Abstract
Objectives
While understanding of complex within-person clustering of health behaviors into meaningful profiles of risk is growing, we still know little about whether and how U.S. adults transition from one profile to another as they age. This study assesses patterns of stability and change in profiles of tobacco and alcohol use and body mass index (BMI).
Method
A nationally representative cohort of U.S. adults 25 years and older was interviewed up to 5 times between 1986 and 2011. Latent transition analysis (LTA) models characterized the most common profiles, patterning of transitions across profiles over follow-up, and assessed whether some were associated with higher mortality risk.
Results
We identified 5 profiles: “health promoting” with normal BMI and moderate alcohol consumption; “overweight”; “current smokers”; “obese”; and “nondrinkers”. Profile membership was largely stable, with the most common transitions to death or weight gain. “Obese” was the most stable profile, while “smokers” were most likely to transition to another profile. Mortality was most frequent in the “obese” and “nondrinker” profiles.
Discussion
Stability was more common than transition, suggesting that adults sort into health behavior profiles relatively early. Women and men were differently distributed across profiles at baseline, but showed broad similarity in transitions.
Keywords: Alcohol, BMI, Latent transition analysis, Tobacco
As the U.S. population ages and the burden of chronic disease rises, it is critical to understand how the patterning of modifiable health behaviors undergirds these changes. Past studies have shown that population levels of some health-compromising behaviors decline as a cohort ages past midlife and changes its behavior. This is the pattern for smoking cessation (Holford et al., 2014) and reductions in alcohol use, though recent birth cohorts have shown slower rates of decline in alcohol use as they age (Kerr, Greenfield, Bond, Ye, & Rehm, 2009; Moore et al., 2005). Body weight has been shown to rise until age 60 or 65, after which it declines (Sheehan, DuBrava, DeChello, & Fang, 2003), though recent cohorts may be showing increases into later ages (Walsemann & Ailshire, 2011). Although understanding the life course changes in each of these health behaviors is valuable, individuals may engage in multiple health-compromising health behaviors, and change them separately or concurrently at different points over the life course, such that their overall health risk may not be evident when considering a single behavior or behavioral change (Coups, Gaba, & Orleans, 2004; Fine, Philogene, Gramling, Coups, & Sinha, 2004; Spring, Moller, & Coons, 2012).
Other studies have shown that health behaviors cluster at a given point in time, and that risk profiles are distributed in socially patterned ways (Berrigan, Dodd, Troiano, Krebs-Smith, & Barbash, 2003; de Vries, Kremers, Smeets, & Reubsaet, 2008; Kvaavik, Batty, Ursin, Huxley, & Gale, 2010; Shaw & Agahi, 2012). Many earlier studies created risk scores by summing across behaviors, but more recent studies have used methods like latent class analysis (LCA) to examine the frequency and predictors of distinctive health behavior profiles, and have revealed considerable complexity (Leventhal, Huh, & Dunton, 2014; Mollborn, James-Hawkins, Lawrence, & Fomby, 2014; Schnuerer et al., 2015). For example, a study of U.S. adults that used LCA found seven health behavior “niches” when considering eight health behaviors ranging from smoking status to flu vaccination. The authors found that while 44% of adults fell into niches characterized by concordant health-promoting behaviors and 26% were in niches characterized by concordant health-compromising behaviors, almost a third showed profiles of discordant health-promoting and -compromising behaviors (Saint Onge & Krueger, 2017). Many of these newer studies are grounded in health lifestyle theory, a perspective that recognizes the social, cultural, and economic forces that shape and constrain individual choices and create complex social patterning across a range of health choices that might not be evident when considering a single behavior in isolation (Cockerham, 2005).
There is increasing recognition of the informative clustering of specific health behaviors into profiles, but most past studies have used cross-sectional data, so we know little about whether individuals maintain a particular health behavioral risk profile as the age, or if they transition across profiles. Just as studies have shown that engaging in one health-compromising behavior does not imply health-endangering choices across the board, behavior change could take many forms, from a “health kick” that involves co-occurring health-promoting changes, to change in a particular behavior while maintaining others, to an increase in risk across a range of behaviors. For example, there is some evidence that smoking initiation is associated with greater alcohol consumption, while quitting smoking may lead to reductions in alcohol consumption (Moore et al., 2005), but increases in body weight (Aubin, Farley, Lycett, Lahmek, & Aveyard, 2012; Pieroni & Salmasi, 2016). However, only a handful of studies have assessed whether and how patterns of stability and change in multiple health behaviors may cluster individuals into distinctive groups as they age.
The relevant evidence to date comes from studies using latent class and trajectory-based approaches to understand linked change across behaviors. For example, a study of Taiwanese adults 60 and older who were followed over 9 years first estimated separate trajectories of smoking, alcohol use, physical activity and having a medical checkup, and then estimated a grouped trajectory model to show profiles of behavioral stability and change (Hsu, Luh, Chang, & Pan, 2013). Most groups showed relatively stable behavioral profiles differentiated by stable or slowly declining smoking, smoking combined with drinking, or low versus high stable levels of regular exercise, but one profile found only for men was distinctive for a sharp reduction in smoking and some decline in alcohol use. Another study used LCA to assess the joint trajectories of smoking, drinking, obesity, and inactivity across four observation points spanning 14 years among U.S. youth transitioning to adulthood (Daw, Margolis, & Wright, 2017). This study yielded seven profiles distinguished by stability in smoking and drinking, or more commonly, increases in binge drinking, smoking, or obesity, and decreases in sedentariness, with varying combinations of these changes making up distinctive profiles.
Drawing on very different periods of the life course and samples exposed to varying health behavioral norms, these studies show that change in behavioral profiles can take many forms, but that change clusters into meaningful patterns. However, past studies have not assessed whether and how U.S. adults transition across health lifestyles. Moreover, past studies that examined change over time have not accounted for variation in survival of individuals with different risk behavior profiles, either because the focus was on earlier life, they had a short duration of follow-up, or because the trajectory models did not identify attrition due to death. This is problematic because some health behavioral profiles are associated with a greater risk for premature mortality than others (Cockerham, Bauldry, Hamby, Shikany, & Bae, 2017; Saint Onge & Krueger, 2017). Ignoring selective mortality could lead researchers to conclude that changes in behavior are generating changes in the population distribution of risk, when in fact there was differential loss from the population of those with particular behavioral profiles.
In this study, we use longitudinal data from a nationally representative sample of U.S. adults recruited in 1986 and re-interviewed up to four more times over 25 years about their tobacco and alcohol use and body mass index (BMI). We apply latent transition analysis (LTA) to characterize the most prevalent health behavior profiles at baseline, as well as how individuals may transition between them as they age over follow-up. An extension of LCA, LTA models use longitudinal data to determine how health behaviors cluster into profiles, estimate transitions across these profiles over time, and assess whether some are associated with a disproportionate risk of mortality. We also stratify our analyses by sex, as past studies have consistently found that men tend to engage in more health-compromising behaviors (Fine et al., 2004; Laska, Pasch, Lust, Story, & Ehlinger, 2009; Schnuerer et al., 2015; Skalamera & Hummer, 2016), and one study of elderly Taiwanese men and women showed that they followed some overlapping but distinctive profiles of behavioral stability and change (Hsu et al., 2013).
Data and Methods
Data
We use data from five waves of the Americans’ Changing Lives (ACL) study to examine stability and change in profiles of health behaviors for periods of up to 25 years across middle and later adulthood. The ACL study began in 1986 with a multistage stratified area probability sample of the continental U.S. household population of adults over the age of 25, with an oversampling of African Americans and people over the age of 60. Baseline face-to-face interviews were conducted with 3,617 men and women. Follow-up interviews were conducted in 1989 (N = 2,867), 1994 (N = 2,559), 2002 (N = 1,787), and 2011 (N = 1,427). Further information about the ACL is available elsewhere (House et al., 1994; Lantz, House, Mero, & Williams, 2005). These analyses use the entire sample of respondents from the baseline wave (N = 3,617). Over follow-up, respondents could miss a wave due to nonresponse (W2: 572, W3: 503, W4: 631, W5: 350), but return in a future wave, or could leave the sample due to death (N = 1,832 by 2012). While the LTA analyses are unweighted, as no software currently accommodates weights, descriptive tables are weighted to make them representative of the noninstitutionalized U.S. population in 1986.
Measures
Health behaviors
Smoking status was assessed at each interview wave with the question “Do you smoke cigarettes now?” and was coded 1 for current smokers and 0 for former or never smokers. Alcohol use was measured at each wave with items assessing the average number of drinks consumed on days that a respondent drinks, and the number of days they consumed alcohol in the past month. We followed as closely as possible the Dietary Guidelines for Americans in 2010 (U.S. Department of Agriculture & U.S. Department of Health and Human Services, 2010), and used gender-specific cutoffs to define heavy drinking. For men, this was more than four drinks on any day or more than two drinks per day over the month, and moderate drinking was drinking two or less drinks per day. For women, the equivalent figures were more than three drinks on any day or more than one drink per day over the month, and moderate drinking was one drink or less per day. Nondrinkers were respondents who indicated they did not drink, or reported zero drinks over the month. BMI was calculated using self-reported information on weight and height. Respondent height was reported at baseline, while weight was reported at each wave. A BMI of below 18.5 was classified as “underweight,” 18.5–24.9 as “normal,” 25–29.9 as “overweight,” and a score of 30 or above was considered “obese.” Few respondents were classified as “underweight” at baseline (N = 89) or over follow-up (N = 206), so BMI information for underweight respondents was treated as missing when assigning them to health behavior profiles.
Mortality
Verification of deaths through 2012 was obtained through the National Death Index (NDI), death certificates, and from informants.
Other covariates
To assess variation in key predictors of health behaviors and behavior change that might be differentially distributed by sex, we used baseline measures of age in years, household income in 1986 dollars, education (less than high school, high school completion, some college, bachelor’s degree or more), race/ethnicity (non-Hispanic black, non-Hispanic white, other race/ethnicity), current employment and marital status, and whether the respondent was ever a parent by 1986. We also included several health-related predictors measured at baseline, including number of existing chronic conditions (sum = 0–7, based on presence of arthritis, lung disease, hypertension, heart attack/heart trouble, diabetes, cancer, foot problems, stroke, broken bones, urine beyond control), degree of functional impairment (1 = not impaired, 4 = severely impaired), whether a respondent had a serious illness in the last 3 years, whether a respondent had ever experienced a life-threatening illness, and self-rated health (1 = low, 5 = high).
Method
To examine the clustering of health behaviors into commonly occurring profiles and assess whether and how individuals transition across them, we conducted a LTA (Lanza & Collins, 2008), using proc LTA in SAS (Lanza, Dziak, Huang, Wagner, & Collins, 2015), and considering all five waves of ACL data. The LTA jointly estimated: (a) a measurement model, relating latent health behavior profiles to observed health behaviors, and (b) transition probabilities between latent health behavior profiles from wave to wave. The measurement model (first component) generated item-propensity scores indicating the probability of observing certain health behaviors within each latent behavior profile. To ensure that the substantive meaning of each latent status does not vary across waves, we restricted the item-response propensities for latent profiles to be the same at each wave. This allows us to most clearly identify similar transitions across individuals. We stratified the LTA by sex to obtain separate estimates for men and women.
To ensure that a global maximum likelihood estimate was obtained using PROC LTA’s expectation–maximization (EM) algorithm, we used five random start-points and chose the result with the largest likelihood. To obtain confidence intervals we conducted a nonparametric bootstrap with 1,000 iterations, with resampling done at the subject level. In each bootstrap sample, we fixed the number of male and female subjects to be the same as in the original data set (1,358 males, 2,259 females), and again used multiple start-points to ensure convergence at a global maximum. We computed percentile bootstrap confidence intervals. Where necessary, the LTA model treated the data as missing at random, dropping it from the likelihood for the wave in which it was missing.
Like most clustering methods, LTA requires the analyst to select the number of latent profiles. We used the Bayesian information criterion (BIC), which penalizes models with large numbers of profiles to avoid overfitting, together with scientific judgment to select the number. Supplementary Appendix A reports the values for different profile solutions. As recommended by Lanza and Collins (2008), we placed more emphasis on interpretability than BIC, and based on our examination of their meaningfulness for health promotion, chose five latent profiles, the model with the second best performance measured by BIC. We also created a sixth, absorbing profile for death by including a mortality indicator in the measurement model and a “dead” category for each of the health behavior measures used in estimation of the latent profiles. Once subjects died, they were coded as dead in all subsequent waves. LTA assumes all profiles are represented in the data at all time points; thus, for computational reasons, since no subjects were dead at baseline, we added one dead subject to the data for each combination of covariates used to predict baseline profile membership (four males and four females total). The LTA generates posterior probabilities of membership that denote the possibility of a respondent being in each latent profile (e.g., a 20% chance being in Profile 1 and a 75% chance of Profile 2). Most respondents had a high posterior probability of membership in only one profile (0.8 or greater), suggesting reasonable model fit. Results from the transition analyses (second component) show patterns of stability in or transition across latent profiles of health behaviors.
Results
Table 1 presents weighted descriptive information on the characteristics of the analytic sample at baseline in 1986, overall and by sex, with results from adjusted t-tests for differences in means between men and women and chi-square tests for categorical variables. Notable sex differences in factors that predict health behaviors motivate our decision to consider men and women separately throughout the analysis.
Table 1.
Descriptive Characteristics of American’s Changing Lives Study Analytic Sample at Baseline in 1986
| Predictor | All sample | Men | Women | Diff |
|---|---|---|---|---|
| Age at baseline | 47.1 | 46.0 | 48.1 | ** |
| SD | (16.4) | (15.9) | (16.8) | |
| Education | ||||
| Less than high school | 25.6% | 24.9% | 26.2% | *** |
| High school | 31.4% | 27.7% | 34.6% | |
| Some college | 23.3% | 23.4% | 23.3% | |
| Bachelor’s degree or more | 19.7% | 24.1% | 15.9% | |
| Race | ||||
| Non-Hispanic white | 83.5% | 84.3% | 82.8% | n.s. |
| Non-Hispanic black | 11.0% | 10.0% | 11.8% | |
| Other | 5.6% | 5.7% | 5.4% | |
| HH income at baseline | $30,449 | $33,127 | $28,065 | *** |
| SD | ($24,043) | ($24,163) | ($23,689) | |
| % Working | 65.6% | 77.3% | 55.2% | *** |
| % Married | 72.9% | 80.1% | 66.5% | *** |
| % Ever parent | 82.9% | 79.7% | 85.7% | *** |
| No. of chronic conditions (1–7) | 1.02 | 0.85 | 1.16 | *** |
| SD | (1.3) | (1.2) | (1.3) | |
| Functional impairment (1 = not impaired, 4 = severely impaired) | 1.27 | 1.21 | 1.32 | *** |
| SD | (0.7) | (0.6) | (0.7) | |
| Self-rated health (1 = low, 5 = high) | 3.70 | 3.76 | 3.64 | * |
| SD | (1.1) | (1.1) | (1.1) | |
| Had serious illness in last 3 years? | 15.4% | 14.1% | 16.6% | |
| Ever have life threatening illness? | 27.0% | 30.8% | 23.6% | *** |
| Smoking | ||||
| Current smoker | 30.4% | 31.9% | 29.1% | *** |
| Never smoker | 42.1% | 32.8% | 50.4% | |
| Former smoker | 27.5% | 35.3% | 20.6% | |
| Alcohol use | ||||
| Nondrinker | 41.2% | 29.6% | 51.5% | *** |
| Moderate drinker | 46.9% | 52.5% | 41.8% | |
| Heavy drinker | 12.0% | 17.9% | 6.7% | |
| BMI | ||||
| Normal | 48.3% | 43.6% | 52.4% | *** |
| Overweight | 34.6% | 41.5% | 28.5% | |
| Obese | 14.8% | 14.0% | 15.6% | |
| Unweighted N | 3,617 | 1,358 | 2,259 | |
Note. Statistics are weighted unless otherwise specified. BMI categories do not sum to 100% because information was treated as missing for underweight respondents (BMI < 18.5, N = 89).
***p < .001. **p < .01. *p < .05.
The sex-stratified LTA model yielded five latent health behavior profiles and one absorbing profile for death over follow-up. Figure 1 panels for female and male respondents show how the profiles are defined by distributions of BMI, drinking, and smoking statuses of incumbents. These figures represent pooled information from across all five waves of follow-up. Our comparisons of the male and female results should be considered exploratory, as the LTA model was sex-stratified and we observe some differences in the characteristics of men and women classified in the same profile.
Figure 1.
Definition of health behavior profiles by distributions of BMI, alcohol use, and smoking statuses of incumbents by sex (Profile 1: “health promoting—normal BMI, moderate drinkers,” Profile 2: “overweight,” Profile 3: “current smokers,” Profile 4: “obese,” Profile 5: “normal or overweight nondrinkers”).
Broadly, the profiles can be interpreted similarly for women (top) and men (bottom). We label them to indicate their primary defining characteristic for ease of discussion, and order them such that Profile 1 has the lowest mortality risk over follow-up and Profile 5 has the highest. Profile 1 (“health promoting”) describes respondents likely to be of normal BMI and to drink moderately. Profile 2 (“overweight”) respondents are likely to be overweight, with men less likely to be nondrinkers and more likely to be moderate drinkers than women in this profile. Profile 3 (“smoker”) captures the current smokers, with men in this profile more likely to be heavy or moderate drinkers than women, but also less likely to be obese. Profile 4 (“obese”) respondents are likely to be obese, with men more likely to be moderate or heavy alcohol drinkers than women in this profile. Profile 5 (“nondrinker”) respondents are either normal or overweight, with men somewhat more likely to be overweight, and are distinct from Profiles 1 and 2 incumbents because they are nondrinkers. The only notable sex difference was that men appeared to report somewhat higher levels of alcohol use than women in the same profile for profiles 2 through 4. Smoking and obesity define specific profiles in this sample (3 and 4, respectively), but alcohol use does not, though only about 7% of women and 18% of men were heavy drinkers at baseline.
Patterns of Stability and Change in Risk Profile Membership
Table 2 shows the distribution of respondents across health behavior profiles overall and by sex, with assignment based on the highest posterior probability estimated by the LTA model for that interview wave. The top panel presents the distribution at Wave 1, when about 29% of respondents was assigned to the “health promoting” Profile 1, 27% were in “smoker” Profile 3, about 13% were in “obese” Profile 4, 18% fell into “overweight” Profile 2, and 13% into “nondrinker” Profile 5. Men were more likely than women to be in the “overweight” profile (21.6% vs 15.2%) and women more likely than men to be in the “health promoting” (31.3% vs 25.9%) and “nondrinker” (15.0% vs 11.5%) profiles.
Table 2.
Membership in Health Behavior Profiles Across Waves
| Profile | All sample | Men | Women |
|---|---|---|---|
| Wave 1 | |||
| Profile 1: Health promoting—normal BMI, moderate drinkers | 28.7% | 25.9% | 31.3% |
| Profile 2: Overweight | 18.2% | 21.6% | 15.2% |
| Profile 3: Current smokers | 27.1% | 28.1% | 26.3% |
| Profile 4: Obese | 12.6% | 12.9% | 12.3% |
| Profile 5: Normal or overweight nondrinkers | 13.3% | 11.5% | 15.0% |
| Profile 6: Deceased | 0.0% | 0.0% | 0.0% |
| Mean age of respondents | 47.1 | 46.0 | 48.1 |
| Unweighted N | 3,617 | 1,358 | 2,259 |
| Wave 2 | |||
| Profile 1: Health promoting—normal BMI, moderate drinkers | 25.7% | 21.6% | 29.1% |
| Profile 2: Overweight | 19.5% | 20.6% | 18.5% |
| Profile 3: Current smokers | 23.1% | 23.4% | 22.8% |
| Profile 4: Obese | 14.4% | 15.4% | 13.6% |
| Profile 5: Normal or overweight nondrinkers | 13.6% | 14.2% | 13.1% |
| Profile 6: Deceased | 3.8% | 4.8% | 3.0% |
| Mean age of respondents | 49.4 | 48.1 | 50.4 |
| Unweighted N | 3,045 | 1,122 | 1,923 |
| Wave 3 | |||
| Profile 1: Health promoting—normal BMI, moderate drinkers | 20.9% | 16.8% | 24.6% |
| Profile 2: Overweight | 20.1% | 21.5% | 18.9% |
| Profile 3: Current smokers | 17.4% | 17.5% | 17.3% |
| Profile 4: Obese | 16.9% | 16.3% | 17.4% |
| Profile 5: Normal or overweight nondrinkers | 13.3% | 14.0% | 12.7% |
| Profile 6: Deceased | 11.4% | 13.9% | 9.2% |
| Mean age of respondents | 53.2 | 51.6 | 54.5 |
| Unweighted N | 3,114 | 1,181 | 1,933 |
| Wave 4 | |||
| Profile 1: Health promoting—normal BMI, moderate drinkers | 16.0% | 11.8% | 19.8% |
| Profile 2: Overweight | 16.2% | 17.0% | 15.4% |
| Profile 3: Current smokers | 11.0% | 10.7% | 11.2% |
| Profile 4: Obese | 18.0% | 17.0% | 18.9% |
| Profile 5: Normal or overweight nondrinkers | 13.0% | 14.3% | 11.2% |
| Profile 6: Deceased | 26.2% | 29.2% | 23.4% |
| Mean age of respondents | 57.5 | 56.0 | 58.7 |
| Unweighted N | 2,986 | 1,132 | 1,854 |
| Wave 5 | |||
| Profile 1: Health promoting—normal BMI, moderate drinkers | 12.9% | 10.2% | 15.2% |
| Profile 2: Overweight | 13.9% | 13.3% | 14.4% |
| Profile 3: Current smokers | 7.1% | 6.3% | 7.9% |
| Profile 4: Obese | 18.3% | 17.5% | 19.0% |
| Profile 5: Normal or overweight nondrinkers | 8.3% | 11.7% | 5.4% |
| Profile 6: Deceased | 39.4% | 40.9% | 38.1% |
| Mean age of respondents | 64.0 | 63.4 | 64.6 |
| Unweighted N | 3,267 | 1,215 | 2,052 |
Note. Proportions weighted by baseline weights, accounting for survey sampling design. N includes respondents at that wave and known decedents.
The next panel of Table 2 shows that between Waves 1 and 2, about 4% of respondents died, and that by Wave 2, slightly fewer men and women were in the “health promoting” or “smoker” profiles. Subsequent panels show a steady loss of respondents from the “health promoting” and “smoker” profiles over each wave of follow-up. By Wave 5, 39% of the sample had died, the percentage in the “obese” profile had grown slightly, and the reduction in the “nondrinker” profile accelerated for men and women after Wave 3, as respondents aged and inter-wave intervals grew longer.
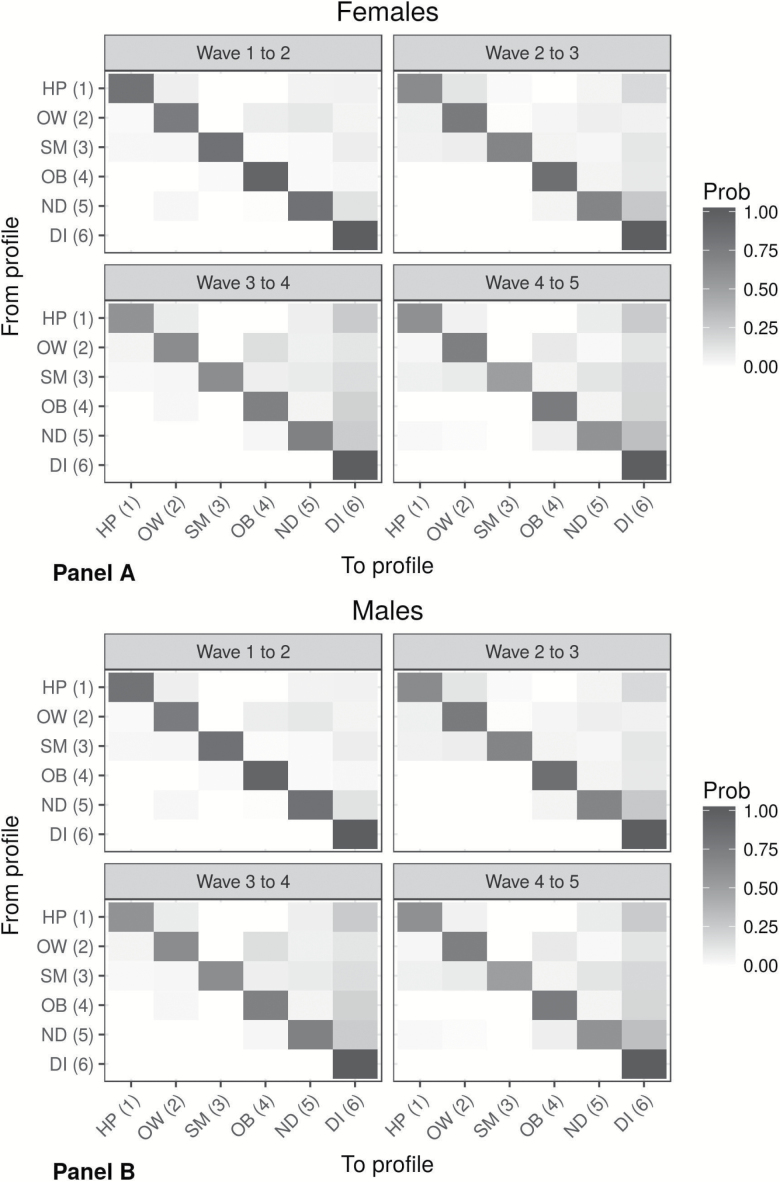
Table 2 shows how the aggregate composition of the sample changed over 25 years of follow-up, and shows how the combined forces of mortality and behavior change contributed to the distribution of health behavior profiles at any point in time. The next step is viewing this process in a longitudinal context. Figure 2 shows the detailed pattern of transitions between health behavior profiles as respondents aged over follow-up, using heat maps of the probabilities of transition from profile to profile across wave to wave transitions. Darker cells indicate a higher transition probability. Each of the four blocks in the figure panels (female on the top and male on the bottom) represents all transition probabilities between two adjacent survey waves, such as from Wave 1 to 2 in the upper left block and Wave 2 to 3 in the upper right. Transitions between each possible pair of health risk profiles are represented as the cells within each block, with the origin profile (at Wave t) indicated on the Y-axis, and destination profile (at Wave t + 1) on the X-axis. For example, the top left cell of the top left block indicates the probability that a woman will stay in the “health promoting” Profile 1 between Waves 1 and 2. Cells on the diagonal from the top left to bottom right of each block represent stability across waves, while those off the diagonal reflect health profile transitions.
Figure 2.
Heat maps of transitions between health behavior profiles from wave to wave by sex (Profile 1: “health promoting—normal BMI, moderate drinkers,” Profile 2: “overweight,” Profile 3: “current smokers,” Profile 4: “obese,” Profile 5: “normal or overweight nondrinkers,” Profile 6: “deceased”).
The dark diagonal present in each block provides evidence of very strong stability in our sample—most respondents remained in the same health behavior profile from wave to wave, though transitions became more frequent as they aged and as the follow-up periods widened from 2.5 years between Waves 1 and 2 to about a decade between Waves 4 and 5. Incumbents of “obese” Profile 4 showed the greatest stability across the entire period, ranging from 94% to 98% among males and females, respectively, from Wave 1 to 2, to 83% and 79%, respectively, from Wave 4 to 5. The large majority of those not remaining in the obese profile died over the observation period. While stability is dominant, there is also evidence of transition across risk behavior profiles over follow-up. The cells above and to the right of the diagonal are more shaded than cells below and to the left, suggesting that men and women tend to transition to profiles associated with a greater risk of death; for example, across the four transitions, 2%–13% of males and 4%–27% of females transitioned from Profile 2 to 4, while only 0%–3% of males and 0%–4% of females transitioned from Profile 4 to 2. Many transitions appear to involve weight gain, such as from “health promoting” Profile 1 to “overweight” Profile 2 (e.g., 15% of males between Waves 2 and 3, and 16% of females between Waves 3 and 4), or from most other profiles to “obese” Profile 4. However, transitions do not always entail risk increases, as shifting from “smoker” Profile 3 to any other profile indicates smoking cessation, a transition made by 8% of female and male respondents between Waves 1 and 2, and by 15%–20% at successive waves. As was evident in Table 2, the likelihood of transitioning to death increases over the 25 years of follow-up, particularly from the “obese” Profile 4, where it increased from 2% between Waves 1 and 2 to 16% between Waves 4 and 5 for both males and females, and from the “nondrinker” Profile 5, where it increased for males from 7% between Waves 1 and 2 to 22% between Waves 4 and 5 and for females from 11% to 62% over the same period.
In exploratory results, we found that women appeared more likely than men to stay in “health promoting” Profile 1 between Waves 1 and 3 (77% vs 56%). Men appeared more likely to transition from “health promoting” Profile 1 directly to death between Waves 2 and 4 (23% vs 3%). Men appeared more likely to stay in the “nondrinker” Profile 5 between Waves 3 and 5 (55% vs 17%), whereas women in this profile appeared more likely to die during the same period (83% vs 33%). With these few exceptions, the broader pattern of stability and change appeared similar for men and women.
Discussion
This study contributes to a growing literature examining how health behaviors cluster into risk profiles that differentiate life courses. We build on prior studies by using a large, nationally representative sample of U.S. adults followed for up to 25 years, and applying LTA. Considering smoking, alcohol use, and BMI, we found profiles that distinguished: (a) “health promoting” behaviors of those with normal weight and moderate drinking, (b) “overweight” moderate drinkers, (c) current “smokers”, (d) “obese” nondrinkers, and (e) normal or overweight “nondrinkers.” We also created an absorbing sixth category to capture mortality, a particular contribution of our methodological approach.
The ACL data offered a view of multiple potential change points over a quarter century. While transition across profiles was less common than stability from wave to wave among survivors, we observed transitions that likely involved weight gain (especially from “overweight” to “obese”), cessation of drinking (from any other profile to “nondrinker”), and cessation of smoking (particularly into the “nondrinker” profile). Respondents in the “obese” and “nondrinker” profiles showed the greatest risk of mortality, despite their abstinence from drinking or smoking. In results not shown, we found that these respondents were significantly older at baseline than those in the “health promoting” profile, and had more chronic health problems and poorer self-rated health, so health-related concerns may already have motivated tobacco and alcohol cessation, or older cohorts may have had fewer lifetime users.
We also observed important mortality transitions, particularly in the later portion of the observation period. In results not shown, we verified that in each wave-to-wave transition, respondents who died were on average older than those transitioning to other profiles or remaining in the same one, regardless of which profile they belonged to in the prior wave. However, those who died directly from the “smoker” profile, rather than transitioning to another profile first, were younger than other decedents. Moreover, in results not shown we found that the average age of incumbents of the “smoker” profile did not change much across waves, clearly showing the premature loss of incumbents to death to a much greater degree than from other profiles. Cross-sectional studies and longitudinal studies that do not directly assess loss of respondents to mortality cannot observe the role of this increasing selectivity of survivors at older ages, a potentially serious limitation if it alters the remaining population composition and the clustering of risk behaviors observed in later life. Not accounting for mortality could mean that researchers overestimate the role of intentional behavior change (as in the case of smoking cessation) in the evolving population distribution of risk behavior profiles across age ranges. However, we found that mortality risk was greatest among those who reported no obvious health-compromising behaviors at the previous wave—they were nondrinking, nonsmoking, nonobese individuals—so the impacts of differential mortality are not simple and likely vary by age and across contexts.
Although we found evidence of weight gain and alcohol and tobacco cessation, results from the transition analysis showed considerable stability: for any wave-to-wave period, and for both women and men, more respondents maintained the same health behavior profile than changed to another (54%–98% overall, except for only 38% remaining in the nondrinking profile among women from Wave 4 to 5). This finding is consistent with prior studies of single behaviors or earlier parts of the life course that have shown healthy and unhealthy behaviors already stabilizing between adolescence and adulthood. A study of Norwegian adolescents followed for 19 years found that about a quarter showed stable, low levels of healthy and unhealthy behaviors over time, while another 38% showed persistently high levels of unhealthy behaviors over time (Wiium, Breivik, & Wold, 2015). This stability for almost two-thirds of the sample appeared to start in early adolescence, though the latent class growth analytic approach may have averaged over some variability and change in order to arrive at three stable trajectory classes. A study of U.S. young adults found that only about one-third showed stably health-promoting or -compromising health behavior profiles, but about 20% of respondents could be classified as transitioning because they were gaining weight (Daw et al., 2017), an indicator not used in the Norwegian study. The present study also showed weight gain as an important driver of transition, but considered an older population not as likely to be initiating behaviors like heavy drinking as young people transitioning to adulthood. More similarly, a study of elderly Taiwanese found profiles distinguished more by varying baseline levels of smoking, alcohol use, regular exercise, and health checkups than by transition, with the exception of a profile defined by men who quit smoking (Hsu et al., 2013).
We also considered these patterns separately for men and women. As in prior studies (Berrigan et al., 2003; Hsu et al., 2013; Schneider, Huy, Schuessler, Diehl, & Schwarz, 2009), we found that women were less likely to smoke or drink than men at baseline, yielding less compromising baseline profiles. However, the pattern of subsequent stability or transition between risk behavior profiles over follow-up appears similar for men and women. Although further research is needed, this finding suggests that sex differences in health behaviors and outcomes in later life are strongly influenced by earlier life mechanisms that sort men and women differentially into risk environments and lifestyles. However, recent discussion of patterns in women’s life expectancy in the United States (Kindig & Cheng, 2013) and in the life expectancy of women in the United States relative to peer nations (Institute of Medicine & National Research Council, 2013) suggests the importance of exploring whether convergence in health behaviors throughout life may shift this pattern.
One explanation for the predominance of stability and its potential contribution to cumulative health disadvantage for some sociodemographic groups can be found in health lifestyle theory, an approach that identifies both individual choices and structural factors as shaping and reinforcing a pattern of health behaviors (Cockerham, 2005). Structural factors include the social circumstances that constrain or enable healthy behavior in a wholesale way, from financial and health care resources to the behavioral practices appropriate to those in one’s social class or social networks, to the racial and gender stratification that cross-cut and fuel those and other circumstances. These results and health lifestyle theory suggest the value of intervening on people, rather than on one behavior at a time (Saint Onge & Krueger, 2017). Our results show that, for example, focusing solely on smoking behavior can be useful, as one health behavior profile is determined entirely by this behavior and it is associated with an increased risk of premature mortality. However, variation in levels of mortality risk and the likelihood of transitioning to other profiles among nonsmokers would be missed if BMI and alcohol use were not considered at the same time. Additionally, a study of physical activity, smoking, and fruit, vegetable and fat consumption found that these behaviors were weakly correlated among Dutch adults, but that individuals who were preparing to change their diet were also likely to be preparing to change another behavior (de Vries et al., 2008). There is some evidence for the efficacy of interventions designed to reduce multiple risk behaviors at the same time (Prochaska et al., 2012), but more research is needed that considers the determinants of health-promoting profile transitions—and of maintaining these—for hints as to the importance of underlying background and structural factors.
This study has some important limitations that point toward important future research. We simplified behavioral measures to estimate these models, partially due to sample size and power issues, but also because of the implausibility of some transitions in the potential matrix (such as from former to never smoker). Simplification of measures increases the difficulty associated with floor and ceiling effects that dampen the potential to observe transitions to better or worse behavioral arrangements. Power issues also precluded looking at socioeconomic status as a predictor or modifier of these associations, though we expect that behavioral change trajectories are associated with education and financial resources (Berrigan et al., 2003; Schneider et al., 2009). Many possible predictors of behavior and of behavior change were not included in the models presented here, due to inadequate power, but these descriptive findings could help to guide future analyses that draw on theory and past empirical evidence about specific kinds of behavior change over the life course. The behaviors we studied here were also all self-reported, though the within-person change design addresses issues of stable reporting style variation across individuals that are typical when using observational data. Moreover, we used only three key health behaviors; other studies have shown the value of considering a wider array of both health-compromising and -promoting behaviors (Saint Onge & Krueger, 2017). Finally, our sample includes individuals aged 25 and older, who face varying life course behavioral norms, incentives and resources to change, and risk of mortality. A study of the transition to adulthood, a time of admittedly greater volatility in behavior, found that the salient health lifestyle profiles changed from late adolescence through early adulthood (Lawrence, Mollborn, & Hummer, 2017). Future research using larger samples could stratify by theoretically meaningful stages of early through late adulthood to explore potential variation in the most salient health risk profiles and the level of stability versus change across them as normative behavior patterns shift with age and as different cohorts pass through the life course.
Supplementary Material
Acknowledgments
Author contributions: S. A. Burgard planned the study, supervised the data analysis, and wrote the article. K. Y. P. Lin and B. D. Segal performed the statistical analyses and contributed to the planning of the study, and the writing and revising of the article. M. R. Elliott supervised the data analysis and contributed to the writing and revising of the article. S. Seelye contributed to the writing and revising of the article.
Funding
This work was supported by the National Institutes on Aging at the National Institutes of Health (5R01AG018418).
Conflicts of Interest
None reported.
References
- Aubin H. J. Farley A. Lycett D. Lahmek P. & Aveyard P (2012). Weight gain in smokers after quitting cigarettes: Meta-analysis. BMJ (Clinical Research ed.), 345, e4439. doi:10.1136/bmj.e4439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrigan D., Dodd K., Troiano R. P., Krebs-Smith S. M., & Barbash R. B (2003). Patterns of health behavior in U.S. adults. Preventive Medicine, 36, 615–623. doi:10.1016/S0091-7435(02)00067-1 [DOI] [PubMed] [Google Scholar]
- Cockerham W. C. (2005). Health lifestyle theory and the convergence of agency and structure. Journal of Health and Social Behavior, 46, 51–67. doi:10.1177/002214650504600105 [DOI] [PubMed] [Google Scholar]
- Cockerham W. C., Bauldry S., Hamby B. W., Shikany J. M., & Bae S (2017). A comparison of black and white racial differences in health lifestyles and cardiovascular disease. American Journal of Preventive Medicine, 52(Suppl. 1), S56–S62. doi:10.1016/j.amepre.2016.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coups E. J. Gaba A. & Orleans C. T (2004). Physician screening for multiple behavioral health risk factors. American Journal of Preventive Medicine, 27, 34–41. doi:10.1016/j.amepre.2004.04.021 [DOI] [PubMed] [Google Scholar]
- Daw J. Margolis R. & Wright L (2017). Emerging adulthood, emergent health lifestyles: Sociodemographic determinants of trajectories of smoking, binge drinking, obesity, and sedentary behavior. Journal of Health and Social Behavior, 58, 181–197. doi:10.1177/0022146517702421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine L. J. Philogene G. S. Gramling R. Coups E. J. & Sinha S (2004). Prevalence of multiple chronic disease risk factors. 2001 National Health Interview Survey. American Journal of Preventive Medicine, 27, 18–24. doi:10.1016/j.amepre.2004.04.017 [DOI] [PubMed] [Google Scholar]
- Holford T. R. Levy D. T. McKay L. A. Clarke L. Racine B. Meza R.,…Feuer E. J (2014). Patterns of birth cohort-specific smoking histories, 1965–2009. American Journal of Preventive Medicine, 46, e31–e37. doi:10.1016/j.amepre.2013.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- House J. S. Lepkowski J. M. Kinney A. M. Mero R. P. Kessler R. C. & Herzog A. R (1994). The social stratification of aging and health. Journal of Health and Social Behavior, 35, 213–234. doi:10.2307/2137277 [PubMed] [Google Scholar]
- Hsu H. C. Luh D. L. Chang W. C. & Pan L. Y (2013). Joint trajectories of multiple health-related behaviors among the elderly. International Journal of Public Health, 58, 109–120. doi:10.1007/s00038-012-0358-9 [DOI] [PubMed] [Google Scholar]
- Institute of Medicine, & National Research Council. (2013). U.S. Health in International Perspective: Shorter Lives, Poorer Health. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Kerr W. C. Greenfield T. K. Bond J. Ye Y. & Rehm J (2009). Age-period-cohort modelling of alcohol volume and heavy drinking days in the US National Alcohol Surveys: Divergence in younger and older adult trends. Addiction (Abingdon, England), 104, 27–37. doi:10.1111/j.1360-0443.2008.02391.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindig D. A. & Cheng E. R (2013). Even as mortality fell in most US counties, female mortality nonetheless rose in 42.8 percent of counties from 1992 to 2006. Health Affairs (Project Hope), 32, 451–458. doi:10.1377/hlthaff.2011.0892 [DOI] [PubMed] [Google Scholar]
- Kvaavik E. Batty G. D. Ursin G. Huxley R. & Gale C. R (2010). Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: The United Kingdom health and lifestyle survey. Archives of Internal Medicine, 170, 711–718. doi:10.1001/archinternmed.2010.76 [DOI] [PubMed] [Google Scholar]
- Lantz P. M. House J. S. Mero R. P. & Williams D. R (2005). Stress, life events, and socioeconomic disparities in health: Results from the Americans’ Changing Lives Study. Journal of Health and Social Behavior, 46, 274–288. doi:10.1177/002214650504600305 [DOI] [PubMed] [Google Scholar]
- Lanza S. T. & Collins L. M (2008). A new SAS procedure for latent transition analysis: Transitions in dating and sexual risk behavior. Developmental Psychology, 44, 446–456. doi:10.1037/0012-1649.44.2.446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza S. T., Dziak J. J., Huang L., Wagner A. T., & Collins L. M (2015). Proc LCA & Proc LTA users’ guide (Version 1.3.2). University Park: The Methodology Center, Penn State. [Google Scholar]
- Laska M. N. Pasch K. E. Lust K. Story M. & Ehlinger E (2009). Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prevention Science, 10, 376–386. doi:10.1007/s11121-009-0140-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence E. M. Mollborn S. & Hummer R. A (2017). Health lifestyles across the transition to adulthood: Implications for health. Social Science & Medicine (1982), 193, 23–32. doi:10.1016/j.socscimed.2017.09.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal A. M. Huh J. & Dunton G. F (2014). Clustering of modifiable biobehavioral risk factors for chronic disease in US adults: A latent class analysis. Perspectives in Public Health, 134, 331–338. doi:10.1177/1757913913495780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollborn S. James-Hawkins L. Lawrence E. & Fomby P (2014). Health lifestyles in early childhood. Journal of Health and Social Behavior, 55, 386–402. doi:10.1177/0022146514555981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore A. A. Gould R. Reuben D. B. Greendale G. A. Carter M. K. Zhou K. & Karlamangla A (2005). Longitudinal patterns and predictors of alcohol consumption in the United States. American Journal of Public Health, 95, 458–465. doi:10.2105/AJPH.2003.019471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieroni L., & Salmasi L (2016). The effect of smoking habit changes on body weight: Evidence from the UK. Economics & Human Biology, 20, 1–13. doi:10.1016/j.ehb.2015.11.002 [DOI] [PubMed] [Google Scholar]
- Prochaska J. O. Evers K. E. Castle P. H. Johnson J. L. Prochaska J. M. Rula E. Y.,…Pope J. E (2012). Enhancing multiple domains of well-being by decreasing multiple health risk behaviors: A randomized clinical trial. Population Health Management, 15, 276–286. doi:10.1089/pop.2011.0060 [DOI] [PubMed] [Google Scholar]
- Saint Onge J. M. & Krueger P. M (2017). Health lifestyle behaviors among U.S. adults. SSM—Population Health, 3, 89–98. doi:10.1016/j.ssmph.2016.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider S. Huy C. Schuessler M. Diehl K. & Schwarz S (2009). Optimising lifestyle interventions: Identification of health behaviour patterns by cluster analysis in a German 50+ survey. European Journal of Public Health, 19, 271–277. doi:10.1093/eurpub/ckn144 [DOI] [PubMed] [Google Scholar]
- Schnuerer I. Baumann S. Haberecht K. Gaertner B. John U. & Freyer-Adam J (2015). Patterns of health risk behaviors among job-seekers: A latent class analysis. International Journal of Public Health, 60, 111–119. doi:10.1007/s00038-014-0623-1 [DOI] [PubMed] [Google Scholar]
- Shaw B. A. & Agahi N (2012). A prospective cohort study of health behavior profiles after age 50 and mortality risk. BMC Public Health, 12, 803. doi:10.1186/1471-2458-12-803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan T. J. DuBrava S. DeChello L. M. & Fang Z (2003). Rates of weight change for black and white Americans over a twenty year period. International Journal of Obesity and Related Metabolic Disorders, 27, 498–504. doi:10.1038/sj.ijo.0802263 [DOI] [PubMed] [Google Scholar]
- Skalamera J. & Hummer R. A (2016). Educational attainment and the clustering of health-related behavior among U.S. young adults. Preventive Medicine, 84, 83–89. doi:10.1016/j.ypmed.2015.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spring B. Moller A. C. & Coons M. J (2012). Multiple health behaviours: Overview and implications. Journal of Public Health (Oxford, England), 34 (Suppl. 1), i3–i10. doi:10.1093/pubmed/fdr111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Agriculture, & U.S. Department of Health and Human Services. (2010). Dietary guidelines for Americans, 2010 (7th ed) Washington, DC: U.S. Government Printing Office. [Google Scholar]
- de Vries H. Kremers S. Smeets T. & Reubsaet A (2008). Clustering of diet, physical activity and smoking and a general willingness to change. Psychology & Health, 23, 265–278. doi:10.1080/14768320701349107 [DOI] [PubMed] [Google Scholar]
- Walsemann K. M., & Ailshire J. A (2011). BMI trajectories during the transition to older adulthood: Persistent, widening, or diminishing disparities by ethnicity and education?Research on Aging, 33, 286–311. doi:10.1177/0164027511399104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiium N. Breivik K. & Wold B (2015). Growth trajectories of health behaviors from adolescence through young adulthood. International Journal of Environmental Research and Public Health, 12, 13711–13729. doi:10.3390/ijerph121113711 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.