Abstract
Renal colic encounters are common; in the United States alone, they represent greater than one million annual emergency department (ED) visits. Most of these stones are managed conservatively with a trial of passage. However, some lead to repeat colic episodes, secondary ED visits, increased anxiety, and increased cost. Of the 5%–10% of symptomatic stones that become lodged at the ureteropelvic junction and are larger than 5 mm, most require operative intervention. In the process of executing a NASA‐funded study of ultrasonic repositioning of kidney stones, the subject was administered fluid to dilate the collecting system, placed in Trendelenburg bed positioning, and rolled to both sides. During this process a symptomatic, obstructing 9‐mm ureteropelvic junction stone moved back into the kidney's lower pole/infundibulum and symptoms were immediately resolved. The patient remained asymptomatic for a period of 5 weeks at which point elective intervention was scheduled. This case demonstrates that ureteropelvic junction stones may be repositioned in a non‐invasive manner, turning a stone that requires urgent intervention into one that can be managed electively.
1. INTRODUCTION
Symptomatic urolithiasis is a common disease, affecting an estimated 11% of men and 7% of women in their lifetime with high risk of recurrence. 1 , 2 Renal colic presentations are commonly associated with acute unilateral flank pain, vomiting, and urinary symptoms.
The majority of symptomatic stones are due to obstruction, which may cause reflexive spasm back pressure along the proximal ureter and kidney associated with hydronephrosis and hydroureter, which can be seen radiographically. Point‐of‐care ultrasound is an option for imaging as the ureterovesical junction or ureteropelvic junction where most stones are located have good acoustic windows. 3 Ultrasound has been shown to predict the need for urologic intervention in the case of uterolithiasis. 4 Ultrasound and computed tomography (CT) were previously compared in the domains of high‐risk diagnoses with complications, adverse events, return emergency department visits and hospitalization, and in that study shown to diagnose stones with similar effectiveness although dissimilar sensitivity. 3 The American Urological Association states that ultrasound is inferior to CT, and other emergency medicine experts have noted that CT has 94% sensitivity for stone versus 54% for ultrasound. 5 , 6 Although most renal stones can be expectantly managed without immediate intervention, ≈10% of patients will require admission or urologic intervention. 1 , 7 Additionally, passing large ureteropelvic junction kidney stones may take weeks, leading to patient anxiety, pain management requirements including opioids, as well as lost productivity or wages.
We present a case in which a symptomatic kidney stone lodged at the ureteropelvic junction was definitively repositioned with a minimally invasive maneuver consisting of hydration to dilate the renal pelvis plus gentle rocking of the patient in Trendelenburg position. The patient was originally enrolled in a National Aeronautics and Space Administration (NASA)‐funded study to investigate the use of ultrasonic propulsion, 8 , 9 a technology that uses an acoustic beam across a narrow region to apply force to potentially reposition symptomatic ureteropelvic junction stones.
In this case, ultrasonic propulsion was not required because the combination of bed angling and hydration obtained during diagnostic ultrasonography was sufficient to reposition a large stone back into the lower pole of the kidney. The patient remained asymptomatic for >5 weeks and did not require a ureteral stent until elective surgery was performed as an outpatient.
2. CASE REPORT
A 46‐year‐old man with history of cholecystectomy presented to a safety‐net ED with flank pain and gross hematuria. The pain was described as unilateral, aching, and intermittent, and nothing aggravated or alleviated the pain, except minimal relief from acetaminophen. Apart from a remote cholecystectomy, medical history was unremarkable. On physical examination, the patient had a pulse rate of 67, a blood pressure of 119/77 mm Hg, a respiratory rate of 18 breaths/min, a temporal temperature of 36.8°C, and an oxygen saturation of 99% on room air. The patient appeared uncomfortable and was continuously trying to find a comfortable position. Heart and lung examination was normal. His abdomen was non‐tender, soft, and non‐distended without palpable masses or signs of peritoneal irritation. The genitourinary examination revealed mild right flank tenderness to percussion. Physical examination was otherwise unremarkable.
Urinalysis findings were unremarkable with the exception of RBC count over 20/hpf; blood chemistry levels were normal including creatinine = 0.70 mg/dL; complete blood count was normal including a WBC count of 6.4 thousand/mL.
A non‐contrast abdomen and pelvis CT scan was obtained in prone position, demonstrating a 0.9 cm right‐sided stone at the ureteropelvic junction with mild prominence of the renal collecting system proximal to the stone and bilaterally decompressed ureters (Figures 1A and 1B). No secondary signs of infection were found.
FIGURE 1.
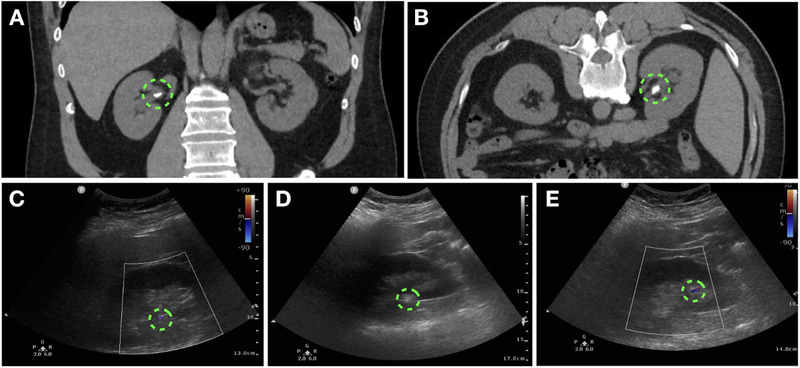
Repositioned ureteropelvic junction stone. (A) Coronal and (B) axial CT images with patient prone demonstrate a 9‐mm right ureteropelvic junction stone with mild hydronephrosis. A coronal ultrasound image prior to stone repositioning (C) shows the same 9‐mm echogenic calcification exhibiting the twinkling artifact at the ureteropelvic junction with no associated hydronephrosis. After hydration, the ultrasound image (D) reveals the same twinkling ureteropelvic junction stone and moderate hydronephrosis as dilation of the hypoechoic region within the kidney. After stone repositioning, (E) shows the stone apparent as echogenic and twinkling now in the lower pole of the kidney. Resolution of hydronephrosis is also seen. Supporting Information Videos S1–S3 correspond to the images (C)–(E)
The patient was enrolled in a research protocol 10 examining the potential for ultrasonic propulsion to reposition symptomatic obstructing ureteropelvic junction stones back into the lower pole of the kidney. Accordingly, the patient drank ≈1 L of water 20 min prior to this maneuver and coronal ultrasound views of the kidney and ureteropelvic junction/renal pelvis stone were obtained by an emergency physician who was fellowship‐trained in sonography with a Philips Sparq Machine (Royal Philips Electronics, Amsterdam) and a curvilinear scanhead (Figure 2).
FIGURE 2.
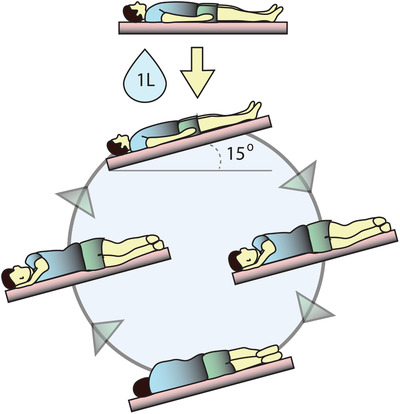
Repositioning a ureteropelvic junction stone. Depiction of the bedside maneuver including hydration, Trendelenburg bed positioning, and rocking from side to side
The patient initially moved gingerly because of stone discomfort and reported an initial pain score of 4/10 around the right flank. Ultrasound prior to intervention displayed no hydronephrosis (Figure 1C). After water, but prior to any maneuver, ultrasound revealed mild hydronephrosis (Figure 1D) with the stone located at the ureteropelvic junction. Along with hydration, the Seattle stone maneuver included the following: the patient was placed in 15° of Trendelenburg bed positioning and gently rocked from right to left lateral decubitus positioning to facilitate acoustic angles for stone visualization and ultrasonic propulsion. He was placed on the left for 5 min while we imaged and then on the right for 5 min and back to the left. The subject moved slowly in discomfort and required 1–2 min to roll over each time. After ≈20 min, the patient indicated a decreased pain score of 1.5/10 along the right flank, described as an ache, and stated that his pain was rapidly resolving. Prior to administration of any therapeutic ultrasonic pulses, re‐imaging with ultrasound revealed that the stone had moved to the target location, the lower pole collecting system, with resolution of hydronephrosis (Figure 1E). The patient smiled, spoke more, sat up for the first time immediately after the stone moved, and was later discharged from the ED asserting no pain. Later, a radiologist blinded to study conditions reviewed the associated ultrasound images and confirmed a change in stone location and resolution of hydronephrosis.
During ultrasound imaging at a follow‐up appointment 15 days later, the stone was noted to be asymptomatic and stably located in the lower pole. The patient scheduled outpatient stone intervention, and remained asymptomatic until an episode of renal colic requiring ED evaluation 5 weeks after initial presentation. The research team, the authors of this paper, were not the treating physicians and did not attempt any additional maneuvers at that time, because the patient's stone was not favorable for repositioning and he became asymptomatic after receiving pain medication. At this ED visit, laboratory studies were unremarkable including a normal serum creatinine, point‐of‐care ultrasound imaging showed the stone had returned to the ureteropelvic junction, and pain was managed with oral oxycodone. Conservative management was again initiated with outpatient follow‐up. The patient had successful elective laser lithotripsy 5 weeks after the second ED visit.
3. DISCUSSION
This case may highlight an alteration in the natural history of symptomatic urolithiasis at the ureteropelvic junction in which our intervention temporized a large symptomatic ureteropelvic junction stone back into the lower pole with resolution of hydronephrosis and symptoms over the course of minutes. We proposed that repositioning was accomplished via a simple, non‐invasive therapeutic maneuver involving hydration and patient positioning that has the potential to be easily reproducible for healthy, compliant patients. Notably, the patient remained asymptomatic for over 5 weeks, potentially demonstrating the ability of this maneuver to transform symptomatic stones near the ureteropelvic junction into events amenable to outpatient follow‐up with a urologist. Because ureteropelvic junction stones comprise ≈5%–10% of the over 1 million annual ED visits of symptomatic kidney stones in the United States, 11 this repositioning maneuver, if effective on a larger scale, could provide relief to thousands of patients per year in the United States alone, resulting in fewer emergent operating room cases or fewer admissions for symptom relief.
Our observations occurred in a subject who was enrolled for a prospective study funded by NASA investigating the use of ultrasound to reposition symptomatic stones. This study is of interest to NASA because a cosmonaut impacted by a renal stone nearly required an emergency deorbit, and ≈30 stone events have occurred within 2 years of flight. 12 , 13 Increased stone risk in flight is multifactorial: demineralization of bones in microgravity leading to increased urinary salts; decreased fluid intake in flight related to both availability and challenges associated with urination; increased ambient carbon dioxide levels altering urine pH and crystal formation; and medications prescribed for visual changes during flight. 12 Stones remain a potential unmitigated risk for NASA exploration class missions. Although the particular intervention described here would not work in the microgravity environment of space, the limited medical resources and challenges of performing procedures in space make quick and noninvasive approaches by which an obstructing ureteropelvic junction stone could be repositioned into the kidney to manage acute renal pain at least until surgical intervention can take place particularly valuable.
Our report is consistent with other described phenomena that indicate symptomatic obstructing stones are dynamic, and therefore, responsive to external mechanical forces and internal stimuli. For example, there are two previous case reports of retrograde peristalsis of symptomatic lower ureter stones depositing into the lower poles spontaneously, 14 , 15 inversion and percussion has been a longstanding therapy for clearance of intra‐kidney fragments after shock wave lithotripsy, 16 and rollercoasters have been demonstrated to help with passage of kidney stones, 17 as has ultrasonic propulsion observed by our own group. 8 Furthermore, we believe ureteropelvic junction stones are particularly amenable to mechanical attempts at repositioning because of the typical funnel‐shaped anatomy of the ureteropelvic junction, which becomes more pronounced with hydronephrosis. Additionally, the ureteropelvic junction is more relaxed due to the relative absence of alpha‐1 receptors as compared to the ureter near the ureterovesical junction. 18
This report is hypothesis generating; the degree to which Trendelenburg positioning, gravity, patient movement, and hydration for ureter pelvicalyceal dilation each contributes to mobility of stones from the ureteropelvic junction to the kidney requires further investigation. If proven effective, this maneuver has the potential to significantly impact management of acute stone symptoms at presentation in light of the relative ease of performance, few contraindications, and substantial benefit of successful symptom reduction. Our suggestion is that clinicians consider trying it.
4. CONCLUSIONS
We present a case of an ED patient in which a symptomatic kidney stone lodged at the ureteropelvic junction was repositioned back into the kidney. Proximal stone movement was temporally related to administration of fluids, Trendelenburg bed angling, and patient positioning. The relationship of symptom resolution with these procedures indicates that non‐invasive repositioning of proximal/ureteropelvic junction stones may be possible. Controlled proof of concept studies will be required before this procedure (the Seattle stone maneuver) can be recommended for routine use, but with little apparent risk, it may be possible to try it or suggest to patients to try it with stones right at the ureteropelvic junction.
CONFLICTS OF INTEREST
Michael Bailey has a consulting agreement with and equity in SonoMotion, Inc., which has licensed from the University of Washington the ultrasonic propulsion technology mentioned in this article.
ACKNOWLEDGMENTS
The clinical trial where this work took place is supported by a contract from ZIN Technologies, Inc. and NASA. The technology being tested in this study is the result of funding from NASA and NIH NIDDK (P01 DK043881).
Hall MK, Samson PC, Kessler R, et al. Pearl‐unjammed: the Seattle stone maneuver for ureteropelvic junction urolithiasis. JACEP Open. 2020;1:252–256. 10.1002/emp2.12047
Supervising Editor: Steven G. Rothrock, MD
REFERENCES
- 1. Wang R. Managing urolithiasis. Ann Emerg Med. 2016;67(4):449‐454. 10.1016/j.annemergmed.2015.10.021 [DOI] [PubMed] [Google Scholar]
- 2. Scales CD, Lin L, Saigal CS, et al. Emergency department revisits for patients with kidney stones in California. Acad Emerg Med. 2015;22(4):468‐474. 10.1111/acem.12632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Smith‐Bindman R, Aubin C, Bailitz J, et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N Engl J Med. 2014;371(12):1100‐1110. 10.1056/NEJMoa1404446 [DOI] [PubMed] [Google Scholar]
- 4. Edmonds ML, Yan JW, Sedran RJ, et al., The utility of renal ultrasonography in the diagnosis of renal colic in emergency department patients. CJEM. 2010;12(3):201‐206. [DOI] [PubMed] [Google Scholar]
- 5. Pearl MS, Goldfarb DS, Assimos, DG , et al. Medical management of kidney stones/2019 guidelines 2019. Available at: https://www.auanet.org/guidelines/kidney-stones-medical-mangement-guideline
- 6. Corbo J, Wang J. Kidney and ureteral stones. Emerg Med Clin North Am. 2019;37(4):637‐648. [DOI] [PubMed] [Google Scholar]
- 7. Wang RC, Rodriguez RM, Fahimi J, et al. Derivation of decision rules to predict clinically important outcomes in acute flank pain patients. Am J Emerg Med. 2016;35(4):554‐563. 10.1016/j.ajem.2016.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Harper JD, Cunitz BW, Dunmire B, et al. First in human clinical trial of ultrasonic propulsion of kidney stones. J Urol. 2016;195(4 Pt 1):956‐964. 10.1016/j.juro.2015.10.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dai JC, Sorensen MD, Chang HC, et al. Quantitative assessment of effectiveness of ultrasonic propulsion of kidney stones. J Endourol. 2019;33(10):850‐857. 10.1089/end.2019.0340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Simon JC, Dunmire B, Bailey MR, Sorensen MD. Developing complete ultrasonic management of kidney stones for spaceflight. J Space Saf Eng. 2016;3(2):50‐57. 10.1016/S2468-8967(16)30018-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Foster G, Stocks C, Borofsky MS. Emergency Department Visits and Hospital Admissions for Kidney Stone Disease, 2009: Statistical Brief #139. February 2006. [PubMed]
- 12. Sibonga JD, Pietrzyk RA. Human Research Program, Human Health Countermeasures Element, Evidence Book. Houston, TX; 2017:1‐26. Available at: https://humanresearchroadmap.nasa.gov/Evidence/ [Google Scholar]
- 13. Buckey JC. Space Physiology. In: Barratt MR, Pool SL, eds. New York, NY: Oxford University Press; 2006:239‐262. [Google Scholar]
- 14. Fallatah M, Tahaineh S, Abu Mughli R, Fallatah SM. Upward migration of a ureteric stone in a military trainer: a case report. Res Rep Urol. 2017;9:15‐17. 10.2147/RRU.S124200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Khan Z, Yaqoob AA, Bhatty TA. Spontaneous retrograde migration of ureterovesical junction stone to the kidney; first ever reported case in the English literature in human. Urol Ann. 2016;8(2):229‐232. 10.4103/0974-7796.176869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chiong E, Hwee STP, Kay LM, Liang S, Kamaraj R, Esuvaranathan K. Randomized controlled study of mechanical percussion, diuresis, and inversion therapy to assist passage of lower pole renal calculi after shock wave lithotripsy. Urology. 2005;65(6):1070‐1074. 10.1016/j.urology.2004.12.045 [DOI] [PubMed] [Google Scholar]
- 17. Mitchell MA, Wartinger DD. Validation of a functional pyelocalyceal renal model for the evaluation of renal calculi passage while riding a roller coaster. J Am Osteopath Assoc. 2016;116(10):647‐652. 10.7556/jaoa.2016.128 [DOI] [PubMed] [Google Scholar]
- 18. Lipkin M, Shah O. The use of alpha‐blockers for the treatment of nephrolithiasis. Rev Urol. 2006;8(Suppl 4):S35‐S42. [PMC free article] [PubMed] [Google Scholar]


