Abstract
Skin conditions are one of the most frequent reasons for visiting a primary health care facility, making it of vital importance that general practitioners (GPs) have the right knowledge and tools to diagnose the most frequent dermatological conditions. Methods: This study evaluates the accuracy of dermatological diagnoses made by 120 GPs based on photographs taken with a smartphone by an anonymous online cross-sectional survey. Results: The study was carried out between August and October 2018. The results show that the majority of the participants are in favor of using mobile phones to communicate with other professionals and use them to consult medical images. The majority (69%) took dermatological photographs and the preferred device was a smartphone (70%). From 22 different images evaluated, in 69% of responses, participants expressed a high degree of confidence in their ability to diagnose the lesion shown and in 72% of the cases, the diagnosis chosen was correct. Conclusions: The study confirms that the use of smartphone to send medical images is growing rapidly and its potential for taking medical images is an opportunity to help primary care teams deal with dermatological problems. The results suggest that GPs need further training in interpreting dermatological images, to increase their diagnostic confidence and to avoid the need for referrals to face-to-face visits.
Keywords: telemedicine, mobile phone, dermatology, primary care
Introduction
Skin conditions are one of the most frequent reasons for consultations with general practitioners (GPs), accounting for around 24% of the total.1,2 Approximately 80% of dermatological consultations performed by GPs concern common skin conditions, which can be adequately managed in the primary health care (PHC) setting, without the need to consult a dermatologist.3
GPs need to be aware of the importance of skin conditions and ensure they are dealt with in their training and everyday practice, since many common skin conditions can be easily recognizable and generally do not require complex diagnostic techniques. GPs are the health system’s first point of contact with the patient and they must know how to correctly diagnose the most frequent dermatological conditions in their region, be aware of the criteria for referral to a specialist, and be familiar with the medications most frequently employed in the treatment of these conditions.
Around 5.5% of all PHC consultations for dermatological conditions are referred to a specialist.3,4 However, this figure has seen a 15.5% increase over the past 5 years and it is expected that an aging population will generate more queries in this specialty since certain common conditions, particularly skin cancer, occur with a much higher frequency in the elderly and they are often more difficult to treat in the presence of age-related comorbidities.
Although dermatology consultations represent an important part of the workload of a GP, there is an increasing number of nurses in PHC, who are autonomously treating patients with minor illnesses and skin conditions in the community. The role of these advanced nurses represents a new approach to offer these services from primary care. However, such nurses often need to be able to consult a doctor for the management of some dermatological conditions and this implies that GPs often act as dermatological imaging consultants.4
It is likely that community nurses and home care nurses will see an increasing number of patients with complex skin conditions, especially elderly patients, together with acute cases and lesions which are making poor progress. As a result, the possibility of using new means of communication, such as mobile devices, can help improve clinical decision making by nursing and treat these conditions in a more agile and adequate way.5
Mobile technology is changing the landscape of the medical profession as the need for support tools for decision making and accessing updated clinical information at the point of care increases.6,7 Various surveys have shown that more than 80% of nurses use smartphone apps as part of their daily work8 and 67% of residents use their own smartphones as part of their clinical care.9 Smartphones offer health professionals a less cumbersome format than electronic medical records for a reasonable price, by combining the features of a conventional telephone, a pager, a camera, and a minicomputer. Their impact on improving efficiency within health care organizations by promoting better time management and improved communications with other health care colleagues over the internet, means they are increasingly used in day-to-day clinical work.10,11
Digital clinical photography is increasingly used among the community of health care professionals to document wounds and skin lesions and conduct remote consultations.12,13 The ability to attach high-quality photos to written notes when detailing the characteristics of the lesion helps provide a record that can be referred back to, track any developments, and provide diagnostic support.14,15
Since health professionals are under ever-greater pressure to take on a greater caseload in response to a growing demand for health care, a wider variety of professionals will treat more patients with skin lesions. The ability to send an image, with or without accompanying data, to a consultant or physician using electronic means helps improve patient care and interprofessional collaboration.16,17 Although initially one might think that the use of such tools would only be of benefit to patients and professionals in rural and remote settings, they are also beneficial for urban patients who face obstacles to accessing specialized health care.18 Unlike hospital settings, community health care provides unique conditions for the use of clinical digital photography and new challenges related to the setting, working practices and the possible absence of health care policies to support such practices.
The adoption of this new communication channel using mobile phones by actors in the community health system could result in the need to reexamine the existing institutional structure with a broader view. This development is shifting the locus of interaction and is opening up to question the team’s acting routines.19 Digital technology has facilitated various types of interactions (and new health professionals roles) and creating a new relationship between community health teams.20
There are often scarce resources available to home care nurses when dealing with certain skin lesions and obtaining the remote support of primary care physicians through the use of a photographic consultations of a skin lesion would be very useful.21 The use of photographs taken with a mobile phone to make a referral in primary care is often necessary for diagnostic purposes and the management of skin conditions.14 It can be a great help to GPs in dealing with a heavy caseload and in making accurate diagnoses.
The objective of the study is to assess the confidence, precision, and reliability of the diagnoses made by GPs, based exclusively on photographs of skin lesions taken with a mobile phone, in order to increase their capacity to resolve and reduce referrals to dermatology clinics.
Materials and Methods
This is a descriptive cross-sectional study, conducted by means of an online survey, between August and October 2018. We used a convenience sample of 154 primary care professionals, all of whom are practicing GPs in Catalonia, Spain. The participants were contacted via email with the help of the Catalan Society of Family and Community Medicine (CAMFIC). An email was sent to the 4300 partners of the society with a valid email address. All of them had previously given their consent to be contacted. Participants were recommended to open the survey from a browser on a desktop PC to correctly view the images. However, this was a recommendation and this issue was not controlled in the study.
The survey was conducted using Google Forms (Google LLC). Participants accessed the online survey via a link sent in a personalized email. There was no financial incentive to participate in the study. The first page of the survey informed the participants as to the purpose of the study and encouraged them to contact the principal investigator if they had any questions or needed any clarification (contact details were also included on the same page). We use a multiple-choice survey because it provides a consistency of choice that cannot be achieved with other survey’s formats.22 This format gave us almost instantaneous responses from questions asked remotely online, taking advantage of all the powerful attributes of multimedia when presenting questions. In concordance studies, a type of statistical adjustment similar to that used in multiple-choice exams can be used to adjust the number of agreements that could have occurred by chance.23
The questionnaire was divided into 2 main sections: the first section contained 9 demographic questions regarding gender, education, workplace, opinions and the usage of apps to take pictures and for consultations; the second section was composed of 22 groups of 8 questions, to evaluate the images included in the survey. Some questions allowed the respondents to add text (eg, “other diagnosis”) and others allowed them to exclude answers (“Yes” or “No” options). As all the questions were required, incomplete questionnaires were not recorded. Only one response was allowed for each email sent. No records were kept of respondents who left the survey before completing it and only completed questionnaires were analyzed. No statistical weighting was applied.
In terms of the images used in the survey, mobile phones were used to take photographs of 22 patients who visited, face to face, 2 different dermatologists on the same day. For the purpose of the study, the diagnoses made by dermatologists are considered to be certain. In some cases, the dermatologist needed confirmation by biopsy, while in others it was exclusively a clinical diagnosis. Whether or not to perform a confirmatory biopsy was left to the dermatologists’ discretion. All the patients were asked for, and subsequently gave their written informed consent, to use the photographs included in the study. The patients were examined at the Dermatology Unit of the University Hospital of Vic by 1 of the 2 dermatologists who participated in the study. Each dermatologist examined approximately half of the patients and gave a single diagnosis. Table 2 shows the different types of diagnoses included in the study.
Table 2.
Characteristics of the Images (N = 22).
| Type of lesion, n (%) | Photograph range | |||
|---|---|---|---|---|
| Close-up, n (%) | Medium, n (%) | Long, n (%) | Total, n (%) | |
| Inflammatory dermatitis | 1 (17) | 3 (50) | 2 (33) | 6 (27) |
| Melanocytic nevus | 4 (80) | — | 1 (20) | 5 (23) |
| Other skin infection | 2 (40) | 3 (60) | — | 5 (23) |
| Skin cancer | 2 (100) | — | — | 2 (9) |
| Eczema | — | 2 (100) | — | 2 (9) |
| Premalignant lesion | 1 (100) | — | — | 1 (5) |
| Seborrheic keratosis | 1 (100) | — | — | 1 (5) |
After the clinical examination by the dermatologist, the patient’s skin lesions were photographed using the camera on a Samsung J7 smartphone. A popular mobile phone model belonging to a relatively recent generation was chosen, although it was not the most recent model. Specifically, the mobile phone chosen to take the photos for the survey was the most popular in Spain in 2017 (Samsung J7). The images had an average resolution of 2592 pixels, with 24-bit color depth. Up to 3 photographs were taken for each patient for each lesion.
The photos were all taken by the same researcher, who had previously been trained in the use of the smartphone’s camera. The distance between the camera and the skin varied between 5 cm and 200 cm, depending on the skin lesion being examined. Depending on the type of injury and the affected area, we classified the photographs as: close-up, taken at the closest possible distance (generally about 10 cm from the lesion); taken at medium distance (approximately 30 cm away from the lesion), which included identifying anatomical elements; and long or general view, in which the image contained the lesions plus approximately 20% of healthy skin surface.24 The images were transferred to a Google Forms online survey and the 22 cases were randomized and numbered for inclusion in the survey. The approval of the Clinical Research Ethics Committee of the Foundation University Institute for Primary Health Care Research Jordi Gol i Gurina (P18/046) was obtained for the study. The invitation email outlined the study’s aims and procedures, the security and confidentiality of the data, and the respondents were also informed as to their right to refuse to participate. The survey, carried out with Google’s online forms tool, did not show any personal or identifying information about participating professionals or patients and remained active only during the data collection period. At the end of the study, the form was deactivated, and the survey became inactive. The results are stored in an encrypted file in Excel format on a server of the Catalan Health Service. The study was carried out in accordance with current data protection laws.25
To determine the professional’s confidence to make a correct diagnosis based on the images, data referring to images classified as “Yes” were considered in response to the question “Could I make a correct diagnosis of the injury based on this image?”
The number of times the participants made the correct diagnosis was calculated for each image as a percentage of the total ([n/120] × 100). The percentages for each image were averaged and the images sorted according to diagnostic group,4,26 as well as by the type of shot (long, medium, and close) (Table 2). In addition, to test whether there was a significant difference in the general or category-specific percentages, the images were compared using the chi-square test (significance level set at P < .05). The analysis was performed using the SPSS program, version 18 (IBM Corporation) and the data summarized as frequencies and percentages.
Results
Participant Characteristics
Of the 154 respondents, 120 were included as study participants. Five respondents were excluded because they were not GPs and 29 for reporting that they had visual problems (Figure 1). The mean age of the 120 participants was 47 years (SD 9.2; range 27-65 years) and the majority (68/82; 82.9%) were women.
Figure 1.
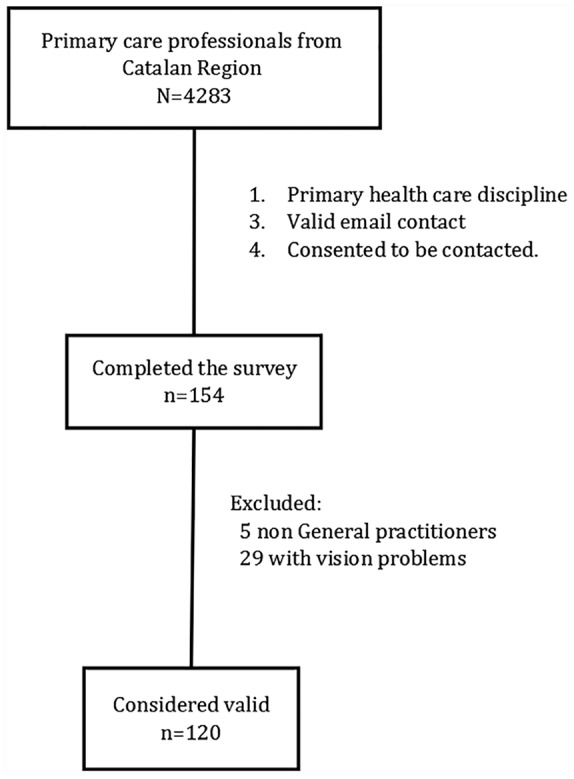
Selection of study participants.
When asked as to their opinion on the use of apps to consult with other health professionals, 85/120 (70.8%) either agree or strongly agree with their use and 63/120 (52.5%) stated that they had previously done so on at least 1 occasion. The majority frequently took dermatological photographs (83/120; 69.2%) and more than half (68/120; 56.7%) use or had used teledermatology (TD). In order of preference, the most used device for taking dermatological photographs was a mobile phone (84/120; 70%), followed by a compact digital camera (17/120; 14.2%) (Table 1).
Table 1.
Demographic Characteristics of the Participants (N = 120).
| Characteristic | n (%) |
|---|---|
| Age (years) | |
| >50 | 43 (35.8) |
| 41-50 | 48 (40.0) |
| 31-40 | 21 (17.5) |
| 20-30 | 8 (6.7) |
| Mean (SD) | 47.25 (9.2) |
| Gendera | |
| Women | 68 (82.9) |
| Men | 14 (17.1) |
| Opinion on using apps to consult with other professionals | |
| Totally agree | 53 (44.2) |
| Agree | 32 (26.7) |
| Neither agree nor disagree | 20 (16.7) |
| Disagree | 9 (7.5) |
| Strongly disagree | 6 (5.0) |
| Consultations using mobile devices (smartphone or iPad) | |
| Yes | 63 (52.5) |
| No | 57 (47.5) |
| Regular user of Teledermatology | |
| Yes | 68 (56.7) |
| No | 52 (43.3) |
| Regularly takes photos of skin lesions | |
| Yes | 83 (69.2) |
| No | 37 (30.8) |
| Preferred type of camera for taking photos of skin lesionsb | |
| Mobile phone camera | 84 (70.6) |
| Compact digital camera | 17 (14.2) |
| Reflex camera (SLR) | 3 (2.5) |
| iPad camera | 2 (1.7) |
| No preference | 13 (10.8) |
Lost cases = 38 (31.7%).
Lost cases = 1 (0.8%).
Characteristics of the Photographs
The survey included 22 different photographs, which were grouped by the type of shot and by the type of dermatological lesion. Half of the images (11/22; 50%) were close-ups and the most frequent type of skin conditions photographed were inflammatory dermatitis (6/22; 27.3%), followed by melanocytic nevus (5/22; 22.7%) (Table 2).
Diagnostic Capacity
To assess the GPs’ confidence to diagnose a lesion by means of a photograph taken by a mobile phone, only affirmative answers to the question regarding the possibility of making a diagnosis based on the image shown in the survey were analyzed. Of the 22 images shown to the 120 participants, the GPs responded that they could make a diagnosis based on the image shown an average of 15.2 times (SD 5.2) (69.1%). The average was significantly higher in 2 situations: among GPs who regularly consult other professionals using their mobile device (mean 16.1; SD 4.9); and among older GPs (Pearson correlation 0.2; P = .04). Participants aged >40 years were more likely to make an image-based diagnosis, with an average of 15.76 affirmative responses (SD 5.1) compared with those aged ≤40 years, with an average of 13.5 affirmative responses (SD 5.2), with P = .04 (Table 3).
Table 3.
Factors Associated With the General Practitioners’ Diagnostic Capacity.
| Mean (SD) | P | |
|---|---|---|
| Age (years) | ||
| >40 | 15.8 (5.1) | |
| ≤40 | 13.5 (5.2) | .04 |
| Previous experience of consultations with mobile devices | ||
| Yes | 16.1 (4.9) | |
| No | 14.2 (5.4) | .04 |
When all the participants’ responses to the various photographs shown in the survey were analyzed, in 1824/2640 cases (69.1%), the GPs considered themselves qualified to make a diagnosis of the lesion based on the image.
There was a significant increase in the number of cases in which the GP was able to make a diagnosis in the long shot images (294/360; 81.7%), followed by the medium shot images (658/960; 68.5%). Differences were also observed according to the type of lesion, with a higher number of respondents prepared to make a diagnosis based on images corresponding to lesions due to skin cancer (175/240; 72.9%) and inflammatory dermatitis (529/720; 73.5%) (P = .07). (Table 4). A significant adjusted odds ratio (OR) value less than 1 (P < .05) indicates that the risk in that category is lower than that of the reference category (adjusted OR = 1). The adjusted OR values in the table confirm the previously observed results.
Table 4.
Medical Diagnostic Confidence According to Shot Distance and Type of Lesion.
| Able to make a diagnosis based on the image | ||||
|---|---|---|---|---|
| Yes (n = 1824), n (%)a | No (n = 816), n (%)a | Adjusted odds ratio (95% CI) | P | |
| Shot | ||||
| Close-up | 872 (66.1) | 448 (33.9) | 0.4 (0.3-0.6) | <.001 |
| Medium shot | 658 (68.5) | 302 (31.5) | 0.5 (0.4-0.7) | <.001 |
| Long shot | 294 (81.7) | 66 (18.3) | 1 | |
| Type of lesion | ||||
| Melanocytic nevus | 410 (68.3) | 190 (31.7) | 0.6 (0.5-0.8) | <.001 |
| Skin cancer | 175 (72.9) | 65 (27.1) | 0.8 (0.5-1.1) | .13 |
| Premalignant lesion | 43 (35.8) | 77 (64.2) | 0.2 (0.1-0.2) | <.001 |
| Seborrheic keratosis | 73 (60.8) | 47 (39.2) | 0.4 (0.3-0.7) | <.001 |
| Eczema | 127 (52.9) | 113 (47.1) | 0.3 (0.2-0.4) | <.001 |
| Inflammatory dermatitis | 529 (73.5) | 191 (26.5) | 0.8 (0.6-1.0) | .07 |
| Other skin infection | 467 (77.8) | 133 (22.2) | 1 | |
Percentages are calculated in terms of the total for each row of data.
Reliability and Accuracy of the GPs’ Criteria
Of a total of 2640 possible diagnostic evaluations based on an image, on 1824 occasions (69.1%) the professional judged themselves to be able to make a diagnosis. Among those 1824 occasions, in 511 (28%) the GP felt confident to make a diagnosis based on an image from the survey but made a misdiagnosis.
In order to analyze the sensitivity and specificity of the criteria of GPs regarding their diagnostic confidence, the responses of all the participants were analyzed, including the responses of the participants who felt capable of diagnosing the injury based on the images and those who did not. With the inclusion of correct answers and errors of all the cases, a sensitivity of 77.2% (95% CI 75.1%-79.2%) and a specificity of 45.6% (95% CI 37%-48.8%) were obtained. The positive predictive value of the clinical trial was 72% (95% CI 69.9%-74.0%) and the negative predictive value was 52.5% (95% CI 48.9%-55.9%). The OR for a positive association was 1.4 (95% CI 1.3-1.5) and for a negative association was 0.5 (95% CI 0.5-0.6). This suggests a limited diagnostic value (Table 5).
Table 5.
Cross-Tabulation of Correct Diagnoses Made by the General Practitioners.a
| General practitioner | Dermatologist | ||
|---|---|---|---|
| Positive | Negative | Total | |
| Positive | 1313 | 511 | 1824 |
| Negative | 388 | 428 | 816 |
| Total | 1701 | 939 | 2640 |
Sensitivity 77.2%; specificity 45.6%; positive predictive value 72.0%; negative predictive value 52.5%; positive odds ratio 1.4; negative odds ratio 0.5.
A comparison was made between the participating GPs to measure the degree of agreement between them (precision) regarding the diagnoses of the 22 images, obtaining a kappa value of 0.3 (95% CI 0.1-0.5), with a Z = 80.2 and P < .001.
Diagnostic Accuracy
When we compare the GPs’ diagnostic accuracy against the control diagnoses previously made by a dermatologist, a sensitivity of 76.7% (95% CI 74.6-78.6) and a 47.0% (95% CI 43.6-50.4) specificity are shown. The corresponding false positive rate, or type I error when accepting the GPs criterion (the GP says they are able to make a diagnosis, but make an incorrect diagnosis) was 28% (95% CI 26-30.1) and the false negative rate or type II error (unable to make a diagnosis in correctly diagnosed cases) increases to 53.0% (95% CI 49.6-56.4).
Discussion
The results of the study suggest that the GPs felt confident to provide a diagnosis in almost two-thirds of the dermatological images generated by a mobile phone. Among those images, approximately two-thirds were correctly diagnosed by the same GP. In terms of reliability, the GPs diagnoses produced many cases of false positives (23%) and their diagnostic specificity drops to 50%. There is a considerable percentage of cases that GPs consider themselves unable to diagnose on the basis of the images and they would be diagnosed incorrectly. These results suggest that GPs need to be trained more in order to acquire greater diagnostic knowledge through images and, until then, it will still be necessary to consult the dermatologist to confirm the diagnosis of some lesions, such as skin melanoma, which can cause very serious consequences for the patient’s health.
The results of this study confirm that most of the primary health care GPs surveyed were in favor of the use of mobile devices to consult other health professionals and most of them are already using apps to conduct such consultations.10,11,27 The preferred camera for taking dermatological photographs in a professional context is a mobile phone camera and most of the participants are currently participating or have participated in some form of TD project.10,13,28
The results showed a greater proportion of participants who considered themselves capable of making a diagnosis based on the images used in the survey among GPs with previous professional experience in the use of apps for consultations. Meanwhile, younger participants, surprisingly, were less inclined to risk making a diagnosis based on mobile phone images. Nevertheless, when the study focused on the participants’ diagnostic capacity, the confidence to correctly diagnose lesions was higher among younger participants, as well as among participants who had previous experience in consultations with mobile devices.
The confidence to diagnose a dermatological lesion based on an image taken with a mobile phone, seems to be related to the distance from which the image was taken and to the type of lesion evaluated. The distance that gave GPs involved in the study greater confidence in the diagnosis was the long or medium shot distance. The type of lesions that offered the least diagnostic confidence to GPs were premalignant lesions and eczemas. When the focus was diagnostic accuracy, the correctly diagnosed images were mostly long or close-up shots and the same types of lesions, premalignant lesions and eczema, were the worst diagnosed in the survey. Melanocytic nevus and seborrheic keratosis were the types of diagnosis that GPs were able to diagnose on the greatest number of occasions.
Although the study showed that a significant proportion of the consultations with the specialized dermatology service could be managed within the PHC system, there is a danger that some patients might end up not being referred to a specialized dermatology consultant, when they ought to be (which is particularly worrying in the case of patients with skin cancer).
The study shows that in most cases, the participating GPs did not feel confident to offer a diagnosis for images corresponding to premalignant skin conditions, which means that those cases will need a face-to-face visit with the GP to unsure diagnostic certainty or a referral to a dermatologist.
The number of GPs and their level of training is not keeping pace with the increasing demand for PHC.2,4,29 GPs have only limited training in dermatology, meaning there is an urgent need to provide them with better education and training regarding prevalent dermatological conditions.
A recent study showed that 21% of referrals to specialized care could be treated in the PHC system,30 though potentially the wrong approach to PHC could lead to patients who ought to be referred to a specialist not being referred or worse, being given a misdiagnosis.4 Meanwhile, it is likely that community and home care nurses will to see a greater number of patients with complex skin conditions, particularly among the elderly1,5,8,16 and the confidence and skills needed to handle complex skin conditions in the community will also require training.
There are many concordance studies in TD but most of them analyze the concordance between dermatologist and mainly with inpatients. A recent study found a moderate diagnosis concordance between the general practitioner and the dermatologist31-33 and it seems that the doctors valued the training sessions positively since they improved their diagnostic capacity and their confidence in the management of skin conditions.34 Other studies show a high proportion of diagnostic and management discordance between GPs and dermatologists and support the potential of TD to improve not only access to outpatient dermatologic care but also clinical outcomes in the primary care setting.33
The study has several limitations which could affect the interpretation of the findings and their applicability to a broader context. The use of a convenience sample with the only participants being GPs from a professional society could have led to selection bias. The opportunity to participate was not equal for all the individuals in the target population and study results were not necessarily generalizable to the whole population. As in all quantitative studies, increasing the sample size would have increased the statistical power of the convenience sample.35
In order to evaluate the confidence of GPs to diagnose lesions that are usually referred to the dermatologist, images of patients from a dermatological consultation were chosen. However, given that probably many of these conditions were referred due to their diagnostic difficulty, a bias could have been generated, as the simplest conditions are not usually referred.
One of the study’s most significant limitations is the lack of clinical information accompanying the images, since in real cases, they usually have a text describing the patient’s clinical situation. The study only included images without any accompanying information34 and the lack of related history or symptoms accompanying the images could cause statistical bias. In addition, the low number of skin lesions recruited on the same day for the survey did not offer an enough variety of types of lesions to make it comparable to different real clinical situations. Nevertheless, the number and types of skin conditions photographed for the survey was the result of random day’s recruitment of actual cases seen as part of a regular dermatologist’s caseload.
Even having advised the participants to use a browser on a desktop PC to access the survey, it is difficult to ensure that all of them have done so and any of them could have accessed from other devices like mobiles or tablets. On the other hand, this disparity, even though it may imply a bias, would also reflect a diverse healthcare reality, in which the same professionals access the images of different devices.
There is also another limitation when offering a multiple-choice questions survey that could have an impact on the results. Multiple-choice questions are elemental to survey writing; they are versatile, intuitive, and they yield clean data that is easy to analyze. Since they provide a fixed list of answer options, they give you structured survey responses and make it easier for your respondents to complete the survey. However, the data one gets back are limited to the choices one provides and that means that if answer options are not comprehensive, one risks bias in the results. The multiple-choice questions in the survey contain only a small proportion of all the diagnostic options that could be asked, so that a participant has more options to find the correct answer and may be lucky or unlucky in the selection.36,37
We must also take into consideration that the researcher who took the photographs was not a professional photographer and some studies have shown that the quality of the images can play a significant role in helping the doctor make their diagnosis. Nonetheless, the fact that the photographer who took the photographs for the study used was a trained GP makes it more realistic and similar to the real world.38
The fact that a GP indicated that they could not make an image-based diagnosis and chose a correct or incorrect diagnosis among the 4 possible could be seen as a limitation in calculating the sensitivity and specificity of the test, but as the diagnosis is finally made (despite feeling empowered or not), we are finally able to evaluate these results objectively. Otherwise, since this is a descriptive study, with no control groups, it is not possible to establish a cause and effect relationship.
We must bear in mind that the images used in this study come from dermatology referrals made by GPs and therefore they are cases in which GPs were unable to make a diagnosis. This introduces a bias in the selection of cases as all of them needed an opinion from a specialist.
Due to the methodology used for the study, there was no blinding of the participants, who were informed about the purpose of the study.
The use of images of skin conditions in mobile health (mHealth) concerns the diagnostic capacity, monitoring and subsequent care of potentially malignant and chronic skin lesions which are based on the use of objective measurements. Several studies have demonstrated high sensitivity and specificity of TD using images taken with mobile phones to evaluate potentially malignant skin lesions.39,40
There have also been various studies on the ability to view images taken with a mobile phone to monitor the care of wounds in specialties such as plastic surgery,41 burns, and postoperative wounds.42 In most cases, studies showed that nonspecialized medical workers (training doctors, nurses, allied health professions) require minimal additional training to take simple photographs.38 This is of considerable importance in rural and remote areas where there are distribution challenges and a shortage of specialists.43
Deep learning technologies have demonstrated the potential to achieve similar results to face-to-face care. Unfortunately, most current mobile app diagnostic systems are based on untested technologies that do not meet the precision standard required. However, in the coming years TD research must refine deep learning and artificial intelligence methods to work with images from highly variable smartphones used in long-distance functional diagnostics. New developments in artificial intelligence systems are achieving great dermatologist-level performance in the diagnosis of melanoma cases. Smartphone industry projects that next-generation devices will put hardware with deep learning capabilities in the hands of consumers. All these advances promise to be a good solution for some of the problems that arose in this study.44
The results of this study provide new data on the use and perceived benefits of using mobile phone images among PHC professionals and, specifically, on their capabilities in terms of their criteria and ability to diagnose skin conditions. This demonstration that health professionals can make use of mobile phone images should alert us to the need to improve their benefits, while also ensuring these new tools are employed in a proper and safe manner. Additional analytical-experimental research which employs more comprehensive methods to recruit participants is essential to confirming and broadening the results of the study.
Conclusions
Despite the growing number of studies on mHealth and TD, there are currently few studies on the ability of PHC teams to autonomously diagnose dermatological conditions using mobile phone photographs. Most studies have sought to analyze the capacity and accuracy of dermatologists when they act as consultants in TD. This limits the extent to which any findings can be extrapolated to low-resource situations, where mHealth and mobile phone images are used.
Sending skin photographs using mobile phone represents an internal tool to deal with simpler dermatological conditions, in the community and from the point of view of the PHC team.
The study shows that GPs involved in the study can diagnose different dermatological conditions based on photographs taken with mobile phones, with 1701 of 2640 (64%) correct diagnoses, and that they can also diagnose skin lesions using only images. However, this percentage increases when the same result is analyzed exclusively on the total number of GPs who claimed to be able to do so, which in this case is 1313 of 1824 (72%). As expected, the successes increase in those cases in which the GP had confidence in his or her diagnostic capacity. Worryingly, premalignant lesions appear to be the skin lesions that lead to the largest number of misdiagnoses, but they are also the lesions that GPs were least able to diagnose based on the images.
The use of mobile phones for medical imaging is growing rapidly. With increasing image quality, the increasing computing power of smartphones, combined with the increasing need for PHC teams to find solutions to the health problems of an aging population, mHealth imaging has the potential to transform the future of medical imaging.
It seems advisable, therefore, that health institutions respond to the need to improve general and specific knowledge regarding the use of cell phone cameras in primary care. Improving and facilitating the use of this tool among primary and community care professionals facilitates interprofessional communication within teams and their ability to treat dermatological conditions in the community. Its use among primary care professionals increases accessibility to not only dermatologists through TD but also with other primary care professionals. The growing potential of artificial intelligence could offer new ways to explore this field in the near future.
Acknowledgments
We would like to express our gratitude to the Unitat d’Investigació de Catalunya Central for their collaboration in conducting the study and to all those PHC professionals who took part in the survey. The study was carried out within the framework of the Universitat de Vic–Universitat Central de Catalunya’s PhD program in Experimental Sciences and Technologies.
Footnotes
Author Contributions: Conceptualization, FXM-G, JV-A, CJS, and RTF; methodology, FXM-G, JV-A, PRP and JMP; software, FXM-G and JV-A; validation, FXM-G, JV-A, CJS, and RTF; formal analysis, FXM-G; investigation, FXM-G and JV-A; resources, FXM-G and JV-A; data curation, FXM-G and JV-A; writing—original draft preparation, FXM-G; writing—review and editing, FXM-G, JV-A, PRP, CJS, RTF, and JMP. All authors have read and agreed to the published version of the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Francesc X. Marin-Gomez  https://orcid.org/0000-0002-6749-0468
https://orcid.org/0000-0002-6749-0468
References
- 1. Schofield JK, Fleming D, Grindlay D, Williams H. Skin conditions are the commonest new reason people present to general practitioners in England and Wales. Br J Dermatol. 2011;165:1044-1050. doi: 10.1111/j.1365-2133.2011.10464.x [DOI] [PubMed] [Google Scholar]
- 2. Goetsch NJ, Hoehns JD, Sutherland JE, Ulven ME, Shiyanbola OO, Rauch MK. Assessment of postgraduate skin lesion education among Iowa family physicians. SAGE Open Med. 2017;5:2050312117691392. doi: 10.1177/2050312117691392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Schofield J, Grindlay D, Williams H. Skin Conditions in the UK: A Health Care Needs Assessment. Centre of Evidence Based Dermatology, University of Nottingham; 2009. Accessed June 13, 2020 http://www.nottingham.ac.uk/ [Google Scholar]
- 4. The King’s Fund. ’How can dermatology services meet current and future patient needs while ensuring that quality of care is not compromised and that access is equitable across the UK? Published March 7, 2014. Accessed June 13, 2020 http://www.bad.org.uk/shared/get-file.ashx?id=2347&itemtype=document
- 5. Danielsen BV, Sand AM, Rosland JH, Førland O. Experiences and challenges of home care nurses and general practitioners in home-based palliative care—a qualitative study. BMC Palliat Care. 2018;17:95. doi: 10.1186/s12904-018-0350-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hernández-Neuta I, Neumann F, Brightmeyer J, et al. Smartphone-based clinical diagnostics: towards democratization of evidence-based health care. J Intern Med. 2019;285:19-39. doi: 10.1111/joim.12820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mosa ASM, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Med Inform Decis Mak. 2012;12:67. doi: 10.1186/1472-6947-12-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Whitehouse A, Griffiths B, Prince N, Round J, Kelly C, Lee HM. G233(P): the smartphone generation. Arch Dis Child. 2014;99(suppl 1):A99-A100. doi: 10.1136/archdischild-2014-306237.227 [DOI] [Google Scholar]
- 9. Raaum S, Vallejo C, Patino AM, Arbelaez C, Milne C. International comparison of smartphone use by resident physicians. Ann Glob Health. 2015;81:81. doi: 10.1016/j.aogh.2015.02.691 [DOI] [Google Scholar]
- 10. Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14:e128. doi: 10.2196/jmir.1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Marin-Gomez FX, Cuyas FG, Reig-Bolano R, et al. Social networking app use among primary health care professionals: web-based cross-sectional survey. JMIR Mhealth Uhealth. 2018;6:e11147. doi: 10.2196/11147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shi RB, Qiu J, Maida V. Towards algorithm-enabled home wound monitoring with smartphone photography: a hue-saturation-value colour space thresholding technique for wound content tracking. Int Wound J. 2019;16:211-218. doi: 10.1111/iwj.13011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Au Y, Holbrook M, Skeens A, et al. Improving the quality of pressure ulcer management in a skilled nursing facility. Int Wound J. 2019;16:550-555. doi: 10.1111/iwj.13112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Institute of Medication Illustrators. IMI National Guidelines: Clinical Photography in Wound Management. Institute of Medical Illustrators; 2007. [Google Scholar]
- 15. Bradshaw LM, Gergar ME, Holko GA. Collaboration in wound photography competency development. Adv Skin Wound Care. 2011;24:85-92. doi: 10.1097/01.ASW.0000393762.24398.e3 [DOI] [PubMed] [Google Scholar]
- 16. Reischl U, Salinas O, Oberleitner R, Mijovic B. Nursing student remote performance assessment using a novel smartphone application. Proc Int Symp Hum Factors Ergon Health Care. 2018;7:17-20. doi: 10.1177/2327857918071000 [DOI] [Google Scholar]
- 17. Chakraborty C. Mobile health (M-Health) for tele-wound monitoring. In: Mobile Health Applications for Quality Healthcare Delivery. IGI Global; 2019:98-116. doi: 10.4018/978-1-5225-8021-8.ch005 [DOI] [Google Scholar]
- 18. Hogenbirk JC, Byrne K, Pong RW, Liboiron-Grenier LJ. National Initiative for Telehealth Guidelines: Environmental Scan of Organizational, Technology, Clinical and Human Resource Issues. NIFTE Research Consortium; 2003. [Google Scholar]
- 19. Giddens A. The Consequences of Modernity. Stanford University Press; 1990. [Google Scholar]
- 20. Orlikowski WJ. The duality of technology: rethinking the concept of technology in organizations. Organ Sci. 1992;3:398-427. doi: 10.1287/orsc.3.3.398 [DOI] [Google Scholar]
- 21. Buckley KM, Adelson LK, Agazio JG. Reducing the risks of wound consultation. J Wound Ostomy Continence Nurs. 2009;36:163-170. doi: 10.1097/01.WON.0000347657.02594.36 [DOI] [PubMed] [Google Scholar]
- 22. Brown RW. Multi-choice versus descriptive examinations. In: 31st Annual Frontiers in Education Conference. Impact on Engineering and Science Education. Conference Proceedings (Cat. No.01CH37193). Vol 1 Reno, NV: IEEE; 2001:T3A-13-18. doi: 10.1109/FIE.2001.963903 [DOI] [Google Scholar]
- 23. Feinstein AR. Principles of Medical Statistics. 1st ed Chapman & Hall/CRC Press; 2001. [Google Scholar]
- 24. Perera C, Chakrabarti R. The utility of mHealth in medical imaging. J Mob Technol Med. 2013;2:4-6. doi: 10.7309/jmtm.2.3.2 [DOI] [Google Scholar]
- 25. Arimany Manso J, Taberner Ferrer R, Pidevall I, Mascaró Ballester JM, Martin-Fumadó C. Implicaciones bioéticas y médico-legales del uso de la fotografía en dermatología. Actas Dermosifiliogr. 2020;111:107-114. doi: 10.1016/j.ad.2019.04.007 [DOI] [PubMed] [Google Scholar]
- 26. Buendía-Eisman A, Arias-Santiago S, Molina-Leyva A, et al. Análisis de los diagnósticos realizados en la actividad ambulatoria dermatológica en España: muestreo aleatorio nacional DIADERM. Actas Dermosifiliogr. 2018;109:416-423. doi: 10.1016/j.ad.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 27. Mobasheri MH, King D, Johnston M, Gautama S, Purkayastha S, Darzi A. The ownership and clinical use of smartphones by doctors and nurses in the UK: a multicentre survey study. BMJ Innov. 2015;1:174-181. doi: 10.1136/bmjinnov-2015-000062 [DOI] [Google Scholar]
- 28. Pecina JL, Wyatt KD, Comfere NI, Bernard ME, North F. Uses of mobile device digital photography of dermatologic conditions in primary care. JMIR Mhealth Uhealth. 2017;5:e165. doi: 10.2196/mhealth.8257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Beroukhim K, Nguyen C, Danesh MJ, Wu JJ, Koo J. The evolving role of primary care practitioners in dermatology: current status and emerging educational resources. J Dermatol Nurses Assoc. 2015;7:325-329. doi: 10.1097/JDN.0000000000000168 [DOI] [Google Scholar]
- 30. Basarab T, Munn SE, Russell Jones R. Diagnostic accuracy and appropriateness of GP referrals to a dermatology outpatient clinic. Br J Dermatol. 1996;135:70-73. [PubMed] [Google Scholar]
- 31. Cutler L, Ross K, Withers M, Chiu M, Cutler D. Teledermatology: meeting the need for specialized care in rural Haiti. J Health Care Poor Underserved. 2019;30:1394-1406. doi: 10.1353/hpu.2019.0097 [DOI] [PubMed] [Google Scholar]
- 32. Dahlén Gyllencreutz J, Paoli J, Bjellerup M, et al. Diagnostic agreement and interobserver concordance with teledermoscopy referrals. J Eur Acad Dermatol Venereol. 2017;31:898-903. doi: 10.1111/jdv.14147 [DOI] [PubMed] [Google Scholar]
- 33. Nelson CA, Takeshita J, Wanat KA, et al. Impact of store-and-forward (SAF) teledermatology on outpatient dermatologic care: a prospective study in an underserved urban primary care setting. J Am Acad Dermatol. 2016;74:484-490.e1. doi: 10.1016/j.jaad.2015.09.058 [DOI] [PubMed] [Google Scholar]
- 34. Costello CM, Cumsky HJL, Maly CJ, et al. Improving access to care through the establishment of a local, teledermatology network. Telemed J E Health. Published online October 15, 2019. doi: 10.1089/tmj.2019.0051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Suen LJW, Huang HM, Lee HH. A comparison of convenience sampling and purposive sampling [in Chinese]. Hu Li Za Zhi. 2014;61:105-111. doi: 10.6224/JN.61.3.105 [DOI] [PubMed] [Google Scholar]
- 36. Burton RF. Quantifying the effects of chance in multiple choice and true/false tests: question selection and guessing of answers. Assess Eval High Educ. 2001;26:41-50. doi: 10.1080/02602930020022273 [DOI] [Google Scholar]
- 37. Royal KD, Stockdale MR. The impact of 3-option responses to multiple-choice questions on guessing strategies and cut score determinations. J Adv Med Educ Prof. 2017;5:84-89. [PMC free article] [PubMed] [Google Scholar]
- 38. Florczak B, Scheurich A, Croghan J, et al. An observational study to assess an electronic point-of-care wound documentation and reporting system regarding user satisfaction and potential for improved care. Ostomy Wound Manage. 2012;58:46-51. [PubMed] [Google Scholar]
- 39. Massone C, Hofmann-Wellenhof R, Ahlgrimm-Siess V, Gabler G, Ebner C, Soyer HP. Melanoma screening with cellular phones. PLoS One. 2007;2:e483. doi: 10.1371/journal.pone.0000483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kroemer S, Frühauf J, Campbell TM, et al. Mobile teledermatology for skin tumour screening: diagnostic accuracy of clinical and dermoscopic image tele-evaluation using cellular phones. Br J Dermatol. 2011;164:973-979. doi: 10.1111/j.1365-2133.2011.10208.x [DOI] [PubMed] [Google Scholar]
- 41. Hsieh CH, Tsai HH, Yin JW, Chen CY, Yang JCS, Jeng SF. Teleconsultation with the mobile camera-phone in digital soft-tissue injury: a feasibility study. Plast Reconstr Surg. 2004;114:1776-1782. [DOI] [PubMed] [Google Scholar]
- 42. Engel H, Huang JJ, Tsao CK, et al. Remote real-time monitoring of free flaps via smartphone photography and 3G wireless internet: a prospective study evidencing diagnostic accuracy. Microsurgery. 2011;31:589-595. doi: 10.1002/micr.20921 [DOI] [PubMed] [Google Scholar]
- 43. Coustasse A, Sarkar R, Abodunde B, Metzger BJ, Slater CM. Use of teledermatology to improve dermatological access in rural areas. Telemed J E Health. 2019;25:1022-1032. doi: 10.1089/tmj.2018.0130 [DOI] [PubMed] [Google Scholar]
- 44. Xiong M, Pfau J, Young AT, Wei ML. Artificial intelligence in teledermatology. Curr Dermatol Rep. 2019;8:85-90. doi: 10.1007/s13671-019-0259-8 [DOI] [Google Scholar]


