Abstract
Bedsharing is associated with both increased breastfeeding and increased risk of sudden and unexpected infant deaths. The objective was to determine impact of sleep location and counseling about sleep location on breastfeeding exclusivity and duration in African-Americans. 1194 mothers of newborns were randomized to receive messaging emphasizing either safe sleep practices to reduce SIDS risk or safe sleep practices to prevent SIDS/suffocation. Mothers completed four interviews in the 6 months after delivery. The most common sleep arrangement was roomsharing without bedsharing (“roomsharing”). Duration of any breastfeeding was 6.1 and 5.3 weeks for infants who usually bedshared or roomshared, respectively (p = 0.01). Duration of exclusive breastfeeding was 3.0 and 1.6 weeks for infants who usually bedshared or roomshared, respectively (p < 0.001). Group assignment did not affect breastfeeding duration. The most common sleep arrangement for African-American infants <6 months was roomsharing. An intervention designed to discourage bedsharing did not impact breastfeeding duration.
Keywords: Bedsharing, Breastfeeding, Sleep location
Introduction
Breastfeeding confers numerous benefits upon the infant and the mother [1]. Breast milk contains maternal antibodies and micronutrients [2, 3], which protect infants from infectious diseases [4]. There is recent evidence that exclusive breastfeeding results in intestinal microbiome that supports immune function [5]. Breastfeeding is also associated with decreased infant mortality and specifically, decreased rates of sudden infant death syndrome (SIDS) [6–8]. The American Academy of Pediatrics (AAP) recommends that infants be exclusively breastfed for approximately 6 months, with continued breastfeeding until 1 year or as long as both the mother and infant desire [1].
Because electrophysiologic and behavioral studies have found that maternal-infant bedsharing may facilitate breastfeeding [9–12], bedsharing has been encouraged by many as a strategy to increase breastfeeding exclusivity and duration [10, 13]. Surveys show that 27–60% of infants aged birth to 12 months routinely or occasionally bedshare, [14–16] with rates higher in some racial/ethnic groups, including African-Americans, Hispanics, and American Indian/Alaska Natives [14, 17, 18]. Reasons for bedsharing cited by parents include convenience for feeding (breast or formula), comforting a fussy or sick infant, helping the infant and/or mother sleep better, bonding and attachment, and because of culture or tradition [15, 19].
However, bedsharing is associated with increased risk of sudden and unexpected infant deaths, including SIDS, accidental suffocation and strangulation in bed, and ill-defined deaths [20–23]. The AAP recommends roomsharing without bedsharing, i.e., having baby in crib, bassinet, or playpen close to the parent, but on a separate sleep surface, as the sleep arrangement that is most protective against SIDS and accidental infant deaths [20–23]. However, there are concerns that roomsharing without bedsharing will result in decreased breastfeeding duration and exclusivity.
Few studies have compared breastfeeding duration with different sleep arrangements [12] or when parents receive health messages about the dangers of bedsharing, [24] and no studies have specifically compared breastfeeding duration when infants are bedsharing or roomsharing without bedsharing. Because African-American infants have lower rates of breastfeeding [25–28] and higher rates of bedsharing [14, 17, 18] than the general U.S. population, and because bedsharing has been encouraged as a strategy for increasing breastfeeding rates, [10, 13] we analyzed data on sleep location and feeding type in an African-American population to determine the impact of sleep location and counseling about sleep location on breastfeeding duration.
Methods
We conducted a randomized controlled trial of African-American mothers with newborn infants. We recruited English-speaking, self-identified African-American women who had just delivered an infant. Mothers were excluded if the infant was preterm (<36 weeks) at birth, was hospitalized for >1 week, or had ongoing medical problems requiring subspecialty care. After written informed consent was obtained, a brief survey asked about current intent with regards to feeding type and sleep location, and demographics, including mother’s age and education, marital status, and infant gender. We also asked about presence of other adults, including the other parent and any senior caregivers (such as a grandmother), in the home, as these variables can impact on parental behaviors with regards to sleep and feeding [29–33]. Mothers were randomized to two groups. The control group received standard messaging emphasizing AAP-recommended safe sleep practices (including roomsharing without bedsharing) for the purposes of SIDS risk reduction. The intervention group received enhanced messaging emphasizing the need to follow AAP-recommended safe sleep practices (including roomsharing without bedsharing) for both SIDS risk reduction and suffocation prevention. Research staff who were blinded to study group assignment then contacted participants for three follow-up telephone interviews about current infant care practices: (1) within 2 weeks of the infant’s birth, (2) when the infant was 2–3 months old, and (3) when the infant was 5–6 months old. All survey questions have been validated by parent groups and used in previous studies [34, 35]. The institutional review boards of MedStar Washington Hospital Center and Children’s National Medical Center approved this study.
The primary outcome variables were feeding type (breastmilk, formula, or both) and infant sleep location. We asked about usual sleep location (during the past week) and sleep location for the night prior to each interview. Asking about both usual and last night practices is typically used in SIDS research, as this encourages frank disclosure of actual sleep practices when the practice is not consistent with safe sleep recommendations [36, 37]. Responses about usual and last night practices were analyzed separately. Baseline characteristics between groups were expressed as means and frequencies to evaluate expected similarities and any differences that would need to be taken into account in multiple variable analyses. Analyses of covariance were conducted to estimate the change in practice in the two groups, controlling for baseline levels. Longitudinal logistic regression models were conducted to assess the post-intervention time-averaged groupwise differences measured across three time points. This model allowed for full use of the repeated assessments to enhance study power and to adjust variance estimates to account for correlation among measurements on the same person.
Results
A total of 3506 interviews were conducted with 1194 mothers. All mothers completed the first interview when the infant was 1–2 days old, 958 (80.2%) completed two interviews (the second one when the infant was a mean age of 12.7 days), 717 (60.1%) completed three interviews (the third one when the infant was a mean age of 82.7 days), and 637 (53.4%) completed four interviews (the last one when the infant was a mean of 183.6 days [6.1 months]) (Fig. 1). For the 1194 mothers, mean age was 26.4 years. Seventy-nine percent of mothers were unmarried, 87.5% had a high school diploma or equivalent, and more than half received WIC and Medicaid benefits. The infant’s father and grandmother lived in 49.2 and 29.1% of the homes, respectively (Table 1). Of the 3506 interviews, 3499 contained complete information about feeding type and sleep location and were included in the analysis. Over the course of 6 months, 985 (28.2%) of interviews were conducted with exclusively breastfeeding mothers, 879 (25.1%) with partially breastfeeding mothers, and 1635 (46.7%) with exclusively formula feeding mothers.
Fig. 1.
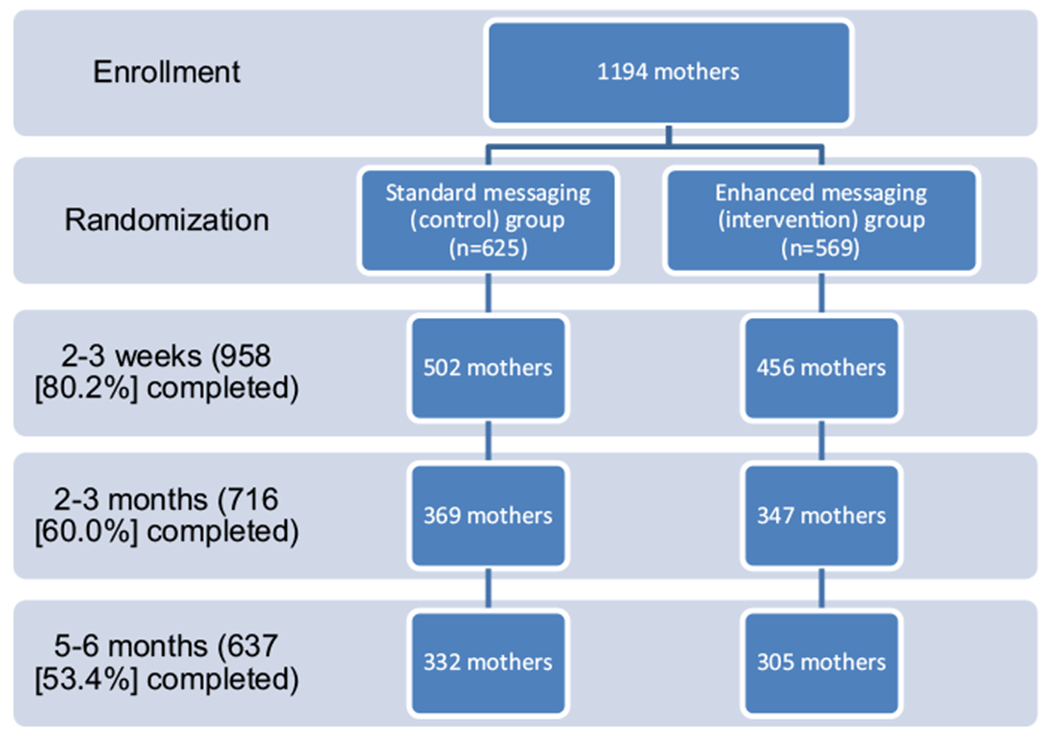
Flow diagram for recruitment, randomization, and study follow-up
Table 1.
Demographic characteristics of respondents (n = 1194)
| Characteristic | N (%) |
|---|---|
| Maternal age (mean 26.4 years; range 18–42) | |
| 18–24 years | 521 (43.6) |
| 25–29 years | 305 (25.5) |
| 30–34 years | 211 (17.7) |
| ≥35 years | 125 (10.5) |
| Did not respond | 32 (2.7) |
| Maternal marital status | |
| Married | 240 (20.1) |
| Never married | 945 (79.1) |
| Divorced/separated | 8 (0.7) |
| Widowed | 1 (0.1) |
| Maternal Education | |
| Did not graduate from high school | 149 (12.5) |
| High school graduate/GED | 815 (68.2) |
| Technical or vocational school graduate | 31 (2.6) |
| 4 year college graduate | 199 (16.7) |
| Infant gender | |
| Female | 588 (49.2) |
| Male | 606 (50.8) |
| Receive WIC benefits | |
| No | 507 (42.4) |
| Yes | 686 (57.5) |
| Did not respond | 1 (0.1) |
| Medical Insurance status | |
| Medicaid or none | 746 (62.5) |
| Private insurance | 448 (37.5) |
| Other people at home (because of multiple responses, total does not equal 100%) | |
| Infant’s mother | 1120 (93.8) |
| Infant’s father | 588 (49.2) |
| Infant’s grandmother | 347 (29.1) |
| Infant’s s grandfather | 117 (9.8) |
| Infant’s sibling | 452 (37.9) |
| Infant’s aunt | 647 (54.2) |
| Infant’s uncle | 152 (12.7) |
| Other (relative or non-relative) | 138 (11.6) |
| Number of people in the household (including infant) | |
| 2 | 40 (3.4) |
| 3 | 265 (22.2) |
| 4 | 339 (28.4) |
| 5 | 265 (22.2) |
| 6 | 142 (11.8) |
| 7 | 83 (7.0) |
| 8 or more | 58 (4.8) |
| Did not respond | 2 (0.1) |
Both exclusive and partial breastfeeding rates decreased with infant age. At 1–2 days of the infant’s life, slightly more than one-third (37.5%) were exclusively breastfeeding, almost one-third (31.2%) were partially breastfeeding, and an additional 31% were exclusively formula feeding. At that time, breastfeeding mothers planned to breastfeed for a mean 24.8 weeks, and exclusively breastfeeding mothers planned to do so for a mean 31.3 weeks. At 2–3 weeks, the proportion of exclusive breastfeeding had declined to 30.5%. The largest decline in exclusive and partial breastfeeding occurred between 2 and 3 weeks and 2–3 months, with proportions of exclusive and partial breastfeeding decreasing to 21.1 and 18.4%, respectively. At 5–6 months, 12.2% of mothers were exclusively breastfeeding and 14.8% partially breastfeeding.
The most commonly reported usual sleep arrangement at all three time points, regardless of feeding type or group assignment, was roomsharing without bedsharing. Almost 80% of 2–3 week olds, 65% of 2–3 month olds, and 55% of 5–6 month olds usually roomshared without bedsharing (Table 2). Similarly, when sleep location last night was reported, roomsharing without bedsharing was the most commonly reported for all groups, with one exception. At 5–6 months, there were similar percentages of exclusively breastfed infants who were bedsharing (4.2%) and roomsharing without bedsharing (3.6%) (Table 3).
Table 2.
Usual sleep location and feeding type at three time points
| Exclusive breastfeeding | Partial breastfeeding | Exclusive formula feeding | Total | |
|---|---|---|---|---|
| 2–3 weeks of age (n = 958) | ||||
| Bedsharing | 61 (6.4%) | 37 (3.9%) | 62 (6.5%) | 160 (16.7%) |
| Roomsharing without bedsharing | 221 (23.1%) | 242 (25.3%) | 300 (31.3%) | 763 (79.6%) |
| Other room | 11 (1.1%) | 5 (0.4%) | 4 (0.4%) | 19 (2.0%) |
| 2–3 months of age (n = 716) | ||||
| Bedsharing | 56 (7.8%) | 35 (4.9%) | 121 (16.9%) | 212 (29.6%) |
| Roomsharing without bedsharing | 81 (11.3%) | 90 (12.6%) | 294 (41.1%) | 465 (64.9%) |
| Other room | 13 (1.8%) | 7 (1.0%) | 19 (2.7%) | 39 (5.4) |
| 5–6 months of age (n = 637) | ||||
| Bedsharing | 88 (13.8%) | 56 (8.8%) | 35 (5.2%) | 179 (28.1%) |
| Roomsharing without bedsharing | 178 (27.9%) | 81 (12.7%) | 90 (14.1%) | 349 (54.8%) |
| Other room | 20 (3.1%) | 13 (2.0%) | 7 (1.1%) | 40 (6.3%) |
Table 3.
Sleep location last night and feeding type at three time points
| Exclusive breastfeeding | Partial breastfeeding | Exclusive formula feeding | Total | |
|---|---|---|---|---|
| 2–3 weeks of age (n = 958) | ||||
| Bedsharing | 33 (3.4%) | 36 (3.8%) | 36 (3.8%) | 105 (11.0%) |
| Roomsharing without bedsharing | 246 (25.7%) | 249 (26.0%) | 321 (33.5%) | 816 (85.2%) |
| Other room | 14 (1.5%) | 11 (1.1%) | 9 (0.9%) | 34 (3.5%) |
| 2–3 months of age (n = 716) | ||||
| Bedsharing | 40 (5.6%) | 14 (2.0%) | 60 (8.4%) | 114 (15.9%) |
| Roomsharing without bedsharing | 97 (13.5%) | 110 (15.4%) | 356 (49.7%) | 563 (78.6%) |
| Other room | 13 (1.8%) | 12 (1.7%) | 18 (2.5%) | 43 (6.0%) |
| 5–6 months of age (n = 637) | ||||
| Bedsharing | 27 (4.2%) | 13 (2.0%) | 64 (10.0%) | 104 (16.3%) |
| Roomsharing without bedsharing | 23 (3.6%) | 55 (8.6%) | 346 (54.3%) | 454 (71.3%) |
| Other room | 14 (2.2%) | 10 (1.6%) | 43 (6.8%) | 67 (10.5%) |
Longitudinal logistic regression controlled for infant age, maternal age, maternal education, medical insurance and number of people in home (Table 4). Infants who received any breastfeeding (exclusive or partial) had odds that were, respectively 1.44 times (95% CI 1.01, 2.06 p = 0.045) and 1.32 (1.32 (95% CI 0.98. 1.78, p = 0.067) greater of bedsharing last night and usually than exclusively formula fed infants. Exclusively breastfed infants were 1.04 times (95% CI 1.02, 1.06) and 1.05 times (95% 1.03, 1.07) more likely to usually bedshare and to have bedshared last night, respectively, and both of these differences were significantly significant (p < 0.001). However, there was no difference in exclusive or partial breastfeeding in infants whose mothers received enhanced health messaging to avoid bedsharing (Tables 5, 6).
Table 4.
Logistic regression analysis of breastfeeding versus exclusive formula feeding
| aOR (95% CI) | p value | |
|---|---|---|
| Any breastfeeding | ||
| Usual bed sharing | 1.32 (0.98–1.78) | 0.067 |
| Bed sharing last night | 1.44 (1.01–2.06) | 0.045 |
| Exclusive breastfeeding | ||
| Usual bed sharing | 1.04 (1.02–1.06) | <0.001 |
| Bed sharing last night | 1.05 (1.03–1.07) | <0.001 |
Ordered logistic regression controlled for infant age, maternal age, maternal education, medical insurance and number of people in home
Table 5.
Longitudinal logistic regression of usual sleep location and feeding type, by group assignment
| Standard |
Enhanced |
Unadjusted | Adjusted |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Exclusive breastfeeding | Partial breastfeeding | Exclusive formula feeding | Exclusive breastfeeding | Partial breastfeeding | Exclusive formula feeding | p value | aOR (95% CI) | p value | |
| 2–3 weeks of life (N = 502 Standard, 456 Enhanced) | |||||||||
| Bedsharing | 35 (23.2%) | 22 (15.0%) | 35 (17.3%) | 26 (18.3%) | 15 (16.7%) | 27 (16.5%) | 0.42 | 1.22 (0.87, 1.70) | 0.25 |
| Roomsharing without bedsharing | 114 (75.5%) | 122 (83.6%) | 164 (81.2%) | 107 (75.4%) | 120 (80.0%) | 136 (82.9%) | |||
| Other room | 2 (1.3%) | 2 (1.4%) | 3 (1.5%) | 9 (6.3%) | 3 (3.3%) | 1 (0.6%) | |||
| 2–3 months of life (N = 369 Standard, 347 Enhanced) | |||||||||
| Bedsharing | 32 (37.6) | 20 (29.8%) | 62 (28.6%) | 24 (36.9%) | 15 (23.1%) | 59 (27.2%) | 0.68 | 0.93 (0.68, 1.28) | 0.67 |
| Roomsharing without bedsharing | 48 (56.5%) | 44 (65.7%) | 142 (65.4%) | 33 (50.8%) | 46 (70.8%) | 152 (70.0%) | |||
| Other room | 5 (5.9%) | 3 (4.5%) | 13 (6.0%) | 8 (12.3) | 4 (6.2%) | 6 (2.8%) | |||
| 5–6 months of life (N = 332 Standard, 305 Enhanced) | |||||||||
| Bedsharing | 26 (45.6%) | 32 (37.6) | 20 (29.8%) | 62 (28.6%) | 24 (36.9%) | 15 (23.1%) | 0.15 | 0.98 (0.71, 1.36) | 0.91 |
| Roomsharing without bedsharing | 36 (42.1%) | 48 (56.5%) | 44 (65.7%) | 142 (65.4%) | 33 (50.8%) | 46 (70.8%) | |||
| Other room | 7 (12.3%) | 5 (5.9%) | 3 (4.5%) | 13 (6.0%) | 8 (12.3) | 4 (6.2%) | |||
Adjusted for maternal age, maternal education, medical insurance, and number of people in home
Parents could select multiple options, so the numbers do not equal 100%. Denominator is the total number enrolled in each group at each time point
Table 6.
Longitudinal logistic regression of sleep location last night and feeding type, by group assignment
| Standard |
Enhanced |
Unadjusted | Adjusted |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Exclusive breastfeeding | Partial breastfeeding | Exclusive formula feeding | Exclusive breastfeeding | Partial breastfeeding | Exclusive formula feeding | p-value | aOR | p-value | |
| 2–3 weeks of life (N = 502 Standard, 456 Enhanced) | |||||||||
| Bedsharing | 17 (11.3%) | 19 (13.0%) | 23 (11.4%) | 16 (11.3%) | 17 (11.3%) | 13 (7.9%) | 0.40 | 1.35 (0.93, 1.97) | 0.12 |
| Roomsharing without bedsharing | 130 (86.1%) | 123 (84.5%) | 174 (86.1%) | 116 (81.7%) | 126 (84.0%) | 147 (89.6%) | |||
| Other room | 4 (2.6%) | 4 (2.7%) | 5 (2.5%) | 10 (7.0%) | 7 (4.7%) | 4 (2.4%) | |||
| 2–3 months of life (N = 369 Standard, 347 Enhanced) | |||||||||
| Bedsharing | 21 (24.7%) | 9 (11.9%) | 27 (12.4%) | 19 (29.2%) | 5 (7.7%) | 33 (15.2%) | 0.87 | 0.78 (0.54, 1.14) | 0.20 |
| Roomsharing without bedsharing | 59 (69.4%) | 55 (82.1%) | 179 (82.5%) | 38 (58.5%) | 55 (84.6%) | 177 (51.6%) | |||
| Other room | 5 (5.9%) | 7 (6.0%) | 11 (5.1%) | 8 (12.3%) | 5 (7.7%) | 7 (3.2%) | |||
| 5–6 months of life (N = 332 Standard, 305 Enhanced) | |||||||||
| Bedsharing | 18 (31.6%) | 6 (16.2%) | 35 (14.7%) | 9 (24.3%) | 7 (17.1%) | 29 (12.8%) | 0.11 | 0.84 (0.60, 1.20) | 0.35 |
| Roomsharing without bedsharing | 30 (52.6%) | 29 (78.4%) | 166 (69.8%) | 23 (62.2%) | 26 (63.4%) | 180 (79.3%) | |||
| Other room | 9 (15.8%) | 2 (5.4%) | 37 (15.6%) | 5 (13.5%) | 8 (19.5%) | 6 (13.5%) | |||
Adjusted for maternal age, maternal education, medical insurance, and number of people in home
Parents could select multiple options, so the numbers do not equal 100%. Denominator is the total number enrolled in each group at each time point
We also calculated duration of breastfeeding, using linear regression analysis, for infants who bedshared usually and last night and for infants who roomshared without bedsharing usually and last night (Table 7). Duration of any breastfeeding for infants who bedshared usually or last night was approximately 1 week longer compared with infants who roomshared without bedsharing. Infants who usually bedshared with their mother continued to receive any breastfeeding for a mean of 6.1 weeks (95% CI 5.5, 6.6), and infants who roomshared without bedsharing received any breastfeeding for a mean of 5.1 weeks (95% CI, 4.8, 5.4) (p = 0.001). Infants who bedshared last night breastfed for a mean of 6.1 weeks (95% CI, 5.4, 6.8), compared with infants who roomshared without bedsharing last night (5.3 weeks, 95% CI, 5.0, 5.5) (p = 0.03). Similarly, duration of exclusive breastfeeding for infants who usually bedshared or bedshared last night was 1-1/2–2 weeks longer compared with infants who roomshared without bedsharing. Infants who usually bedshared with their mother exclusively breastfed for a mean of 3.0 weeks (95% CI 2.5, 3.4), and infants roomshared without bedsharing exclusively breastfed for a mean of 1.6 weeks (95% CI, 1.4, 2.5) (p < 0.001). Infants who bedshared last night exclusively breastfed for a mean of 3.6 weeks (95% CI, 3.0, 4.2), compared with infants who roomshared without bedsharing last night (1.7 weeks, 95% CI, 1.4, 1.9) (p < 0.001). Notably, there was no difference in breastfeeding duration in the two messaging groups (Fig. 2).
Table 7.
Duration of breastfeeding with different sleep arrangements, logistic regression analysis
| Duration (95% CI) | p value | ||
|---|---|---|---|
| Any breastfeeding | Usual bed sharing | 6.1 weeks (5.5, 6.6) | 0.001 |
| Usual room sharing without bed sharing | 5.1 weeks (4.8, 5.4) | ||
| Bed sharing last night | 6.1 weeks (5.4, 6.8) | 0.03 | |
| Room sharing without bed sharing last night | 5.3 weeks (5.0, 5.5) | ||
| Exclusive breastfeeding | Usual bed sharing | 3.0 weeks (2.5, 3.4) | <0.001 |
| Usual room sharing without bed sharing | 1.6 weeks (1.4, 2.5) | ||
| Bed sharing last night | 3.6 weeks (3.0, 4.2) | <0.001 | |
| Room sharing without bed sharing last night | 1.7 weeks (1.4, 1.9) |
Ordered logistic regression controlled for infant age, maternal age, maternal education, medical insurance and number of people in home
Fig. 2.
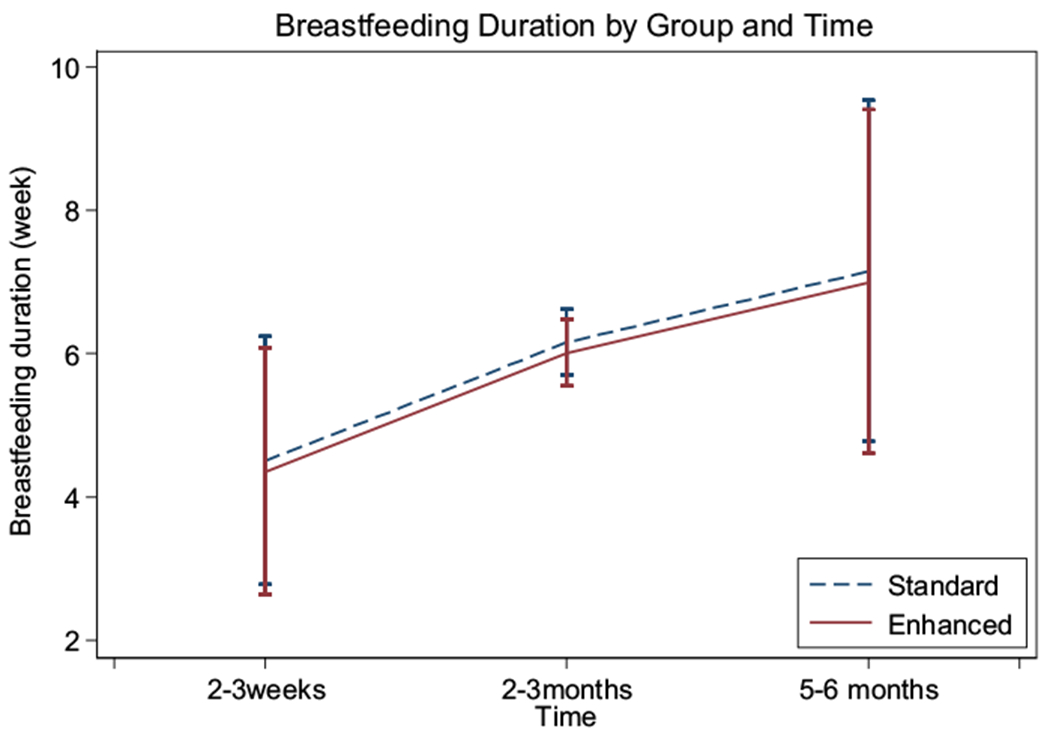
Breastfeeding duration in the standard and enhanced messaging groups
Discussion
To our knowledge, this is the first study to specifically compare breastfeeding duration when infants are bedsharing or roomsharing without bedsharing in any population. In this African-American cohort, the duration of any and exclusive breastfeeding was approximately 1 week and 1–2 weeks longer on average, respectively, for infants who bedshared, compared with those who roomshared without bedsharing. Although this is statistically significant, the clinical significance of this is unclear. The mean duration of breastfeeding in this African-American cohort is much shorter than the 6 months of exclusive breastfeeding that is recommended by the AAP, [1] and only 14.8% of mothers were still exclusively breastfeeding at 5–6 months. Notably, there was no difference in the proportion of breastfeeding infants or on breastfeeding duration when mothers were given health messages to avoid bedsharing.
In our cohort, the proportion of breastfeeding infants decreased rapidly with age, with the largest decline in both exclusive and partial breastfeeding when the infants were between 2 and 3 weeks and 2–3 months of life. This is comparable to national data for breastfeeding. In 2008, 58.9% of African-American infants initiated breastfeeding, and 30.1% were breastfeeding at 6 months, [38] compared to 69% and 29%, respectively, in our cohort.
There has been vociferous debate about bedsharing in recent years, because it is associated with increased duration and exclusivity of breastfeeding [9–12] but is also associated with an increased risk for sudden unexpected infant death [20–23]. However, bedsharing is not essential to breastfeeding success [39]. At all three time points, the majority of exclusively breastfeeding mothers reported roomsharing without bedsharing usually and last night, with the exception of the 5–6 month time point. Although 62% of exclusively breastfed 5–6 month old infants usually roomshared without bedsharing, only 35.9% of these mothers reported roomsharing without bedsharing the prior night, compared with 42% who bedshared the prior night. Indeed, it is interesting that the adjusted odds ratios for bedsharing were lower for exclusively breastfeeding mothers than for those who were doing any breastmilk. In addition, an emphasis on avoidance of bedsharing for these mothers did not impact the proportion of infants breastfed or the duration of breastfeeding. These findings are consistent with those of a recent study of a nationally representative sample that found that most breastfeeding mothers usually roomshared without bedshring, that advice to both room-share without bedsharing and to breastfeed did not result in lower breastfeeding rates [24]. In particular, for African-American mothers, other factors may be more important than sleep location in promoting increased breastfeeding duration and exclusivity. A mixed-method study of 412 African-American parents found that mothers with lower socioeconomic status were 1.9 times and 1.8 times, respectively, more likely to breastfeed exclusively or at all if they bedshared. However, bedsharing was not associated with breastfeeding among higher socioeconomic status African-American mothers. Breast pain, lack of support, and maternal skepticism about breastfeeding benefits were cited by mothers as important barriers to breastfeeding success [40].
We acknowledge that our study sample was limited to a specific geographic area and was less likely to be married and attend college, and more likely to have Medicaid health insurance than the national norms of African-American women [41]. However, bedsharing and breastfeeding practices mirror those seen in other surveys [14, 27], so we believe that these responses are fairly representative of the general African-American population. In addition, African-American mothers are more likely to bedshare [14, 17, 18], and less likely to breastfeed [25–28], and thus it is particularly important to find health messages that will resonate with this subset and improve breastfeeding rates while enhancing sleep safety. Further studies will be needed to confirm these findings and to determine whether findings are consistent in other geographic and racial/ethnic populations.
In conclusion, the most commonly reported sleep arrangement in this African-American cohort was roomsharing without bedsharing. An intervention designed to discourage bedsharing had no impact on breastfeeding duration. While infant sleep location may influence breastfeeding duration and exclusivity, other factors may be equally or more important for improving breastfeeding rates in this population, and efforts to improve breastfeeding duration and exclusivity may need to focus on factors other than infant sleep location.
Acknowledgements
This project was supported by the Maternal and Child Health Bureau, Health Resources Service Administration 1R40MC21511 and the National Institute for Minority Health and Health Disparities P20MD000198.
Funding This project was supported by the Maternal and Child Health Bureau, Health Resources Service Administration 1R40MC21511 and the National Institute for Minority Health and Health Disparities P20MD000198.
Footnotes
Clinical Trials Registration: ClinicalTrials.gov identifier NCT01361880.
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Eidelman AI, Schanler RJ (2012). AAP section on breastfeeding, policy statement: breastfeeding and the use of human milk. Pediatrics, 129(3):e827–e41.22371471 [Google Scholar]
- 2.Heinig MJ (2001). Host defense benefits of breastfeeding for the infant. Effect of breastfeeding duration and exclusivity. Pediatric Clinics of North America, 48(1), 105–123. [DOI] [PubMed] [Google Scholar]
- 3.Kramer MS, Guo T, Platt RW, et al. (2003). Infant growth and health outcomes associated with 3 compared with 6 mo of exclusive breastfeeding. The American Journal of Clinical Nutrition, 78(2), 291–295. [DOI] [PubMed] [Google Scholar]
- 4.Duijts L, Jaddoe VW, Hofman A, & Moll HA (2010). Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics, 126(1), e18–e25. doi: 10.1542/peds.2008-3256. [DOI] [PubMed] [Google Scholar]
- 5.Highet AR, Berry AM, Bettelheim KA, & Goldwater PN (2014). Gut microbiome in sudden infant death syndrome (SIDS) differs from that in healthy comparison babies and offers an explanation for the risk factor of prone position. International Journal of Medical Microbiology, 304(5–6), 735–741. doi: 10.1016/j.ijmm.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Ip S, Chung M, Raman G, Trikalinos TA, & Lau J (2009). A summary of the agency for healthcare research and quality’s evidence report on breastfeeding in developed countries. Breastfeeding Medicine, 4(Suppl 1), S17–S30. doi: 10.1089/bfm.2009.0050. [DOI] [PubMed] [Google Scholar]
- 7.Vennemann MM, Bajanowski T, Brinkmann B, et al. (2009). Does breastfeeding reduce the risk of sudden infant death syndrome? Pediatrics, 123(3), e406–e410. doi: 10.1542/peds.2008-2145. [DOI] [PubMed] [Google Scholar]
- 8.Hauck FR, Thompson J, Tanabe KO, Moon RY, & Vennemann M (2011). Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics, 128(1), 103–110. doi: 10.1542/peds.2010-3000. [DOI] [PubMed] [Google Scholar]
- 9.Mosko S, Richard C, & McKenna J (1997). Infant arousals during mother-infant bed sharing: implications for infant sleep and sudden infant death syndrome research. Pediatrics, 100(5), 841–849. [DOI] [PubMed] [Google Scholar]
- 10.McKenna JJ, Mosko S, & Richard CA (1997). Bedsharing promotes breastfeeding. Pediatrics, 100(2), 214–219. [DOI] [PubMed] [Google Scholar]
- 11.Gettler LT, & McKenna JJ (2011). Evolutionary perspectives on mother-infant sleep proximity and breastfeeding in a laboratory setting. American Journal of Physical Anthropology, 144(3), 454–462. doi: 10.1002/ajpa.21426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang Y, Hauck FR, Signore C, et al. (2013). Influence of bedsharing activity on breastfeeding duration among US mothers. JAMA Pediatrics, 167(11):1038–1044. doi: 10.1001/jamapediatrics.2013.2632. [DOI] [PubMed] [Google Scholar]
- 13.Wiessinger D, West D, Smith LJ, & Pitman T (2014). Sweet sleep: nighttime and naptime strategies for the breastfeeding family. New York, NY: Ballantine Books. [Google Scholar]
- 14.Colson ER, Willinger M, Rybin D, et al. (2013). Trends and factors associated with infant bed sharing, 1993–2010: the National Infant Sleep Position study. JAMA Pediatrics, 167(11):1032–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hauck FR, Signore C, Fein SB, & Raju TN (2008). Infant sleeping arrangements and practices during the first year of life. Pediatrics, 122(Suppl 2), S113–S120. doi: 10.1542/peds.2008-1315o. [DOI] [PubMed] [Google Scholar]
- 16.Kendall-Tackett K, Cong Z, Hale TW (2010). Mother-infant sleep locations and nighttime feeding behavior: U.S. data from the survey of mothers’ sleep and fatigue. Clinical Lactation, 1(Fall):27–31. [Google Scholar]
- 17.Fu LY, Moon R, Hauck FR (2010). Bed sharing among black infants and sudden infant death syndrome: interactions with other known risk factors. Academic Pediatrics, 10(6):376–382. [DOI] [PubMed] [Google Scholar]
- 18.Lahr MB, Rosenberg KD, & Lapidus JA (2007). Maternal-infant bedsharing: risk factors for bedsharing in a population-based survey of new mothers and implications for sids risk reduction. Maternal and Child Health Journal, 11(3), 277–286. [DOI] [PubMed] [Google Scholar]
- 19.Ward TC (2015). Reasons for mother-infant bed-sharing: a systematic narrative synthesis of the literature and implications for future research. Maternal and Child Health Journal, 19(3), 675–690. doi: 10.1007/s10995-014-1557-1. [DOI] [PubMed] [Google Scholar]
- 20.Blair PS, Fleming PJ, Smith IJ, et al. (1999). Babies sleeping with parents: case-control study of factors influencing the risk of the sudden infant death syndrome. CESDI SUDI research group. BMJ, 319(7223), 1457–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carpenter RG, Irgens LM, Blair PS, et al. (2004). Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet, 363, 185–191. [DOI] [PubMed] [Google Scholar]
- 22.Mitchell EA, & Thompson JMD (1995). Co-sleeping increases the risk of SIDS, but sleeping in the parents’ bedroom lowers it In Rognum TO (Ed.), Sudden infant death syndrome: new trends in the nineties (pp. 266–269). Oslo: Scandinavian University Press. [Google Scholar]
- 23.Tappin D, Ecob R, & Brooke H (2005). Bedsharing, roomsharing, and sudden infant death syndrome in Scotland: a case control study. The Journal of Pediatrics, 147(1), 32–37. [DOI] [PubMed] [Google Scholar]
- 24.Smith LA, Geller NL, Kellams AL, et al. (2016). Infant sleep location and breastfeeding practices in the United States: 2011–2014. Academic Pediatrics, doi: 10.1016/j.acap.2016.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Office of disease prevention and health promotion, department of health and human services. Healthy people 2020. maternal, infant, and child health. Accessed March 23, 2012, from http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx.
- 26.Belanoff CM, McManus BM, Carle AC, McCormick MC, & Subramanian SV (2012). Racial/ethnic variation in breastfeeding across the US: A multilevel analysis from the National Survey of Children’s Health, 2007. Maternal and Child Health Journal, 16(Suppl 1), S14–S26. doi: 10.1007/s10995-012-0991-1. [DOI] [PubMed] [Google Scholar]
- 27.Scanlon KS (2010). Racial and ethnic differences in breastfeeding initiation and duration, by state—National Immunization Survey, United States, 2004–2008. MMWR, 59(11), 327–335. [PubMed] [Google Scholar]
- 28.McDowell MM, Wang C-Y, Kennedy-Stephenson J. Breastfeeding in the United States: findings from the National Health and Nutrition Examination Surveys, 1999–2006. Hyattsville, MD: National Center for Health Statistics; 2008. Contract No.: 5. [PubMed] [Google Scholar]
- 29.Brenner R, Simons-Morton BG, Bhaskar B, et al. (1998). Prevalence and predictors of the prone sleep position among inner-city infants. JAMA, 280, 341–346. [DOI] [PubMed] [Google Scholar]
- 30.Brenner RA, Simons-Morton BG, Bhaskar B, Revenis M, Das A, & Clemens JD (2003). Infant-parent bed sharing in an inner-city population. Archives of Pediatrics and Adolescent Medicine, 157(1), 33–39. [DOI] [PubMed] [Google Scholar]
- 31.Battersby S (2010). Understanding the social and cultural influences on breastfeeding today. The Journal of Family Health Care, 20(4), 128–131. [PubMed] [Google Scholar]
- 32.Bentley ME, Caulfield LE, Gross SM, et al. (1999). Sources of influence on intention to breastfeed among African-American women at entry to WIC. Journal of Human Lactation, 15(1), 27–34. [DOI] [PubMed] [Google Scholar]
- 33.Pisacane A, Continisio GI, Aldinucci M, D’Amora S, & Continisio P (2005). A controlled trial of the father’s role in breastfeeding promotion. Pediatrics, 116(4), e494–e498. [DOI] [PubMed] [Google Scholar]
- 34.Moon RY, Oden RP, & Grady KC (2004). Back to sleep: educational intervention with women, infants, and children program clients. Pediatrics, 113(3), 542–547. [DOI] [PubMed] [Google Scholar]
- 35.Moon RY, & Oden RP (2003). Back to sleep: Can we influence child care providers? Pediatrics, 112(4), 878–882. [DOI] [PubMed] [Google Scholar]
- 36.Hauck FR, Herman SM, Donovan M, et al. (2003). Sleep environment and the risk of sudden infant death syndrome in an urban population: The Chicago Infant Mortality Study. Pediatrics, 111(5 Part 2), 1207–1214. [PubMed] [Google Scholar]
- 37.Willinger M, Ko CW, Hoffman HJ, Kessler RC, & Corwin MJ (2003). Trends in infant bed sharing in the United States, 1993–2000: The National Infant Sleep Position study. Archives of Pediatrics and Adolescent Medicine, 157(1), 43–49. [DOI] [PubMed] [Google Scholar]
- 38.Allen JA, Li R, Scanlon KS, et al. (2013). Progress in increasing breastfeeding and reducing racial/ethnic differences—United States, 2000–2008 births. MMWR. Morbidity and Mortality Weekly Report, 62, 77–80. [PMC free article] [PubMed] [Google Scholar]
- 39.Joyner BL, Oden R, Ajao TI, & Moon R (2010). Where should my baby sleep? A qualitative study of African-American infant sleep location decisions. Journal of the National Medical Association, 102(10), 881–889. [DOI] [PubMed] [Google Scholar]
- 40.Kadakia A, Joyner B, Tender J, Oden R, & Moon RY (2015). Breastfeeding in African Americans may not depend on sleep arrangement: a mixed-methods study. Clinical Pediatrics, 54(1), 47–53. doi: 10.1177/0009922814547565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.U.S. Census Bureau. (2012). 2006–2010 American Community Survey. Accessed July 19, 2016, from http://factfinder2.census.gov.


