Abstract
Purpose
To report a case of endogenous Exophiala dermatitidis endophthalmitis.
Observations
An immunosuppressed patient with a history of hairy cell leukemia undergoing chemotherapy presents with rapidly progressing panophthalmitis. The patient was treated medically without improvement and underwent a pars plana vitrectomy which showed multiple retinal abscesses. Vitreous fluid cultures grew a rare fungal organism, Exophiala dermatitidis.
Conclusions and Importance
This is the first reported case of E. dermatitidis causing endogenous endophthalmitis. Rare fungal organisms can present with rapid progression to panophthalmitis in immunocompromised hosts.
Keywords: Endogenous, Endophthalmitis, Exophiala, Wangiella, Dermatitidis
1. Introduction
Endogenous endophthalmitis can occur in immunocompromised patients.1 For this patient population, the source is often fungal and the most common species is Candida.2 Here, we present a unique case of endogenous fungal endophthalmitis caused by the rare organism Exophiala (previously Wangiella) dermatitidis.
2. Case report
A 67-year-old man was transferred to our institution from an inpatient rehab facility with a two-day history of rapidly progressing redness and irritation of the right eye with periorbital edema. His past medical history is significant for hairy cell leukemia and recent acute ischemic left anterior cerebral artery stroke. Of note, he had been receiving chemotherapy from a peripherally inserted central catheter (PICC) for two months. The patient had no known previous ocular history or surgery. On physical exam, the patient had altered mental status and was nonverbal. Ophthalmic exam of the right eye (OD) revealed light perception visual acuity, restricted motility in all directions, significant periorbital erythema, and marked chemosis with necrosis of the inferior conjunctiva due to exposure (Fig. 1). The left eye (OS) was unremarkable. On funduscopic exam there was no red reflex appreciated OD and cotton wool spots were noted in the periphery OS. B-scan ultrasound OD showed dense vitreous debris, choroidal effusions, and thickened sclera with T-sign. MRI of brain was remarkable for acute on subacute infarcts of the bilateral anterior cerebral arteries and proptosis of the right eye with marked edema.
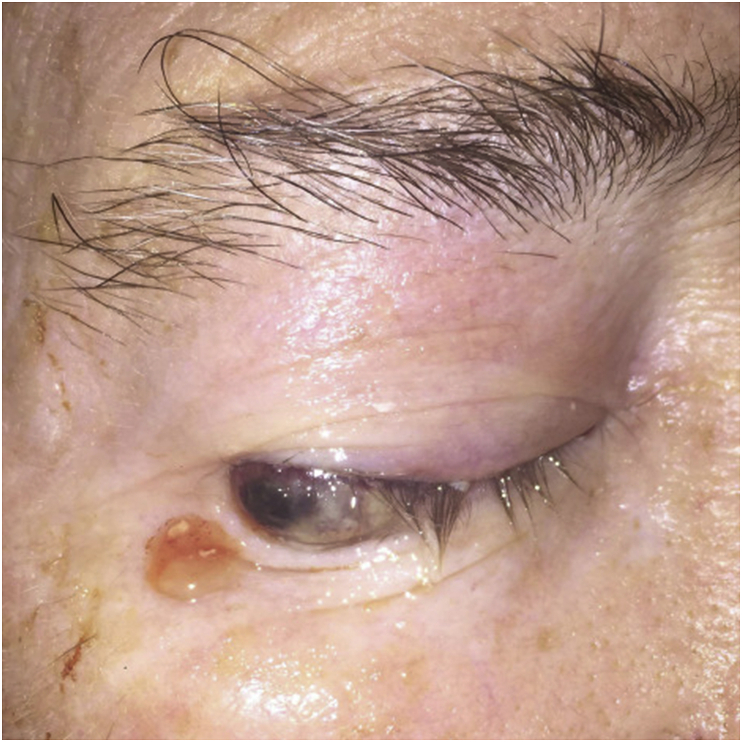
Fig. 1.
Marked necrotic chemosis of the right eye.
Endogenous panophthalmitis was considered the most likely diagnosis given the patient's immunocompromised status secondary to chemotherapy and history of leukemia and long-term indwelling PICC line. A bacterial source was suspected considering the rapid onset of symptoms, but fungal source remained high on the differential.
The patient underwent a vitreous tap with intravitreal injection of vancomycin (1 mg/ 0.1 mL), ceftazidime (2.25 mg/ 0.1 mL), and voriconazole (100 mcg/ 0.1 mL) and was admitted for further work up. Cultures of vitreous fluid and blood showed no growth. A chest X-ray and transthoracic echocardiogram revealed no source of infection. The patient was started empirically on systemic vancomycin and cefepime along with topical prednisolone forte, atropine, and erythromycin ointment.
Given minimal improvement, the patient underwent 3 additional rounds of repeat vitreous tap and injection vancomycin/ceftazidime/voriconazole/amphotericin B as well as systemic voriconazole. After 15 days, cultures of vitreous fluid obtained by vitreous tap grew a rare fungal organism, E. dermatitidis. The patient also had an elevated Fungitell β-D Glucan assay of 207pg/mL making contamination less likely. Further work up with transesophageal echocardiogram revealed no source of infection. Three weeks after initial presentation, the patient showed no improvement in visual acuity of light perception and continued dense vitritis OD. The patient subsequently underwent cataract extraction and pars plana vitrectomy with silicone oil OD. Intraoperatively, the patient had notable retinal abscesses involving the superior hemi-retina. The retina overlying the abscess was found to be thin and necrotic. Inspection of the peripheral retina demonstrated retinal detachment from areas of retinal necrosis due to the infection. The areas of retinal necrosis were focally detached and all vitreous traction was relieved. Given the friable nature of the necrotic retina and the subretinal abscesses in areas of attached retina, the decision was made not to excise the abscesses or perform retinectomy of the superior retina as this would have involved excising the macula. Nondilute vitreous fluid cultures at the time of vitrectomy confirmed the presence of E. dermatitidis.
The patient was followed closely post-operatively and received one additional intravitreal injection of voriconazole/amphotericin B as well as oral voriconazole. The patient received a total of five rounds of intravitreal injections and 37 days of oral voriconazole treatment. His visual acuity gradually improved to hand motion and he was discharged to a nursing facility. Unfortunately, the patient experienced sudden cardiac death seven weeks after initial presentation and expired.
3. Discussion
We present a unique case of Exophiala (previously known as Wangiella) dermatitidis endogenous endophthalmitis in an immunocompromised patient. Given the rapid progression of symptoms, the source was initially thought to be bacterial rather than fungal. Two weeks after initial presentation, vitreous fluid cultures grew a rare fungal organism, E. dermatitidis.
Exophiala species are dimorphic dematiaceous fungi. Our organism of interest, E. dermatitidis, was found to be the most prevalent Exophiala species identified clinically in the United States.3 Infections by Exophiala species are most commonly seen in deep tissues, especially the lungs, or cutaneous tissues. Intraocular infections are rare and comprise only 6.8% of infections caused by Exophiala species.3
To date, there are no previous reports of endogenous endophthalmitis caused by E. dermatitidis in the literature. Most cases of endogenous fungal endophthalmitis are due to Candida infection1,2 and Exophiala is an extremely rare organism to cause endophthalmitis.3,4 Of the four cases reported of E. dermatitidis endophthalmitis, all were exogenous in nature occurring in patients with a history of ocular surgery.4, 5, 6, 7 Two of the cases reported involvement of the cornea6,7 and only one had presence of retinal abscesses as demonstrated in our case.6
Voriconazole is the current treatment of choice in the treatment of E. dermatitidis.8 Of the cases reported of E. dermatitidis endophthalmitis, two cases had improvement with a combination of surgical intervention, voriconazole, and fluconazole treatment4,7 and the other two cases resulted in enucleation.5,6
4. Conclusion
This case illustrates the organism E. dermatitidis as an unusual cause of fungal endogenous endophthalmitis with rapid progression to panophthalmitis. Rare fungal organisms must be considered as a causative agent of endogenous endophthalmitis, particularly in immunocompromised hosts who fail standard therapy.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support was obtained for this study.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures to make: MGV, AH, JW, KH, RS.
Acknowledgements
None.
References
- 1.Kuriyan A., Schwartz S.G., Davis J.L., Flynn H.W. Ryan's Retina. Sixth Edit. Elsevier Inc.; 2018. Endogenous bacterial and fungal endophthalmitis; pp. 1700–1708. [DOI] [Google Scholar]
- 2.Connell P.P., O'Neill E.C., Fabinyi D. Endogenous endophthalmitis: 10-year experience at a tertiary referral centre. Eye. 2011;25(1):66–72. doi: 10.1038/eye.2010.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeng J.S., Sutton D.A., Fothergill A.W., Rinaldi M.G., Harrak M.J., De Hoog G.S. Spectrum of clinically relevant Exophiala species in the United States. J Clin Microbiol. 2007;45(11):3713–3720. doi: 10.1128/JCM.02012-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Homa M., Manikandan P., Saravanan V. Exophiala dermatitidis endophthalmitis: case report and literature review. Mycopathologia. 2018;183(3):603–609. doi: 10.1007/s11046-017-0235-4. [DOI] [PubMed] [Google Scholar]
- 5.Margo C.E., Fitzgerald C.R. Postoperative endophthalmitis caused by Wangiella dermatitidis. Am J Ophthalmol. 1990;110(3):322–323. doi: 10.1016/s0002-9394(14)76363-9. [DOI] [PubMed] [Google Scholar]
- 6.Clamp M.F., Jumper J.M., Ku C.W. Chronic exogenous exophiala. Retin Cases Brief Rep. 2014;8(4):265–268. doi: 10.1097/ICB.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 7.Quintero-Estades J.A., Walter S., Valenzuela F., Amescua G. Delayed-onset postoperative endophthalmitis secondary to Exophiala. BMJ Case Rep. 2015 doi: 10.1136/bcr-2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vasquez A., Zavasky D., Chow N.A. Management of an outbreak of Exophiala dermatitidis bloodstream infections at an outpatient oncology clinic. Clin Infect Dis. 2018;66(6):959–962. doi: 10.1093/cid/cix948. [DOI] [PubMed] [Google Scholar]