improve formulation of practical guidance regarding optimal macronutrient intake.
Supplementary Material
ACKNOWLEDGEMENTS
We wish to acknowledge Tom McLellan for collection and collation of data from multiple international sources. We thank the US Army Medical Research and Development Command and Department of Defense Center Alliance for Nutrition and Dietary Supplement Research for funding the research. This research was also supported in part by an appointment to the Research Participation Program at the US Army Medical Research Institute of Environmental Medicine administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and US Army Medical Research and Development Command.
The authors’ contributions were as follows—HRL: participated in formulating the research question, design of analyses, interpretation of the data, drafting the manuscript, revising the manuscript, and the approval of the final version; VLF: participated in the design of analyses, dietary data analysis, interpretation of the data, drafting the manuscript, revising the manuscript, and approval of the final version; SA: participated in interpretation of the data, drafting the manuscript, revising the manuscript, and approval of the final version; SMP: participated in interpretation of the data, drafting the manuscript, revising the manuscript, and approval of the final version; and CEB: participated in interpretation of the data, drafting the manuscript, revising the manuscript, and approval of the final version; and all authors: read and approved the final version of the manuscript and are responsible for all aspects of the manuscript. HRL, SMP, and CEB report no conflicts of interest. VLF III as Senior Vice President of Nutrition Impact LLC provides database analyses and food/nutrition consulting to the food/beverage industry. SA is a principal at NutriScience LLC which provides nutrition consulting to the food/beverage industry.
Notes
Supported by the US Army Military Research and Development Command and the Department of Defense Center Alliance for Nutrition and Dietary Supplements Research.
The US data described in the article are publicly available at the NHANES website: https://www.cdc.gov/nchs/nhanes/Default.aspx. The international data are all publicly available on websites and publications cited in the article; the analytic code will be made available upon request pending application and appropriate regulatory approval.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Army or the Department of Defense. Any citations of commercial organizations and trade names in this article do not constitute an official Department of the Army endorsement of approval of the products or services of these organizations.
Supplementary Figure 1 is available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Abbreviations used: AMDR, Acceptable Macronutrient Distribution Range; GDP, gross domestic product; NCI, National Cancer Institute; NH, non-Hispanic; PIR, poverty income ratio; UI, individual usual intake; USD, US dollars.
Contributor Information
Harris R Lieberman, Military Nutrition Division, US Army Research Institute of Environmental Medicine, Natick, MA, USA.
Victor L Fulgoni, III, Henry M Jackson Foundation, Bethesda, MD, USA.
Sanjiv Agarwal, Oak Ridge Institute for Science and Education, Belcamp, MD, USA.
Stefan M Pasiakos, Military Nutrition Division, US Army Research Institute of Environmental Medicine, Natick, MA, USA.
Claire E Berryman, Military Nutrition Division, US Army Research Institute of Environmental Medicine, Natick, MA, USA; Oak Ridge Institute for Science and Education, Belcamp, MD, USA; Department of Nutrition, Food, and Exercise Sciences, Florida State University, Tallahassee, FL, USA.
References
- 1. U.S. Department of Health and Human Services and U.S. Department of Agriculture 2015–2020 Dietary Guidelines for Americans. 8th Edition 2015; [Internet]. Available at: http://health.gov/dietaryguidelines/2015/guidelines/. [Google Scholar]
- 2. Freedman MR, King J, Kennedy E. Popular diets: a scientific review. Obes Res. 2001;9:1S–40S. [DOI] [PubMed] [Google Scholar]
- 3. Freeman JM, Kossoff EH, Hartman AL. The ketogenic diet: one decade later. Pediatrics. 2007;119:535–43. [DOI] [PubMed] [Google Scholar]
- 4. Brand Miller J, Mann N, Cordain L. Paleolithic nutrition: what did our ancestors eat?In: Selinger A, Greene A(editors). Genes to Galaxies: The Lecture Series of the 35th Professor Harry Messel International Science School Sydney: Science Foundation for Physics; 2019;p. 28–40. [Google Scholar]
- 5. Atkin RC. Atkins for Life. New York: St Martin's Griffin; 2004. [Google Scholar]
- 6. U.S. News Reveals Best Diets Rankings for 2018 US News Information 3 Jan, 2018 [cited 19 March, 2018] [Internet]. Available at: https://www.usnews.com/info/blogs/press-room/articles/2018-01-03/us-news-reveals-best-diets-rankings-for-2018.
- 7. Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, McManus K, Champagne CM, Bishop LM, Laranjo N et al.. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360:859–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tang JL, Armitage JM, Lancaster T, Silagy CA, Fowler GH, Neil HA. Systematic review of dietary intervention trials to lower blood total cholesterol in free-living subjects. BMJ. 1998;316:1213–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vanstone M, Giacomini M, Smith A, Brundisini F, DeJean D, Winsor S. How diet modification challenges are magnified in vulnerable or marginalized people with diabetes and heart disease: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. 2013;13:1–40. [PMC free article] [PubMed] [Google Scholar]
- 10. Vanstone M, Rewegan A, Brundisini F, Giacomini M, Kandasamy S, DeJean D. Diet modification challenges faced by marginalized and nonmarginalized adults with type 2 diabetes: a systematic review and qualitative meta-synthesis. Chronic Illn. 2017;13:217–35. [DOI] [PubMed] [Google Scholar]
- 11. Dansigner M, Gleason JA, Griffith JL, Selker HP, Schaefer EJ. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA. 2005;293:43–53. [DOI] [PubMed] [Google Scholar]
- 12. Hammarstrom A, Wiklund AF, Lindahl B, Larsson C, Ahlgren C. Experiences of barriers and facilitators to weight-loss in a diet intervention – a qualitative study of women in northern Sweden. BMC Womens Health. 2014;14:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Metzgar M, Rideout TC, Fontes-Villalba M, Kuipers RS. The feasibility of a Paleolithic diet for low-income consumers. Nutr Res. 2011;31:444–51. [DOI] [PubMed] [Google Scholar]
- 14. Genoni A, Lo J, Lyons-Wall P, Devine A. Compliance, palatability and feasibility of PALEOLITHIC and Australian guide to healthy eating diets in healthy women: a 4-week dietary intervention. Nutrients. 2016;8(8):481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peters JC, Harper AE. Influence of dietary protein level on protein self-selection and plasma and brain amino acid concentrations. Physiol Behav. 1984;33:783–90. [DOI] [PubMed] [Google Scholar]
- 16. Sorensen A, Mayntz D, Raubenheimer D, Simpson SJ. Protein-leverage in mice: the geometry of macronutrient balancing and consequences for fat deposition. Obesity (Silver Spring). 2008;16:566–71. [DOI] [PubMed] [Google Scholar]
- 17. Harper AE, Peters JC. Protein intake, brain amino acid and serotonin concentrations and protein self-selection. J Nutr. 1989;119:677–89. [DOI] [PubMed] [Google Scholar]
- 18. de Castro JM. What are the major correlates of macronutrient selection in Western populations?. Proc Nutr Soc. 1999;58:755–63. [DOI] [PubMed] [Google Scholar]
- 19. de Castro JM. Macronutrient selection in free feeding humans. Evidence for long term regulation. In: Berthoud HR, Seeley RJ (editors). Neural Control of Macronutrient Selection. New York: CRC Press; 2000, p. 43–59. [Google Scholar]
- 20. Berthoud HR, Munzberg H, Richards BK, Morrison CD. Neural and metabolic regulation of macronutrient intake and selection. Proc Nutr Soc. 2012;71:390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gietzen DW, Aja SM. The brain's response to an essential amino acid-deficient diet and the circuitous route to a better meal. Mol Neurobiol. 2012;46:332–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Leathwood PD, Ashley DV. Strategies of protein selection by weanling and adult rats. Appetite. 1983;4:97–112. [DOI] [PubMed] [Google Scholar]
- 23. Simpson SJ, Raubenheimer D. Obesity: the protein leverage hypothesis. Obes Rev. 2005;6:133–42. [DOI] [PubMed] [Google Scholar]
- 24. Martinez-Cordero C, Kuzawa CW, Sloboda DM, Stewart J, Simpson SJ, Raubenheimer D. Testing the protein leverage hypothesis in a free-living human population. Appetite. 2012;59:312–15. [DOI] [PubMed] [Google Scholar]
- 25. Center for Disease Control and Prevention National Health and Nutrition Examination Survey Data, Hyattsville, MD. [Internet] 2015; [cited 10 December, 2017]. Available at: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm. [Google Scholar]
- 26. Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith SM, Subar AF, Dodd KW. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. 2010;29:2857–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Australian Bureau of Statistics Australian Health Survey Nutrition; State and Territory Results 2011–12. Canberra, ACT, 2015. [Google Scholar]
- 28. Batal M, Makvandi E, Imbeault P, Gagnon-Arpin I, Grenier J, Chomienne MH, Bouchard L. Comparison of dietary intake between francophones and anglophones in Canada: data from CCHS 2.2. Can J Public Health. 2013;104:S31–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Boylan S, Welch A, Pikhart H, Malyutina S, Pajak A, Kubinova R, Bragina O, Simonova G, Stepaniak U, Gilis-Januszewska A et al.. Dietary habits in three Central and Eastern European countries: the HAPIEE study. BMC Public Health. 2009;9:439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pietinen P, Paturi M, Reinivuo H, Tapanainen H, Valsta LM. 2010 FINDIET 2007 survey: energy and nutrient intakes. Public Health Nutr. 2010;13:920–4. [DOI] [PubMed] [Google Scholar]
- 31. Castetbon K, Vernay M, Malon A, Salanave B, Deschamps V, Roudier C, Oleko A, Szego E, Hercberg S. Dietary intake, physical activity and nutritional status in adults: the French nutrition and health survey (ENNS, 2006–2007). Br J Nutr. 2009;102:733–43. [DOI] [PubMed] [Google Scholar]
- 32. Wittig F, Hummel E, Wenzler G, Heuer T. Energy and macronutrient intake over the course of the day of German adults: a DEDIPAC-study. Appetite. 2017;114:125–36. [DOI] [PubMed] [Google Scholar]
- 33. Walton J. National Adult Nutrition Survey Summary Report March 2011. Cork, Ireland: Irish Universities Nutrition Alliance; 2011. [Google Scholar]
- 34. Nanri A, Eguchi M, Kuwahara K, Kochi T, Kurotani K, Ito R, Pham NM, Tsuruoka H, Akter S, Jacka F et al.. Macronutrient intake and depressive symptoms among Japanese male workers: the Furukawa Nutrition and Health Study. Psychiatry Res. 2014;220:263–8. [DOI] [PubMed] [Google Scholar]
- 35. Yoshita K, Arai Y, Nozue M, Komatsu K, Ohnishi H, Saitoh S, Miura K. Total energy intake and intake of three major nutrients by body mass index in Japan: NIPPON DATA80 and NIPPON DATA90. J Epidemiol. 2010;20:S515–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shin HJ, Cho E, Lee HJ, Fung TT, Rimm E, Rosner B, Manson JE, Wheelan K, Hu FB. 2014 Instant noodle intake and dietary patterns are associated with distinct cardiometabolic risk factors in Korea. J Nutr. 2014;144:1247–55. [DOI] [PubMed] [Google Scholar]
- 37. Hulshof KF, Brussaard JH, Kruizinga AG, Telman J, Lowik MR. Socio-economic status, dietary intake and 10 y trends: the Dutch National Food Consumption Survey. Eur J Clin Nutr. 2003;57:128–37. [DOI] [PubMed] [Google Scholar]
- 38. Totland TH, Melnaes BK, Lundberg-Hallen N, Helland-Kigen KM, Lund-Blix NA, Myhre JB, Johansen AMW, Loken EB, Andersen LF.. Norkost 3: A nationally representative dietary survey in men and women in Norway aged 18–70 years, 2010–11 (Norkost 3: En landsomfattende kostholdsundersøkelse blant menn og kvinner i Norge i alderen 18–70 år, 2010–11). In: The Norwegian Directorate of Health, The Norwegian Food Safety Authority, The University of Oslo; 2012. [Google Scholar]
- 39. Bates B, Lennox A, Prentice A, Bates C, Page P, Nicholson S, Swan G. National Diet and Nutrition Survey. Results from Years 1–4 (combined) of the rolling programme (2008/2009–2011/2012) London, UK: Public Health England; 2014. [Google Scholar]
- 40. Gerbens-Leenes PW, Nonhebel S, Krol MS. Food consumption patterns and economic growth. Increasing affluence and the use of natural resources. Appetite. 2010;55:597–608. [DOI] [PubMed] [Google Scholar]
- 41. Kant AK, Graubard BI. Secular trends in regional differences in nutritional biomarkers and self-reported dietary intakes among American adults: National Health and Nutrition Examination Survey (NHANES) 1988–1994 to 2009–2010. Public Health Nutr. 2018;21:927–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Darmon N, Briend A, Drewnowski A. Energy-dense diets are associated with lower diet costs: a community study of French adults. Public Health Nutr. 2004;7:21–7. [DOI] [PubMed] [Google Scholar]
- 43. Murakami K, Sasaki S, Okubo H, Takahashi Y, Hosoi Y, Itabashi M. Monetary costs of dietary energy reported by young Japanese women: association with food and nutrient intake and body mass index. Public Health Nutr. 2007;10:1430–9. [DOI] [PubMed] [Google Scholar]
- 44. Subar AF, Freedman LS, Tooze JA, Kirkpatrick SI, Boushey C, Neuhouser ML, Thompson FE, Potischman N, Guenther PM, Tarasuk V et al.. Addressing current criticism regarding the value of self-report dietary data. J Nutr. 2015;145:2639–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. National Academy of Sciences, Institute of Medicine, Food and Nutrition Board Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington (DC): National Academy of Sciences; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


