SUMMARY
Background
Patients with progressive chronic kidney disease face a series of treatment decisions that will impact the quality of life of themselves and their family. Renal replacement therapy option education (RRTOE), generally provided by nurses, is recommended by international guidelines
Objectives
To provide nurses with advice and guidance on running RRTOE.
Design
A consensus conference.
Participants
Four nurses, 5 nephrologists and 1 clinical psychologist (9 renal units; 6 European countries) from units that had extensive experience in RRTOE or were performing research in this field.
Approach
Experts brainstormed and discussed quality standards for the education team, processes, content/topics, media/material/funding and quality measurements for RRTOE.
Results
Conclusions and recommendations from these discussions that are particularly pertinent to nurses are presented in this paper.
Conclusions
Through careful planning and smooth interdisciplinary cooperation, it is possible to implement an education and support programme that helps patients choose a form of RRT that is most suited to their needs. This may result in benefits in quality of life and clinical outcomes.
Application to Practice
There are large differences between renal units in terms of resources available and the demographics of the catchment area. Therefore, nurses should carefully consider how best to adapt the advice offered here to their own situation. Throughout this process, it is crucial to keep in mind the ultimate goal – providing patients with the knowledge and skill to make a modality choice that will enhance their quality of life to the greatest degree.
Keywords: End‐stage kidney disease, renal replacement therapy, education, predialysis
INTRODUCTION
The majority of patients with progressive chronic kidney disease (CKD) will be presented with several important choices regarding their treatment. The decisions they take may impact quality of life more than clinical outcome. Therefore, patient involvement in the decision‐making process is crucial to satisfaction and adherence to treatment. To prepare patients to make these decisions, European (Covic et al. 2010) and American (Saggi et al. 2012) guidelines recommend that renal replacement therapy option education (RRTOE) is provided.
The objective of RRTOE is to support all patients who are likely to progress to end‐stage kidney disease to make an optimal choice on treatment modality in good time, by providing unbiased information in a clear and engaging way. An additional objective is to ensure that patients with end‐of‐life care needs are suitably prepared.
RRTOE should provide well‐balanced information on all possible therapies (Covic et al. 2010). If a modality is contraindicated, the reasons for this should be explained.
Studies have shown that the benefits of RRTOE include reduced urgent dialysis starts (Levin et al. 1997); earlier placement of permanent vascular access (Lindberg et al. 2005); a greater likelihood of choosing a self‐care modality (Manns et al. 2005); extended time to requiring dialysis (Devins et al. 2003); improved adherence (Tourette‐Turgis and Isnard‐Bagnis 2013); and reduced mortality (Wu et al. 2009).
However, in general clinical practice, there is only moderate patient satisfaction with RRTOE (Pastor and Julián, 2010; Fadem et al. 2011). This seems to result from the above‐mentioned objectives of RRTOE not being achieved. Specifically, either information is not presented in a way that engages or motivates the patient (Tourette‐Turgis and Isnard‐Bagnis 2013; Lee et al. 2008) or the patient does not feel that they have an active choice of modality (Winterbottom et al. 2012a). This may result from a lack of clear, practical guidance in the literature on how best to ensure and provide high‐quality RRTOE.
To help address this need, the current authors composed a consensus statement intended to give more detailed and practical guidance to health care practitioners (HCPs) on how to approach every stage of RRTOE (Isnard Bagnis et al. 2014). The purpose of the current paper is to tailor this guidance to nurses and to provide advice on how to individualise RRTOE according to best practices. We provide clear example of education team structures and the processes by which RRTOE can be effectively delivered. Sound advice on how to navigate the sometimes‐overwhelming abundance of materials and resources available is offered.
ROLE OF THE NURSE IN A MULTIDISCIPLINARY EDUCATIONAL TEAM
MULTIDISCIPLINARY EDUCATIONAL TEAM
The core members of the RRTOE team are the nurse and nephrologist (Da Silva‐Gane et al. 2002; Prieto‐Velasco et al. 2014), although the nurse is generally the key contact point for the patient. This core team is supported by other HCPs (Figure 1) (National Institutes of Health 1994). The disciplines of the other HCPs are not specified in the current guidelines, although they recommend that teams are multidisciplinary (Renal Association 2009; Saggi et al. 2012; Haute Autorité de Santé 2007). There is some limited evidence to suggest that education from multidisciplinary teams (versus care from a nephrologist(s) alone) may be advantageous in terms of clinical parameters and survival (Bastos and Kirsztajn 2011). Therefore, meetings with team members other than the nurse and nephrologist should be offered to the patient.
Figure 1.
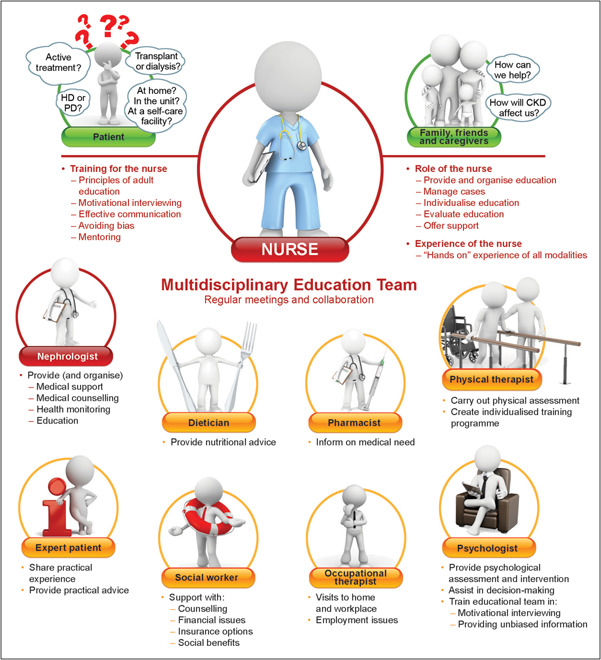
Role of the nurse in a multidisciplinary educational team.
Some units assign each patient to a contact person, whilst in other units the whole educational group acts as the contact. Regardless of set‐up, regular team meetings to discuss each patient's progress are essential.
ROLE OF THE NURSE
The role of the nurse varies greatly within and between countries. However, in renal units offering time‐intensive education on treatment choice, it can be expected that the nurse will play a very large role. This may be as organiser and provider of RRTOE, case manager or both.
Time out activity.
Is your role in RRTOE clearly defined? Do you know exactly what is expected of you from your manager, peers and patients?
NURSE AS THE KEY PROVIDER AND ORGANISER OF RRTOE
Whilst there are no comprehensive data, studies in Australia (Fortnum [Link]) and Europe (Prieto‐Velasco et al. 2014) indicate that a high proportion of education is provided by a nurse, as nephrologists have limited time for one‐on‐one education. This allows nurses an understanding of the patient's needs for education and psychosocial and economic issues that affect their ability to adhere to treatment plans. Patients consider nephrology nurses or nurse practitioners to be the most important caregivers to address their problems and concerns (Lewis et al. 2010).
The key tasks of the nurse are to decrease the complexity surrounding dialysis, to inform the patients about all treatment options and to help them make a modality choice.
NURSE AS THE CASE MANAGER
In some units, an additional role of the nurse may be to act as ‘case manager’. The key responsibilities of a case manager are scheduling appointments with the patient, obtaining a medical history, assessing needs of the patient/family, providing and evaluating educational sessions and communicating with other members of the education team and the patient's general practitioner (GP) (Provincial PD Coordinating Committee 2006).Essentially, nurses are given greater responsibility for individual patients (cases), and act as the key contact and care coordinator for their own cases.
TRAINING AND EXPERIENCE REQUIRED FOR THE NURSE
European (Covic et al. 2010) and American (Saggi et al. 2012) guidelines offer no recommendations for minimal levels of training or experience. However, as the guidelines stress that information presented to the patient should be ‘unbiased’, it may be inferred that nurses should have substantial experience of all available treatment modalities. Some centres compensate for any potential bias from a single nurse by ensuring that the patient has contact with several nurses working with different modalities.
Whilst training in topics such as education and communication is not mandatory for nurses, it should nevertheless be considered as extremely valuable. Long‐term experience with the treatment modalities does not guarantee that the nurse is skilled in the sensitive communication required when delivering RRTOE.
In the authors' experience, there are several useful areas for training, which are listed below. Sometimes this training can be arranged and funded internally, but in some units nurses organise this themselves to further their professional development.
Time out activity.
Did you identify any gap between what is expected of you in your role as patient educator and your current skill set or knowledge? What training would help you bridge this gap?
PRINCIPLES OF ADULT (OR PATIENT) EDUCATION
To the best of our knowledge, France is the only country in Europe to make training in patient education mandatory for HCPs involved in this field (Haute Autorité de Santé 2007). This guideline is applicable to all forms of patient education. There are many courses on adult/patient education available. A key consideration when choosing a course is whether RRTOE is generally delivered on a one‐to‐one basis or in a classroom format (see 3.3). The key skill to take from such training is to distinguish between ‘teaching’ and ‘learning’. The aim of RRTOE should not be to ‘teach’, but that the patient ‘learns’. Thus, the patient's understanding of the material covered should be checked regularly.
COMMUNICATION SKILLS
In general, sensitive and tactful communication is essential when providing education to patients. In RRTOE, the educator may have to give unwelcome news to the patient or discuss upsetting topics such as end‐of‐life care needs. Training to deal with such situations can be very helpful. Such training would ideally be provided by someone trained in renal psychology; however, such training providers are not easily accessible across Europe. Nevertheless, it is important to have such training tailored to fit the particular challenges of dealing with renal patients and their unique concerns.
MOTIVATIONAL INTERVIEWING
Motivational interviewing is a style of counselling that aims to engage the intrinsic motivation of the patient to change behaviour. In this context, it may help change behaviours that encourage indecisiveness or procrastination. In the clinical setting, motivational interviewing has been shown to outperform traditional advice giving in the treatment of a broad range of behavioural problems and diseases (Lundahl and Burke 2009; Rubak et al. 2005).
AVOIDING BIAS WHEN GIVING INFORMATION
To provide well‐balanced, unbiased information to the patient, the educator should avoid giving personal views or recommendations. In practice, this can be challenging – particularly if the patient insists on hearing the educator's opinion. Two useful tools are appropriate training and patient decision aids (PDAs).
Training in motivational interviewing or communications skills (see above) may incorporate skills on how to avoid inducing bias. However, any further training in client‐centred counselling may also help.
PDAs refer to materials specifically designed to support patients in making decisions about screening, treatment or other interventions. These come in a variety of formats, and are described in more detail in section 4.2.
MENTORING
Several of the authors' units use a mentoring scheme in which the more experienced nurses train and assist the new members to the team.
ROLE OF THE EDUCATION TEAM IN THE CARE OF THE PATIENT
An important question is whether or not the education team should be dedicated purely to providing RRTOE and have no role in the subsequent care of the patient.
A team that is only responsible for education (and not for subsequent care) may be more neutral concerning the patient's treatment choice. This model also removes the possibility of the patient choosing a particular modality simply because it would allow them to continue seeing the same HCPs who provided their education.
However, there are potential drawbacks to such an approach. It is possible that the benefits of a neutral education team may be offset by the subsequent stress of having an entirely new team of HCPs. Also, a combined education/care team should be able to present information in a neutral way – particularly if they have experience of all modalities and utilise tools such as PDAs (see Choosing materials & resources).
For units that promote self‐care treatment (whether haemodialysis (HD) or peritoneal dialysis (PD)), having an education team comprising only of HCPs working in self‐care may increase the number of patients choosing and receiving a self‐care modality. One author's unit uses such an approach, and the same team is also responsible for erythropoietin administrations and intravenous iron infusions, which provide further opportunities to discuss with the patient. This has been found to contribute to a high rate of patients (73%) who began treatment with the self‐care modality they originally selected (Goovaerts et al. 2012).
KEY PROCESSES TO ENSURE HIGH‐QUALITY RRTOE
An overview of the key processes is presented in Figure 2.
Figure 2.
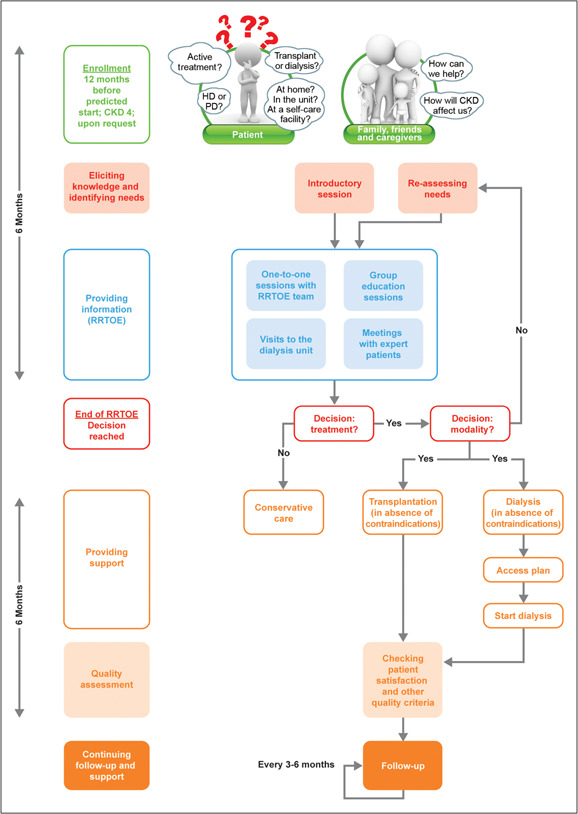
Key processes to ensure high‐quality RRTOE.
ENROLMENT
In the authors' units, enrolment into RRTOE generally takes place at stage 4 CKD (15–29 mls/min/1.73m2) or 12 months before the predicted start of dialysis. This is in line with US guidelines (9–12 months before predicted dialysis start (Saggi et al. 2012)).
The aim is to offer RRTOE to all these patients, with their family or caregiver if desired. If the patient requests RRTOE at an earlier stage, it could be made available – particularly considering the benefits of early referral (Goovaerts et al. 2005; Owen et al. 2006).
ELICITING KNOWLEDGE & IDENTIFYING NEEDS
The educator may be tempted to systematically work through a list of pre‐prepared topics during a meeting with the patient. However, it is important to find out (elicit) the patient's knowledge of RRT options and their current concerns. The topics covered in that meeting and the materials used can then be adjusted to best address the patient's main concerns and fully engage them.
It is possible that the patient begins RRTOE with no interest in being an active part of the decision‐making process, and transfers responsibility to the nurse or nephrologist. In such cases, highlighting the consequences of this decision (or lack of) may help the patient realise the benefits of active participation. Providing time and space for the patient to work through this choice is crucial. If encouragement and time are not effective, the patient may benefit from contact with other patients (expert patients, group sessions, patient associations). Referral to a psychologist may assist the patient in overcoming their apathy or reluctance to participate in treatment.
The patient actually has to make a series of related decisions before deciding on a treatment modality (Golper and Schreiber 2012):
Should I have active treatment or opt for conservative care?
Should I have dialysis and/or a (pre‐emptive) transplant?
Should I have dialysis at home, at a self‐care facility or in the unit?
Should I have HD or PD?
What type of HD (standard, nocturnal, short frequent) or PD (continuous ambulatory PD (CAPD), automated PD (APD)) should I have?
To avoid providing information that addresses a question which the patient is not currently dealing with, the educator can use the “elicit, provide, elicit” model of information exchange – in other words, find out what the patients already know before providing new information, then find out what they have learnt (see Motivational interviewing and Avoiding bias when giving information). Motivational interviewing and good communication, in general, is based on this model.
This process of elicitation can help determine not only what information should be provided, but also the most effective form for this particular patient (e.g. booklet or website) (see Choosing materials & resources).
In France, an initial interview to assess patient needs is actually mandatory before education (Ayav et al. 2013); however, a brief re‐assessment should take place at the beginning of every session. Such assessments can also help the educator take account of the patient's general condition, age, comorbidities, potential problems with memory and/or cognitive impairment, disease progression rate, disease stage, willingness to take an active role in treatment and their desire for RRT.
Another key purpose of the initial interview is to stress to patients that the purpose of these sessions is to assist them in making an active decision on treatment. In the absence of contraindications, it is their right to decide upon an active treatment (or lack of) (Concern for the Dying 1983). This point should be repeated.
Time out activity.
Do you (1): actively identify the patient's current concerns/knowledge gaps before giving information? or (2) provide all available information in a pre‐defined order and allow the patient to decide what is relevant?
PROVIDING INFORMATION (RRTOE)
ONE‐TO‐ONE SESSIONS
The number of one‐to‐one sessions required for the patient to reach a decision on treatment may vary substantially. Careful assessment of the patient's needs and background knowledge, as described above, will help ensure that the optimum number of sessions is provided.
All authors report a large variation in the number of sessions required for RRTOE; however the 3–6 sessions recommended in the US guidelines (Saggi et al. 2012) is considered reasonable considering the large amount of information patients are faced with. French guidelines (applicable to patient education across therapeutic areas) recommend 2–3 sessions per year (Haute Autorité de Santé 2007).
There is no standard period between RRTOE sessions. However, if education begins 12 months before the predicted start of dialysis and a treatment decision is expected around 6 months before the start, this leaves 6 months for RRTOE. With the recommended 3–6 sessions, this would translate into monthly or two‐monthly sessions. In practice, however, these sessions could take place over a single weekend, especially if the patients need to travel far.
GROUP SESSIONS
There is a wide variety amongst authors in the utilisation of group education sessions. Some of the authors' units offer no group sessions, and others offer group sessions to all patients. Such sessions can be led by expert patients (see Meetings with expert patients). Group sessions with other patients may offer levels of companionship and understanding that the educator cannot provide. Moreover, other patients can offer advice on the day‐to‐day practicalities of living with CKD. However, there are some challenges, such as (1) logistical difficulties (e.g. finding a suitable time/place); (2) the risk of a naive patient relying too heavily on the group's conclusions (or those of a dominant participant), particularly as these could be misleading or incorrect; and (3) the lack of a common language/culture creating obstacles to clear communication in ethnically diverse areas (see Optimising education for culturally and linguistically diverse (CALD) populations).
VISITS TO THE DIALYSIS UNIT
Visits to the HD and PD units are generally offered to each patient. Such visits can be helpful, but may also be disturbing for the patient – particularly for units based in or near an emergency department. Therefore, some preparation before the visit, such as discussing what they will see there, may be helpful.
MEETINGS WITH EXPERT PATIENTS
Expert patients are defined as people living with a long‐term health condition who are able to take more control over their health by understanding and managing their conditions, leading to an improved quality of life. Meeting expert patients or attending expert‐patient‐led courses is always the choice of the patients themselves.
Patients have a great influence upon other patients' choice of treatment (Winterbottom et al. 2012b). Depending upon the skill, neutrality and knowledge of the expert patient, they may produce a large beneficial or negative effect. Hence, there is a wide range of views and opinions on the extent of their role in RRTOE. Some of the authors' units do not arrange meetings with expert patients, some train expert patients before allowing them to meet other patients and other units arrange meetings with several expert patients using different modalities.
CONTACT WITH THE GP
Close collaboration with the patient's GP should be sought (Tourette‐Turgis and Isnard‐Bagnis 2013). One author's unit posts update letters to the GP after each session. Ideally, the dialogue should be a two‐way process, as patients may also provide information to the GP that they have not given to the education team, and vice versa.
Maintaining contact with the GP is generally a task of the nephrologist or nurse case manager. Regular team meetings are important to ensure all HCPs are up‐to‐date with the patient's progress and condition.
LOCATION OF RRTOE
Ideally, RRTOE could take place in the location of the patient's choosing. However, considering limited resources, this is not practical.
Most of the authors' units are not in a position to offer home visits. One unit, however, does provide home visits by the CKD nurse if it is difficult for the patient to come to the unit. Another unit always conducts the first RRTOE session at the patient's home. This allows an initial assessment of the patient's social situation and coping skills. Home visits also allow an evaluation of the possibility of home treatment.
One unit offers a 2‐day group education session at an off‐site facility. Both expert patients and HCPs contribute. Meals and evenings are spent together in an informal atmosphere.
For frail patients who cannot make many trips to the hospital, it may be necessary to use these trips for blood tests, etc. and to have RRTOE conducted at home. In such cases, involvement of the family or caregiver is crucial.
Time out activity.
In the context of available resources and demographics, what is the optimal structure for RRTOE at your own renal unit?
PROVIDING SUPPORT
RRTOE should last for as long as required. Ideally, RRTOE ends when a decision on treatment (or lack of) is reached and the treatment has begun. However, contact between the RRTOE team and the patient should be maintained, so the team can offer support and engage in follow‐up (see Continuing follow‐up and support).
CHECKING PATIENT SATISFACTION AND OTHER QUALITY CRITERIA
After RRTOE finishes, the initial follow‐up is an opportunity to assess patient satisfaction with the education they received, whether they would have liked anything to have been done differently, and any other relevant quality assurance measures (e.g. level of patient involvement with RRTOE).
CONTINUING FOLLOW‐UP AND SUPPORT
Regular follow‐ups to ensure that the patient is still satisfied with his or her treatment choice are essential. Changes in life circumstances may cause the patient to re‐evaluate their decision. Repeating RRTOE may be useful for some patients.
INDIVIDUALISING RRTOE
Individualised RRTOE refers to an adaption of a standard process, format or piece of material in order to meet a patient's needs or wishes. Ideally, all patients should receive individualised RRTOE. The patient's learning style, preferences, concerns, comorbidities as well as work, social and family situations should be taken into account. Of the education team, nurses are generally best placed to identify such factors. Eliciting such information from the patient during the introductory session is vital.
The processes of RRTOE described in the previous section may require significant changes due to factors outside of the educator's control (e.g. crash landers, rate of disease progression and complications). However, the educator does have direct control over the structuring of content and the use of materials and resources. Skilful choices on what or who to present to the patient and when to present are the key to success. This includes, for example, recognising that a patient may not be comfortable with using the internet and thus providing suitable booklets instead of recommending websites.
It is important to note that materials (e.g. a booklet or DVD) cannot be individualised. Instead, individualisation comes from how the educator engages with the materials. The educator should not simply provide a piece of material or a resource, but also gauge the patient's response. For example, some patients may understand a booklet while others may have difficulty with the same booklet; likewise patients may respond well to expert patients and others not.
STRUCTURING THE CONTENT
Whilst there is no standard curriculum for RRTOE, the authors' programmes contain very similar topics. Broadly, the topics addressed include a description of the disease and the treatment options, ways of managing the disease and practical suggestions (from transport to advanced health care directives) (Isnard Bagnis et al. 2014; Da Silva‐Gane et al. 2002).
There are suggestions in the literature on how best to deliver this content according to disease stage (CKD stages 2–5) (Bates 2012; Wu et al. 2009; Kidney Health Australia 2012). However, in the authors' experience, patients are generally referred for RRTOE at CKD stage 4 (progressive). Therefore, the breakdown of content by stage is not practical. Figure 3 presents a possible content checklist to be used by the educator at each RRTOE session. In this figure, content is ordered according to whether or not the patient has made a decision on treatment. This is a guide to help educators ensure they have covered the basic topics. Patient concerns and wishes should be the primary criteria to determine which topics will be covered in the session.
Figure 3.
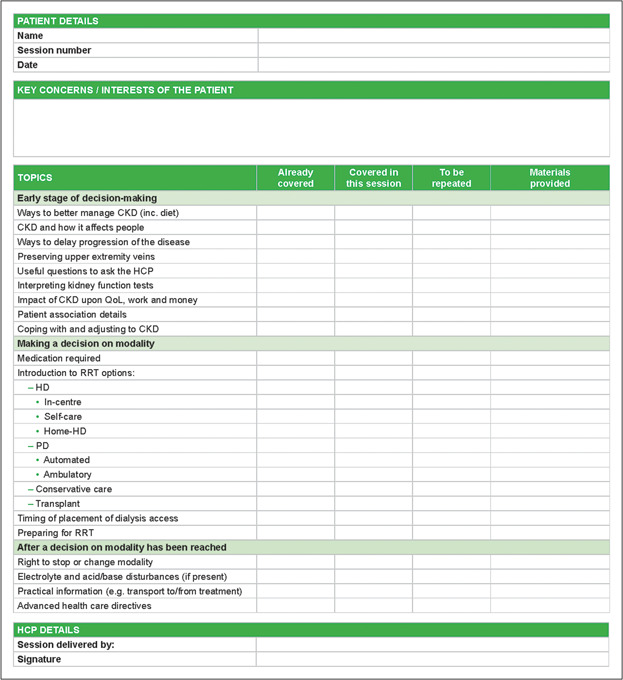
Individualising RRTOE: Structuring the content.
CHOOSING MATERIALS & RESOURCES
Materials (such as booklets and videos) and resources (such as expert patients) should support the educator in providing ‘well‐balanced’ information. The educator has a huge variety of materials and resources that he or she can draw upon (Figure 4). This allows important information to be presented to patients in several forms, which may help them to remember the key points.
Figure 4.
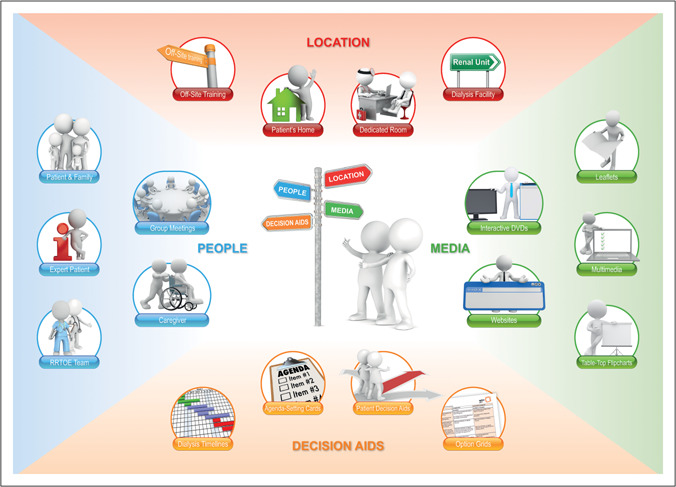
Individualising RRTOE: Choosing resources & materials.
However, the huge variety of subtypes of materials and resources leads to a lack of standardisation and problems with ensuring quality. For example, a UK study found that of 32 renal units, 31 were using different leaflets in RRTOE (Winterbottom et al. 2007), and 90% of leaflets were scored as difficult to read. This can lead to confusion for the patient and/or unintentional bias.
Even high‐quality content presented in a format that is unsuitable for the patient (e.g. small font, technical expertise necessary) or at a time when the patient is not ready to receive this information (e.g. end‐of‐life care needs) can also produce confusion or bias.
Time out activity.
How were the materials and resources for RRTOE chosen at your unit? Do the patients engage well with these materials? Do patients frequently request another form of materials (e.g. DVD, booklets in large print or with diagrams)?
Therefore, when choosing materials and resources to use, it is the responsibility of the educator to (1) assess their quality; (2) assess their suitability for the patient; and (3) decide upon a suitable time in the RRTOE to introduce them.
When assessing the quality and suitability of a material/resource the educator should consider:
Will I feel comfortable using it?
Will it enhance the understanding of disease and treatment?
Will it present the consequences of the patient's decision?
Will it encourage the patient to use their own reasoning?
Will it help the patient to develop realistic expectations?
Will it supplement rather than replace the information provided by the educator?
A high‐quality PDA should provoke a positive response to each of the six questions above. PDAs are used when there is more than one reasonable therapy option available and patient preferences and values have a large impact on choice. These may be booklets, videos or web‐based tools. A recent Cochrane review concluded that use of PDAs is often linked to greater patient participation and making treatment choices that are aligned with underlying values (Stacey et al. 2011). PDAs should meet the criteria laid out by the International Patient Decision Aid Standards (IPDAS) Collaboration (http://ipdas.ohri.ca).
Some resources may be more likely to induce bias – e.g. an expert patient who is particularly positive about a certain modality or a booklet describing just one modality. In such cases, the educator should use a range of materials and resources to minimise this effect.
Many units have developed their own materials. For example, one of the author's centres has developed an in‐house interactive DVD, which features interviews with real patients, frequently asked questions with HCPs and demonstrations of dialysis techniques. The DVD is used in conjunction with the information provided by the nurse, and a summary brochure is provided. IPDAS Collaboration criteria should be utilised when developing such materials.
OPTIMISING EDUCATION FOR CULTURALLY AND LINGUISTICALLY DIVERSE (CALD) POPULATIONS
CALD populations present a unique challenge to educators. Linguistic barriers present many problems for communication and possibilities for misunderstanding. Cultural and religious values may mean that the patient's priorities and expectations are profoundly different to those of the educator.
There is relatively little information available on how best to deal with RRTOE for CALD populations. Results from a focus group in Australia stated that HCPs recommend recruiting health workers from CALD communities to assist them to elicit and address the needs of RRTOE patients (Komaric et al. 2012).
Concerning language barriers, several of the authors' units use translators/interpreters, who can be reached via telephone or face‐to‐face. One unit relies upon other HCPs who can speak the patient's language. All units have some translation of the written materials, but may also rely upon family or friends of the patient to translate. Picture sets may be helpful during these sessions.
Concerning cultural and religious issues, the educator should be aware that the patient may have perceptions of health and disease, patient and doctor, doctor and nurse, etc. that are radically different from their own. There may also be obligations and beliefs concerning diet and/or treatment that could impact upon the patient's decision‐making. The role of the particular CALD community in support of its elderly members should also be considered.
A study conducted in one author's unit showed that patients who believed their adopted language was good enough for group education sessions (confirmed by the HCPs) did not perform well (Hagman and Nilsson 2013). Specifically, they had problems understanding the content, were afraid of being misunderstood and did not feel that they belonged to the group. As a result, international health advisors (IHAs) were added to the RRTOE team. IHAs are HCPs who qualified in the country of origin of the patient. These IHAs held the education sessions with CALD patients and the multidisciplinary team was an additional resource.
ASSESSING WHETHER THE OBJECTIVES OF RRTOE HAVE BEEN MET
Assessing the quality of RRTOE may only be carried out if the programme has clear objectives. Each of these objectives may then be assessed individually, using a wide variety of tools.
An overview of key objectives and assessment criteria is presented in Figure 5. Assessment criteria cover both the more objective service‐driven criteria (e.g. percentage of patients receiving RRTOE before treatment) and the more subjective patient‐related criteria (e.g. satisfaction with RRTOE). Currently, there is a lack of well‐evaluated tools for measuring many of these subjective criteria.
Time out activity.
Are there clear objectives for RRTOE at your unit? Are these objectives ranked in order of importance? Is the whole RRTOE team aligned on these objectives? How are the most important objectives assessed and how is this reported to the team?
Figure 5.
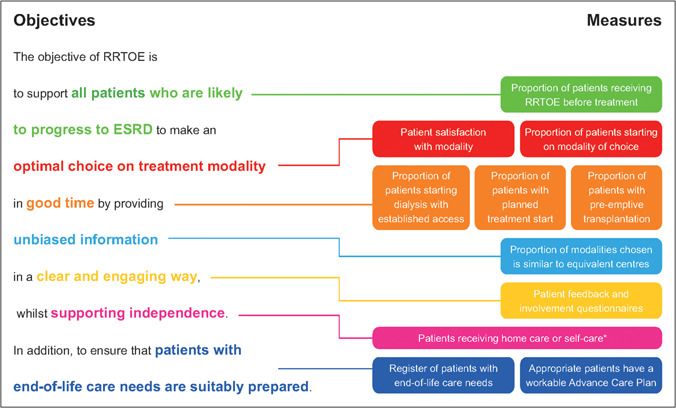
Assessing whether the objectives of RRTOE have been met. * This outcome is used by some of the authors. It may be compared against an internal target of the unit, a target recommended by external guidance (e.g. (All Party Parliamentary Kidney Group (UK), 2013)) or against the uptake of home/self‐care in similar renal units. However, other authors do not advocate the use of this measure as it could encourage the RRTOE team to recommend particular modalities rather than remain neutral.
CONCLUSION
Optimal RRTOE involves far more than simply providing the patient with information. Ideally, patients would enter a structured programme with a range of qualified HCPs in good time to allow them to reach an informed and unbiased modality choice. This programme should have enough flexibility to accommodate differences between patients' needs, expectations, concerns and learning styles, whilst still ensuring all relevant material is presented in an engaging way. Such a programme requires very careful planning, taking into account the resources and demographics of each renal unit. Continued quality assessment is crucial in ensuring that the aims and objectives of RRTOE are being met.
CONFLICT OF INTEREST
All authors have served as consultants to Baxter Healthcare Corporation. T.G. has served as a consultant to Gambro AB, Fresenius, and Amgen. A.M. is on the speaker list for Sanofi, BMS, MSD, Shire, Amgen and Pfizer. M.P.‐V. has advised, consulted or received speaker honoraria from Baxter, Fresenius, Gambro, Abbvie, Shire and Sanofi Renal.
AUTHOR CONTRIBUTIONS
This paper was written following a consensus meeting on 26 March 2013 in Zurich, Switzerland. The suggestions, views and experiences of authors presented at the meeting were compiled into a suggested outline of this paper by Archimed Medical Communication AG. Following approval of the outline, several drafts of the paper were written based on this outline. All authors were expected to thoroughly review and provide suggestions for improving each draft. This process of feedback and redrafting was repeated several times until all authors provided final approval.
All authors meet ICMJE criteria. All authors have:
Made substantial contributions to the conception or design of the work; or the acquisition, analysis or interpretation of data for the work; AND
Drafted the work or revised it critically for important intellectual content; AND
Given final approval of the version to be published; AND
Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
ACKNOWLEDGEMENTS
Archimed Medical Communication AG, Zofingen, Switzerland, provided medical writing support for the manuscript. Financial support for the medical writing was given by Baxter Healthcare Corporation, Zurich, Switzerland.
Biography
Tony Goovaerts is a nephrology nurse with managing qualifications and 40 years' experience in the field. He is the nurse manager of the Home Haemodialysis, the PD and the Pre‐treatment Counselling Programme, and of a self‐care haemodialysis satellite unit in Brussels, Belgium. He has been a Committee member of the EDTNA/ERCA President of the XX Annual EDTNA/ERCA Conference in Brussels, Belgium, was a co‐founder of the WFRC (World Foundation for Renal Care) and its Vice‐President from 1996 to 2002. Tony has given presentations at several international conferences and participated in many educational activities in developing countries.

Goovaerts T., Isnard Bagnis C., Crepaldi C., Dean J., Melander S., Mooney A., Prieto‐Velasco M., Trujillo C., Zambon R., Nilsson E‐L. (2014). Continuing education: preparing patients to choose a renal replacement therapy. Journal of Renal Care 41(1), 62–75.
REFERENCES
- All Party Parliamentary Kidney group (UK) . (2013). A Report of the Findings of the 2013 Home Dialysis Summit.
- Ayav C., Empereur F. & Kessler M. (2013). [Taking into consideration patient concerns for the elaboration of educational programs for chronic renal failure patients.] Néphrologie & Thérapeutique, E‐Pub ahead of print. [DOI] [PubMed] [Google Scholar]
- Bastos M.G. & Kirsztajn G.M. (2011). Chronic kidney disease: importance of early diagnosis, immediate referral and structured interdisciplinary approach to improve outcomes in patients not yet on dialysis. Jornal brasileiro de nefrologia 33, 93–108. [PubMed] [Google Scholar]
- Bates M. (2012). Improving kidney health and awareness through community based education. www.slideshare.net/Sammy17/ckd‐education (accessed 19 Nov 2013).
- Concern for the Dying . (1983). The right to refuse treatment: a model act. American Journal of Public Health 73, 918–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covic A., Bammens B., Lobbedez T. et al (2010). Educating end‐stage renal disease patients on dialysis modality selection. Nephrology, Dialysis, Transplantation Plus 3, 225–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Silva‐Gane M., Goovaerts T., Elseviers M.M. et al (2002). Information and counselling for patients approaching end‐stage renal failure in selected centres across Europe. EDTNA/ERCA journal (English ed.) 28, 49–55. [DOI] [PubMed] [Google Scholar]
- Devins G.M., Mendelssohn D.C., Barre P.E. et al (2003). Predialysis psychoeducational intervention and coping styles influence time to dialysis in chronic kidney disease. American Journal of Kidney Disease, 42, 693–703. [DOI] [PubMed] [Google Scholar]
- Fadem S.Z., Walker D.R., Abbott G. et al (2011). Satisfaction with renal replacement therapy and education: the American Association of Kidney Patients survey. Clinical Journal of the American Society of Nephrology 6, 605–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortnum D. Predialysis education ‐ A national Australian survey (Jan 2012). Kidney Health Australia. 2012. www.kidney.org.au.
- Golper T.A. & Schreiber M.J.J. (2012). The course of therapy: changing the paradigm In: Issues in Dialysis (ed Fadem S.). pp. 35–49. New York: Nova Science Publishers Inc. [Google Scholar]
- Goovaerts T., Jadoul M. & Goffin E. (2005). Influence of a pre‐dialysis education programme (PDEP) on the mode of renal replacement therapy. Nephrology Dialysis Transplantation, 20, 1842–1847. [DOI] [PubMed] [Google Scholar]
- Goovaerts T., Jadoul M. & Goffin E. (2012). Influence of a predialysis education program on the choice of renal replacement therapy. American Journal of Kidney Disease 60, 499; author reply 499–500. [DOI] [PubMed] [Google Scholar]
- Hagman P. & Nilsson E.‐L. (2013). Grupputbildning på modersmål möjligt med Internationella Hälsokommunikatörer. Dialäsen 3, 31–32. [Google Scholar]
- Haute Autorité De Santé . (2007). Structuration d'un programme d'éducation thérapeutique du patient dans le champ des maladies chroniques. http://www.has‐sante.fr/portail/upload/docs/application/pdf/etp_‐_guide_version_finale_2_pdf.pdf (accessed June 2013).
- Isnard Bagnis C., Crepaldi C., Dean J. et al (2014). Quality standards for predialysis education: results from a consensus conference. Nephrology Dialysis Transplantation In press [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kidney Health Australia . (2012). Treatment options‐teaching patients (including a summary of “Predialysis Education Survey”). http://homedialysis.org.au/health‐professional/educating‐patients/teaching‐patient‐options/.
- Komaric N., Bedford S. & Van Driel M.L. (2012). Two sides of the coin: patient and provider perceptions of health care delivery to patients from culturally and linguistically diverse backgrounds. BioMed Central Health Services Research 12, 322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A., Gudex C., Povlsen J.V. et al (2008). Patients' views regarding choice of dialysis modality. Nephrology Dialysis Transplantation 23, 3953–3959. [DOI] [PubMed] [Google Scholar]
- Levin A., Lewis M., Mortiboy P. et al (1997). Multidisciplinary predialysis programs: quantification and limitations of their impact on patient outcomes in two Canadian settings. American Journal of Kidney Disease 29, 533–540. [DOI] [PubMed] [Google Scholar]
- Lewis A.L., Stabler K.A. & Welch J.L. (2010). Perceived informational needs problems, or concerns among patients with stage 4 chronic kidney disease. Nephrology Nursing Journal 37, 143‐148; quiz 149. [PubMed] [Google Scholar]
- Lindberg J.S., Husserl F.E., Ross J.L. et al (2005). Impact of multidisciplinary, early renal education on vascular access placement. Nephrology News & Issues 19, 35–36, 41–43. [PubMed] [Google Scholar]
- Lundahl B. & Burke B.L. (2009). The effectiveness and applicability of motivational interviewing: a practice‐friendly review of four meta‐analyses. Journal of Clinical Psychology 65, 1232–1245. [DOI] [PubMed] [Google Scholar]
- Manns B.J., Taub K., Vanderstraeten C. et al (2005). The impact of education on chronic kidney disease patients' plans to initiate dialysis with self‐care dialysis: a randomized trial. Kidney International 68, 1777–1783. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health . (1994). Morbidity and mortality of renal dialysis: an NIH consensus conference statement. Consensus Development Conference Panel 121, 62–70. [DOI] [PubMed] [Google Scholar]
- Owen J.E., Walker R.J., Edgell L. et al (2006). Implementation of a pre‐dialysis clinical pathway for patients with chronic kidney disease. International Journal for Quality in Health Care 18, 145–151. [DOI] [PubMed] [Google Scholar]
- Pastor J.L. & Julián J.C. (2010). Claves del proceso de información y elección de modalidad de diálisis en pacientes con insuficiencia renal crónica. Nefrologia 1, 15–20. [Google Scholar]
- Prieto‐Velasco P., Isnard Bagnis C., Dean J. et al (2014). Predialysis Education in Practice: A Questionnaire Survey of Centres with Established Programmes. BMC Research Notes In submission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provincial Pd Coordinating Committee . Provincial Peritoneal Dialysis Joint Initiative, Resource Manual, Detailed Strategy On Increasing Peritoneal Dialysis (Pd) Use In Ontario. 2006.
- Renal Association . RA Guidelines ‐ Planning, initiating and withdrawal of renal replacement therapy. 2009. www.renal.org. [DOI] [PubMed]
- Rubak S., Sandbaek A., Lauritzen T. et al (2005). Motivational interviewing: a systematic review and meta‐analysis. The British Journal of General Practice 55, 305–312. [PMC free article] [PubMed] [Google Scholar]
- Saggi S.J., Allon M., Bernardini J. et al (2012). Considerations in the optimal preparation of patients for dialysis. Nature Reviews Nephrology 8, 381–389. [DOI] [PubMed] [Google Scholar]
- Stacey D., Bennett C.L., Barry M.J. et al (2011). Decision aids for people facing health treatment or screening decisions. The Cochrane Database of Systematic Reviews CD 001431. [DOI] [PubMed] [Google Scholar]
- Tourette‐Turgis C. & Isnard‐Bagnis C. (2013). [Patient education]. Néphrologie & thérapeutique 9, 235–240. [DOI] [PubMed] [Google Scholar]
- Winterbottom A., Bekker H.L., Conner M. et al (2012a). Choosing dialysis modality: decision making in a chronic illness context. Health Expectations E‐Pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winterbottom A., Conner M., Mooney A. et al (2007). Evaluating the quality of patient leaflets about renal replacement therapy across UK renal units. Nephrology Dialysis Transplantation 22, 2291–2296. [DOI] [PubMed] [Google Scholar]
- Winterbottom A.E., Bekker H.L., Conner M. et al (2012b). Patient stories about their dialysis experience biases others' choices regardless of doctor's advice: an experimental study. Nephrology Dialysis Transplantation 27, 325–331. [DOI] [PubMed] [Google Scholar]
- Wu I.W., Wang S.Y., Hsu K.H. et al (2009). Multidisciplinary predialysis education decreases the incidence of dialysis and reduces mortality–a controlled cohort study based on the NKF/DOQI guidelines. Nephrology Dialysis Transplantation 24, 3426–3433. [DOI] [PubMed] [Google Scholar]


