Abstract
Purpose
To describe a case of macular hole retinal detachment in a high myope following intravitreal ocriplasmin injection.
Observations
A 71-year-old highly myopic (−18.63 Dioptres) female received 125 μg of intravitreal ocriplasmin (Jetrea, Oxurion, Leuven, Belgium) to treat a right, full-thickness macular hole (FTMH) with vitreomacular adhesion. Presenting best-corrected visual acuity (BCVA) letter score was 45, using the Early Treatment Diabetic Retinopathy Study chart. Past ocular history in the affected, pseudophakic eye included anisometropic amblyopia, but with a documented pre-morbid BCVA of 75 letters. One week post-injection the vitreomacular adhesion persisted. One month post-injection, a large posterior macular hole retinal detachment developed with BCVA of 45 letters. Over the course of one year she underwent three pars plana vitrectomies aiming to treat the retinal detachment and close the FTMH. The detachment was treated successfully but the FTMH persisted, albeit with a reduced diameter. Final BCVA was 55 letters.
Conclusions
The pathogenesis of this macular hole detachment may be related to the combination of a FTMH and high myopia. Ocriplasmin functions in a twofold manner; inducing a posterior vitreous detachment and as a proteolytic enzyme digesting the fibronectin and laminin at the pathological vitreoretinal interface. With access through a FTMH, ocriplasmin may exert an enzymatic effect on the interphotoreceptor matrix and the photoreceptor-retinal pigment epithelium interface that normally helps maintain neuroretinal adhesion to the retinal pigment epithelium. The reported increase in basal diameter of FTMHs following ocriplasmin supports this hypothesis. High myopia was another likely contributing factor. Highly myopic patients were excluded from the initial ocriplasmin registration studies, mainly due to the risk of retinal detachment, but were eligible for subsequent large trials.
Importance
Clinicians should be aware of a potential association between ocriplasmin and macular hole detachments in eyes with high myopia.
Keywords: Ocriplasmin, Myopia, Macular hole, Macular hole detachment, Vitreomacular adhesion, Retinal detachment
1. Introduction
We present a case of posterior macular hole retinal detachment following intravitreal ocriplasmin injection in a highly myopic eye, which may suggest a possible association.
2. Report of a case
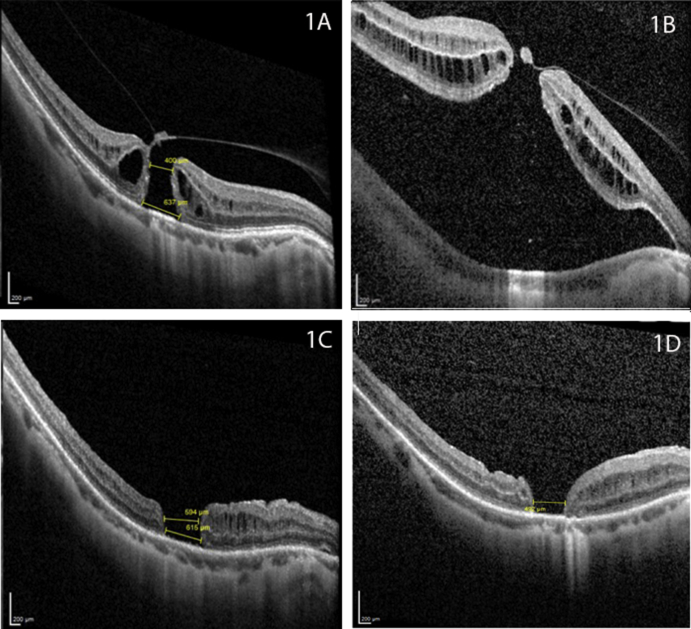
A 71-year-old highly myopic female received an intravitreal injection of 125 μg ocriplasmin (Jetrea, Oxurion, Leuven, Belgium) in her right, pseudophakic eye, to treat a full-thickness macular hole (FTMH) with vitreomacular adhesion (Fig. 1A). Right eye refractive spherical equivalent was −18.63 Dioptres (left: −7.38 Diopters). Right axial length measured 29.07mm (left: 27.74mm). The FTMH had an apical diameter of 400μm and a basal diameter of 637μm. Her pre-injection Early Treatment Diabetic Retinopathy Study (EDTRS) letter score was 45 letters. She had a past history of right anisometropic amblyopia, but had a recent best-corrected visual acuity (BCVA) of 75 ETDRS letters. One week post-injection, the vitreomacular adhesion was still evident with mild sub-foveal fluid; BCVA was unchanged at 45 letters. At a month post-injection review, a large, posterior, macular hole detachment (MHD) was evident, with persisting vitreous adhesion (Fig. 1B). BCVA remained 45 letters. Pars plana vitrectomy, internal limiting membrane peel and perfluoropropane tamponade successfully treated the MHD but the FTMH persisted (Fig. 1C). BCVA still remained 45 letters. The FTMH did not close with a subsequent vitrectomy and perfluoropropane, albeit with subjective benefit and a gain of BCVA to 55 letters, 2 months after surgery. The FTMH had a basal diameter of 612μm. A final vitrectomy and perfluoropropane tamponade was undertaken and this resulted in a smaller FTMH with a basal diameter of 497μm (Fig. 1D) at 2 months after surgery. Her BCVA was maintained at 55 letters. These three procedures were undertaken over a course of a year from the development of the MHD.
Image 1.
Spectral domain optical coherence tomography of the macula. Image A shows the macular hole at presentation, with an apical diameter of 400μm, and basal diameter of 637μm. Image B shows one month post-ocriplasmin. Image C shows the appearance after the initial vitrectomy, with an apical diameter of 594μm and basal diameter of 615μm. Image D shows the macula at final review, 2 months after her third and final vitrectomy, with a basal diameter of 497μm.
3. Discussion
Ocriplasmin is a 27.2-kDa recombinant serine protease, that is a truncated form of human plasmin, manufactured using recombinant DNA technology.1 Ocriplasmin functions in a twofold manner; by inducing a posterior vitreous detachment and as a proteolytic enzyme digesting fibronectin and laminin at the pathological vitreoretinal interface.1 With access through a FTMH, ocriplasmin's proteolytic action may also affect the interphotoreceptor matrix, particularly its fibronection and laminin components, as well as the interface between the outer photoreceptor segments and RPE, thereby, weakening neuroretinal adhesion.2,3 Consistent with this hypothesis, increased basal diameter of FTMHs following ocriplasmin have been reported,2 which may reflect a lifting of the margin of the hole due to weakened interphotoreceptor adhesion. Furthermore, the Microplasmin Intravitreal Injection for Traction Release without Surgical Treatment (MIVI TRUST) trial found that subfoveal lucency developed in nearly all closed holes, but its width was increased from that of the original hole. It was also larger and persisted for longer in eyes treated with ocriplasmin compared to placebo or vitrectomy groups.4 Subfoveal lucency is a focal neurosensory detachment similar to our case, albeit to a lesser extent.3 It has been described as a hyporeflective space within the central 1 mm macular field on SD-OCT, not associated with angiographic leakage.4 Additionally, perhaps due to its small molecular size, ocriplasmin appears able to cross the retina to the subretinal space, as subfoveal lucency has been described in the presence of vitreomacular adhesion or traction without holes.3 However, this study suggested that the development of subfoveal lucency due to ocriplasmin did not carry a visual impact, rather, persistent subfoveal lucency in ocriplasmin-treated eyes at 6 months only translated to poorer visual acuity if it was associated with vitreomacular adhesion or traction.
We presume that high myopia was also contributory. Due to the excessive globe elongation and the resultant abnormal contour at the vitreomacular interface, highly myopic eyes are prone to macular detachments.5 These risks may be further increased with ocriplasmin use. A case series of eight patients with rhegmatogenous retinal detachment occurring after ocriplasmin injection included one high myope.6 The ocriplasmin registration trials excluded myopia greater than 8D,1 although subsequent large trials did not.7
Clinicians should be aware of a potential association between ocriplasmin and MHD in eyes with high myopia.
Declaration of competing interest
Dr Goh, Mr Motta and Professor Jackson are/were employed by King's College Hospital NHS Trust, which receives site payments for participants enrolled on clinical trials of ocriplasmin (Jetrea, Oxurion, Leuven, Belgium). Prof. Jackson is also an advisor to Alcon.
None of the authors received any funding for their role in producing this piece of work.
Abbreviations
- FTMH
Full thickness macular hole
- ETDRS
Early treatment diabetic retinopathy study
- MHD
Macular hole detachment
Patient consent
The patient consented to publication of the case in writing.
Author contributions
Li Yen Goh – Conceptualisation, project administration, visualization, roles/writing – original draft, writing – review and editing.
Lorenzo Motta - Conceptualisation, project administration, visualization, writing – review and editing. Timothy L. Jackson - Conceptualisation, project administration, visualization, writing – review and editing, supervision.
References
- 1.Stalmans P., Benz M.S., Gandorfer A. Enzymatic vitreolysis with ocriplasmin for vitreomacular traction and macular holes. N Engl J Med. 2012;367(7):606–615. doi: 10.1056/NEJMoa1110823. [DOI] [PubMed] [Google Scholar]
- 2.Haynes R.J., Yorston D., Laidlaw D.A., Keller J., Steel D.H. Real world outcomes of ocriplasmin use by members of the British and Eire Association of Vitreoretinal Surgeons. Eye. 2017;31(1):107–112. doi: 10.1038/eye.2016.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas A.S., Folgar F.A., Jaffe G.J., Toth C.A., Mahmoud T.H. Subfoveal lucency after treatment of vitreomacular traction without macular hole in the phase 3 trials of ocriplasmin vitreolysis. Ophthalmol Retina. 2019;3(1):42–52. doi: 10.1016/j.oret.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Folgar F.A., Jaffe G.J., Toth C.A., Mahmoud T.H. Recovery of foveal anatomy and subfoveal lucency after pharmacologic and surgical macular hole closure in the ocriplasmin phase III trials. Ophthalmol Retina. 2017;1(3):240–248. doi: 10.1016/j.oret.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 5.Gohil R., Sivaprasad S., Han L.T., Mathew R., Kiousis G., Yang Y. Myopic foveoschisis: a clinical review. Eye. 2015;29(5):593–601. doi: 10.1038/eye.2014.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madi H.A., Haynes R.J., Depla D. Rhegmatogenous retinal detachment following intravitreal ocriplasmin. Graefes Arch Clin Exp Ophthalmol. 2016;254(12):2333–2338. doi: 10.1007/s00417-016-3398-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dugel P.U., Tolentino M., Feiner L., Kozma P., Leroy A. Results of the 2-year ocriplasmin for treatment for symptomatic vitreomacular adhesion including macular hole (OASIS) randomized trial. Ophthalmology. 2016;123(10):2232–2247. doi: 10.1016/j.ophtha.2016.06.043. [DOI] [PubMed] [Google Scholar]