Abstract
Vitreous biopsy is essential for establishing a definitive diagnosis and guiding potential therapy in patients with refractory vitritis and posterior uveitis, among other indications. Especially in cases where one must rule out intraocular lymphoma, obtaining a significant amount of undiluted vitreous increases diagnostic yield. We demonstrate our technique for obtaining a significant amount of undiluted vitreous using pars plana vitrectomy with air infusion.
Keywords: Vitrectomy, Pars plana vitrectomy, Uveitis, Posterior uveitis, Vitreous biopsy, Biopsy
1. Introduction
Numerous techniques exist for sampling the vitreous in patients with refractory vitritis and posterior uveitis. Obtaining undiluted vitreous increases diagnostic yield, which is critical when one attempts to rule out intraocular lymphoma using cytopathologic and flow cytometric analyses. To obtain a “dry” vitreous specimen, one is limited in the amount of undiluted vitreous that can be aspirated before the globe experiences significant hypotony. Vitreous biopsy using pars plana vitrectomy (PPV) with air infusion to maintain intraocular pressure (IOP) has been previously described.1,2 In this article, we describe our technique using 25-gauge (25G) PPV with air infusion to obtain a dry vitreous specimen. This method of utilizing a small-gauge vitrectomy system has not been previously well described. Its advantages include ensuring an adequate amount of undiluted vitreous while minimizing the risks of post-operative hypotony.
2. Case report
A 63-year-old male was initially referred for evaluation of posterior uveitis in both eyes (OU). His past ocular history was unremarkable until one year prior when he was diagnosed with a branch retinal artery occlusion likely due to retinal vasculitis in the right eye (OD) as well as posterior uveitis OU. His best corrected visual acuity (BCVA) was 20/20 OU, and the anterior segment exam was unremarkable. Fundus examination revealed moderate vitreous cell OU with mild vascular sheathing along the inferior arcade vessels in the OD. Fluorescein angiography confirmed mild perivascular leakage along the inferior arcade vessels OD, while the left eye exhibited a normal appearance. Extensive laboratory testing revealed only a mildly elevated antinuclear antibody titer of 1:80. Magnetic resonance imaging of brain and orbits with contrast were unremarkable. Given the persistence and duration of the vitritis, there was concern for possible masquerade syndrome involving intraocular lymphoma. The patient elected to undergo a vitreous biopsy of the OD.
We utilize the 25G PPV Constellation System (Alcon, Fort Worth, TX) for this procedure; however, a 27-gauge approach is an appropriate alternative. Prior to the beginning of the case, the cassette and infusion line were primed with balanced salt solution (BSS); however, the vitrectomy probe was not primed. Once completed, we clamp-closed the infusion line and detached the infusion tubing distal to the auto-infusion valve. The line was flushed with 10 ml of sterile air to eliminate any BSS within the line and then was reattached to the auto-infusion valve. The vitrectomy probe was attached to the console; however, the suction line was disconnected from the probe and attached to a 10 ml syringe for manual aspiration.
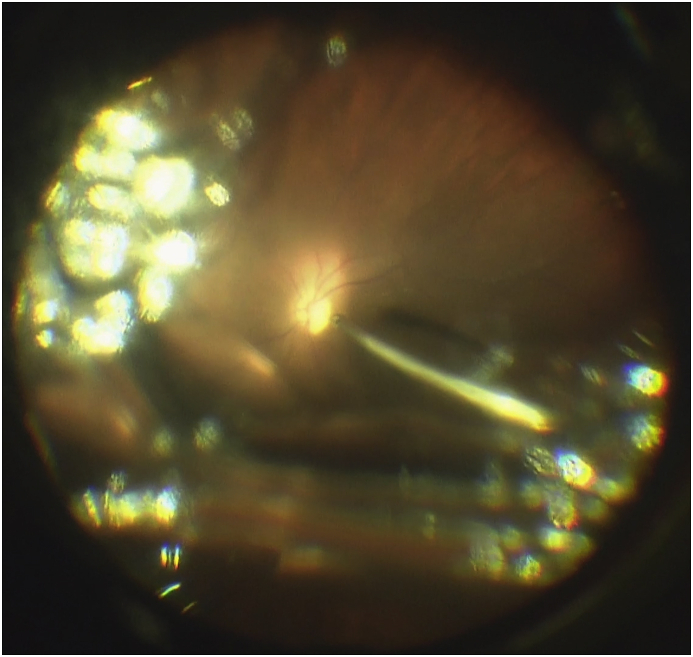
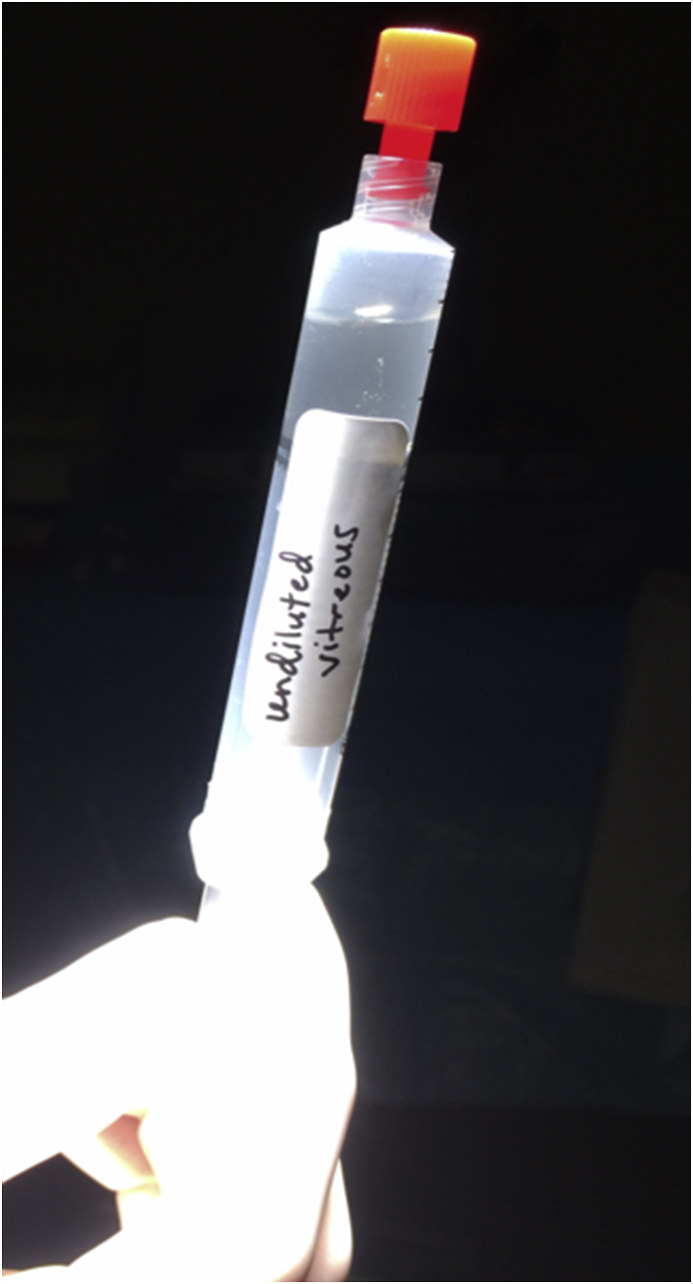
After the eye was prepped and draped, standard three-port 25G pars plana sclerotomy ports were made using valved trocars and cannula system (MIVS, Alcon, Fort Worth, TX), taking care to displace the overlying conjunctiva. The infusion cannula was inserted into the inferior-temporal port, and intravitreal placement was confirmed prior to initiating sterile air infusion at an intraocular pressure (IOP) of 35 mmHg. Using the RESIGHT noncontact viewing system (Carl Zeiss Meditech, Jena, Germany) for direct visualization, the endo-illumination and vitrectomy probe were inserted into the eye (Fig. 1). Taking care to keep the instruments in the mid-vitreous cavity, cutting was initiated at a low rate (3000 cuts per minute) to maintain appropriate IOP while manually collecting vitreous sample. The cutter tip was placed just beneath the air-vitreous interface and progressively lowered towards posterior pole as the air bubble expanded. The air infusion maintained IOP, allowing for an extended vitreous biopsy. When approximately 3–4 ml of vitreous sample was obtained, the instruments were removed from the eye, the syringe was detached (Fig. 2), the suction line was reattached to the vitrectomy probe, and the infusion was switched over to BSS at an IOP of 25 mmHg. Care must be taken to stop the procedure either when the adequate amount of vitreous is obtained or the vitrector tip has reached at a safe distance from surface of retina. We often noticed that air infusion into gel vitreous leads to formation of multiple bubbles and obscures view of the fundus and makes further procedure difficult. In such situation, it is advisable to gently swipe the vitrector from side to side in mid vitreous cavity in order to coalesce multiple air bubbles into one, thereby enhancing visualization.
Fig. 1.
Intraoperative image of vitreous biopsy using pars plana vitrectomy with air infusion to maintain intraocular pressure.
Fig. 2.
Pure, undiluted vitreous was collected directly into the syringe that can be sent directly to the laboratory for further analysis.
The vitreous specimen was passed off the surgical field for processing, and the cut rate for the vitrectomy probe was increased to 10,000 cpm. Instruments were then reinserted into the eye, and a standard core vitrectomy was then performed. At this stage, induction of posterior vitreous detachment (PVD) in ‘cutter-off’ mode can be accomplished via application of active vacuum at the margin of optic disc. Although this additional step depends on the choice of the surgeon, it has the potential to enhance the diagnostic yield in posterior uveitis especially with fewer vitreous cells. Once complete, a 360-degree scleral depressed exam was performed to rule out any peripheral retinal pathology. The trocars were removed, and the sclerotomy wounds were found to be self-sealed with an appropriate IOP.
Postoperatively, the patient maintained a BCVA of 20/20 in the OD. Vitreous biopsy sample revealed inflammatory cells, but a malignancy was not detected. The patient was eventually initiated on immunomodulatory therapy for long-term management of uveitis.
Patient consent
Informed consent was obtained from the patient for this study.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship
Declaration of competing interest
The following authors have no financial disclosures: PHT, SK, QDN.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2020.100768.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Gariano R.F. Vitreous biopsy with air infusion: safety and effectiveness. Retina. 2000;20:422–423. doi: 10.1097/00006982-200004000-00031. [DOI] [PubMed] [Google Scholar]
- 2.Mansour A.M., Hrisomalos N.F. Dry vitreous biopsy with gas-vitreous exchange. Arch Ophthalmol. 1987;105:1478. doi: 10.1001/archopht.1987.01060110024009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.