Abstract
Aims and objectives
The aim was to explore and describe the child's active participation in daily healthcare practice at children's hospital units in Sweden.
Objectives
(a) Identify everyday situations in medical and nursing care that illustrate children's active participation in decision‐making, (b) identify various ways of active participation, actual and optimal in situations involving decision‐making and (c) explore factors in nursing and medical care that influence children's active participation in decision‐making.
Background
Despite active participation being a fundamental right for children, they are not always involved in decision‐making processes during their health care. There still remains uncertainty on how to support children to actively participate in decisions concerning their health care.
Design
A qualitative study with overt, nonparticipant observations fulfilling the COREQ checklist criteria.
Methods
Observations of interactions between children aged 2 and 17 years with both acute and chronic conditions, their parents, and healthcare professionals were conducted at three paediatric hospitals in Sweden. The Scale of Degrees of Self Determination was used to grade identified situations. The scale describes five levels of active participation, with level one being the least and level five being the most active level of participation. Normative judgements were also made.
Results
Children's active participation was assessed as being generally at levels four and five. Children demonstrated both verbal and nonverbal ways of communication during decision‐making. Findings indicated that children's, parents' and healthcare professional's actions influenced children's active participation in decision‐making processes involving healthcare.
Conclusions
Healthcare professionals specialised in paediatrics need to embrace both a child perspective and a child's perspective, plan care incorporating key elements of a child‐centred care approach, to ensure children's active participation at a level of their choosing.
Relevance to clinical practice
There is a need for awareness creation to help healthcare professionals facilitate children's active participation in their care and decision‐making.
Keywords: child perspective, child‐centred care, children, child's perspective, decision‐making, healthcare situations, medical care, nonparticipant observations, nursing care, participation
What does this paper contribute to the wider global clinical community?
Children continue to experience obstacles to having their opinions, wishes and valuations heard in healthcare decision‐making.
Some healthcare professionals make a good effort to facilitate children's participation in decision‐making, but practice remains variable.
Healthcare professionals need organisational, social, paediatric and pedagogical competence in how to support and promote children's participation in decision‐making and to deliver care that is planned from both a child and a child's perspective.
1. INTRODUCTION
The United Nations Convention on the Rights of the Child (UNCRC, 1989) upholds core values on the rights of a child and defines a child as ‘any human being under the age of 18 years unless under the law, applicable to the child, majority is attained earlier’. This study will refer to all persons, including teenagers under the age of 18 years as a child. Both Articles 12 and 13 of the UNCRC highlight the child's right to expression of his/her views and the right to receive information. Despite a child being able to express needs and opinions, decisions about treatment in the healthcare setting are usually made either by healthcare professionals or by the healthcare professionals and parents (Bessell, 2011).
In a Patient Law enacted in Sweden in 2015 (2014:821), the rights of the child as stated in the UNCRC were reinforced. This present research focuses on articles three and four from the Patient Law: ‘When the patient is a child the child's caregiver also should be given information’, and ‘The child's perception to the care or treatment should be mapped out as far as possible and recognized according to age and maturity’ (Government Offices of Sweden, 2017). Ensuring that Swedish legislation is written in accordance with the UNCRC, children are treated with respect and their voices are heard, and children's rights are made known to children themselves, parents and all those working with children, are some of the strategies Sweden has incorporated to strengthen the rights of the child in healthcare (Government Offices of Sweden, 2010). Nevertheless, a recent evaluation of the implementation of the Patient Law from an adult perspective showed no improvements in clinical practice. Instead, a reduction in terms of accessibility, information and participation for adults and for caregivers (parents) was reported. Further, in a comparative international analysis of the adult patient's participation in clinical practice, Sweden was found to lag behind compared to Norway, Finland and Denmark (Swedish Agency for Health & Care Services Analysis, 2017).
2. BACKGROUND
There is no single definition of participation; in this research, the term active participation is used. Active participation is not a one‐step scenario. It can be seen as a multilayered concept with many different processes, which imply a transfer of information and power such that the participant's views influence decision‐making (Franklin & Sloper, 2005; Sinclair, 2004). Active participation requires that structures are put into place and an enabling environment created where each child is seen as a social actor with unique needs (Council of Europe [CE], 2012). Two aspects of active participation: actual and optimal are referred to in this research. The former implies the current status quo of active participation in daily clinical practice, whilst the latter refers to the acceptable level of active participation with regard to age and maturity of the child, rules and regulations, clinical guidelines, policy documents, etc. There are key elements of active participation embedded in Article 13 of the UNCRC that are integral to this research. These elements are that the child receives relevant information, is given an opportunity to freely express own views, and his/her opinions, wishes and valuations are considered in the process of decision‐making (EC, 2014). Healthcare professionals find it challenging to engage children in active participation (Harder, Söderbäck, & Ranheim, 2016). Knowledge from literature reviews shows that very few decisions opposed by children and their parents were reconsidered by the healthcare professionals. In addition, competing factors such as age, gender, communication issues, professional attitude, information offered, previous encounters with healthcare services and psychosocial circumstance were highlighted as factors affecting involvement (Coyne, 2008; Davies & Randall, 2015).
Discourses in research are beginning to look at child‐centred care (CCC) as an alternative way of care delivery for the child, since implementation of a family‐centred care (FCC) approach has been met with numerous challenges (Coyne, Murphy, Costello, O'Neill, & Donnellan, 2013; Dall'Oglio et al., 2018; Davies & Randall, 2015; Ladak et al., 2013). Planning care solely through a FCC lens may pose as a hindrance to the rights of the child recognised in the UNCRC. In the CCC approach, the child is the prime focus of care delivery. The child's right to actively participate in healthcare matters are recognised, and care is tailored to reflect the needs and wishes of the child (Coyne, Hallstrom, & Soderback, 2016; Ford et al., 2018; Wimo, Fagerdahl, & Mattsson, 2018). To enhance children's active participation, it requires healthcare professionals to embrace a child perspective, which include attention towards the child's perspective (the child's understanding of the situation) in the healthcare settings (Söderbäck, Coyne, & Harder, 2011; Sommer, Samuelsson, & Hundeide, 2010).
In the follow‐up to the implementation of the patient law, an evaluation of how children's best interests are upheld and expressed in hospital settings was absent which is a serious omission (Swedish Agency for Health and Care Services Analysis, 2017). Despite ethical, and pragmatic arguments in favour of supporting children to be active participants in healthcare discourses, there is still uncertainty about how to involve children in active participation (Carlsson, Nygren, & Svedberg, 2018; National Board of Health & Welfare, 2015). Therefore, it is necessary to describe the child's active participation in daily healthcare practice.
3. OVERALL AIM
The aim was to explore and describe the child's active participation in daily healthcare practices at children's hospitals.
3.1. Objectives
Identify everyday situations in medical and nursing care that illustrate children's active participation in decision‐making.
Identify various ways of active participation, actual and optimal in situations involving decision‐making.
Explore factors in nursing and medical care that influence children's active participation in decision‐making.
4. METHODS
4.1. Research design
In this exploratory qualitative study, overt, nonparticipant observations were used (Creswell & Plano, 2011). In overt nonparticipant observations, participants are fully aware of the researcher's presence, who takes a passive role and only observes the ongoing interactions of the participants (Greig & Taylor, 2001). This research technique provided the opportunity for the first author to observe interactions and to listen to the views expressed by the children, parents and healthcare professionals. Observations is a method that facilitates the capturing of tacit knowledge (nonverbal communications, artefacts, symbols or hidden cultures) that are an integral part of participants’ daily lives (Dahlgren, Emmelin, & Winkvist, 2007). The methods adhere to the consolidated criteria for reporting qualitative studies (COREQ; see File S1).
4.2. Ethical considerations
Ethical approval was granted by Lund Regional Research Ethics Committee (ref 2014/411). Study was conducted in accordance with the Helsinki Declaration (World Medical Association [WMA], 2013) and General Data Protection Regulations (2018). All departmental managers at the children's hospitals approved the study. Participants were assured of confidentiality and informed of their right to withdraw from the study at any time without this affecting their health care.
4.3. Data collection
4.3.1. Setting
This exploratory study was conducted over an eight‐month period (2017 to 2018), at one paediatric regional hospital and two paediatric units at a tertiary university hospital in the southern part of Sweden. A total of 14 departments were invited to participate and one declined due to limited resources and staffing issues. The departments included four inpatient units, two emergency units and seven outpatient units. The emergency departments, even though under different contextual factors, were chosen to enable the exploration of multiple realities among the participants. Additionally, children admitted to the emergency departments equally have the right to be accorded the important nuances that ensure active participation. The departments included a range of conditions such as congenital malformations, surgery, ears–nose–throat, ophthalmology, plastic surgery, orthopedics, oncology, cardiology and diabetes.
4.3.2. Participant recruitment
Prior to recruiting participants, the contact details of the respective departmental managers were obtained. Meetings were held with departmental managers to provide information concerning the study. The first and last author took advantage of the departments' daily meetings to meet healthcare professionals and inform them about the study. The first author had a contact person (nurse or a secretary), in each department, to help with obtaining schedules of children due for an appointment at the hospital. This was conducted ahead of the child's date of appointment. Information obtained from the scheduled appointments included the child's age, gender, type of diagnosis, type of hospital visit and time of appointment, to ensure purposeful recruitment. For the emergency departments, children were recruited upon arrival. If the healthcare professionals deemed it suitable, the child and his/her parents were informed about the study. Some children had regular appointments at the children's departments making the healthcare professionals to be well acquainted with them and were in a position to judge whether or not asking the child to participate would cause them to feel stressed. On the child's admission, the nurse provided a short introductory letter to the child and his/her parents, informing them about the study. If the child and parents showed interest in taking part in the study, the nurse informed the first author. The first author then met with the child and his/her parents either in the waiting room or in patient rooms to provide further information about the study and to obtain their consent. In cases where a child's parents showed interest to participate but the child did not, the child's wishes took precedence and were not recruited. Parents gave their own consent. Assent from children <15 years was obtained, and both their parents were required to give written consent on their behalf. Children ≥15 years were asked for written and oral assent. Age‐appropriate information was given to the children. Observations began when written assent was obtained from the child and the child's parents.
4.3.3. Participants
The sample invited to participate were 45 children and their parents. Of these, 11 children (six boys and five girls) and their parents declined to take part. Some children had sensitive conditions (complications with their reproductive organs) and did not wish for the first author to be present during their visit. Some parents of children <15 years were uninterested; others had children with intellectual disabilities and did not want their child to participate. In total, 34 children and their parents were observed. In the analysis, only observations from 32 children were included, as the absent parents of two children did not provide consent. The demographics of the observed children are shown in Table 1.
Table 1.
Background variables of observed children included in analysis
| Gender | |
| Girl | 18 |
| Boy | 14 |
| Age range (median age = 8 years) | |
| 2–6 years | 13 |
| 7–11 years | 9 |
| 12–18 years | 10 |
| Nativity of parents | |
| Both native Swedish | 17 |
| One or two parents born abroad | 15 |
| Type of hospital visit | |
| Outpatient | 20 |
| Inpatient | 12 |
| Accompanied by | |
| One parent | 16 |
| Both parents | 15 |
| Alone | 1 |
| Length of hospitalisation | |
| 0–1 hr 59 min | 8 |
| 2 hr–9 hr 59 min | 8 |
| 10 hr–23 hr 59 min | 0 |
| 24 hr–71 hr 59 min | 5 |
| 72 hr+ | 11 |
For reasons of confidentiality, we are not able to provide detailed descriptions of the participants in the study. Children with acute life‐threatening diagnosis were excluded. Healthcare professionals who were involved in the care of the children during their hospital stay were eligible to participate. Posters with information about the study were put in all participating departments, to inform healthcare professionals. Indicated in the posters too was that healthcare professionals who did not wish to participate could opt out of the study by either informing the first author in‐person, by email or by telephone call. The healthcare professionals from the three children's hospitals caring for children included in the observations agreed to take part, except for two professionals who felt unprepared to participate. No observations of situations involving these two were made. Healthcare professionals observed included general nurses, assistant paediatric nurses, paediatric nurses, specialist children's nurses, doctors, anaesthetists, surgeons, cardiologists, etc.
4.3.4. Observations
The first author followed the child and his/her parents throughout their hospital visit. Generally, the first author sat near the door, or stood in a corner of the examination room, observing interactions as they occurred. Prior to each observation period, the child and his/her parents were asked if the observations could continue (Runeson, Hallstrom, Elander, & Hermeren, 2002). For visits that lasted more than an hour, the first author took short breaks every 30 min, to record field notes. Field notes included descriptions of any interactions that occurred between the children, their parents, and healthcare professionals (Runeson et al., 2002). Additionally, verbal and nonverbal communications such as participant's body language, description of people present, time and place were recorded in the field notes. The first author's reactions and feelings were also recorded and distinguished from what was observed. The observations conducted in the inpatient units went on for as long as there were interactions occurring between the child, and the healthcare professionals. In outpatient units, the observations were conducted for as long as the child's appointment lasted. The first author withdrew from observing situations if: the child was asleep, or the child was in the play therapy, or there were no further interactions occurring between the child, and healthcare professionals, or the healthcare professionals did not wish to participate, or if there were restrictions as to how far the first author could follow the patient, for example operation theatre, or postoperation recovery rooms. The observations ended when the child was discharged from the hospital. No follow‐ups were made. The field notes were then transcribed into English in a narrative text format. The communication interactions between the child, their parents and the healthcare professionals were transcribed in the Swedish language and later translated into English by the first author. The last author, a native Swedish speaker, verified the translations. After the first four observations, the last author read through the full transcripts to check that observations and content of transcripts were as detailed as needed. Observations ranged from 25 min to 72 hr, with four hours the median length.
4.4. Data analysis
To identify everyday situations in medical and nursing care that illustrate children's active participation in decision‐making, each individual observation, and field notes were read thoroughly by the first author. Any information that might have been omitted during the transcription was added later by the first author. The analysis of the observations followed three steps as described by Runeson et al. (2002).
In this research, we define a situation as ‘events occurring between children, and healthcare professionals within the healthcare setting, where decisions about medical and nursing care are made’. A situation was selected if it met both of the following conditions: (a) it contained an event where a decision‐making process reflecting nursing or medical care was made, and (b) the child and the healthcare professionals were involved in this decision‐making process.
In step one, each observation transcript was read through by the first author who identified 426 situations that reflected children's active participation in nursing and medical care. Identifying the situations was enhanced by reflecting on questions like ‘What is the decision that was made?’ ‘Was the decision made about nursing or medical care?’ Thereafter, the last author independently went through all identified situations. The two authors reflected upon each identified situation together and discussed if the situation reflected nursing or medical care. During these reflections, 110 situations were omitted. Situations were omitted if:
Events in the situation did not reflect any nursing or medical care
A medical or nursing decision was made only between the healthcare professionals and the child's parents, excluding the child,
A nursing or medical decision was made only between the child and his/her parents, excluding the healthcare professionals,
Events were informational, that is, healthcare professionals informing the children of routine activities to engage in, or giving a child information about what the child was going to undergo prior to an operation or medical examination.
The joint discussions and reflections resulted into both the collation and removal of situations that resulted in 300 identified situations (see Figure 1).
Figure 1.
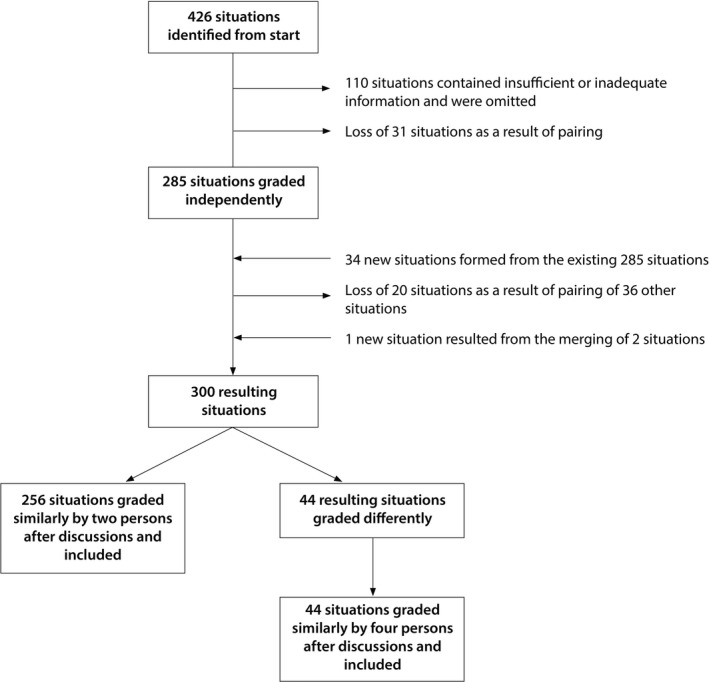
The process of identifying everyday situations in medical and nursing care that illustrates children's participation in decision‐making
In step two, the Scale of Degrees of Self Determination developed by Hermerén (1996) was used to grade the situations. The scale was developed as a theoretical scale, based on philosophy and ethical principles, to grade ways in which an individual's integrity can be respected. Since it is easy to violate a person's integrity when their autonomy is reduced, Hermeren formulated a principle of integrity ‘If one does not respect a person's views, wishes and valuations, one does not respect that person’ (Hermerén, 1996, p151). Compared to other scales, this scale was chosen as it (a) can be used for individuals of all ages, (b) can be used to assess an individual's actual participation and the subsequent respect shown for their integrity and (c) has been used in previous research to assess children's and parent's participation in decision‐making during hospitalisation (Runeson, 2002; Runeson, Elander, Hermeren, & Kristensson‐Hallstrom, 2000;Runeson et al., 2002). The scale divides active participation in decision‐making into five levels, and it describes various levels of attending to individual's opinions, wishes and values. The scale, however, only describes what is done by the member of staff, but falls short in describing how it is done.
A (member of the staff) does not listen to B's (child's) opinions, wishes and valuations.
A listens but refuses to discuss the opinions of B with B; no consultation, no two‐way communication exists.
A communicates with B but does not care about B's answer; B's opinions, wishes and valuations do not influence A's action.
A cares about what B says but acts only partly in accordance with B's opinions, wishes and valuations.
A acts in accordance with B's opinions, wishes and valuations.
In step three, each situation was scrutinised and analysed separately by the first, and last authors, in terms of children's degree of active participation. During the grading process, the questions: ‘What is the decision?’ ‘Who initiates the decision?’ ‘Who is present during this decision‐making?’ ‘Who is deciding? Is it mutual?’ ‘Is the decision reconsidered? If so why?’ ‘How was the decision implemented?’ were used as guiding questions, to arrive at a grade (Hallstrom & Elander, 2004). Of the 300 situations identified in step one, 256 were graded similarly by the first, and last authors. The remaining 44 situations were graded differently. These 44 situations were further graded independently by the second and third authors. Any disagreements arising from the grading were resolved in joint discussions, where authors returned to the main observation transcripts to get a more comprehensive picture. No situation was omitted as all authors agreed on same grading in the joint discussions. A final of 300 situations were included. Further in the analysis, normative assessments were made in order to gain a deeper understanding and make comparisons of how things are and how things ought to be. Normative assessments were done independently by all four authors. Judgements of what could be an optimal level of active participation was done in accordance with the child's age, maturity, scrutinising the situation observed, looking at the planned procedure and what could have been alternatives, the decision made and being aware of guiding documents as the UNCRC (UNCRC, 1989) and the Swedish Law (Government Offices of Sweden, 2017).
5. FINDINGS
5.1. Judgement of children's actual participation in nursing and medical care
The findings show that children's active participation was supported in varying degrees. Level five had the most number of graded situations (156), followed by level four (84), then level three (36) whilst both levels two, and level one, had the same number of graded situations (12). The findings are described below. Examples are given to illustrate each level. Table 2 shows how children's active participation was distributed across the different levels.
Table 2.
Observed children's active participation in situations distributed in different levels
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | |
|---|---|---|---|---|---|
| 2–6 years | 6 | 12 | 19 | 57 | 70 |
| 7–11 years | 0 | 0 | 8 | 10 | 43 |
| 12–18 years | 6 | 0 | 11 | 17 | 43 |
| Total | 12 | 12 | 38 | 84 | 156 |
5.1.1. Level one: A (member of the staff) does not listen to B's (child's) opinions, wishes, and valuations
Here, 12 situations were judged as belonging to level one. This level denotes situations where minimal efforts were made by the healthcare professional to communicate directly with the child even if the child was a teenager. This also included children with intellectual disabilities. Communication was solely with the parents. The children's integrity may not have been respected by the fact that some healthcare professionals asked the parents, and not the child, if they could examine their child's body parts. Some children had received medication without being told what they were being given, or underwent routine checks without being told the reason why. Also, use of restraint was not objected by some of the healthcare professionals.
A doctor attending to a 16‐year old child tells the child ‘We are thinking of taking some tests that are missing, it is important that we take note of acid in the blood, HB, and things like that’. The doctor turns his eye contact towards the child’s father. The doctor and the child’s father discuss the child’s treatment between the two of them. The child is quiet, listening to the back and forth discussions between the father and the doctor. At the end of their discussion, the doctor shifts eye contacts between the child and the father, telling them the nurses will soon come and take the needed tests on the child. He then leaves the room. (Observation 28)
5.1.2. Level two: A listens but refuses to discuss the opinions of B with B; no consultation, no two‐way communication exists
Also, identified in level two were 12 situations, highlighting situations where both the verbal and nonverbal actions of the children were not considered by some healthcare professionals. Use of restraint during: insertion or removal of an intravenous cannula, lying on a table for an X‐ray examination, removal of plasters on various body parts, cleaning operation wounds, taking off clothes, routine examinations, including mouth, nose, ears, were not objected by some healthcare professionals. In some situations, information was not provided to the children nor their parents, and in situations where information was given, minimal efforts were made by the healthcare professionals to check whether the child had understood the information or not.
A doctor tells the mother of a 2.5 year old child that he wants to examine the child to see how the child is responding to the medicine taken some hours ago. The child sits on the mother's laps. ‘Shall we look a little at your body again?’ The doctor asks the child. ‘I do not want’ says the child. He suggests to the mother that the child stands on her laps. The child continues to refuse to be checked. The mother makes her child to stand on her laps. The mother pulls her child's jersey upwards. The doctor quickly checks the child's skin. ‘I do not want’ the child begins to cry. The child's trousers are pulled downwards by the mother. The doctor holds onto the child's legs. The child screams and begins to kick its legs. The doctor holds onto the child's legs tightly, and examines the legs. He tells the child's mother ‘I am satisfied’ and he sits down. The child stops crying. (Observation 34)
5.1.3. Level three: A communicates with B, but B's opinions, wishes and valuations do not influence the actions of A
Judged as belonging to level three were 36 situations where there was a two‐way communication between the healthcare professional and the child. The healthcare professionals made an effort to try and engage the child to participate in their planned care. They also explained procedures to the child and gave information about what was to happen during the examinations. However, despite the healthcare professional's efforts to motivate the children to take part in a planned procedure, the protests of the child against taking part in the procedure did not affect the initial planning, and sometimes use of restraint was not objected. Such situations included finger pricks, cleaning of operation wounds, taking medication, routine measurements including height, weight, temperature and blood pressure, medical examinations.
An anesthetist is attending to a 2‐year old child. ‘Hi, I am going to spray a bit more into your nose’ he says, showing the child the spray. Upon seeing the spray, the child immediately screams ‘no!’ looking away from the anesthetist. The child’s head is held upright by the mother. The child screams, kicks the legs and wriggles the body. The anesthetist sprays into the child’s nose. The child cries bitterly… (Observation 21)
5.1.4. Level four: A cares about what B says but acts only partially in accordance with B's opinions, wishes and valuations
Identified here were 84 situations. Of prominence in this level were situations where children voiced their opinions, and there was a two‐way communication between the healthcare professionals and the children about the planned care. Situations here were often characterised by medical orders such as undergoing medical examinations or taking blood samples. Sometimes, the children were not in agreement with the planned care, so healthcare professionals tried to find alternative means of delivering the care. The child was encouraged to make partial decisions, but this did not significantly influence the planned care. Sometimes restraint was used here too.
A 6‐year old child is seated on the mother's laps, about to have its finger pricked. The father stands beside them. ‘Do you know why you are here today and what we will do?’ the nurse attending to the child asks. The child makes a frown on the face saying ‘I do not want you to prick my finger’. Both the mother and the nurse laugh. The nurse gently rubs the child’s hand and assures the child all will be well. The child is asked to choose which finger to be pricked. The child suggests to count to three before being pricked. When asked to count to three, the child hesitates, shaking the shoulders up and down. The child’s mother suggests she will count to three but the child refuses. ‘I do not want you to count. I will count’ the child angrily says to the mother. ‘One, two …’ the child counts but hesitates for some seconds. The child seems really scared, breathing in and out very fast. ‘Say three!’ the father says in a commanding voice. The child looks very tense. Finally the child says ‘three’. As the nurse is pricking the finger the child screams out ‘aw aw aw’ kicking the legs. The father holds the child’s legs tightly. (Observation 2)
5.1.5. Level five: A acts in accordance with B's wishes, opinions and valuations
There were 156 situations that were graded as level 5. These were situations where children either agreed to the planned care after having received and understood information regarding their upcoming planned care, or the children's integrity was respected and no restraints were used.
‘Now we shall take some blood tests and later you will get some cortisone’ a nurse says to a 10‐year old child. ‘But I want to sleep now. My head aches’ the child complains to the nurse. ‘Yes I understand that it hurts, but we must take the test otherwise we will not know what is troubling you. Shall we get some pain killers for you?’ the nurse asks. The child, still complaining about the pain, nods the head to indicate a yes. The nurse asks ‘Do you want to have it in tablet or liquid form?’ The child looks at the father before deciding. The father raises his eyebrows encouraging the child to decide. The child takes a deep breath, telling the nurse ‘I want the liquid form’. The nurse goes to bring the medicine, and some water. The child refuses to get the water saying: ‘No I want to have the water in my water bottle’ The father gets the water bottle from a back pack. The child then drinks the medicine. (Observation 27)
5.2. Normative judgements of children's participation
Children's active participation could not be considered as optimal in all of the situations graded at levels one (12 situations), two (12 situations) and three (36 situations). See Table 3. The healthcare professionals could have done more to engage the children in these situations. A total of 73 out of 83 situations judged as belonging to level four were considered as optimal levels of active participation. In most of these situations, the children received information and clarity over things they did not understand, and compromises to planned care were reached. An example was when a child did not wish to lie down for her heart examination as suggested by a doctor. She preferred to sit and the doctor respected her wish. Considered as optimal were 153 out of 157 situations judged as belonging to level five. All possibilities of the children's participation were considered by the healthcare professionals. Nonetheless, four situations judged as belonging to level five were considered as nonoptimal. In these situations, too much responsibility seems to have been placed on the child. For instance, a 6‐year‐old child decided when and where to have an intravenous cannula removed, or a 14‐year‐old child was presented with the opportunity to remove an intravenous cannula with the nurse's careful supervision. The 14‐year‐old child did not seem to be comfortable with this suggestion and requested that the nurse removes the cannula instead.
Table 3.
Numbers of optimal and nonoptimal situations at each level
| Level | Optimal | Nonoptimal |
Total (N = 300) |
|---|---|---|---|
| 1 | 0 | 12 | 12 |
| 2 | 0 | 12 | 12 |
| 3 | 0 | 36 | 36 |
| 4 | 73 | 10 | 83 |
| 5 | 153 | 4 | 157 |
5.3. Interactions between children, parents and the healthcare professionals with regard to children's active participation in the decision‐making process
The actions of children, the parents and the healthcare professionals were the factors that impacted positively or negatively on children's active participation in decision‐making.
5.3.1. The children's actions
The children reacted in different ways to the planned care they were expected to receive and during the decision‐making process. Apart from voicing their concerns verbally, children were also observed to communicate and participate using nonverbal cues. The nonverbal cues included: watching curiously with eyes wide open, contemplating on an issue before deciding an action, crying, shaking heads from side to side, moving shoulders up and down, retracting hands, legs or body away from healthcare personnel or their parents to indicate a refusal, nodding head to indicate an acceptance, murmuring words that could not be fully understood, smiling, laughing, making various facial expressions. Most of the nonverbal cues were observed among children aged 2–6 years. The teenagers were more vocal and expressed themselves by speaking up. Some children, by virtue of their personality, appeared more active, asking questions about their planned care and requesting more time before the planned care was administered. Meanwhile, other children appeared passive, observing quietly. The children resisted or protested the care that was given to them. One child expressed he was not interested in receiving information that was being given to him, as it had been repeated at previous visits.
5.3.2. The parents' actions
In some situations, some parents were more involved in the decision‐making process than their child. Some parents were at times unsupportive of their child's actions as they did not request for alternative solutions to painful and unpleasant procedures that their child was expected to undergo. This was seen in situations judged as belonging to levels one, and two. For some children with parents from other countries, the parents tried to liaise with the child in their language. When children did not comply with an examination, some parents sometimes raised their voices against their child and also indicated to their child that they were sad. Sometimes, some parents lost their patience, restrained the child and urged the healthcare professional to just proceed with the planned care. Other parents protected their child from a painful procedure by asking for alternative solutions for their child. Conversely, in other situations, some parent's requests on behalf of their child were not met. For instance, in one situation no provision was made for a child to meet with the surgeon prior to the surgery despite parents’ vocalisations.
5.3.3. Healthcare professional's actions
In some situations, there was minimal effort from the healthcare professional to involve the child in discussions which they had with parents. This was true even for children who were observed to have a reserved personality. When some parents suggested restraint of their child, threatened or raised their voices against their child, some healthcare professionals did not act in favour of the child. Other healthcare professionals had to juggle their time taking care of other patients and sometimes this infringed on the extent to which they would engage children into active participation. Two examples are given below where the same child is engaged differently by two healthcare professionals.
A 3.5 year old child is about to undergo an EKG examination. A nurse attending to the child says ‘Shall we put the tubes again?’ The child refuses by shaking the head from side to side. The nurse tries to convince the child but the child still refuses. The nurse receives a call on her work phone. She excuses herself and leaves the room. (Observation 11)
In other situations, the healthcare professionals made real efforts to engage the children in decision‐making. They tried to create a trusting environment for the children to open up and participate freely. Children scheduled for a surgery were shown pictures of procedures they would undergo and medical equipment they should expect to see. Some healthcare professionals played games with the children and used dolls to describe to the children what would happen to them.
Another nurse in the room walks closer to the 3.5 years old child. Holding the electrodes, she says to the child ‘Does H know colors?’ The child nods the head. ‘Really? Ok where should we put the yellow tube then’ the nurse says in a child‐like voice. The child smiles shyly, putting a finger in the mouth. ‘Shall we put it on the nose?’ The nurse asks the child. The child shakes the head from side to side, smiling. The nurse makes a sad face. ‘aww aww where shall we put it then?’. The child laughs. The child points at its own chest. ‘Shall we put it there?’ The nurse asks the child. The child nods the head. The nurse sticks one of the electrodes on the child’s chest. The nurse continues asking the child where to place the rest of the coloured electrodes. The child seems to be enjoying the game. Before the child realises it, all the electrodes have been placed in their rightful positions. (Observation 11)
6. DISCUSSION
The findings reveal that children's active participation varied and was seen most evident at levels four and five. Active participation was both optimal and nonoptimal. Children's way of communication during decision‐making was both verbal and nonverbal. The actions of children, the parents and the healthcare professionals were the factors that impacted positively or negatively on children's active participation in decision‐making.
6.1. Children's actual and optimal participation
The grading and normative judgements reveal that there were no elements of optimal participation observed in levels one, two nor three. This was seen across all the age groups, including children with intellectual disabilities. These findings are not in accordance with elements of the UNCRC, nor the patient law enacted in Sweden, which all emphasise children's rights to freely express themselves and for their views to be given due weight in accordance with age and maturity (Government Offices of Sweden, 2017; UNCRC, 1989). One may reflect that some of the healthcare professionals may not be fully aware of the patient law and what it entails of them. It could also be that healthcare professionals are aware of the patient law, but may have uncertainties as to how to engage children to actively participate in decisions concerning their health care. Healthcare professionals may need managerial support on how to support the rights of the child in daily clinical practice. It has been suggested by the Swedish Society of Nursing (2014) that up to 60% of nurses within child and adolescent healthcare lack specialist training. Children in Sweden are cared for by a mix of healthcare professionals who both have, and who lack specialised skills and experience in childcare. This may have an influence on how children are cared for, and thus, their active participation. However, this does not exclude organisational factors of the children's services.
In level three participation, children were communicated with; yet, decisions made in the long run may not indicate that some of the healthcare professionals reconsidered opposed decisions. Healthcare professionals in the study by Carlsson et al. (2018) were of the view that children's active participation in the healthcare context was limited and that children could only decide in trivial matters such as deciding which arm the cannula could be inserted, but had little say on the planned treatment. Research by Stålberg, Sandberg, and Söderbäck, (2015) suggests that children as young as three years old are able to communicate their health and treatment needs as well as opinions. Nevertheless, despite the evidence, children are still rarely consulted with or included in discourses pertaining to their own health at a desirable level (Carlsson et al., 2018; Coyne, 2008; Coyne, Amory, Kiernan, & Gibson, 2014).
Highlighted also in this study is that children reacted to various situations in the healthcare setting both through verbal and nonverbal cues. Yet, it appeared that not all nonverbal cues made by the children triggered the desired reactions from some of the healthcare professionals. Stålberg, Sandberg, Larsson, Coyne, and Soderback (2017) also reported on a number of nonverbal cues expressed by children in the healthcare setting. In other research, by Wimo et al. (2018), they argued that the phenomenon of participation must be redefined to include nonverbal bodily actions. Having a child perspective would imply that the healthcare professionals couple their knowledge of what the planned care entails in a specific situation, with the attention and motivation to understand what the child's perceptions, experiences and actions in that specific situation might be (Sommer et al., 2010). This in turn may enhance the healthcare professional's understanding and interpretation of a child's actions in a particular situation and what alternatives to offer the child. Embracing a CCC approach means that healthcare professionals recognise the child as a social being capable of taking part in situations within its own competence (Ford et al., 2018; Söderbäck et al., 2011; Wimo et al., 2018). The child belongs to a family, of which the child is the key agent in the partnerships. Information‐sharing involving the child would then require that the child is included, and duly guided by an adult with opportunity to increase competence, whilst taking care not to only have a child perspective (Coyne et al., 2016).
The findings in this present study indicate that children's active participation across all the ages was seen more at levels four and five. The healthcare professionals involved in these situations might have been more proficient on how to facilitate the individual child's active participation. This is to be welcomed because active participation forms a crucial preparatory foundation for children to make decisions in the future (Runeson et al., 2002; Sinclair & Franklin, 2000). Children's active participation in decisions regarding their own treatment has been associated with decreased anxiety, increased sense of value and control, improvements in their psychological and physical recovery from surgery, more rapid recovery; increased cooperation with procedures, and improved perceptions of treatment services (Walker & Doyon, 2001).
Despite level five being considered as the best level of active participation, there were situations judged as belonging to level five, but not having an optimal level of participation. Some healthcare professionals seemed to actively engage the child by supporting the child to decide beyond what was deemed as optimal. In the case of the 14‐year‐old child who was to remove a cannula, some could argue that a child of this age could still be able to remove a cannula with careful supervision from the healthcare professional. In this particular situation, the child experienced it as a huge responsibility and could not control the situation. Beauchamp and Childress (2013) indicate that competence, which is the ‘the ability to perform a task’ is relative to the decision to be made and is situation based. In determining a child's competence, healthcare professionals need to carefully consider the child's age, illness, maturity and situation.
6.2. Factors affecting children's active participation
Children's, parents’ and healthcare professional's actions were observed as factors that influenced children's active participation. Of children who seemed passive and not to ‘actively’ participate despite efforts from the healthcare professional, Rogoff, Paradise, Mejía‐Arauz, Correa‐Chavez, and Maricela Angelillo (2003) caution that one should be careful not to judge these children as not actively engaging in participation. On the contrary, children who prefer to participate by simply observing a situation can still be seen as active and skilled learners. This is where the ability of healthcare professionals to understand and interpret nonverbal cues of children becomes crucial. Children learn nuances of a situation by observing, and when they are presented with the same or similar situation next time, they are able to use their previous experience from one situation, to either engage or disengage themselves from the next situation. Lave and Wenger (1991) identify this as situated learning, where both verbal and nonverbal expressions demonstrate experiences of learning in previous situations. This is important because a negative or positive situation in which a child was once involved in, will influence their experiences and skills in the healthcare setting. A negative event may lead to a child's withdrawal or unwillingness to actively participate in a situation, whilst a positive event may lead to motivation and engagement in a situation. With age and maturity, children become capable to reason as they gradually develop a better understanding of their environment and situations (Walker & Doyon, 2001). A child's refusal to take part in a particular treatment plan should be taken seriously and the child should be seen as being rational and competent in his/her own means.
Some parents either protected their child from painful procedures by asking for alternative solutions, or sometimes other parents resorted to the use of restraint during various medical procedures, which some of the healthcare professionals did not object. Similar findings have been reported in other research (Coyne, 2008). With reference to use of restraint, one then questions what role healthcare professionals ought to play when parents suggest actions that might not always be in the child's best interest. Healthcare professionals can assume the role of surrogate decision‐maker, having a commitment to the incompetent patient's interests, free of conflicts of interest and free of controlling influence by those who might not act in the patient's best interest (Beauchamp & Childress, 2013). Also, healthcare professionals have a legal responsibility to ensure that the rights, dignity and safety of children are upheld during their hospital stay. Therefore, the use of restraint (forceful physical restraint of children by their parents so that a medical procedure can be undertaken) may be considered as a violation of the child's basic right to physical and psychological protection during their hospital stay (European Association for Children in Hospital [EACH], 2018). Others have argued for the use of restraint to protect a patient. If restraint is to be considered as a way of protecting the patient, then it should be seen as a separate treatment, presented as an alternative form of care. It has to be done with the patient's consent/knowledge. Conversely, research in paediatrics has suggested that restraint may be associated with speech and language problems, a negative self‐image, fear of a procedure, distrust of medical care and post‐traumatic stress disorder (Brenner, 2007; McGrath, Forrester, Fox‐Young, & Huff, 2002). Guidelines such as the ‘safe sedation of children undergoing therapeutic procedures’ from the Scottish Intercollegiate Guidelines network calls restraint during a medical procedure that is not lifesaving as unacceptable (EACH, 2018).
There were some situations where the child was supported to decide beyond what was deemed as optimal. This may indicate a lack of communication by some of the healthcare professionals with the child, on the options available and limitations during the decision‐making process. An alternative explanation could be that the presence of a child's parents may have influenced the extent to which the child could be given limitations by some of the healthcare professionals. Results from a review by Coyne (2008) indicated that there were high levels of uncertainty among healthcare professionals, of the extent to which children should be included in decision‐making. Having children's opinions to reflect in decisions made may imply that healthcare professionals relinquish to a certain level, their authority to the children. Nonetheless, it has been suggested by Coyne (2008) that this may make healthcare professionals feel threatened to deal with children who are well empowered to challenge them. Professional competence (at organisational, social and pedagogical levels) in care situations is thus inevitable. According to Söderbäck (2010), organisational competence entails the ability to create an enabling environment for the child, whilst being time conscious. Social skills require the aptitude to facilitate a two‐way communication with the child. Pedagogical competence demands that information, preparation and implementation of activities reflect the child's competence, its needs and its rights to protection and participation (Söderbäck, 2010).
6.3. Strengths and limitations
Trustworthiness in this study was enhanced by triangulation of data collection. Participants with varying diagnoses, age, ethnicity and gender were recruited. All observations were conducted by the first author, hence enhancing consistency in data collection. Detailed observation descriptions lead to richness of data, producing more than 300 situations to analyse. Data analysis was conducted by all four authors. The first author, not having any nursing or medical background, was able to take an impartial role when interacting with the healthcare professionals, the children and the parents. Prior to the research, the first author had never met or known any of the study participants, nor worked in any of the environments nor had any children treated in any of the children's hospitals and departments included in the research.
The first author, not having had a level of preunderstanding as a healthcare professional, might be seen as a limitation. Nevertheless, throughout data collection and analysis, guidance was given by the other three authors who are educated in paediatrics, have experience of working in the area and are familiar with the daily routines of the departments. The first author, not a native Swedish speaker, may have missed out certain nuances of the language, leading to loss of information in the observations. Observations were captured in field notes; hence, the first author depended mainly on recall and written notes. To overcome this challenge, being well informed of a patient's condition prior to an observation played an important role. Field notes were written immediately or after short breaks to reduce recall bias, but no matter how detailed descriptions of observations are, much still remains invisible. With experience in conducting observations, the last author was able to review observations and give guidance. Due to the explorative nature of our method design, we did not include the following in our analysis: variability in level of participation across units, differences in departmental contextual factors, and whether or not the same healthcare professionals were observed interacting with more than one child. The first author tried to establish a relation with the children and their parents before the observations which may have influenced the children's and parents' behaviour. Likewise, healthcare professionals could have altered their actions, leading to false impressions for the first author to note, but with time, they all appeared to become at ease with the first author's presence and resumed their natural behaviour.
7. CONCLUSION
Active participation can be said to occur at different levels, and factors that influence active participation include the child's, parents' and healthcare professional's actions. Daily clinical practice in children's hospital units does not fully fulfil the requirements of the Swedish patient law. Managerial support in daily clinical practice is needed for healthcare professionals to emulate professional competence, for key elements of active participation (a. Receiving relevant information, b. being given an opportunity to freely express own views, c. consideration of opinions, wishes and valuations in the process of decision‐making) to be availed to children. Care delivery for the child needs to be planned by professionals specialised in paediatrics, with both a child perspective and a child's perspective, planning care with core elements of a child‐centred care approach. Future research could focus on combining observations with interviews of children, their parents and healthcare professionals to gain a deeper understanding of their experiences of the child's active participation in their own health care.
8. RELEVANCE TO CLINICAL PRACTICE
When children are actively involved in decision‐making in their health care, they are usually better informed, thereby facilitating and benefiting the work of the healthcare professionals. There remains a need for interventions aimed at educating healthcare professionals on children's rights and how they can facilitate children's active participation based on the child's needs and competence.
CONFLICT OF INTEREST
The authors do not have any conflicts of interest to declare.
Supporting information
ACKNOWLEDGEMENTS
The authors wish to thank all the children, parents and healthcare professionals who took part in this study. The authors also wish to thank all the unit managers from the participating hospital departments for facilitating this study.
Quaye AA, Coyne I, Söderbäck M, Hallström IK. Children's active participation in decision‐making processes during hospitalisation: An observational study. J Clin Nurs. 2019;28:4525–4537. 10.1111/jocn.15042
Funding information
This research is funded by the Swedish Research Council and SRC for Health, Working Life, and Welfare (2013/2101).
REFERENCES
- Beauchamp, T. L. , & Childress, J. F. (2013). Principles of biomedical ethics. New York, NY: OUP. [Google Scholar]
- Bessell, S. (2011). Participation in decision‐making in out‐of‐home care in Australia: What do young people say? Children and Youth Services Review, 33(4), 496–501. 10.1016/j.childyouth.2010.05.006 [DOI] [Google Scholar]
- Brenner, M. (2007). Child restraint in the acute setting of pediatric nursing: An extraordinarily stressful event. Issues in Comprehensive Pediatric Nursing, 30(1–2), 29–37. 10.1080/01460860701366658 [DOI] [PubMed] [Google Scholar]
- Carlsson, I. M. , Nygren, J. M. , & Svedberg, P. (2018). Patient participation, a prerequisite for care: A grounded theory study of healthcare professionals' perceptions of what participation means in a paediatric care context. Nursing Open, 5(1), 45–52. 10.1002/nop2.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council of Europe (2012). Participation of children and young people under the age of 18. Retrieved from https://rm.coe.int/CoERMPublicCommonSearchServices/DisplayDCTMContent?documentId=090000168046c478 [Google Scholar]
- Coyne, I. (2008). Children's participation in consultations and decision‐making at health service level: A review of the literature. International Journal of Nursing Studies, 45(11), 1682–1689. 10.1016/j.ijnurstu.2008.05.002 [DOI] [PubMed] [Google Scholar]
- Coyne, I. , Amory, A. , Kiernan, G. , & Gibson, F. (2014). Children's participation in shared decision‐making: Children, adolescents, parents and healthcare professionals' perspectives and experiences. European Journal of Oncology Nursing, 18(3), 273–280. 10.1016/j.ejon.2014.01.006 [DOI] [PubMed] [Google Scholar]
- Coyne, I. , Hallstrom, I. , & Soderback, M. (2016). Reframing the focus from a family‐centred to a child‐centred care approach for children's healthcare. Journal of Child Health Care, 20(4), 494–502. 10.1177/1367493516642744 [DOI] [PubMed] [Google Scholar]
- Coyne, I. , Murphy, M. , Costello, T. , O'Neill, C. , & Donnellan, C. (2013). A survey of nurses' practices and perceptions of family‐centered care in Ireland. Journal of Family Nursing, 19(4), 469–488. 10.1177/1074840713508224 [DOI] [PubMed] [Google Scholar]
- Creswell, J. W. , & Plano, C. V. L. (2011). Designing and conducting mixed methods research. Los Angeles, CA: SAGE Publications. [Google Scholar]
- Dahlgren, L. , Emmelin, M. , & Winkvist, A. (2007). Qualitative methodology for international public health, 2nd ed. Umeå, Sweden: Print och Media, Umeå University. [Google Scholar]
- Dall'Oglio, I. , Di Furia, M. , Tiozzo, E. , Gawronski, O. , Biagioli, V. , Di Ciommo, V. M. , … Raponi, M. (2018). Practices and perceptions of family centered care among healthcare providers: A cross‐sectional study in a pediatric hospital. Journal of Pediatric Nursing, 43, e18–e25. 10.1016/j.pedn.2018.07.015 [DOI] [PubMed] [Google Scholar]
- Davies, A. , & Randall, D. (2015). Perceptions of children's participation in their healthcare: A critical review. Issues in Comprehensive Pediatric Nursing, 38(3), 202–221. 10.3109/01460862.2015.1063740 [DOI] [PubMed] [Google Scholar]
- European Association for Children in Hospital (2018). Forced immobilization (‘Restraint’) during Medical Procedures in young children. An ethical and legal investigation of a common practice. Retrieved from https://www.each-for-sick-children.org/
- Ford, K. , Dickinson, A. , Water, T. , Campbell, S. , Bray, L. , & Carter, B. (2018). Child centred care: Challenging assumptions and repositioning children and young people. Journal of Pediatric Nursing, 43, e39–e43. 10.1016/j.pedn.2018.08.012 [DOI] [PubMed] [Google Scholar]
- Franklin, A. , & Sloper, P. (2005). Listening and responding? Children's participation in health care within England. International Journal of Children's Rights, 13(1–2), 11–29. 10.1163/1571818054545277 [DOI] [Google Scholar]
- General Data Protection Regulation (2018). Chapter 3: Rights of the data subject. Retrieved from https://gdpr-info.eu/
- Government Offices of Sweden . (2010). Strategi för att stärka barnets rättigheter i Sverige [Strategy to strengthen the rights of the child in Sweden]. Retrieved from https://www.regeringen.se/informationsmaterial/2011/10/s2010.026/ [Google Scholar]
- Government Offices of Sweden (2017. ). Barnkonventionen ska bli svensk lag [The children's convention shall be Swedish law]. Retrieved from http://www.regeringskansliet.se/debattartiklar/2015/02/barnkonventionen-ska-bli-svensk-lag/ [Google Scholar]
- Greig, A. , & Taylor, J. (2001). Doing Research with Children, 1st ed. London: SAGE Publications. [Google Scholar]
- Hallstrom, I. , & Elander, G. (2004). Decision‐making during hospitalization: Parents' and children's involvement. Journal of Clinical Nursing, 13(3), 367–375. 10.1046/j.1365-2702.2003.00877.x [DOI] [PubMed] [Google Scholar]
- Harder, M. , Söderbäck, M. , & Ranheim, A. (2016). Being in care situations with young children presents ambiguous challenges. Nordic Journal of Nursing Research, 36(2), 68–73. 10.1177/0107408315605997 [DOI] [Google Scholar]
- Hermerén, G. (1996). Kunskapens pris: Forskningsetiska problem och principer i humaniora och samhällsvetenskap HSFR [The price of knowledge: Research ethical problems and principles in the humanities and social sciences]. Sweden, Uppsala. [Google Scholar]
- Ladak, L. A. , Premji, S. S. , Amanullah, M. M. , Haque, A. , Ajani, K. , & Siddiqui, F. J. (2013). Family‐centered rounds in Pakistani pediatric intensive care settings: Non‐randomized pre‐ and post‐study design. International Journal of Nursing Studies, 50(6), 717–726. 10.1016/j.ijnurstu.2012.05.009 [DOI] [PubMed] [Google Scholar]
- Lave, J. , & Wenger, E. (1991). Situated learning: Legitimate peripheral participation. Cambridge, UK: Cambridge University Press. [Google Scholar]
- McGrath, P. , Forrester, K. , Fox‐Young, S. , & Huff, N. (2002). “Holding the child down” for treatment in paediatric haematology: The ethical, legal and practice implications. Journal of Law and Medicine, 10(1), 84–96. [PubMed] [Google Scholar]
- National Board for Health and Welfare (2015). Bedöma barns mognad för delaktighet. Assessing children's maturity for participation Socialstyrelsen. Retrieved from http://www.socialstyrelsen.se/publikationer2015/2015-12-22 [Google Scholar]
- Rogoff, B. , Paradise, R. , Mejía‐Arauz, R. , Correa‐Chavez, M. , & Maricela Angelillo, C. (2003). Firsthand learning through intent participation. Annual Review of Psychology, 54(1), 175–203. 10.1146/annurev.psych.54.101601.145118 [DOI] [PubMed] [Google Scholar]
- Runeson, I. (2002). Children's participation in decision‐making in health care. (Doctoral thesis, Department of Medical Ethics, Lund University, Sweden). [Google Scholar]
- Runeson, I. , Elander, G. , Hermeren, G. , & Kristensson‐Hallstrom, I. (2000). Children's consent to treatment: Using a scale to assess degree of self‐determination. Pediatric Nursing, 26(5), 455–458, 515. [PubMed] [Google Scholar]
- Runeson, I. , Hallstrom, I. , Elander, G. , & Hermeren, G. (2002). Children's participation in the decision‐making process during hospitalization: An observational study. Nursing Ethics, 9(6), 583–598. 10.1191/0969733002ne553oa [DOI] [PubMed] [Google Scholar]
- Sinclair, R. (2004). Participation in practice: Making it meaningful, effective and sustainable. Children & Society, 18(2), 106–118. 10.1002/chi.817 [DOI] [Google Scholar]
- Sinclair, R. , & Franklin, A. (2000). A quality protects research briefing: Young people's participation. London, UK: Department of Health, Research in Practice and Making Research Count. [Google Scholar]
- Söderbäck, M. (2010). Barns rätt i vården. Allmänna Barnhusets förlag. Children's Right in Healthcare. Stockholm, Sweden: General Children's House Publishers. [Google Scholar]
- Söderbäck, M. , Coyne, I. , & Harder, M. (2011). The importance of including both a child perspective and the child's perspective within health care settings to provide truly child‐centred care. Journal of Child Health Care, 15(2), 99–106. 10.1177/1367493510397624 [DOI] [PubMed] [Google Scholar]
- Sommer, D. , Samuelsson, P. I. , & Hundeide, K. (2010). Child perspectives and children's perspectives in theory and practice. London, UK: Springer. [Google Scholar]
- Stålberg, A. , Sandberg, A. , Larsson, T. , Coyne, I. , & Soderback, M. (2017). Curious, thoughtful and affirmative‐Young children's meanings of participation in healthcare situations when using an interactive communication tool. Journal of Clinical Nursing, 27(1–2), 235–246. 10.1111/jocn.13878 [DOI] [PubMed] [Google Scholar]
- Stålberg, A. , Sandberg, A. , & Söderbäck, M. (2015). Younger children's (three to five years) perceptions of being in a health‐care situation. Early Child Development and Care, 186(5), 832–844. 10.1080/03004430.2015.1064405 [DOI] [Google Scholar]
- Swedish Agency for Health and Care Services Analysis (2017). Lag utan genomslag [Law without impact]. Retrieved from http://www.vardanalys.se/Rapporter/2017/Lag-utan-genomslag/ [Google Scholar]
- The Swedish Society of Nursing (2014). SATSA på specialistsjuksjörterskan– För säkrare, tryggare och effektivare vård [Focus on specialist nurses for safer, secure and effective care]. Retrieved from https://www.swenurse.se/Sa-tycker-vi/publikationer/Utbildning/Satsa-pa-specialistsjukskoterskan/ [Google Scholar]
- The United Nations (1989). Convention on the rights of the child. Treaty Series, 1577, 3. [Google Scholar]
- Walker, N. E. , & Doyon, T. (2001). Fairness and reasonableness of the child's decision: A proposed legal standard for children's participation in medical decision making. Behavioral Sciences & the Law, 19(5–6), 611–636. 10.1002/bsl.461 [DOI] [PubMed] [Google Scholar]
- Wimo, E. , Fagerdahl, A.‐M. , & Mattsson, J. (2018). Children's participation in the PICU from the nurses' perspective, an observational study. Journal of Nursing Education and Practice, 9(4), 65. [Google Scholar]
- World Medical Association (2013). World Medical Association declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects, Helsinki. Retrieved from https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


