Abstract
Pruritus is a debilitating symptom for patients with Alagille syndrome (ALGS). In a previously reported trial of maralixibat, an investigational antipruritic agent, itching was assessed using a digital diary based on twice‐daily caregiver observation of itching severity (Itch Reported Outcome, ItchRO[Observer]). The goal of this study was to characterize pruritus in participants with ALGS at baseline in this trial, as assessed by the ItchRO instrument and the physician‐observed clinician scratch scale (CSS), relative to biomarkers putatively associated with pruritus and health‐related quality of life assessment. Thirty‐seven participants with ALGS (median age of 6 years; range 1‐17 years) were enrolled. No association was identified between CSS and ItchRO(Obs) (r = 0.22, P = 0.2). Neither CSS nor ItchRO were associated with serum bile acids (r = −0.08, P = 0.6 for both) or autotaxin (r = 0.22, P = 0.2; r = 0.28, P = 0.12). There was no significant association between Pediatric Quality of Life Inventory total parent scores and CSS or ItchRO (r = −0.23, P = 0.2; r = −0.16, P = 0.36). There was a significant association between ItchRO and Multidimensional Fatigue Scale and Family Impact Module total scores (Pearson correlation coefficient −0.575, P = 0.0005; 0.504, P = 0.002). In exploratory analysis, selected questions relating to fatigue and sleep disturbance (n = 12) from Pediatric Quality of Life Inventory, Multidimensional Fatigue Scale, and Family Impact Module were correlated with pruritus scores; positive associations were identified. Conclusion: Itching scores did not correlate with each other, nor with putative serum biomarkers of pruritus, and further, did not correlate with quality of life. Hypothesis‐generating analyses implicate sleep disturbance and fatigue as key associations with caregiver observations of itching. This is highly relevant to the selection of surrogate endpoints for clinical trials of pruritus therapies.
Itching scores did not correlate with each other, nor with putative serum biomarkers of pruritus, and did not correlate with quality of life. Hypothesis‐generating analyses implicate sleep disturbance and fatigue as key associations with caregiver observations of itching. This is highly relevant to the selection of surrogate endpoints for clinical trials of pruritus therapies.

Abbreviations
- ALGS
Alagille syndrome
- CSS
Clinician Scratch Scale
- FIM
Family Impact Module
- GGT
gamma‐glutamyltransferase
- HRQOL
health‐related quality of life
- ItchRO
Itch‐Reported Outcome
- MFS
Multidimensional Fatigue Scale
- PedsQL
Pediatric Quality of Life Inventory
- PRO
patient‐reported outcome
- TB
total bilirubin
Alagille syndrome (ALGS) is an autosomal‐dominant, variably penetrant multisystem genetic disorder and one of the most common causes of inherited cholestasis in children. Pruritus is a debilitating symptom for many patients with ALGS and has been reported to be an important determinant of health‐related quality of life (HRQOL) in this population.( 1 ) Pruritus in cholestasis is a management challenge, and novel therapies are currently under evaluation. However, the pathophysiology and biochemical correlates of cholestasis‐induced pruritus have not been elucidated, resulting in difficulties in selecting appropriate endpoints for the evaluation of novel therapies for pruritus in children.( 2 ) Patient‐reported outcomes (PROs) are considered a crucial endpoint in the evaluation of therapies that target symptoms; however, there are a limited number of disease‐specific or symptom‐specific instruments to measure PROs in children. To address this gap, a tool to specifically assess pruritus in children with ALGS was recently developed using standard qualitative methodology.( 3 ) This instrument, Itch‐Reported Outcome (ItchRO), was administered as an electronic daily diary to caregivers and age‐eligible subjects enrolled in a randomized double‐blind placebo‐controlled trial (ITCH, NCT02057692) of maralixibat (previously LUM001; SHP625), an apical sodium‐dependent bile acid transporter inhibitor, for cholestasis‐induced pruritus in ALGS.( 4 )
The goal of the current study was to characterize pruritus, as assessed by the ItchRO instrument, relative to current scales, HRQOL assessment, and associated biomarkers in participants with ALGS at baseline in the ITCH trial. We hypothesized that ItchRO would be associated with markers of cholestasis, such as serum bile acids and/or bilirubin. We further hypothesized that pruritus would be associated with impaired HRQOL in this cohort and that, in particular, child and parental fatigue and sleep disturbance would be consequences of pruritus in cholestatic children with ALGS.
Experimental Procedures
Children with ALGS were enrolled in the ITCH trial as per the study inclusion/exclusion criteria.( 4 ) Written informed consent was obtained from caregivers, and assent was obtained when appropriate from the child according to local institutional review board rules. This study was approved by local institutional review boards and complied with the Declaration of Helsinki and Good Clinical Practice Guidelines. The study was registered at ClinicalTrials.gov (02057692).
Itching was assessed at baseline (i.e., before administration of maralixibat or placebo in participants using the digital diary based on twice‐daily caregiver observation of itching severity [ItchRO(Obs)])( 3 ) (Fig. 1). Scores range from 0‐4, with 4 being the most severe itching in a day observed by caregivers, with the overall score calculated as the average of the daily ItchRO scores over the 2 consecutive weeks during the screening period. Subjects were eligible for the trial if they had an average daily ItchRO(Obs) score of 2 or higher over 2 consecutive weeks during the screening period. The Clinician Scratch Scale (CSS) was also assessed by the study investigator at baseline. This scale is based on clinician observation of scratching and/or physical evidence of scratching, such as excoriations, and is also scored 0‐4, with 4 representing the worst scratching.( 5 )
Fig. 1.
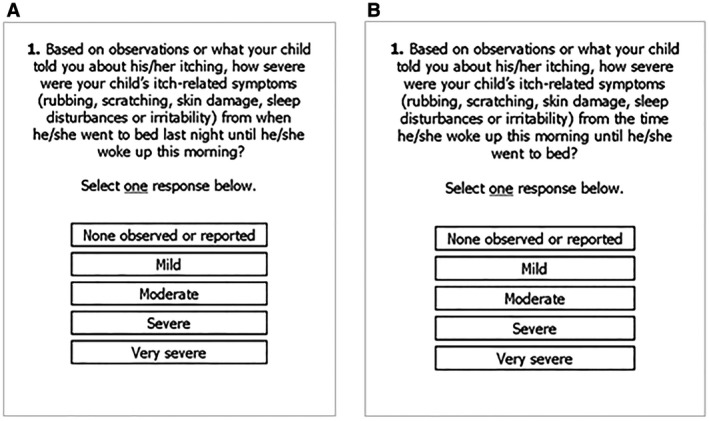
Screenshots of morning (A) and evening ItchRO (B) electronic diary.
HRQOL was assessed at baseline in the study cohort using three measurement tools. The Pediatric Quality of Life Inventory (PedsQL) is a validated, generic tool designed to measure HRQOL in children and adolescents.( 6 ) The PedsQL Family Impact Module (FIM) measures the impact of pediatric chronic health conditions on parents and the family. The FIM encompasses parent self‐reported physical, emotional, social, and cognitive functioning; communication; and family daily activities.( 7 ) The Multidimensional Fatigue Scale (MFS) is another module of PedsQL that specifically measures fatigue in children and has been validated in chronic disease populations.( 8 )
Liver‐related biochemistries were recorded. In addition, serum biomarkers considered to be associated with pruritus were assessed at baseline. These putative pruritus‐associated biomarkers, included fasting bile acids, autotaxin (the enzyme synthesizing lysophosphatidic acid),( 9 ) and C4 (7‐alpha‐hydroxy‐4‐cholesten‐3‐one, a biomarker of bile acid biosynthesis).
Statistical Analysis
Pearson correlations were calculated to assess the association between baseline itching scores and biomarkers.
On the PedsQL Generic Core Scales, items are reverse‐scored and linearly transformed to a 0‐100 scale, so that higher scores indicate better HRQOL. The Total Scale Score is the average of all items completed (i.e., the sum of all items divided by the number of items answered on all the scales).( 10 ) For this study, Total Scale Scores were generated by caregiver/parent reporting. In a large, healthy population, the mean and SD were 82.3 and 15.6.( 6 ) A value of 1 SD below the population mean for the PedsQL Total Scale Score (65.4 for parent proxy) is considered a threshold score for an at‐risk status for impaired HRQOL relative to a population sample.( 6 ) The PedsQL FIM has 36 items measured on a 5‐point Likert scale from 0 (never) to 4 (almost always). Scores are reverse‐scored and transformed to a 0‐100 scale (i.e., 0 = 100, 1 = 75, 2 = 50, 3 = 25, and 4 = 0) before averaging the relevant items for scale scores for the eight dimensions and all items for the total score.( 7 ) The PedsQL MFS has 18 items measured on a 5‐point Likert scale (as described previously) or on a 3‐point scale for young children (ages 5‐7), with 0 (not at all), 2 (sometimes), and 4 (a lot). Scores are reverse‐scored and transformed as described previously and averaged for three scale scores for three dimensions and for an overall total score.( 8 ) For the MFS and FIM scales, higher scores indicate fewer problems.
Results
Thirty‐seven participants with median age of 6 years (range 1‐17 years) were enrolled. Thirty‐five had disease‐causing mutations in JAGGED1 and two in NOTCH2. Baseline characteristics of the cohort (Table 1) indicated that the group had elevated gamma‐glutamyltransferase (GGT) levels, with variable elevations of total bilirubin, fasting serum bile acid levels, and total cholesterol. Serum alanine aminotransferase levels were modestly elevated. The median ItchRO score at baseline was 2.9, which was expected, as an ItchRO score of 2 or higher was an enrollment criterion. Of note, this cohort of children with cholestatic ALGS reported low median Total Scale Scores on parent‐reported PedsQL (67, interquartile range 51‐80), which represents impaired HRQOL, similar to data we previously published in a large cohort of subjects with ALGS.( 11 )
Table 1.
Baseline Characteristics of ALGS Study Cohort (N = 37)
| Mean (SD) | Median (IQR) | |
|---|---|---|
| TB, mg/dL | 5.3 (6.18) | 2.1 (0.9‐7.2) |
| ALT, U/L | 159 (86.5) | 137 (91‐214) |
| GGT, U/L | 495 (379.8) | 329 (203‐834) |
| Total cholesterol, mg/dL | 406 (313.6) | 320 (231‐443) |
| Bile acids, μM | 216 (203.3) | 155 (57‐310) |
| C4, ng/mL | 13.7 (28.23) | 4.0 (1.5‐12.8) |
| ATX, ng/mL | 2,621 (1,672) | 2,114 (1,574‐3,264) |
| CSS | 3.0 (1.07) | 3 (2‐4) |
| ItchRO | 2.9 (0.60) | 2.9 (2.6‐3.1) |
| PedsQL total score | 65 (20.1) | 67 (51‐80) |
Abbreviations: ALT, alanine aminotransferase; ATX, autotaxin; C4, complement component 4; IQR, interquartile range; TB, total bilirubin.
Surprisingly, no association was identified between CSS (physician‐observed) and ItchRO (caregiver‐reported) scores (r = 0.22, P = 0.2). None of these measures of pruritus, CSS, and ItchRO were associated with the putative biomarkers of cholestasis, total bilirubin (r = −0.15, P = 0.4 for CSS; r = −0.14, P = 0.4 for ItchRO), serum bile acids (r = −0.08, P = 0.6 for both), or autotaxin levels (r = 0.22, P = 0.2 for CSS; r = 0.28, P = 0.1 for ItchRO).
Despite the markedly reduced PedsQL (parent) total scores, there was no significant association between these scores and CSS or ItchRO scores (r = −0.23, P = 0.2 for CSS; r = −0.16, P = 0.36 for ItchRO). Of note, there was a statistically significant association between ItchRO and both the MFS total score (Pearson correlation coefficient −0.575, P = 0.0005) and the FIM total score (Pearson correlation coefficient −0.504, P = 0.002). The associations between the subdomains of these scores is given in Table 2. There was a negative association between CSS and the MFS or FIM total scores.
Table 2.
PedsQL Pearson Correlations: ItchRO(Obs) and CSS Versus MFS and FIM
| PedsQL Domains | ItchRO | CSS | ||
|---|---|---|---|---|
| r | P Value | r | P Value | |
| MFS total score | −0.575 | 0.0005 | −0.196 | 0.2755 |
| Dimension score, general fatigue | −0.616 | 0.0005 | −0.139 | 0.2755 |
| Dimension score, sleep/rest fatigue | −0.518 | 0.0020 | −0.187 | 0.2985 |
| Dimension score, cognitive fatigue | −0.376 | 0.0312 | −0.200 | 0.2649 |
| FIM total score | −0.504 | 0.0020 | −0.285 | 0.0969 |
| Family functioning summary score | −0.328 | 0.0543 | −0.294 | 0.0867 |
| Parent HRQOL summary score | −0.522 | 0.0013 | −0.275 | 0.1096 |
| Dimension score, physical functioning | −0.508 | 0.0018 | −0.228 | 0.1874 |
| Dimension score, emotional functioning | −0.499 | 0.0023 | −0.307 | 0.0724 |
| Dimension score, social functioning | −0.424 | 0.0112 | −0.205 | 0.2366 |
| Dimension score, cognitive functioning | −0.344 | 0.0431 | −0.205 | 0.2368 |
| Dimension score, communication | −0.399 | 0.0176 | −0.144 | 0.4098 |
| Dimension score, worry | −0.429 | 0.0101 | −0.186 | 0.2843 |
| Dimension score, daily activities | −0.354 | 0.0372 | −0.248 | 0.1506 |
| Dimension score, family relationships | −0.276 | 0.1085 | −0.293 | 0.0873 |
Bold values are those that are statistically significant with P < 0.05.
Although the clinician and caregiver assessments of itch did not demonstrate association with PedsQL total scores, based on the positive associations noted with the MFS and the FIM, we proceeded with an exploratory analysis to test the hypothesis that pruritus, as assessed by ItchRO, in a child with ALGS may be associated with child and parental fatigue and/or sleep disturbance. Selected questions (n = 12) from PedsQL, MFS, and FIM were tested for their association with CSS and ItchRO scores (Table 3). The correlations for individual questions were not reverse‐scored, as was done for the subscales of the PedsQL, to aid in interpretation. Thus, the magnitude of the correlation coefficient is of interest (and may not be negative depending on the wording of the individual PedsQL question). This analysis revealed a negative association between ItchRO scores and CSS with questions from the Physical Function domain of the PedsQL, which are related to physical activity. However, individual questions related to sleep and fatigue from each tool did show an association with ItchRO(Obs), with one exception: There was a negative association with CSS (Table 3). For instance, questions to parents/caregivers regarding their children having trouble sleeping and having difficulty sleeping through the night were strongly associated with ItchRO(Obs) (P = 0.002 and P = 0.005, respectively). These associations were not seen with CSS. In addition, questions that specifically explored parental fatigue in the morning and throughout the day were also strongly associated with ItchRO(Obs) (P < 0.001 and P = 0.001, respectively).
Table 3.
Pearson Correlations Between ItchRO(Obs) and CSS Versus Selected Questions From HRQOL Tool Questions Related to Physical Function or Fatigue
| ItchRO | CSS | |||
|---|---|---|---|---|
| r | P Value | r | P Value | |
| Measurements of effect on patient, reported by parent/caregiver* | ||||
| Physical function, hard to walk more than 1 block | −0.022 | 0.9015 | −0.131 | 0.4586 |
| Physical function, hard to run | 0.045 | 0.8023 | −0.045 | 0.7988 |
| Physical function, hard to do sports activity | 0.086 | 0.6298 | 0.111 | 0.5329 |
| Physical function, low energy* | 0.486 | 0.0035 | 0.231 | 0.1878 |
| Emotional functioning, trouble sleeping* | 0.504 | 0.0024 | 0.137 | 0.4396 |
| School functioning, paying attention in class (doing school activities as peers) | 0.088 | 0.6695 | 0.053 | 0.7970 |
| MFS, feeling tired † | 0.671 | <0.0001 | 0.102 | 0.5723 |
| MFS, difficulty sleeping through the night † | 0.480 | 0.0047 | 0.043 | 0.8103 |
| Measurements of effect on family (identify family, parent, patient), reported by parent/caregiver ‡ | ||||
| Parent family impact module, feeling tired during the day | 0.627 | < 0.0001 | 0.044 | 0.8005 |
| Parent family impact module, feeling tired when I wake up in the morning | 0.531 | 0.0010 | 0.227 | 0.1897 |
| Parent family impact module, feeling too tired to do the things I like to do | 0.388 | 0.0211 | 0.348 | 0.0403 |
| Parent family impact module, feeling too tired to finish household tasks | 0.288 | 0.0930 | 0.238 | 0.1685 |
Bold values are those that are statistically significant with P < 0.05.
Select questions from PedsQL.
Select questions from MFS.
Select questions from FIM (these four questions reflect how parents feel about themselves).
Those specific questions showing a strong association with ItchRO(Obs) were tested for correlations with the putative biomarkers of pruritus, which were explored previously (total bilirubin, serum bile acids, total cholesterol, GGT, or autotaxin) and no clear associations were seen.
Discussion
This study highlights the complexity of assessing pruritus in children with ALGS; these challenges are easily extrapolated to other cholestatic conditions. Unexpectedly, there was a lack of association between clinician and caregiver observations of itching. Furthermore, our data did not demonstrate any association between clinician and caregiver observations of itching among patients with moderate to severe itching with putative serum biomarkers of pruritus. The biomarkers assessed in this study included traditional measures of cholestasis, bilirubin, and GGT, as well as markers such as autotaxin. It is of particular note that the CSS and ItchRO were not associated with serum bile acids, as these are the target of the drug (maralixibat) that was evaluated in the ITCH trial.
In this study, subjects with ALGS at the beginning of the trial had impaired HRQOL, as assessed with a generic tool, but the PedsQL total scores did not vary by the level of pruritus, as reported by caregivers or clinicians. We previously reported that HRQOL is impaired in a larger cohort of children with ALGS, using PedsQL; similarly, pruritus was not identified as a determinant of HRQOL.( 11 ) It is possible that other factors, such as cardiac defects and growth failure, have a stronger impact that minimizes the incremental change in generic HRQOL across the spectrum of moderate to severe pruritus. HRQOL tools that are specifically designed to assess sleep and fatigue in patients, and impact of a chronic disease on caregivers’ fatigue, did show strong associations with ItchRO. The finding that sleep and itching are linked is not surprising to health care professionals caring for children with ALGS; however, this is the first study to identify and quantify the strength of this association. These associations were supported by hypothesis‐generating analyses that demonstrated relationships of pruritus scores with selected QOL questions relating to sleep and fatigue. This highlights the limitations of relying solely on generic measures of HRQOL, as these may dilute or mask clinically important associations. These data support our hypothesis that sleep disturbance is associated with pruritus and, together, these likely impact HRQOL. These data also suggest that detailed assessment of sleep, with newer questionnaires (e.g., the Patient‐Reported Outcomes Measurement Information System Pediatric Sleep Disturbance and Sleep‐Related Impairment item banks)( 12 ) or with novel tools (e.g., actigraphy), could be used to characterize the sleep disturbance and fatigue in children with ALGS. Such assessments could be incorporated into future clinical trial design to evaluate the effects of novel pruritus therapies.
Pruritus is also a hallmark symptom of atopic dermatitis, and scratching is often worse at night. The relationship between itching and sleep disturbance with subsequent negative impact on individual and family quality of life has been well‐studied in atopic dermatitis.( 13 , 14 ) A recently published longitudinal study of almost 14,000 children (of whom 4,938 had atopic dermatitis) reported on repeated sleep questionnaire–based data throughout childhood.( 15 ) Children with atopic dermatitis had similar sleep duration than those without; however, their sleep quality was markedly impaired, and they reported sleep disturbance such as difficulty falling asleep and early morning waking. These findings are consistent with smaller cross‐sectional studies that used polysomnography and actigraphy. The studies reported poor sleep efficiency and sleep fragmentation among children with atopic dermatitis.( 16 , 17 ) Such detailed assessments and characterization of sleep disturbance are clearly lacking in children with cholestatic pruritus.
This study is limited by the relatively small sample size, although the prospective nature and detailed assessments of the cohort obviate some of this limitation. It should also be noted that only patients with moderate to severe pruritus were studied, as this was a requirement for inclusion in the clinical trial. Hence, any potential associations with the full spectrum of pruritus, including mild or minimal pruritus, could not be observed. In addition, pruritus was assessed using caregiver, rather than patient, reports, as ItchRO is not administered to children under the age of 8 years. This was necessary to maintain consistency across the cohort, and a tool to capture pruritus in younger children with cholestasis is not available. Finally, this study only assessed baseline measures. Longitudinal patient‐specific alterations in associated outcomes or biomarkers await further study.
In conclusion, this study highlights the challenges of assessing pruritus in children with ALGS, and likely other cholestatic conditions. Clinician and caregiver observations of itching did not correlate with each other, nor with putative serum biomarkers of pruritus. The severity of pruritus, measured with either a physician‐observed tool or disease‐specific caregiver PRO, did not correlate with quality of life, assessed with a generic tool. Hypothesis‐generating analyses performed here implicate sleep disturbance and fatigue in patients and their parents/caregivers as key associations with caregiver observations of itching. These observations are highly relevant to the selection of surrogate endpoints for clinical trials of therapies for pruritus and argue in favor of the inclusion of specific assessments of sleep disturbance in ALGS in future studies. PROs are highly valued in clinical trials; however, there are particular problems with the use of PROs in pediatric studies, as they typically rely on parent/caregiver observations. The lack of association of any of these instruments or individual questions with biomarkers of pruritus also highlights the gaps in knowledge regarding mechanisms underlying pruritus and the elusive cholestatic pruritogen. Until a true biomarker of cholestatic pruritus is identified, we are constrained by available clinical instruments. Perhaps objective assessment of sleep disturbance may improve measurement of the severity and impact of pruritus and the evaluation of novel therapies.
Acknowledgments
The authors thank Heather Van Doren, senior medical editor with Arbor Research Collaborative for Health, for providing editorial assistance on this manuscript.
Financial Support: National Institute of Diabetes and Digestive and Kidney Diseases (DK 62436, DK 62445, DK 62453, DK 62456, DK 62466, DK 62470, DK 62481, DK 62497, DK 62500, DK 84536, DK 84538, DK 84575, DK103135, DK103140, and DK103149); and the National Center for Advancing Translational Sciences (UL1 RR025014, UL1 TR000423, UL1 TR001857, UL1 TR001872, UL1 TR001878, UL1 TR002535, UL1TR00130, and UL1TR002378).
Potential conflict of Interest: Dr. Setchell owns stock in Asklepion. He consults for and received grants from Retrophin. Dr. Molleston received grants from Gilead, Abbvie, and Mirum. Dr. Karpen consults for Albireo, Mirum, Intercept, Spruce Bioscience, and LogicBio. Dr. Loomes consults for and received grants from Albireo and Mirum. Dr. Mack consults for Albireo. Dr. Miethke consults for Mirum and Metacrine. Dr. Rosenthal consults for and received grants from Gilead, Abbvie, and Retrophin. He consults for Albireo, Mirum, and Audentes. He received grants from Merck. Dr. Sokol consults for and received grants from Shire and Mirum. He consults for Retrophin and Albireo. Dr. Spino consults for Albireo. Dr. Kamath consults for and received grants from Mirum and Albireo. She also consults for Shire. Dr. Murray consults for and received grants from Gilead. She received grants from Merck.
References
- 1. Elisofon SA, Emerick KM, Sinacore JM, Alonso EM. Health status of patients with Alagille syndrome. J Pediatr Gastroenterol Nutr 2010;51:759‐765. [DOI] [PubMed] [Google Scholar]
- 2. Beuers U, Kremer AE, Bolier R, Elferink RP. Pruritus in cholestasis: facts and fiction. Hepatology 2014;60:399‐407. [DOI] [PubMed] [Google Scholar]
- 3. Kamath BM, Abetz‐Webb L, Kennedy C, Hepburn B, Gauthier M, Johnson N, et al. Development of a novel tool to assess the impact of itching in pediatric cholestasis. Patient 2018;11:69‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shneider BL, Spino C, Kamath BM, Magee JC, Bass LM, Setchell KD, et al. Placebo‐controlled randomized trial of an intestinal bile salt transport inhibitor for pruritus in Alagille syndrome. Hepatol Commun 2018;2:1184‐1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Whitington PF, Whitington GL. Partial external diversion of bile for the treatment of intractable pruritus associated with intrahepatic cholestasis. Gastroenterology 1988;95:130‐136. [DOI] [PubMed] [Google Scholar]
- 6. Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 2003;3:329‐341. [DOI] [PubMed] [Google Scholar]
- 7. Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P. The PedsQL Family Impact Module: preliminary reliability and validity. Health Qual Life Outcomes 2004;2:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Varni JW, Burwinkle TM, Szer IS. The PedsQL Multidimensional Fatigue Scale in pediatric rheumatology: reliability and validity. J Rheumatol 2004;31:2494‐2500. [PubMed] [Google Scholar]
- 9. Kremer AE, Gonzales E, Schaap FG, Elferink RP, Jacquemin E, Beuers U. Serum autotaxin activity correlates with pruritus in pediatric cholestatic disorders. J Pediatr Gastroenterol Nutr 2016;62:530‐535. [DOI] [PubMed] [Google Scholar]
- 10. Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800‐812. [DOI] [PubMed] [Google Scholar]
- 11. Kamath BM, Chen Z, Romero R, Fredericks EM, Alonso EM, Arnon R, et al. Quality of life and its determinants in a multicenter cohort of children with Alagille syndrome. J Pediatr 2015;167:390‐396.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Forrest CB, Meltzer LJ, Marcus CL, de la Motte A, Kratchman A, Buysse DJ, et al. Development and validation of the PROMIS Pediatric Sleep Disturbance and Sleep‐Related Impairment item banks. Sleep 2018;41:1‐13. [DOI] [PubMed] [Google Scholar]
- 13. Lewis‐Jones S. Quality of life and childhood atopic dermatitis: the misery of living with childhood eczema. Int J Clin Pract 2006;60:984‐992. [DOI] [PubMed] [Google Scholar]
- 14. Yang EJ, Beck KM, Sekhon S, Bhutani T, Koo J. The impact of pediatric atopic dermatitis on families: a review. Pediatr Dermatol 2019;36:66‐71. [DOI] [PubMed] [Google Scholar]
- 15. Ramirez FD, Chen S, Langan SM, Prather AA, McCulloch CE, Kidd SA, et al. Association of atopic dermatitis with sleep quality in children. JAMA Pediatr 2019;173:e190025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chang YS, Chou YT, Lee JH, Lee PL, Dai YS, Sun C, et al. Atopic dermatitis, melatonin, and sleep disturbance. Pediatrics 2014;134:e397‐e405. [DOI] [PubMed] [Google Scholar]
- 17. Fishbein AB, Mueller K, Kruse L, Boor P, Sheldon S, Zee P, et al. Sleep disturbance in children with moderate/severe atopic dermatitis: a case‐control study. J Am Acad Dermatol 2018;78:336‐341. [DOI] [PubMed] [Google Scholar]


