Abstract
Fibroepithelial polyps (acrochordon or skin tag) are benign tumors that usually occur in skin folds, such as the axilla, genital area or neck. They can be solitary or multiple. Their dimensions usually do not exceed 1-2 millimeters. Sometimes, they can reach huge dimensions. In the literature, a giant fibroepithelial polyp with a size of 42 centimeters has been reported. Although the etiology and the factors that cause excessive growth have not been elucidated, it is stated that obesity and insulin resistance might trigger growth. Lymphedematous fibroepithelial polyps described in recent years show that prolonged lymphatic stasis and chronic inflammation may lead to the growth of fibroepithelial polyps. We present a 21-year-old patient with a giant fibroepithelial polyp with a size of 14x6 centimeter, located in the midline on the anterior chest wall. To our knowledge, this is the first case in the literature, in this location, which makes our case unique. Herein, we presented our patient along with the review of current literature pertaining to the diagnosis and the treatment of fibroepithelial polyps (FEPs) and the factors leading to excessive growth.
Keywords: Giant, fibroepithelial, lymphedematous
Fibroepithelial polyps or acrochordons are benign tumors of mesenchymal and ectodermal origin. They frequently occur in places where skin folds are present. Generally, their size does not exceed 5 millimeters. However, a case with a 42 centimeters long FEP has been reported in the literature.[1] There are different opinions about how FEPs reach these sizes and what triggers the growth. It is stated that the sensitivity of epithelium to hormones and hormonal changes may be the cause of the growth of FEPs, which are located in the genital tract and reached huge sizes.[2] It is also remarkable that FEPs located in this area are seen more frequently in women and in reproductive age.[3]
It is not known exactly what triggered the growth of the FEPs that are located in other locations and reached huge sizes. However, a positive correlation between obesity, insulin resistance and FEP growth has been proposed.[4–6]
Our case was unique concerning the FEP location. We did not find a similar case in terms of location and size in the literature. Our patient also had a ventriculoperitoneal shunt for six years due to idiopathic hydrocephalus. The shunt was 2 centimeters away from FEP. It may be thought that the foreign body reaction in this area may be an effect on FEP growth. In this report, we aimed to present our approach to a giant FEP and to examine the factors that cause FEP growth.
Case Report
A 21-year-old female patient presented with a 14 centimeters long hyperpigmented, polypoid mass with an 8x4 centimeters base located in the midline on the anterior chest wall (Figs. 1, 2). She stated that the mass had existed at birth, but it had been growing for the last 10 years. The patient underwent ventriculoperitoneal shunting six years ago due to increased idiopathic intracranial pressure and the shunt could be palpated manually under the skin at a distance of 2 centimeters from the FEP. Apart from this, the systemic examination was unremarkable and the patient had no additional disease. A thorax magnetic resonance imaging (MRI) showed nevoid formation at the dermis level, which has not invaded subcutaneous tissues. Then, the patient was scheduled for surgical excision. Patient’s informed consent form was obtained for this report. Under general anesthesia, the tumor was excised up to the superficial fascia with a 5 millimeters safety margin. The defect area was repaired with a split-thickness skin graft taken from the anterior aspect of the left thigh. The pathology of the lesion was reported as a fibroepithelial polyp covered with stratified squamous epithelium, edematous fibrovascular stroma (Fig. 3) and congested, proliferated and dilated vascular structures within the stroma (Fig. 4). No recurrence was seen in the third-month follow-up of the patient (Fig. 5).
Figure 1.

A polypoid mass on the midline on the anterior chest wall.
Figure 2.

A polypoid mass on the midline on the anterior chest wall.
Figure 3.
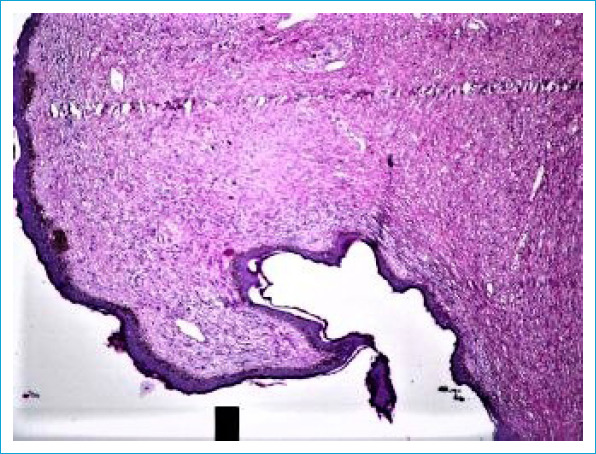
Tissue slide showing edematous stroma covered with papillomatous stratified squamous epithelium (Hematoxylin-Eosin, x4).
Figure 4.
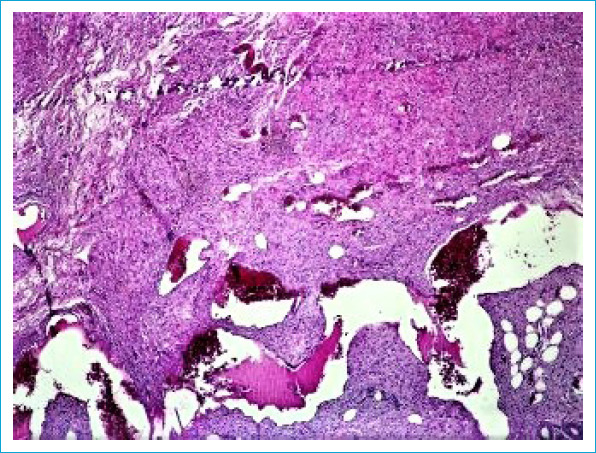
Conjugated, proliferated, dilated vascular structures in the stroma (Hematoxylin-Eosin, x4).
Figure 5.

Postoperative third month.
Discussion
Fibroepithelial polyps or acrochordons are benign skin tumors of mesenchymal and ectodermal origin. They are seen in 25% of the population and their frequency increases with age.[7] They are often found in areas with skin folds, such as the neck, axilla, submandibular or inguinal region. However, they can also be located in the genital tract. In this case, they have a hormone-sensitive epithelial structure and their incidence increases, especially in women at reproductive age.[2, 3]
There are three clinical types of FEPs: furrowed papules approximately 2 millimeters in width and height; filiform lesions, approximately 2 millimeters in width and 5 millimeters in height; and large bag-like protuberances. The term ‘acrochordon’ is used for the smaller lesions, while FEP is generally used for the latter.[8] They occasionally grow more than 5 centimeters and these are called giant FEP. In the literature, FEPs larger than 15 cm have been reported in the following locations: vulva,[2] axilla,[7] and thigh.[9, 10]
There are various hypotheses about why FEPs grow that much. It has been proposed that the epithelium of the FEPs located in the genital tract are hormone-sensitive, and extended hormone intake, pregnancy or hormonal changes can trigger their growth.[2, 3]
In the study presenting an 18 centimeters long giant FEP located at the axilla, it was suggested that morbid obesity of the patient might be the cause of the growth of FEP.[7] Indeed, insulin resistance and obesity have also been shown in different studies as a factor for the growth of FEPs.[6, 11]
The fact that our patient has a normal body mass index suggests that obesity and insulin resistance may not be a factor in the growth of FEP.
In 2004, Fetsch et al.[12] described a lymphedematous FEP on the penis associated with the use of chronic condom catheters. According to this study, allergic reactions that arise from edema, inflammation, latex allergy due to chronic condom catheter use may play a role in the pathogenesis of lymphedematous FEP. In the same study, local recurrence has been reported in two patients who continued to use the condom catheter after the excision of lymphedematous FEP.
The differences between lymphedematous FEP described by Fetsch et al. and cutaneous FEP were size, the presence of significant stromal edema and vascular dilatation, and higher stromal cellularity.
Due to congenital idiopathic hydrocephalus, a ventriculoperitoneal shunt was applied at certain intervals from birth in our patient. The shunt was 2 centimeters away from the current giant FEP. The presence of the shunt might have caused the excessive growth of the FEP, which was present at birth and grew to a length of 14 centimeters over time. Shunts can cause chronic inflammation due to foreign body reactions. This foreign body inflammation at the cellular level might have resulted in stromal edema and lymphatic stasis. It is also remarkable that stromal edema and increased numbers of inflammatory cells were reported in the pathology result. With these properties, it is similar to a lymphedematous FEP. However, the lymphedematous FEP described by Fetsch is seen only in the penis. Although our case is considered as cutaneous FEP, chronic inflammation, which is caused by the shunt, may be considered as a factor for excessive growth.
Although FEPs are benign skin tumors, they tend to regrow if not totally excised.[13] They can be treated with cryotherapy or cauterization when their size is in millimeters, while surgical excision is required in larger FEPs.[8] Therefore, we excised the lesion with a 5 millimeters safety margin. It is possible to close the resulting defect with local flaps or skin grafts. Reconstruction was planned with a skin graft in our patient who did not want additional scars on the anterior chest wall. If a large scar develops in the long term, a scar revision can be considered with the use of tissue expanders.
Disclosures
Informed consent: Written informed consent was obtained from the patient for the publication of the case report and the accompanying images.
Peer-review: Externally peer-reviewed.
Conflict of Interest: None declared.
Authorship Contributions: Concept – B.C.; Design – B.C.; Supervision – B.C.; Materials – B.C., A.Y.O.; Data collection &/or processing – B.C.; Analysis and/or interpretation – B.C.; Literature search – B.C.; Writing – B.C.; Critical review – B.C.
References
- 1.Kumar A, Hasin N, Sinha AK, Kumar S, Bhadani P. Giant fibro epithelial polyp in a young girl:A rare case report. Int J Surg Case Rep. 2017;38:83–5. doi: 10.1016/j.ijscr.2017.06.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agarval A, Garg C, Mukherjee S, Kakkar KP. Giant acrochordon of vulva:A rare occurence. NLJVD. 2015;13:70–2. [Google Scholar]
- 3.Banik R, Lubach D. Skin tags:localization and frequencies according to sex and age. Dermatologica. 1987;174:180–3. doi: 10.1159/000249169. [DOI] [PubMed] [Google Scholar]
- 4.Sari R, Akman A, Alpsoy E, Balci MK. The metabolic profile in patients with skin tags. Clin Exp Med. 2010;10:193–7. doi: 10.1007/s10238-009-0086-5. [DOI] [PubMed] [Google Scholar]
- 5.Tamega Ade A, Aranha AM, Guiotoku MM, Miot LD, Miot HA. Association between skin tags and insulin resistance. An Bras Dermatol. 2010;85:25–31. doi: 10.1590/s0365-05962010000100003. [DOI] [PubMed] [Google Scholar]
- 6.Rasi A, Soltani-Arabshahi R, Shahbazi N. Skin tag as a cutaneous marker for impaired carbohydrate metabolism:a case-control study. Int J Dermatol. 2007;46:1155–9. doi: 10.1111/j.1365-4632.2007.03287.x. [DOI] [PubMed] [Google Scholar]
- 7.Alkhalili E, Prapasiri S, Russell J. Giant acrochordon of the axilla. BMJ Case Rep. 2015;2015:bcr2015210623. doi: 10.1136/bcr-2015-210623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elder DE, Elenitsas R, Johnson BL, Ioffreda MD, Miller J, Miller OF. Fibroepithelial polyp. 2nd ed. Philadelphia: Lippincott Williams &Wilkins; 2007. Atlas and Synopsis of Lever's Hstopathology of the Skin; pp. 65–6. [Google Scholar]
- 9.Gupta R, Smita S, Sinha R, Sinha N, Sinha L. Giant fibroepithelial polyp of the thigh and retroperitoneal fibromatosis in a young woman:a rare case. Skeletal Radiol. 2018;47:1299–304. doi: 10.1007/s00256-018-2904-x. [DOI] [PubMed] [Google Scholar]
- 10.Bahce ZS, Akbulut S, Sogutcu N, Oztas T. Giant Acrochordon Arising from the Thigh. J Coll Physicians Surg Pak. 2015;25:839–40. [PubMed] [Google Scholar]
- 11.Bhargava P, Mathur SK, Mathur DK, Malpani S, Goel S, Agarwal US, et al. Acrochordon, diabetes and associations. Indian J Dermatol Venereol Leprol. 1996;62:226–8. [PubMed] [Google Scholar]
- 12.Fetsch JF, Davis CJ, Jr, Hallman JR, Chung LS, Lupton GP, Sesterhenn IA. Lymphedematous fibroepithelial polyps of the glans penis and prepuce:a clinicopathologic study of 7 cases demonstrating a strong association with chronic condom catheter use. Hum Pathol. 2004;35:190–5. doi: 10.1016/j.humpath.2003.08.021. [DOI] [PubMed] [Google Scholar]
- 13.Orosz Z, Lehoczky O, Szoke J, Pulay T. Recurrent giant fibroepithelial stromal polyp of the vulva associated with congenital lymphedema. Gynecol Oncol. 2005;98:168–71. doi: 10.1016/j.ygyno.2005.01.020. [DOI] [PubMed] [Google Scholar]


