Abstract
The COVID-19 pandemic has engendered rapid and significant changes in patient care. Within the realm of surgical training, the resultant reduction in clinical exposure and case volume jeopardizes the quality of surgical training. Thus, our general surgery residency program proceeded to develop a tailored approach to training that mitigates impact on resident surgical education and optimizes clinical exposure without compromising safety. Residents were engaged directly in planning efforts to craft a response to the pandemic. Following the elimination of elective cases, the in-house resident complement was effectively decreased to reduce unnecessary exposure, with a back-up pool to address unanticipated absences and needs. Personal protective equipment availability and supply, the greatest concern to residents, has remained adequate, while being utilized according to current guidelines. Interested residents were given the opportunity to work in designated COVID ICUs on a volunteer basis. With the decrease in operative volume and clinical duties, we shifted our educational focus to an intensive didactic schedule using a teleconferencing platform and targeted areas of weakness on prior in-service exams. We also highlighted critical COVID-19 literature in a weekly journal club to better understand this novel disease and its effect on surgical practice. The long-term impact of the COVID-19 pandemic on resident education remains to be seen. Success may be achieved with commitment to constant needs assessment in the changing landscape of healthcare with the goal of producing a skilled surgical workforce for public service.
Key words: covid, coronavirus, education, surgery, training, safety
Competencies: Patient Care, Professionalism, Interpersonal and Communication Skills, Practice-Based Learning and Improvement, Systems-Based Practice
Introduction
Since the first confirmed case of coronavirus in the United States, movement restrictions and physical distancing have become a mainstay in slowing transmission.1, 2, 3 Hospitals have focused on mitigation strategies including postponing or cancelling elective surgical procedures using triage guidelines,4, 5, 6 converting clinics to telemedicine visits, and suspension of in-person meetings including didactic sessions for trainees. The reduction in clinical exposure and surgical cases from the COVID-19 pandemic jeopardizes the quality of surgical training.7
For training programs aiming to address educational gaps, the safety of trainees should be the top priority. The Houston Methodist Hospital (HMH) surgical department was familiar with disaster response planning having recently experienced Hurricane Harvey in 2017. The catastrophic flooding required immediate redesign of the residency program with capacity to adapt with changing needs. The COVID-19 pandemic is different in the national impact, uncertain duration and significant healthcare risk to residents. As national infection rates increased exponentially, a surgery departmental response plan in conjunction with the institution was being discussed among faculty, however, residents were not initially aware. A Cisco WebEx townhall meeting was held to address the mounting anxiety and concerns. Major resident concerns included personal protective equipment (PPE) availability, limiting COVID-19 exposure, and impact on surgical training experience (Table 1 ). To address these concerns, our general surgery residency program rapidly developed and deployed a comprehensive, modified training paradigm to minimize COVID-19’s impact on resident surgical education and optimize resident safety while meeting essential clinical needs.
Table 1.
Resident Concerns During COVID-19 Pandemic and Corresponding Departmental Response
| Resident Concern | Approach |
|---|---|
| PPE availability and appropriate use | Institutional supply supplemented with outpatient clinic stockpile Training for extended PPE such as Powered Air-Purifying Respirators Institutional protocol for PPE use in specific encounters according to CDC guidelines |
| COVID-19 exposure and testing | Outline employee health triage criteria for suspected exposures Provide information on designated testing sites for employees Determine duration of quarantine in symptomatic or COVID-19 positive employees |
| Elective surgeries and clinic schedule | Postponement or cancellation of non-urgent surgical cases in accordance with the Surgeon General and ACS recommendations Combination of inpatient surgical services with decreased resident complement Creation of rotating surgical teams for inpatient care and back-up pool Transition outpatient clinics to telemedicine, excluding resident participation |
| Didactic schedule | Weekly didactic schedule targeting ABSITE topic areas COVID-19 journal club Mock orals sessions |
| Psychological health | Daily institutional mindfulness pause, mental health round table Weekly program director check in Access to licensed mental health professionals in peer support teams |
ACS, American College of Surgeons; PPE, personal protective equipment.
Resident Safety and Wellness
The surgery department, following American College of Surgeons recommendations, canceled or postponed elective cases.4 , 6 This allowed the decrease of in-house residents, thereby reducing unnecessary exposure. Outpatient clinic was converted to telemedicine visits and in-person visits were reserved for patients needing physical attention. Resident participation in the outpatient setting was eliminated and Advanced Practice Providers were utilized when necessary.
Initially, our Graduate Medical Education (GME) office prohibited residents from engaging in the care of COVID-19 positive patients. As the volume of patients increased at HMH, the policy was altered to include residents in their care. Emerging details of nationwide PPE shortages and rationing fueled concern among residents for PPE availability given this new directive. The institution provided PPE, supplemented with outpatient clinic stock, and stayed abreast of innovative ways to conserve existing PPE.8 Residents also received training in advanced PPE, such as powered air-purifying respirators for aerosolizing procedures. PPE standards were harmonized across the Texas Medical Center, including all sites of externally rotating residents. Several safety protocols were instituted by the surgical department in the operating room to minimize exposure. Foremost, only anesthesia staff remained in the room for intubation and extubation of all patients. In addition, smoke evacuators for laparoscopic cases were trialed by faculty before residents were allowed to participate in laparoscopic cases. Participation in high risk aerosolizing procedures such as bronchoscopy and tracheostomy were limited to experienced upper level surgical residents and N95 masks and powered air-purifying respirators were required. A tracheostomy placement protocol was developed among all service lines which included a mandatory 21 day period since positive testing and/or 2 negative tests within 48 hours prior to the procedure and along with respiratory hold when entering the trachea intraoperatively. On the wards, there was limited resident prerounding on COVID positive patients and exams conducted by attendings only when appropriate to limit exposure as well as PPE usage. Regarding accessibility of COVID-19 testing, the institution adopted a screening pathway based on symptoms and exposure risk.
Residents highlighted psychological health as a major concern driven by the uncertain outcome of the pandemic and limited therapeutic options. Several virtual townhalls were scheduled to provide updates on institutional guidelines and viable therapies as supporting evidence became more available. To combat the mental stress, psychological health resources allowing for either group or individual activities were shared with residents. These include daily mindfulness pauses, access to chaplains and other trained mental health professionals, weekly “check-ins” with program leadership, and other resources for stress management. These resources remain available to all residents as the psychological impact of the COVID-19 pandemic may persist for some (Table 1).
Clinical Experience
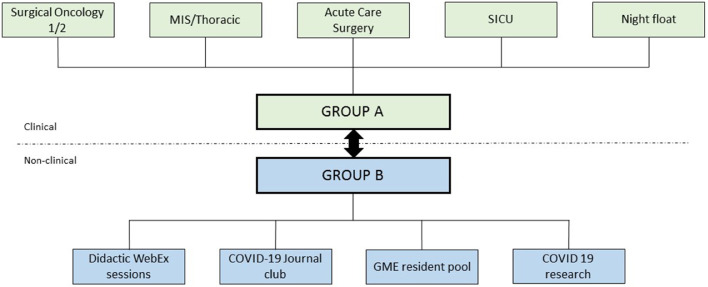
To provide uninterrupted quality care to patients while limiting resident exposure, we modified surgical services and resident case coverage. HMH residents complete certain subspecialty rotations at other training programs in the Texas Medical Center and rotate at satellite HMH campuses for their community experience. Of 31 residents in the program, 10 who were participating in external rotations were maintained at their locations to limit interruptions in education and patient care. Residents at satellite locations were pulled to the main campus resulting in a cohort of 21 available residents. They were divided into Groups A and B which would alternate in 14-day blocks with one group covering surgical cases and inpatient responsibilities while the other group was off clinical duties at home (Fig. 1 ). The 14-day block allowed for an appropriate quarantine period should an exposure or illness occur. With the reduction in elective caseload, surgical services were combined into fewer services, allowing for a decrease in the typical resident complement. The acute care surgery service was anticipated to have a consistent caseload and remained separate with the most residents assigned.
Figure 1.
Resident deployment in clinical and nonclinical duties during COVID-19 pandemic. MIS, minimally invasive surgery; SICU, surgical intensive care unit; GME, graduate medical education.
There was a coordinated multidisciplinary response including the surgery and medicine departments, ICU directors and the GME to determine appropriate deployment of trainees to primarily COVID-19 settings such as the ICU. As the volume of COVID-19 patients at our hospital was not at peak capacity, the institution requested resident volunteers for this purpose. Five residents volunteered to work alongside critical care-trained surgical staff and learn the complexities of COVID-19 patient management, which was beneficial especially for those interested in a surgical critical care career. In preparation for peak capacity, the institution created a trainee registry including documentation of personal risk and procedural skill level to guide resident deployment. ICU patient volume was monitored daily by the ICU directors who coordinated resident deployment with the program director. Fortunately, we did not reach peak capacity at our hospital and resident involvement in COVID-19 ICUs remained voluntary.
Prior to implementation of the modified schedule, 2 in-house residents and 1 externally rotating resident tested positive for COVID-19. They were removed from clinical duties for a period of isolation and recovery. They recovered and returned to work symptom free after a 14-day period of isolation and 2 negative COVID-19 tests >24 hours apart. After the modification of the schedule, no further residents tested positive for COVID-19. While there was discussion between HMH and external site program directors on resident responsibilities and PPE access, a protocol for work-related exposure and testing was less defined. We concluded that ultimately, the home institution is responsible for testing and follow-up.
Didactics
With the decrease in operative volume and clinical duties, we shifted our educational focus to an intensive didactic schedule. In addition to maintaining our usual protected educational time for all residents every Wednesday morning, we hold daily hour-long didactics on a Cisco WebEx video conferencing platform, followed by oral boards-style questions, required for all nonclinical residents and encouraged for those in-house. Sessions are led by residents in the back-up resident pool and proctored by surgical faculty experts in corresponding fields and were recorded for future access. Topics are based on our previous weekly curriculum combined with the Surgical Council on Resident Education (SCORE) curriculum, “This Week In Score” (TWIS).9 Based on compiled 2020 ABSITE score reports, we also identified topics where program scores were lowest and dedicated weekly sessions to these areas. Of the 21 residents available, 14 to 15 residents participated in the virtual curriculum daily including in-house residents as clinical volume allowed. The curriculum was well received by residents both in terms of the content and flexibility of the virtual platform with means for future access. In addition, via the chat function, the speaker and other participants could address all questions and comments in a controlled fashion. Furthermore, multiple experienced faculty could attend each session with limited disruption in their clinical duties resulting in engaging discussions on different approaches to patient management.
It was critical that we remained knowledgeable about the evolving treatment strategies for COVID-19 management. We incorporated a weekly “COVID-19 Journal Club” to discuss the latest academic literature with our intensive care staff caring for COVID-19 patients. Residents also participated in COVID-19-related research opportunities within the department.
Lessons Learned
The COVID-19 pandemic has impacted all aspects of healthcare delivery and the resolution remains uncertain without a proven cure or a vaccine.2 , 4 , 5 , 10 The disruption in traditional clinical pathways and reduction in surgical case volume has prompted discussion about the optimal response to ensure resident safety and maintain quality surgical education.7 , 11 , 12
Clear and transparent communication with all team members is central to any crisis response plan even when the crisis is not well understood.13 As residents are the first-line responders on most surgical services, we included them early in pertinent administrative discussions. This allowed a targeted response to resident concerns and also provides the opportunity to learn the fundamentals of crisis leadership which will be useful in their careers. PPE availability and supply, the greatest concern to residents, has remained adequate, while being utilized according to current Center for Disease Control guidelines.8 Almost a third of our residents participate in external rotations which represents a unique challenge. Communication between our program director, external site program directors and department chairs was undertaken early and regularly to collaborate on PPE standards as those evolved. COVID-19 testing criteria was also standardized to ensure testing was accessible to all residents. While ensuring physical safety with these measures, resident wellness and efforts to combat psychological distress were essential elements of our strategy. The emotional toll of the pandemic caused by multiple stressors can strain the already challenging residency experience of surgical trainees. The psychological health resources remain available for residents to access at their convenience. We expanded didactic sessions using a flexible teleconferencing platform which improved faculty turnout and permitted remote access that was more amenable to clinical demands. Utilizing technology to enhance surgical education in innovative ways should be embraced by all surgical educators. For instance, remote learning access has been extended to active learning communities developed on social media platforms.14 To better understand this novel disease, and we highlighted critical COVID-19 literature in dedicated journal clubs. Pairing relevant literature review with hands on experience will provide invaluable experience with a disease that may persist beyond the initial phase.
Despite the proactive and comprehensive modification of our surgical training program, challenges remain. Given the highly procedural nature of surgical training, technical skill acquisition, retention, and refinement needs to be addressed. Furthermore, this degree of rotation modification impacts resident evaluation given limited interactions with faculty. How many clinical encounters is a reasonable basis for staff to evaluate residents on all ACGME core competencies? Trainee evaluation will need to be adapted and educational opportunities for operative encounters maximized. Simulation has traditionally supplemented intraoperative exposure, however its use during this crisis proves challenging. In-person simulation as previously performed is no longer feasible while animal or cadaveric models are resource intensive and difficult to execute with PPE shortages. Programs may provide low-fidelity box-trainers for each resident while investigating remote virtual reality training with the potential of providing opportunity for assessment and feedback.15 , 16 Another way to engage residents is the virtual delivery of healthcare. Telemedicine has been hindered by regulation and limited payment structure but currently, most outpatient healthcare has transitioned to telehealth interactions as recommended by the Center for Disease Control.1 , 17 It is likely the widespread use of telehealth will persist and programs may need to consider formal resident training in telehealth use.18 The ACGME supports this shift by accelerating implementation of the Common Program Requirements for supervision of telemedicine visits by trainees.7
The long-term impact of the COVID-19 pandemic on surgical education and trainee preparedness for independent practice remains to be seen. This supports stronger consideration of competency-based rather than volume-based evaluation of trainees and efforts to accelerate its research and validation. While online educational resources geared towards trainees during this crisis are available, individual programs will need to tailor their response to the unique influence on their hospital and clinical experience. Success may be achieved with commitment to constant needs assessment in the changing landscape of healthcare with the goal of producing a skilled surgical workforce.
Author Agreement
All authors have seen and approved the final version of the manuscript being submitted.
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Centers for Disease Control and Prevention. Implementation of mitigation strategies for communities with local COVID-19 transmission. Centers for Disease Control and Prevention; March 12, 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/downloads/community-mitigation-strategy.pdf. Accessed April 2, 2020.
- 2.Centers for Disease Control and Prevention. Interim guidance for healthcare facilities: preparing for community transmission of COVID-19 in the United States. February 29, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhealthcare-facilities%2Fguidance-hcf.html. Accessed April 3, 2020.
- 3.Holshue M.L., DeBolt C., Lindquist S. First case of 2019 novel coronavirus in the United States. New Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American College of Surgeons. COVID-19: guidance for triage of non-emergent surgical procedures. March 17, 2020. Available at: https://www.facs.org/covid-19/clinical-guidance/triage. Accessed April 4, 2020.
- 5.American College of Surgeons. COVID-19: recommendations for management of elective surgical procedures. March 13, 2020. Available at: https://www.facs.org/covid-19/clinical-guidance/elective-surgery. Accessed April 2, 2020.
- 6.Society of Surgical Oncology. COVID 19 resources. April 6, 2020. Available at: https://www.surgonc.org/resources/covid-19-resources/. Accessed April 8, 2020.
- 7.Accreditation Council for Graduate Medical Education. “ACGME response to coronavirus (COVID19)". Last Updated, March 18, 2020. Available at: https://acgme.org/Newsroom/NewsroomDetails/ArticleID/10111/ACGME-Response-to-the-Coronavirus-COVID-19. Accessed April 4, 2020.
- 8.Centers for Disease Control and Prevention. Strategies to optimize the supply of PPE and equipment. April 3, 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/index.html. Accessed April 5, 2020.
- 9.Joshi A.R.T., Klingensmith M.E., Malangoni M.A. “Best practice for implementation of the SCORE portal in general surgery residency training programs. J Surg Educ. 2018;75:e11–e16. doi: 10.1016/j.jsurg.2018.04.014. Nov. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID‐19). February 27, 2020. Available at: https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf. Accessed April 4, 2020.
- 11.Daoudu O., Panda N., Lopushinsky S., Varghese T.K., Brindle M.. COVID-19 – Considerations and implications for surgical learners. March 24, 2020. Available at: https://journals.lww.com/annalsofsurgery/Documents/COVID-19%20%E2%80%93%20Considerations %20and%20Implications%20for%20Surgical% 20Learners.pdf. Accessed April 4, 2020. [DOI] [PubMed]
- 12.Nassar A.H., Zern N.K., M L.K. Emergency restructuring of a general surgery residency program during the coronavirus disease 2019 pandemicthe University of Washington Experience. JAMA Surg. 2020 doi: 10.1001/jamasurg.2020.1219. Published online April 6. [DOI] [PubMed] [Google Scholar]
- 13.Argenti P.A.. Communicating through the Coronavirus Crisis. Harvard Business Rev. 2020 https://hbr.org/2020/03/communicating-through-the-coronavirus-crisis March 13Available at. Accessed April 8, 2020. [Google Scholar]
- 14.Chick R.C., Clifton G.T., Peace K.M. Using technology to maintain the education of residents during the COVID-19 pandemic [published online ahead of print, 2020 Apr 3] J Surg Educ. 2020 doi: 10.1016/j.jsurg.2020.03.018. S1931-7204(20)30084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sroka G., Feldman L S., Vassiliou M C., Kaneva P A., Fayez R., Fried G M. Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg. 2010;199:115–120. doi: 10.1016/j.amjsurg.2009.07.035. [DOI] [PubMed] [Google Scholar]
- 16.Gurusamy K.S., Aggarwal R., Palanivelu L., Davidson B.R. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD006575.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Keesara S., Jonas A., Schulman K.. Covid-19 and health care's digital revolution. April 2, 2020. DOI: 10.1056/NEJMp2005835. [DOI] [PubMed]
- 18.Nikolian V.C., Williams A.M., Jacobs B.N. Pilot study to evaluate the safety, feasibility, and financial implications of a postoperative telemedicine program. Ann Surg. 2018;268:700–707. doi: 10.1097/SLA.0000000000002931. [DOI] [PubMed] [Google Scholar]