Abstract
Background/Aims
The functional luminal imaging probe (FLIP) can measure tissue distensibility and geometric changes through volumetric distention. The esophagogastric junction has been well studied using EndoFLIP, studies on pylorus are lacking. We aim to study biomechanical properties of pylorus using EndoFLIP to create normative data.
Methods
We performed a prospective study of 20 healthy volunteers (ages, 18-54 years; 10 men) who underwent pylorus evaluation using 12-cm FLIP placed across the pyloric sphincter. FLIP data were analyzed using FLIP planimetry plots at baseline and after administration of hyoscine butyl bromide injection.
Results
The median pylorus distensibility index (P-DI) was 8.37 mm2/mmHg (interquartile range, 4.22-13.04 mm2/mmHg) at 40 mL balloon volume. The 90th percentile at 40 mL balloon for P-DI was 14.89 mm2/mmHg, for cross-sectional area was 244.20 mm2/mmHg, and diameter and pressure were 17.58 mm and 48.84 mmHg, respectively. There was significant increase in P-DI after administration of hyoscine butyl bromide injection (P < 0.05).
Conclusion
The normative values can be used as reference values for pyloric distensibility. This reference can be used in studies of related to pyloric diseases such as gastroparesis.
Keywords: Gastroparesis, Manometry, Pylorus
Introduction
The functional luminal imaging probe (FLIP) uses the principles of high-resolution impedance planimetry to study biomechanical properties of the gastrointestinal sphincters such as esophagogastric junction (EGJ).1,2 EndoFLIP can measure tissue distensibility and geometric changes through volumetric distention with real-time images. FLIP has emerged as a valuable tool for evaluation of diseases such as achalasia cardia, eosinophilic esophagitis, and other esophageal motility disorders. EndoFLIP features of the lower esophageal sphincter and EGJ have been extensively characterized.1
Pyloric sphincter is physiologically crucial in the regulation of gastric emptying. Although there has been a longstanding interest in understanding pyloric mechanisms and therapies for conditions like gastroparesis, this has been hampered by the lack of appropriate tools for pyloric assessment.3,4 Techniques like antro-duodenal manometry are time consuming and have sparse availability with limitations to measure compliance of the sphincteric region although it can assess antro-duodenal peristalsis.5 Therefore, EndoFLIP has been proposed to be a novel and complimentary assessment strategy for assessment of pyloric function in humans.
A subset of gastroparesis patients has long been known to have pyloric dysfunction. Paralytic strategies into the pylorus (eg, botulinum toxin) have been largely unsuccessful due to non-targeted inclusion of patients without a comprehensive assessment of pyloric function. With the advent of Gastric Per Oral Endoscopic Myotomy (G-POEM), endoscopic gastric electrical stimulation, and pyloroplasty, there is a resurgence in the interest for an augmented functional assessment of the pylorus.6,7 Additionally, this may be helpful to design instruments targeting duodenum such as Duodenum-Jejunal Bypass Liners. As the pylorus is a physiological sphincter, its physiology can be studied using FLIP. However, a reference database of pyloric EndoFLIP parameters in healthy individuals is lacking. We aim to evaluate the motor activity of pyloric sphincter using EndoFLIP parameters such as pressure, diameter, cross-sectional area (CSA), and distensibility in healthy women and men at rest and after injection of hyoscine, an antispasmodic. We hypothesize that there will be gender-based differences in pyloric function and significant changes in distensibility of the pylorus after administration of hyoscine. An overarching goal is to provide a normogram which can be used for evaluation of pyloric function in conditions like gastroparesis and to design novel Duodenum-Jejunal Bypass liners for treatment of obesity and diabetes.
Materials and Methods
The authors declare that the study was performed in a manner to conform to the Helsinki Declaration of 1975, as revised in 2000 and 2008, concerning human and animal rights. The protocol was approved by the Institutional Ethics Committee of Asian Institute of Gastroenterology (Approval No. AIG/IEC30/09.2017-03) and informed consent was obtained from the study subjects. The authors are responsible for the findings and the contents of the paper. Healthy Indian adult volunteers who are free of gastric or esophageal symptoms were invited to participate. Potential candidates were excluded if they had a prior historical diagnosis of esophageal or gastric disease.
The exclusion criteria also included use of antacids or proton pump inhibitors, use of opioids or anti-cholinergic medications, body mass index (BMI) more than 30 kg/m2, previous history of upper abdominal surgery, and tobacco or alcohol consumption. Volunteers were also excluded if there was any evidence of functional gastrointestinal disorders. Quality of life and overall dyspeptic symptoms were assessed by Gastrointestinal Quality of Life Index (GIQLI). The GIQLI score varies from 0 (worst quality of life possible) to 144 (best quality of life). Volunteers with a GIQLI score less than 125 were also excluded.
EndoFLIP Method
The subjects fasted for at least 8 hours prior to the study. The study was performed under sedation using monitored anesthesia (propofol) in the left lateral decubitus position. Initial endoscopic examination was performed to assess anatomy for stomach, pylorus, and duodenum. The EndoFLIP (EF-322N; Medtronic, Inc, Shoreview, MN, USA) is a catheter of 2.8 mm outer diameter with 16 serial impendence electrodes spaced 8 mm apart which is enclosed in a 12-cm long compliant balloon. The balloon is connected to a pump which allows 0 mL to 60 mL of solution in and out. Balloon was calibrated to atmospheric pressure before placement. An EndoFLIP catheter was passed along the endoscope into the pylorus under direct endoscopic visualization. The second portion of duodenum is not a natural sphincter like pylorus. EndoFLIP measurements were done when there was single waist in EndoFLIP graphs indicating that there was no interference due to the second portion of the duodenum.
The pylorus was assessed stepwise by distending the balloon with the volume of EndoFLIP at 20, 30, 40, and 50 mL balloon volume distensions. Each stepwise distension volume was maintained for 30 seconds to 60 seconds (Machine EndoFLIP Model EF-100 with Revision D software; Medtronic, Inc). Pressure was measured by a pressure transducer inside the balloon. CSA was measured using impedance planimetry based on Ohm’s law. The narrowest diameter was recorded. To ensure internal repeatability and consistency at least 3 recordings were made and the average of 3 readings was recorded. These measurements were assessed at each balloon distension for minimum of 5 seconds. Distensibility was calculated as minimum CSA/pressure at each balloon fill volume. Once the EndoFLIP measurements completed at rest, 10 mg of hyoscine was administered intravascularly, and the same measurements were repeated.
Statistical Methods
Data were collected using standard proforma and recorded into a Microsoft Excel sheet (version 15.21.1; Microsoft Corp, Redmond, WA, USA) Database. Qualitative data were expressed as percentage and quantitative data as mean with standard deviation or median with interquartile range (IQR) as appropriate. Baseline and post injection hyoscine parameters were compared using paired t test. The correlation between age, height, weight and BMI with pylorus distensibility index (P-DI) was done with Pearson’s correlation coefficient. The P-value less than 0.05 was considered as statistically significant. For data analysis the SPSS statistical software (version 23.0.1; IBM Corp, Armonk, NY, USA) was used.
Results
Twenty healthy volunteers were evaluated, with mean age of 34.4 (range, 18-54) years and 10 (50%) were men. The mean (SD) of height, weight, and BMI was 167 (7.9) cm, 66.5 (7.1) kg, and 23.81 (0.96) kg/m2, respectively. Esophagogastroduodenoscopy was normal in all subjects. None of the subjects had any evidence of organic or functional gastrointestinal disorders. None of the subjects were on any medications in the previous 3 months. Mean GIQLI score was 134 ± 5.
Fasting Pylorus Compliance and Pressure
The baseline parameters for balloon inflation at 20, 30, 40, and 50 mL are summarized in Table 1. The median P-DI was 8.37 (IQR, 4.22-13.04) mm2/mmHg at 40 mL balloon volume. The median narrowest pylorus CSA was 133 (IQR, 78.25-181.75) mm2 with corresponding diameter of 13 (IQR, 9.9-15.2) mm, and the median intra-balloon pressure was 20.3 (IQR, 7.7-37) mmHg. The 90th percentile at 40 mL balloon for P-DI was 14.89 mm2/mmHg, for CSA was 244.20 mm2, and diameter and pressure were 17.58 mm and 48.84 mmHg, respectively. There was no statistically significant difference between male and female volunteers at baseline. There was a trend towards negative correlation in distensibility with increasing age, however is has not reached statistical significance level (P > 0.05). Similarly, we did not find significant correlation of height, weight and BMI with distensibility (P > 0.05).
Table 1.
Normative Values at Baseline
| Balloon volume | Overall | Male | Female |
|---|---|---|---|
| 20 mL | |||
| Diameter (mm) | 6.36 (1.77) | 6.21 (2.09) | 6.5 (1.49) |
| Pressure (mmHg) | 18.44 (13.91) | 17.82 (14.46) | 19.05 (14.09) |
| CSA (mm2) | 29.65 (12.20) | 24.50 (5.72) | 34.8 (14.91) |
| Distensibility index (mm2/mmHg) | 2.79 (2.29) | 2.52 (2.16) | 3.05 (2.49) |
| 30 mL | |||
| Diameter (mm) | 9.97 (3.57) | 8.72 (3.83) | 11.22 (2.97) |
| Pressure (mm Hg) | 14.46 (11.46) | 12.68 (10.32) | 16.24 (12.80) |
| CSA (mm2) | 86.45 (57.15) | 67.70 (53.43) | 105.20 (57.09) |
| Distensibility index (mm2/mmHg) | 8.86 (7.12) | 7.65 (7.53) | 10.07 (6.86) |
| 40 mL | |||
| Diameter (mm) | 13.01 (3.37) | 12.7 (2.82) | 13.32 (3.97) |
| Pressure (mm Hg) | 23.62 (15.28) | 20.3 (14.83) | 26.94 (15.76) |
| CSA (mm2) | 141.70 (75.04) | 17.77 (56.19) | 150.80 (92.45) |
| Distensibility index (mm2/mmHg) | 8.42 (4.69) | 9.07 (4.92) | 7.77 (4.62) |
| 50 mL | |||
| Diameter (mm) | 15.38 (3.21) | 15.46 (3.27) | 15.3 (3.32) |
| Pressure (mmHg) | 38.02 (18.95) | 30.50 (18.95) | 45.53 (16.53) |
| CSA (mm2) | 193.40 (80.65) | 195.40 (80.94) | 191.40 (84.69) |
| Distensibility index (mm2/mmHg) | 7.56 (6.33) | 9.89 (7.53) | 5.23 (3.97) |
CSA, cross-sectional area.
Values are expressed as mean (SD).
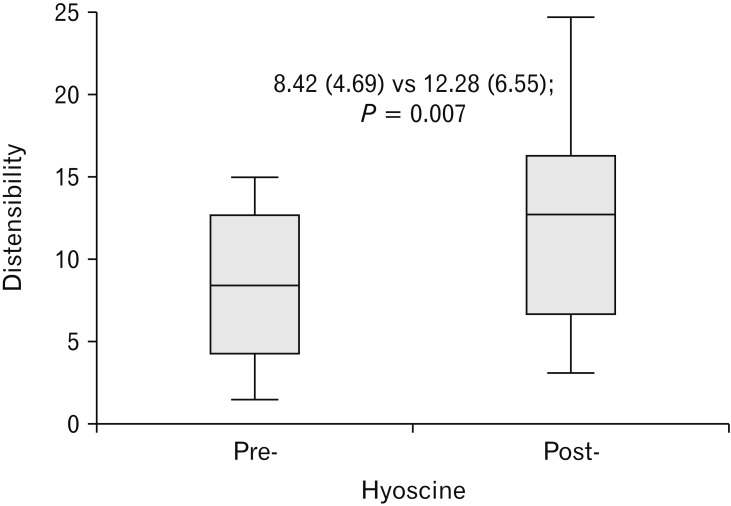
Fasting Pylorus Compliance and Pressure After Hyoscine Administration (See Figure)
Figure.
Effect of injection hyoscine butylbromide on pylorus distensibility at 40 mL balloon distention.
The median P-DI was 12.69 (IQR, 6.28-16.67) mm2/mmHg at 40 mL balloon volume. The median narrowest pylorus CSA was 176 (IQR, 115.5-199.3) mm2 with corresponding diameter of 14.3 (IQR, 12.13-15.90) mm, and the median intra-balloon pressure was 15.25 (IQR, 8.25-32.48) mmHg. The 90th percentile at 40 mL balloon after hyoscine administration for P-DI was 22.11 mm2/mmHg, for CSA was 274 mm2, and diameter and pressure were 18.65 mm and 43.60 mmHg, respectively.
There was a statistically significant increase in distensibility after administration of hyoscine at 20 mL balloon (2.79 ± 2.29 vs 8.19 ± 9.23, P = 0.013); at 30 mL balloon (8.86 ± 7.12 vs 13.97 ± 10.44, P = 0.012); at 40 mL balloon (8.42 ± 4.69 vs 12.28 ± 6.55, P = 0.007); and at 50 mL balloon (7.56 ± 6.33 vs 11.87 ± 11.64, P = 0.043) as shown in Table 2.
Table 2.
Pylorus Distensibility Index––Baseline and Post-hyoscine Administration
| Balloon volume | Overall | Male | Female | |||
|---|---|---|---|---|---|---|
| Baseline | Post-hyoscine | Baseline | Post-hyoscine | Baseline | Post-hyoscine | |
| 20 mL | 2.79 (2.29)a | 8.19 (9.23) | 2.52 (2.16) | 8.91 (4.94) | 3.05 (2.59) | 7.47 (2.92) |
| 30 mL | 8.86 (7.12)a | 13.97 (10.44) | 2.65 (5.07)a | 16.10 (12.12) | 10.07 (7.57) | 11.84 (10.41) |
| 40 mL | 8.42 (4.69)a | 12.28 (6.55) | 9.07 (7.22)a | 13.99 (14.32) | 7.77 (9.99) | 10.56 (8.87) |
| 50 mL | 7.56 (6.33)a | 11.87 (11.64) | 9.89 (6.91) | 12.24 (9.30) | 5.23 (4.56) | 11.50 (7.24) |
Indicates statistical significance P < 0.05.
Values are expressed as mean (SD).
In male volunteers, there was statistically significant difference of increase in distensibility after administration of hyoscine at 30 mL and 40 mL balloon (7.65 ± 4.92 vs 16.10 ± 13.55, P = 0.017 and 9.07 ± 4.92 vs 13.99 ± 5.31, P = 0.028). Though at 20 mL and 50 mL balloon, there was increase in distensibility after hyoscine administration it has not reached level of significance (2.52 ± 2.16 vs 8.19 ± 9.48, P = 0.051 and 9.89 ± 7.53 vs 12.24 ± 7.29, P = 0.148). In female volunteers, there was no statistically significant change in distensibility after hyoscine administration at all balloon volumes; though numerically post-hyoscine values were more than baseline as shown in Table 2.
There is positive correlation between diameter and CSA at 40 mL balloon volume (Pearson’s correlation coefficient = 0.99, P < 0.001) and negative correlation between pressure and distensibility at 40 mL balloon volume (Pearson’s correlation coefficient = –0.74, P < 0.001) at baseline.
Discussion
EndoFLIP as a novel technique to assess pyloric sphincter physiologic characteristics, specifically the diameter, length, pressure, CSA, and distensibility.2 In our study, we evaluated the fasting pylorus compliance and pressure with balloon distension at 20, 30, 40, and 50 mL, respectively pre- and post-administration of intravenous hyoscine. The 90th percentile at 40 mL balloon for P-DI was 14.89 mm2/mmHg, for CSA was 244.2 mm2, and diameter and pressure were 17.58 mm and 48.84 mmHg, respectively. These values can be used as a normogram to evaluate pyloric channel related diseases such as gastroparesis. However, median pyloric distensibility in the current study was lower than a previously published study, this difference may be due to different ethnical and racial populations.8 We found a statistically significant increase of distensibility after administration of hyoscine at 20, 30, 40, and 50 mL balloon distension, respectively. This suggests that EndoFLIP based assessment of pyloric function are dynamic and responsive to pharmacological stimuli. Gourcerol et al8 have evaluated fasting pyloric compliance in gastroparesis and compared it with healthy volunteers and in patients who had undergone esophagectomy without pyloroplasty. Ninety percentile cut-off for compliance in healthy volunteers at 40 mL of inflation was 10 mm2/mmHg, in the present study it was 14.89 mm2/mmHg. The pylorus is more distensible than the lower esophageal sphincter since the pylorus is not affected by stiffness of the diaphragm.9 The median EGJ distensibility index was 5.8 (IQR, 4.9-6.7) mm2/mmHg at 60 mL balloon volume.10
This is the first study to determine the pyloric sphincter physiology using the EndoFLIP technique in healthy women and men. In addition, changes in pyloric parameters following hyoscine injection suggest that EndoFLIP can be used to determine responsiveness to pharmacological agents. There is a statistical significance in the pyloric sphincter physiology parameters post-hyoscine injection, more precisely with 40 mL balloon distension. These changes after hyoscine administration will provide dynamic alterations in pyloric function. There is no gender difference in pyloric compliance at baseline. This study could not achieve significant change in distensibility of the pylorus in gender subgroups post-hyoscine administration, though numerically values are higher after hyoscine administration in men and women. This could be due to the low number of samples. There was nonsignificant trend towards decreased pyloric with increasing age. Similarly, we did not find significant difference with height, weight, or BMI. Pyloric distensibility may be affected by obesity, but the current study has excluded obese patients, and mean BMI (SD) in this study was 23.81 (0.96) kg/m2. In the current study, we also found that there is positive correlation between diameter and CSA and negative correlation between pressure and distensibility. This could be inferenced as pyloric distensibility that may be low at high pressure meaning basal pyloric tone or intrinsic fasting pressure of pyloric channel affects distensibility. Hyoscine butylbromide is an anticholinergic drug with high affinity for muscarinic receptors of smooth muscle cells of the gastrointestinal tract.11 Similar to botulinum, it can block excessive cholinergic activity and allows pyloric sphincter to relax and increase its distensibility.12,13 Our study has opened a new paradigm to predict pyloric responsiveness to pharmacotherapy which can be utilized to test agents targeted at the pylorus sphincter and to potentially predict response to endoscopic therapies like G-POEM, and design novel Duodenum-Jejunal Bypass Liners to prevent device migration.
The pylorus is an important gastrointestinal sphincter which controls the flow of content between the stomach and duodenum. It is a zone of elevated pressure that relaxes with antral peristalsis and contracts in response to physiological duodenal stimuli.14 The pyloric diameter is controlled by the tonic contraction of the distal pyloric ring, which sets the baseline resistance to flow.15 The pyloric tone and flow resistance is affected by nutrient foods and acid secretion.16
The pyloric activity was previously studied using dynamic contrast radiography, in conjunction with pressure transducers,15,17 which demonstrated that pyloric tonic activity controls the luminal diameter and flow resistance with patent pylorus much of the time. Apart from this, antroduodenal manometry can be used to assess pyloric function. However, it regularly misses contractile activity and interferes with some pyloric functions.18,19 Two reflexes, namely the antro-sphincteric inhibitory reflex and sphinctero-antral excitatory reflex act to churn and allow transport of gastric contents to the duodenum which are studied using manometry.20 The previous study in the patients with gastroparesis has shown that there is a wide range in distensibility of the pylorus (1-55 mm2/mmHg) with inverse symptoms correlation, mainly of early satiety and postprandial fullness with pyloric sphincter diameter and CSA.21 Another study has shown that fasting pylorus compliance is decreased in patients with gastroparesis and is inversely correlated with gastric emptying time.8 Pyloric dilatation in low pyloric compliance patients showed improvement in GIQLI in the same study.8
Earliest studies have demonstrated that the pylorus is a true physiological sphincter using measuring Potential Difference between stomach and duodenum with high pressure zone in between the two.14 Few studies have demonstrated pyloric compliance as a new relevant metric in gastroparesis patients, and may be useful to target such patients for pyloric dilatation or botulinum toxin injection.8,21 The isolated pyloric pressure waves are confined to a narrow pyloric zone which can be stimulated by ingestion or intra-duodenal infusion. The suppression of antral contractility with isolated pyloric pressure waves leads to cessation or decrease of trans-pyloric transport.22 Prominent and persistently uninterrupted isolated pyloric waves are implicated as a pathophysiological abnormality causing diabetic gastroparesis. Attenuation of isolated pyloric pressure waves by botulinum toxin injection with symptomatic improvement the suggests role of pyloric dysmotility in diabetic gastroparesis.23
In our study, we could not perform antro-duodenal manometry and gastric emptying studies in the study population to compare it with the EndoFLIP parameters. Additionally, we relied on the GIQLI score to ensure enrollment of subjects without organic and functional gastrointestinal disease. Volunteers with a GIQLI score less than 125 were excluded. The small sample size may lead to bias and compromise our results.
In summary, these pyloric physiological findings in healthy women and men create baseline values that will be helpful for multiple reasons. This assessment of the pyloric sphincter may be useful in the future to decide the subset of patients who would benefit from pyloric sphincter targeted therapies. Subjects with a small diameter and low distensibility pylorus would benefit compared to large diameter, high distensibility, and pylorus sphincter. Additionally, these will aid bioengineering and development of new Duodenum-Jejunal Bypass Liners useful in treating obesity and diabetes. Further studies combining EndoFLIP with high-resolution measurement of gastro-duodenal manometric parameters will help in tackling select subjects with pyloric sphincter abnormalities. More broadly, a rapid advancement in these techniques is critically needed as the G-POEM sees an expansion in management of gastroparesis patients.
Acknowledgments
Acknowlegements: All authors acknowledge Metamodix Inc, Plymouth, MN, USA for providing technical support in this research.
Footnotes
Financial support: None.
Conflicts of interest: None.
Author contributions: Nitin Jagtap and Rakesh Kalapala had designed the study, acquired data, critically analyzed data, and prepared manuscript; D Nageshwar Reddy gave important intellectual inputs and critically revised article; and Nitin Jagtap is guarantor of the article. All authors gave final approval of the manuscript.
References
- 1.Kwiatek MA, Pandolfino JE, Hirano I, Kahrilas PJ. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP) Gastrointest Endosc. 2010;72:272–278. doi: 10.1016/j.gie.2010.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hirano I, Pandolfino JE, Boeckxstaens GE. Functional lumen imaging probe for the management of esophageal disorders: expert review from the clinical practice updates committee of the AGA institute. Clin Gastroenterol Hepatol. 2017;15:325–334. doi: 10.1016/j.cgh.2016.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramkumar D, Schulze KS. The pylorus. Neurogastroenterol Motil. 2005;17(suppl 1):22–30. doi: 10.1111/j.1365-2982.2005.00664.x. [DOI] [PubMed] [Google Scholar]
- 4.Armitage AK, Dean AC. Function of the pylorus and pyloric antrum in gastric emptying. Gut. 1963;4:174–178. doi: 10.1136/gut.4.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patcharatrakul T, Gonlachanvit S. Technique of functional and motility test: how to perform antroduodenal manometry. J Neurogastroenterol Motil. 2013;19:395–404. doi: 10.5056/jnm.2013.19.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh S, McCrary J, Kedar A, et al. Temporary endoscopic stimulation in gastroparesis-like syndrome. J Neurogastroenterol Motil. 2015;21:520–527. doi: 10.5056/jnm15046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim BJ, Kuo B. Gastroparesis and functional dyspepsia: a blurring distinction of pathophysiology and treatment. J Neurogastroenterol Motil. 2019;25:27–35. doi: 10.5056/jnm18162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gourcerol G, Tissier F, Melchior C, et al. Impaired fasting pyloric compliance in gastroparesis and the therapeutic response to pyloric dilatation. Aliment Pharmacol Ther. 2015;41:360–367. doi: 10.1111/apt.13053. [DOI] [PubMed] [Google Scholar]
- 9.Snape WJ, Lin MS, Agarwal N, Shaw RE. Evaluation of the pylorus with concurrent intraluminal pressure and EndoFLIP in patients with nausea and vomiting. Neurogastroenterol Motil. 2016;28:758–764. doi: 10.1111/nmo.12772. [DOI] [PubMed] [Google Scholar]
- 10.Carlson DA, Kou W, Lin Z, et al. Normal values of esophageal distensibility and distension-induced contractility measured by functional luminal imaging probe panometry. Clin Gastroenterol Hepatol. 2019;17:674–681.:e1. doi: 10.1016/j.cgh.2018.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tytgat GN. Hyoscine butylbromide: a review of its use in the treatment of abdominal cramping and pain. Drugs. 2007;67:1343–1357. doi: 10.2165/00003495-200767090-00007. [DOI] [PubMed] [Google Scholar]
- 12.Ukleja A, Tandon K, Shah K, Alvarez A. Endoscopic botox injections in therapy of refractory gastroparesis. World J Gastrointest Endosc. 2015;7:790–798. doi: 10.4253/wjge.v7.i8.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ezzeddine D, Jit R, Katz N, Gopalswamy N, Bhutani MS. Pyloric injection of botulinum toxin for treatment of diabetic gastroparesis. Gastrointest Endosc. 2002;55:920–923. doi: 10.1067/mge.2002.124739. [DOI] [PubMed] [Google Scholar]
- 14.Fisher R, Cohen S. Physiological characteristics of the human pyloric sphincter. Gastroenterology. 1973;64:67–75. doi: 10.1016/S0016-5085(73)80092-7. [DOI] [PubMed] [Google Scholar]
- 15.Dillard S, Krishnan S, Udaykumar HS. Mechanics of flow and mixing at antroduodenal junction. World J Gastroenterol. 2007;13:1365–1371. doi: 10.3748/wjg.v13.i9.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keinke O, Schemann M, Ehrlein HJ. Mechanical factors regulating gastric emptying of viscous nutrient meals in dogs. Q J Exp Physiol. 1984;69:781–795. doi: 10.1113/expphysiol.1984.sp002868. [DOI] [PubMed] [Google Scholar]
- 17.Malbert CH, Ruckebusch Y. Duodenal pH dips as an index of transpyloric flow in conscious dogs. Gastroenterology. 1993;105:755–763. doi: 10.1016/0016-5085(93)90893-H. [DOI] [PubMed] [Google Scholar]
- 18.Indireshkumar K, Brasseur JG, Faas H, et al. Relative contributions of “pressure pump” and “peristaltic pump” to gastric emptying. Am J Physiol Gastrointest Liver Physiol. 2000;278:G604–G616. doi: 10.1152/ajpgi.2000.278.4.G604. [DOI] [PubMed] [Google Scholar]
- 19.Boulby P, Moore R, Gowland P, Spiller RC. Fat delays emptying but increases forward and backward antral flow as assessed by flow-sensitive magnetic resonance imaging. Neurogastroenterol Motil. 1999;11:27–36. doi: 10.1046/j.1365-2982.1999.00133.x. [DOI] [PubMed] [Google Scholar]
- 20.Shafik A, El Sibai O, Shafik AA, Shafik IA. Mechanism of gastric emptying through the pyloric sphincter: a human study. Med Sci Monit. 2007;13:CR24–CR29. [PubMed] [Google Scholar]
- 21.Malik Z, Sankineni A, Parkman HP. Assessing pyloric sphincter pathophysiology using EndoFLIP in patients with gastroparesis. Neurogastroenterol Motil. 2015;27:524–531. doi: 10.1111/nmo.12522. [DOI] [PubMed] [Google Scholar]
- 22.Heddle R, Dent J, Toouli J, Read NW. Topography and measurement of pyloric pressure waves and tone in humans. Am J Physiol. 1988;255(4 Pt 1):G490–G497. doi: 10.1152/ajpgi.1988.255.4.G490. [DOI] [PubMed] [Google Scholar]
- 23.Gupta P, Rao SS. Attenuation of isolated pyloric pressure waves in gastroparesis in response to botulinum toxin injection: a case report. Gastrointest Endosc. 2002;56:770–772. doi: 10.1016/S0016-5107(02)70140-5. [DOI] [PubMed] [Google Scholar]