Abstract
Objective:
Numerous systematic reviews and meta-analyses on the interventions to reduce burnout of physicians and nurses have been published nowadays. This study aimed to summarize the evidence and clarify a bundled strategy to reduce burnout of physicians and nurses.
Methods:
Researches have been conducted within Cochrane Library, PubMed, Ovid, Scopus, EBSCO, and CINAHL published from inception to 2019. In addition, a manual search for relevant articles was also conducted using Google Scholar and ancestral searches through the reference lists from articles included in the final review. Two reviewers independently selected and assessed, and any disagreements were resolved through a larger team discussion. A data extraction spreadsheet was developed and initially piloted in 3 randomly selected studies. Data from each study were extracted independently using a pre-standardized data abstraction form. The the Risk of Bias in Systematic reviews and assessment of multiple systematic reviews (AMSTAR) 2 tool were used to evaluate risk of bias and quality of included articles.
Results:
A total of 22 studies published from 2014 to 2019 were eligible for analysis. Previous studies have examined burnout among physicians (n = 9), nurses (n = 6) and healthcare providers (n = 7). The MBI was used by majority of studies to assess burnout. The included studies evaluated a wide range of interventions, individual-focused (emotion regulation, self-care workshop, yoga, massage, mindfulness, meditation, stress management skills and communication skills training), structural or organizational (workload or schedule-rotation, stress management training program, group face-to-face delivery, teamwork/transitions, Balint training, debriefing sessions and a focus group) and combine interventions (snoezelen, stress management and resiliency training, stress management workshop and improving interaction with colleagues through personal training). Based on the Risk of Bias in Systematic reviews and AMSTAR 2 criteria, the risk of bias and methodological quality included studies was from moderate to high.
Conclusions:
Burnout is a complicated problem and should be dealt with by using bundled strategy. The existing overview clarified evidence to reduce burnout of physicians and nurses, which provided a basis for health policy makers or clinical managers to design simple and feasible strategies to reduce the burnout of physicians and nurses, and to ensure clinical safety.
Keywords: burnout, meta-analyses, nurses, overview, physicians, systematic reviews
1. Introduction
Burnout refers to a prolonged response to chronic emotional and interpersonal stressors caused by work, manifested as emotional exhaustion, depersonalization, and reduced personal accomplishment.[1] Burnout prevalence data were extracted from 182 studies involving 109628 physicians in 45 countries, where overall prevalence ranged from 0% to 80.5%, emotional exhaustion 0% to 86.2%, depersonalization 0% to 89.9%, and low personal accomplishment 0% to 87.1%.[2] Among physicians in China (9302 participants from 11 studies), burnout prevalence ranged from 66.5% to 87.8%.[3] The highest levels of burnout were reported among nurses, although all healthcare providers showed high burnout,[4] and the prevalence has been increasing in recent years.[5] Burned-out physicians and nurses not only suffer from more substance abuse, broken interpersonal relationships, and suicide ideation,[6,7] they also overwhelmingly believe they deliver poorer quality care, and patients seem to be less satisfied with burned-out physicians and nurses (impacting patient outcomes, in terms of patient experiences, quality of care, and medical errors).[8–14] Reducing burnout has been recognized as a fundamental health care policy goal across the globe, and health care organizations are encouraged to invest efforts to improve physicians’ and nurses’ wellness, particularly for early-career physicians and nurses.[14–16]
Burnout among healthcare providers is in relation to their gender, marital status, work environment, interpersonal and professional conflicts, emotional distress, and low social support.[4,17] Individual-focused, structural or organizational, or combine solutions were required.[11,18–21] Previous studies have already carried out systematic review on the physicians’ burnout.[22] However, due to the limited database and literature, no schemes have been proposed, which can be popularized and applied in real life. Recently, COVID-19 has swept the world, which has drawn pay more attention to the mental health of human beings,[23] especially front-line health care workers.[24] This study aimed to discuss bundled strategy to reduce burnout of physicians and nurses, and attempted to present a protocol of intervention model.
2. Methods
The current overview for systematic reviews (SRs) and meta-analyses was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
2.1. Eligibility and exclusion Criteria
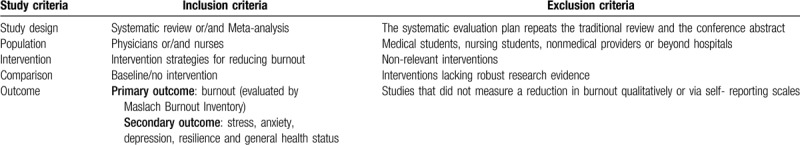
The inclusion criteria and exclusion were seen in Table 1.
Table 1.
Inclusion and exclusion criteria.
2.2. Search Strategy and Data Sources
Databases including Cochrane Library, PubMed, Ovid, Scopus, EBSCO and CINAHL database were chosen and searched for publications from inception to December 2019 with no restriction on language, which covered a wide range of subjects including medicine, psychosociology and nursing. In addition, a manual search for relevant articles was also conducted using Google Scholar and ancestral searches through the reference lists of articles included in the final review. The search strategy included combinations of 3 key blocks of terms (burnout; physicians and nurses; interventions) using medical subject headings (MESH terms) and text words. Consultation has been conducted between the project team and information specialists before finalizing the search strategy (see Additional file 1).
2.3. Study Selection
Search results were exported from Endnote X7 and duplicates were removed. Study selection was completed in 2 stages. Titles and abstracts of the studies were screened and subsequently full texts of the selected studies were accessed and further screened against the eligibility criteria. The title and abstract screening were undertaken by XJ. Z and YQ. S. Two reviewers independently selected and evaluated, and any disagreements were resolved through a larger team discussion.
2.4. Data Extraction
A data extraction spreadsheet was developed and initially piloted in 3 randomly selected studies. Following data were retrieved from articles included in this review: study characteristics (eg, first author, year of publication, country, search period, and number of primary studies included), participant characteristics (eg, sample size), outcome measures (eg, MBI, JSS, PSS, ESS, BP and HR), and study methods (eg, interventions in experimental/control groups). Data from each study were extracted independently using a pre-standardized data abstraction form.
2.5. Assessment of risk of bias and quality
The Risk of Bias in Systematic reviews (ROBIS) and AMSTAR 2 scale were used to evaluate risk of bias (RoB) and methodological quality of the included systematic reviews and/or meta-analyses, which were evaluated independently by 2 authors. The ROBIS[25] is a tool to assess RoB of SRs which comprised phase 2 (4 domains) and phase 3. Four domains in phase 2 are study eligibility criteria, identification and selection of studies, data collection and study appraisal, and synthesis and findings. The results of each domain and phase 3 were rated as high risk, low risk, or unclear risk. The AMSTAR 2[26] includes 16 items and is not designed to generate an overall ‘score’. A high score may disguise critical weaknesses in specific domains, such as an inadequate literature search or a failure to assess RoB within individual studies that were included in a systematic review. In making an overall rating of systematic review, it is important to take account of flaws in critical domains, which may greatly weaken the confidence that can be placed in a systematic review.
2.6. Data synthesis
A quantitative analysis of the included SRs was not performed due to information from overlapping RCTs between SRs. On the other hand, literature of different design types cannot be quantitatively synthesized. Therefore, a qualitative synthesis of the included studies was conducted instead. Literature search results and data extraction results were summarized descriptively. To exclude duplicate RCTs, 2 authors reviewed all of the RCTs in each SR. A summary of efficacy outcomes was presented based on the different outcome measures, controls and interventions. A narrative synthesis was therefore generated considering the total number of SRs that reported results, the methodological quality of SRs and RCTs, and the quality of evidence for the outcomes to yield final conclusions.
2.7. Ethics
Ethics approval is not required in overview of SRs and meta-analyses.
3. Results
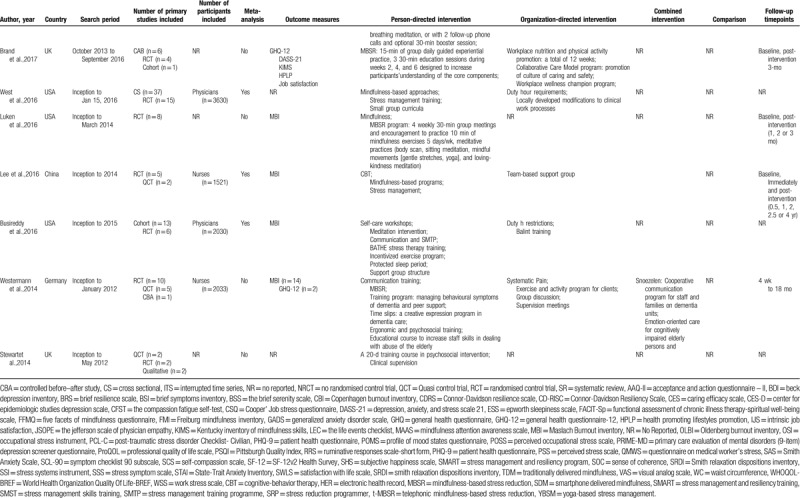
The search strategy yielded 841 potential studies. After removing duplications (n = 334) and eliminating 486 by a first pass through the titles and abstracts, the potentially relevant literature was screened in 2 rounds and resulted in 22 studies from 2014 to 2019 (Fig. 1).[15,16,18–21,27–42] The included researchers are from the USA (n = 7), UK (n = 4), Australia (n = 3), China (n = 2), Italy (n = 2), Germany, Iran, Finland and Malaysia. The search period of included research was from the inception to 2019. The 38.10% included research were meta-analyzed. The measurement instruments used in the literature are shown in Table 2 , and MBI is the most widely used questionnaire to evaluate burnout. Follow-up time ranged from 0 to 7 years. The detailed characteristics of the included research are presented in Table 2 .
Figure 1.
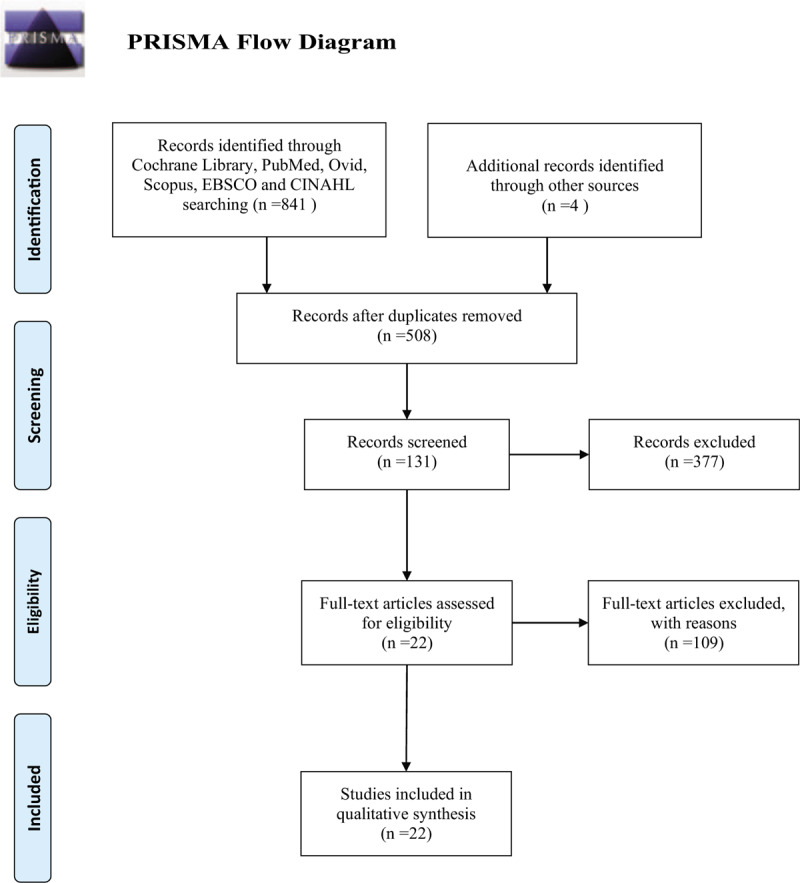
Flowchart of the literature selection process.
Table 2.
Characteristics of the included systematic reviews/ meta-analysis on the use of interventions for reducing burnout of physicians and nurses.
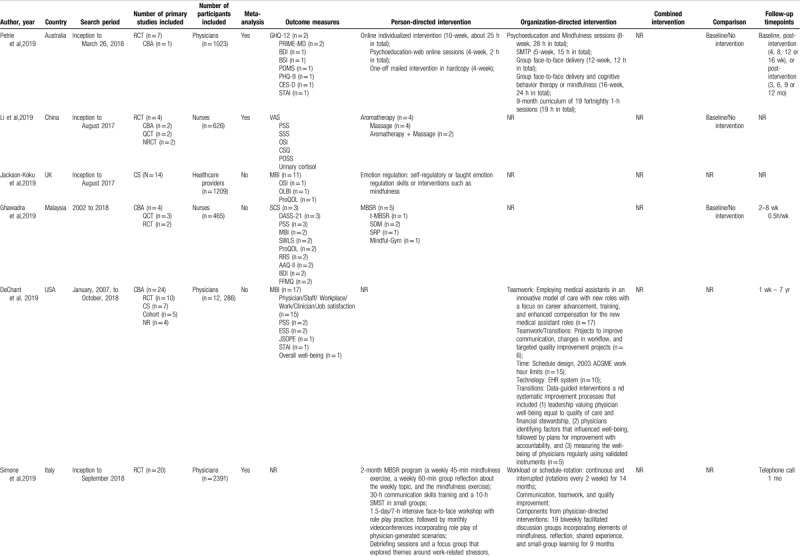
Table 2 (Continued).
Characteristics of the included systematic reviews/ meta-analysis on the use of interventions for reducing burnout of physicians and nurses.
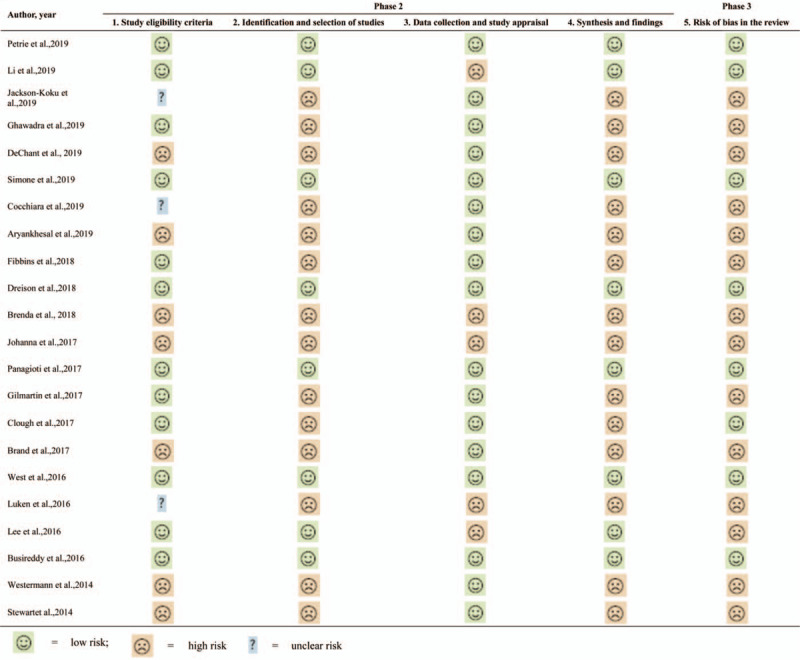
3.1. Assessment of risk of bias
The RoB of the included studies was assessed by ROBIS. Table 3 presents the results of assessment. The first domain aims to assess whether primary study eligibility criteria were prespecified, clear, and appropriate to the review question.[25] 12 out of 22 studies were rated low risk and 3 were unclear risk. The second domain aims to assess whether any primary studies that would have met the inclusion criteria were not included in the review. 8 out of 22 studies were rated low risk. The third domain aims to assess whether bias may have been introduced through the data collection or risk of bias assessment processes. 17 studies were of low risk while 5 studies were graded as high risk. The fourth domain aimed to assess whether the data was combined from the included primary studies. Only 8 studies rated low risk of bias. The final phase considers whether the systematic review as a whole is at risk of bias, 14 studies were rated high risk and 8 were low.
Table 2 (Continued).
Characteristics of the included systematic reviews/ meta-analysis on the use of interventions for reducing burnout of physicians and nurses.
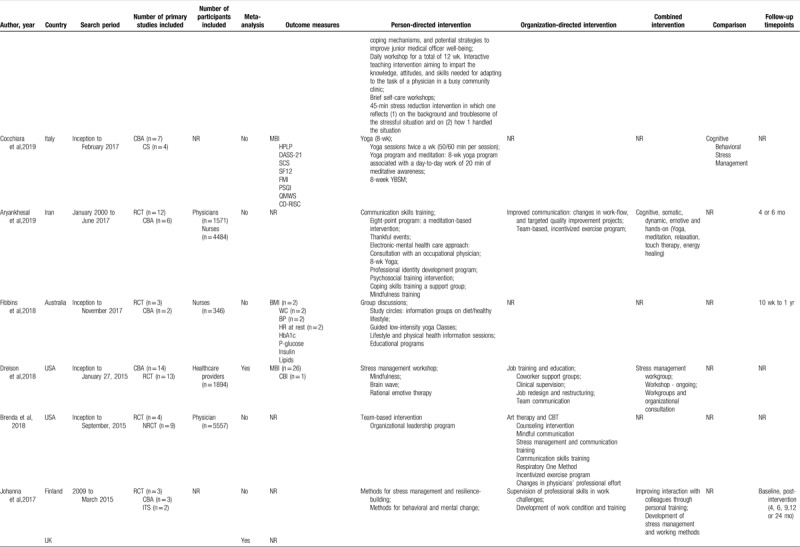
Table 3.
Risk of bias of included systematic reviews/ meta-analysis.
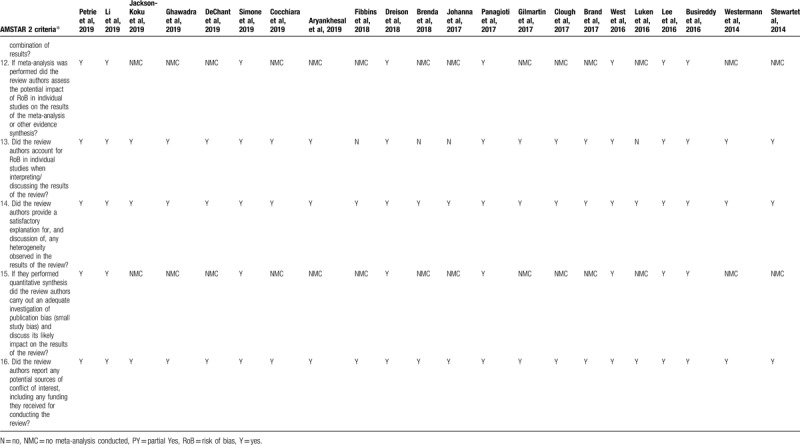
3.2. Assessment of quality
The quality of included studies was assessed by AMSTAR 2 (Table 4 ), which is not designed to generate an overall ‘score’ to avoid disguising critical weaknesses in specific domains, such as an inadequate literature search or are a failure to assess risk of bias with individual studies that were included in an overview.[26] 12 of the 16 items were reported over 60% of compliance, which were as followed: the research questions and inclusion criteria for the review include the components of PICO (item 1); explain their selection of the study designs for inclusion in the review (item 3); use a comprehensive literature search strategy (item 4); perform study selection in duplicate (item 5); perform data extraction in duplicate (item 6); provide a list of excluded studies and justify the exclusions (item 7); describe the included studies in adequate detail (item 8); use a satisfactory technique for assessing the RoS in individual studies that were included in the review (item 9); account for RoB in individual studies when interpreting/ discussing the results of the review (item 13); provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review (item 14); carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review (item 15) and report any potential sources of conflict of interest, including any funding they received for conducting the review (item 16). 4 items with compliance lower than 40% were the main reporting limitations to be blamed: contain an explicit statement that the review methods were established prior to conduct of the review and did the report justify any significant deviations from the protocol (item 2, 27.27%); report on the sources of funding for the studies included in the review (item 10, 0.00%); use appropriate methods for statistical combination of results (item 11, 36.36%); and assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis (item 12, 36.36%). As a whole, the methodological quality and quality of included studies was from moderate to high.
Table 2 (Continued).
Characteristics of the included systematic reviews/ meta-analysis on the use of interventions for reducing burnout of physicians and nurses.
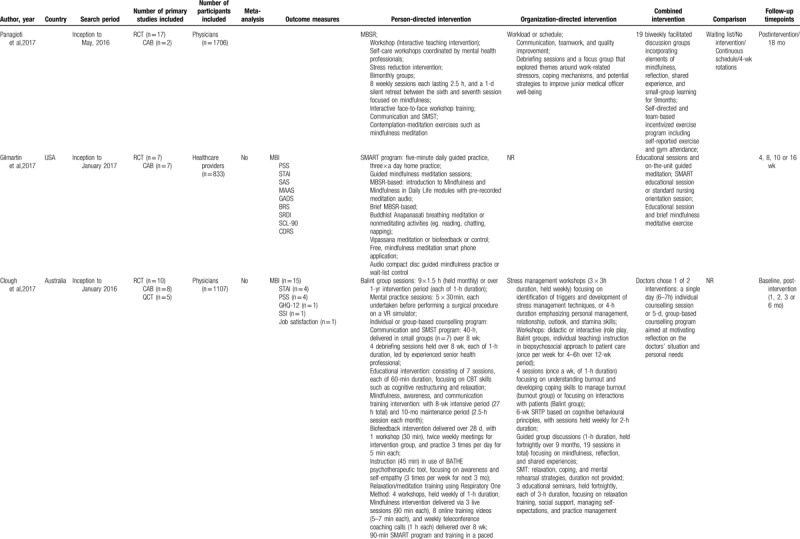
Table 4.
Quality assessment (AMSTAR 2) of included systematic reviews/ meta-analysis.
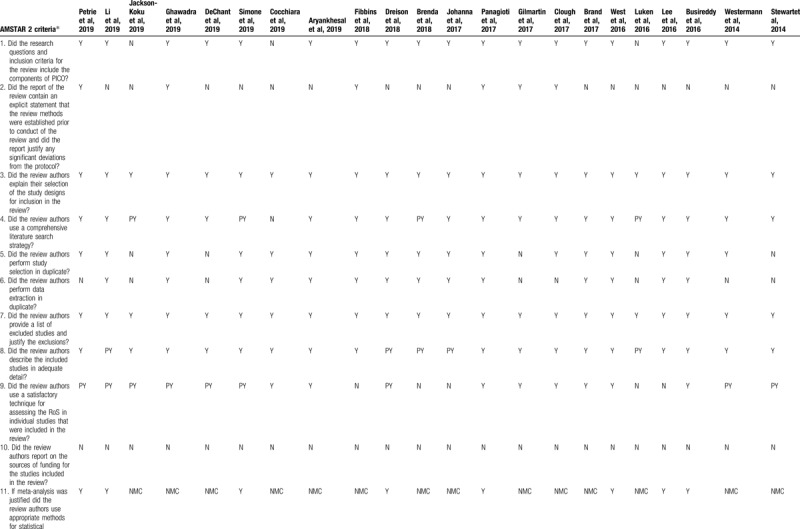
Table 4 (Continued).
Quality assessment (AMSTAR 2) of included systematic reviews/ meta-analysis.
3.3. Interventions of reducing burnout of physicians and nurses
Previous studies have reported on the content, intensity, form, evaluation, and timepoint of follow-up of interventions to reduce the burnout of physician and nurses (Table 2 ). There were three types of interventions: individual-focused, structural or organizational, and combine interventions. Emotion regulation was an important psychological variable, which associated with burnout. The self-regulatory or emotion regulation skills such as mindfulness was used to reduce the doctors’ burnout.[28] Individual-focused interventions included self-care workshops,[19,31,40] stress management skills[31,37,39,42] and communication skills training.[19,20,42] Other interventions such as yoga,[16,32,33] massage,[15] mindfulness[16,18,20,31,37,39,42] and meditation[16,19,35,40] have been reported. Structural or organizational interventions included workload or schedule-rotation,[19,31] stress management training program,[27] group face-to-face delivery,[19,27,31] teamwork/transitions,[30,42] Balint training,[20,40] debriefing sessions and a focus group.[19,20,31] Team-based primary care redesign, “Primary Care 2.0”, with the goal of addressing the Quadruple Aim of health care (ie, the Triple Aim plus reducing workforce burnout) with the following components:
-
(1)
an expanded “care coordinator” role for medical assistants including scribing, population health management, and between-visit care management,
-
(2)
health coaching and motivational interviewing,
-
(3)
“lean” quality improvement to support a Learning Health System,
-
(4)
telehealth,
-
(5)
protected physician time for care coordination, and
-
(6)
an onsite extended interdisciplinary care team (ie, mental health, pharmacy, physical therapy).[30]
Combine individual-focused and structural or organizational interventions included Snoezelen,[21] stress management and resiliency training,[34] stress management workshops[18,20] and improving interaction with colleagues through personal training.[34] Training and follow-up were conducted by face-to-face,[27,31] phone,[20,31,35] e-mail,[27] video[20,31] or online,[18,20] and the timepoint of follow-up ranged from 0 to 7 years (Table 2 ).
4. Discussion
4.1. Summary of main findings
The purpose of this study was to summarize the evidence and clarify a bundled strategy to reduce burnout of physicians and nurses. According to ROBIS, 12 research were in low risk in domain 1, 8 in domain 2, 17 in domain 3, and 8 in phase 3. By using AMSTAR 2 to assess the methodological quality and quality of included research, most of those were considered as relatively good quality.
4.2. Implication for future study
Burnout of physicians and nurses has become a global public health problem. This overview analyzed the contents of 22 papers with results that physician-directed interventions are associated with small reductions in symptoms of common mental health disorders among physicians. Organizational interventions that ignore individual factors cannot really reducing burnout of physicians and nurses. Therefore, based on theories and studies, when physicians and nurses face stressors caused by work, they will make different coping strategies.[43] Coping refers to the “cognitive and behavioral efforts to manage specific external and/or internal demands that are appraised as taxing or exceeding the resources of the person”.[44]
Emotional intelligence theory suggests that emotion regulation skills facilitate the maintenance of appropriate emotions, reducing or adapting undesirable emotions in oneself and others.[28] Physicians and nurses constantly alternate between exhaustion and happiness, Resilience is the bridge from burnout to wellness.[45,46] Based on previous theories and studies, physicians and nurses experience a dynamic change between burnout and wellness. If positive intervention strategies can be adopted to enhance resilience, the incidence of burnout of physicians and nurses is greatly reduced and the wellness improved (Fig. 2).
Figure 2.

The path of bundle strategy to reduce burnout of physicians and nurses.
4.3. Strength and limitations
This research included studies in different settings, which brought to light the range of interventions, which could provide the direction for further research. The current overview clarified evidence to reduce burnout of physicians and nurses, which provide a basis for health policy makers or clinical managers to design simple and feasible strategies to reduce the burnout of physicians and nurses, and to ensure clinical safety. Considering partial databases selected and gray literature not included, the results are used only as an overview of the field.
5. Conclusion
This overview has included 22 systematic reviews and meta-analyses to summarize the relevant studies of interventions to reduce the burnout of physicians and nurses and form an evidence resource, which provides reliable evidence support for further intervention. It is an urgent need to implement and evaluate the long-term effect of bundle strategy.
Author contributions
XJZ, YQS and TYS designed, performed and analyzed the research. XJZ, YQS, TYS and TTJ advised on article inclusion and exclusion. XJZ and ND designed the Tables. XJZ, YQS and TTJ wrote the manuscript. XJZ, YQS, TTJ, ND and TYS read and revised the manuscript. All authors read and approved the final manuscript.
Footnotes
Abbreviations: AMSTAR 2 = assessment of multiple systematic reviews 2, RoB = risk of bias, ROBIS = the Risk of Bias in Systematic reviews, SRs = systematic reviews.
How to cite this article: Zhang Xj, Song Y, Jiang T, Ding N, Shi Ty. Interventions to reduce burnout of physicians and nurses: an overview of systematic reviews and meta-analyses. Medicine. 2020;99:26(e20992).
Xiu-jie Zhang and Ying-qian Song have the same contribution.
This study is supported by Basic Research Project of Higher Learning Institution in Liaoning Province (Code: LQ2017014), which provided financial support during data analysis and manuscript preparation.
Data availability statement No additional data available.
Patient and Public Involvement None.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
- [1].Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol 2001;52:397–422. [DOI] [PubMed] [Google Scholar]
- [2].Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA 2018;320:1131–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lo D, Wu F, Chan M, et al. A systematic review of burnout among doctors in China: a cultural perspective. Asia Pac Fam Med 2018;17:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dubale BW, Friedman LE, Chemali Z, et al. Systematic review of burnout among healthcare providers in sub-Saharan Africa. BMC Public Health 2019;19:1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015;90:1600–13. [DOI] [PubMed] [Google Scholar]
- [6].West CP. Physician well-being: expanding the triple aim. J Gen Intern Med 2016;31:458–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA 2011;305:2009–10. [DOI] [PubMed] [Google Scholar]
- [8].Rathert C, Williams ES, Linhart H. Evidence for the quadruple aim: a systematic review of the literature on physician burnout and patient outcomes. Med Care 2018;56:976–84. [DOI] [PubMed] [Google Scholar]
- [9].Kivimaki M, Jokela M, Nyberg ST, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 2015;386:1739–46. [DOI] [PubMed] [Google Scholar]
- [10].Shanafelt TD, Bradley KA, Wipf JE, et al. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002;136:358–67. [DOI] [PubMed] [Google Scholar]
- [11].Shin S, Park J-H, Bae S-H. Nurse staffing and nurse outcomes: a systematic review and meta-analysis. Nurs Outlook 2018;66:273–82. [DOI] [PubMed] [Google Scholar]
- [12].Prapanjaroensin A, Patrician PA, Vance DE. Conservation of resources theory in nurse burnout and patient safety. J Adv Nurs 2017;73:2558–65. [DOI] [PubMed] [Google Scholar]
- [13].Olszewski R, Owoc J, Manczak M, et al. How burnout affects errors among physicians: meta-analysis. Eur Heart J 2019;40:2578. [Google Scholar]
- [14].Panagioti M, Geraghty K, Johnson J, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med 2018;178:1317–30. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [15].Li H, Zhao M, Shi Y, et al. The effectiveness of aromatherapy and massage on stress management in nurses: a systematic review. J Clin Nurs 2019;28:372–85. [DOI] [PubMed] [Google Scholar]
- [16].Aryankhesal A, Mohammadibakhsh R, Hamidi Y, et al. Interventions on reducing burnout in physicians and nurses: a systematic review. Med J Islam Repub Iran 2019;33:77–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Canadas-De la Fuente GA, Ortega E, Ramirez-Baena L, et al. Gender, marital status, and children as risk factors for burnout in nurses: a meta-analytic study. Int J Environ Res Public Health 2018;15:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Dreison KC, Luther L, Bonfils KA, et al. Job burnout in mental health providers: a meta-analysis of 35 years of intervention research. J Occupational Health Psychol 2018;23:18–30. [DOI] [PubMed] [Google Scholar]
- [19].Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians a systematic review and meta-analysis. JAMA Intern Med 2017;177:195–205. [DOI] [PubMed] [Google Scholar]
- [20].Clough BA, March S, Chan RJ, et al. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev 2017;6:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Westermann C, Kozak A, Harling M, et al. Burnout intervention studies for inpatient elderly care nursing staff: systematic literature review. Int J Nurs Stud 2014;51:63–71. [DOI] [PubMed] [Google Scholar]
- [22].Kalani S, Azadfallah P, Oreyzi H, et al. Interventions for physician burnout: a systematic review of systematic reviews. Int J Prev Med 2018;9:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020;7:228–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7:e15–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Whiting P, Jelena S, Higgins JPT, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol 2016;69:225–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Petrie K, Crawford J, Baker STE, et al. Interventions to reduce symptoms of common mental disorders and suicidal ideation in physicians: a systematic review and meta-analysis. Lancet Psychiatry 2019;6:225–34. [DOI] [PubMed] [Google Scholar]
- [28].Jackson-Koku G, Grime P. Emotion regulation and burnout in doctors: a systematic review. Occup Med (Lond) 2019;69:9–21. [DOI] [PubMed] [Google Scholar]
- [29].Ghawadra SF, Abdullah KL, Choo WY, et al. Mindfulness-based stress reduction for psychological distress among nurses: a systematic review. J Clin Nurs 2019;28:3747–58. [DOI] [PubMed] [Google Scholar]
- [30].DeChant PF, Acs A, Rhee KB, et al. Effect of organization-directed workplace interventions on physician burnout: a systematic review. Mayo Clin Proc Innov Qual Outcomes 2019;3:384–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].De Simone S, Vargas M, Servillo G. Organizational strategies to reduce physician burnout: a systematic review and meta-analysis. Aging Clin Exp Res 2019;1–0. [DOI] [PubMed] [Google Scholar]
- [32].Cocchiara RA, Peruzzo M, Mannocci A, et al. The use of yoga to manage stress and burnout in healthcare workers: a systematic review. J Clin Med March 2019;8:284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Fibbins H, Ward PB, Watkins A, et al. Improving the health of mental health staff through exercise interventions: a systematic review. J Ment Health 2018;27:184–91. [DOI] [PubMed] [Google Scholar]
- [34].Romppanen J, Häggman-Laitila A. Interventions for nurses’ well-being at work: a quantitative systematic review. J Adv Nurs 2017;73:1555–69. [DOI] [PubMed] [Google Scholar]
- [35].Gilmartin H, Goyal A, Hamati MC, et al. Brief mindfulness practices for healthcare providers - a systematic literature review. Am J Med 2017;130:1211–9. [DOI] [PubMed] [Google Scholar]
- [36].Brand SL, Thompson Coon J, Fleming LE, et al. Whole-system approaches to improving the health and wellbeing of healthcare workers: a systematic review. PloS one 2017;12:e0188418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016;388:2272–81. [DOI] [PubMed] [Google Scholar]
- [38].Luken M, Sammons A. Systematic review of mindfulness practice for reducing job burnout. Am J Occup Ther 2016;70:1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Huan-Fang L, Chia-Chi K, Tsair-Wei C, et al. A meta-analysis of the effects of coping strategies on reducing nurse burnout. Appl Nurs Res 2016;31:100–10. [DOI] [PubMed] [Google Scholar]
- [40].Busireddy K, Jonathan M, Ellison KE, et al. Efficacy of interventions to reduce resident physician burnout: a systematic review. J Gen Intern Med 2016;9:294–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Stewart W, Terry L. Reducing burnout in nurses and care workers in secure settings. Nurs Stand 2014;28:37–45. [DOI] [PubMed] [Google Scholar]
- [42].Wiederhold BK, Cipresso P, Pizzioli D, et al. Intervention for physician burnout: a systematic review. Open Med (Wars) 2018;13:253–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Stewart MT, Reed S, Reese J, et al. Conceptual models for understanding physician burnout, professional fulfillment, and well-being. Curr Probl Pediatr Adolesc Health Care 2019;49:100658. [DOI] [PubMed] [Google Scholar]
- [44].Folkman S. Personal control and stress and coping processes: a theoretical analysis. J Pers Soc Psychol 1984;46:839–52. [DOI] [PubMed] [Google Scholar]
- [45].Mahmoud NN, Rothenberger D. From burnout to well-being: a focus on resilience. Clin Colon Rectal Surg 2019;32:415–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Murali K, Makker V, Lynch J, et al. From burnout to resilience: an update for oncologists. Am Soc Clin Oncol Educ Book 2018;38:862–72. [DOI] [PubMed] [Google Scholar]


