Dear Editor,
We read with interest the recent article by de Lange et al. entitled “ICU beds, less is more? No” [1]. We agree with the authors that the increasing number of vulnerable and elderly patients, of complex surgical procedures and of “just in case” ICU admissions for observation, may require a transformation of our hospitals. The COVID-19 crisis also revealed the limitations of our current structures to welcome a surge of acutely ill patients requiring hospitalization and close monitoring. However, although increasing the number of ICU beds is an option, we believe that upgrading monitoring methods on hospital wards may be part of the solution as well.
Multiple wireless wearable sensors are now available to monitor vital signs non-invasively and continuously. They include adhesive patches, necklaces, and finger sensors to monitor heart rate, respiratory rate, oxygen saturation, skin temperature, and/or changes in blood pressure [2]. They are increasingly used in surgical wards to detect postoperative complications at an early stage and tackle “failure to rescue” [3]. When nurses spot-check vital signs every 4–8 h, they miss a significant number of adverse events, including severe hypoxemic events [3]. Studies have shown that continuous monitoring of vital signs enables the immediate detection of clinical deterioration and, pending appropriate intervention, a decrease in cardiac arrest and ICU admission [2, 4]. During the COVID-19 crisis, a large number of patients requiring oxygen and at risk of rapid deterioration have been admitted at the same time. Several hospitals have therefore quickly equipped their wards with wireless pulse oximeters to cope with that surge.
On hospital wards, the nurse/patient ratio is much lower than in ICUs and clinicians are not used to deal with life-threatening clinical situations. Therefore, we cannot envision to simply acquire existing ICU monitoring systems to install them on the wards. We have to implement systems specifically designed for the wards. Such systems are currently under development or evaluation. They usually include wearable sensors which are easy to set up (e.g., adhesive patch on the skin) and enable wireless monitoring, which, in the context of epidemics, has the advantage to decrease the number of physical interactions and the risk of contamination. Artifacts and false alarms, common in non-sedated patients, need to be filtered, and machine learning algorithms may help to achieve that goal [5]. Medical-grade connectivity protocols are necessary to prevent connectivity disruptions, common with classical Bluetooth connections. Smart algorithms are also needed to aggregate and fuse vital signs into a single early warning score or deterioration index so that nurses can only respond to “smart” alerts received at a central station or directly on their pager [4]. By doing so, one may envision the possibility to ask ward nurses to look after a large number of patients without increasing their workload [2]. Indeed, focusing on patients who are deteriorating, as soon as they do, should improve work efficiency. However, this remains to be confirmed by large clinical studies done in real-life conditions. Finally, to be useful, such remote monitoring systems need to direct the alert to the right person. For instance, if ward nurses could be informed first in case of mild deterioration, rapid response teams would need to be alerted directly in case of life-threatening clinical condition requiring immediate intervention.
Therefore, in the hospital of the future, ICU beds could be reserved to patients requiring organ support such as mechanical ventilation and renal replacement therapy. Patients who would simply need close monitoring could safely stay on the wards and benefit from smart and continuous monitoring (Fig. 1). This strategy may help to improve patient safety and quality of hospital care without dramatically increasing the number of ICU beds and associated costs.
Fig. 1.
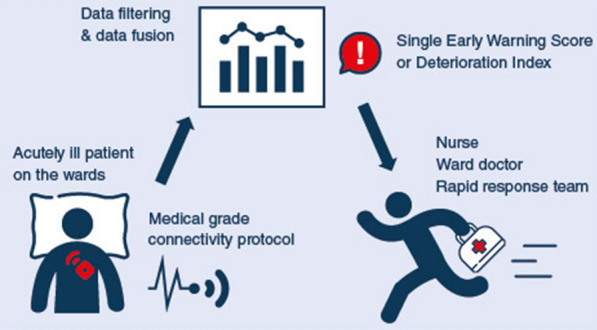
On hospital wards, continuous monitoring of vital signs with wearable and wireless sensors may enable the early detection of clinical deterioration, timely intervention, and the prevention of severe adverse events such as cardiac arrest, ICU transfer, and death
Compliance with ethical standards
Conflicts of interest
FM is the founder and managing director of MiCo (michardconsulting.com), a Swiss consulting firm that provides advisory and research services to medtech companies, some of them developing mobile monitoring solutions. MiCo does not sell any medical products and FM does not own shares from any medtech company. BS has received honoraria for consulting, honoraria for giving lectures, refunds of travel expenses or institutional restricted research grants from Edwards Lifesciences (Irvine, CA, USA), Pulsion Medical Systems (Feldkirchen, Germany), CNSystems (Graz, Austria), Retia Medical (Valhalla, NY, USA), Philips (Böblingen, Germany), and Tensys Medical (San Diego, CA, USA). BV has no conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.de Lange DW, Soares M, Pilcher D. ICU beds: less is more? No. Intensive Care Med. 2020 doi: 10.1007/s00134-020-06089-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michard F, Bellomo R, Taenzer A. The rise of ward monitoring: opportunities and challenges for critical care specialists. Intensive Care Med. 2019;45:671–673. doi: 10.1007/s00134-018-5384-5. [DOI] [PubMed] [Google Scholar]
- 3.Sessler DI, Saugel B. Beyond “failure to rescue”: the time has come for continuous ward monitoring. Br J Anaesth. 2019;122:304–306. doi: 10.1016/j.bja.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Subbe CP, Duller B, Bellomo R. Effect of an automated notification system for deteriorating ward patients on clinical outcomes. Crit Care. 2017;21:52. doi: 10.1186/s13054-017-1635-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen L, Dubrawski A, Wang D, et al. Using supervised machine learning to classify real alerts and artifact in online multisignal vital sign monitoring data. Crit Care Med. 2016;44:e456–463. doi: 10.1097/CCM.0000000000001660. [DOI] [PMC free article] [PubMed] [Google Scholar]


