Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has had a significant impact on practical activities and didactic teaching of residents and fellows. This survey aimed to propose long-term changes for ophthalmology training based on the changes experienced by trainees and their perception of new training opportunities.
Methods
An online survey was distributed to ophthalmology trainees in multiple countries. Descriptive statistics were used to analyse the data.
Results
A total of 504 analyzable responses were collected from 32 different countries. The current impact of COVID-19 pandemic was described as “severe” by most trainees (55.2%); however, the future perspective was more optimistic as demonstrated by the greater number of responses reporting a presumed “moderate” (37.3%), “mild” (14.1%) or “slight” (4.2%) long-term impact. The vast majority of trainees reported a decrease ≥50% of clinical activity (76.4%) and >75% of surgical activity (74.6%). Although an initial gap in didactic teaching has been experienced by many (55.4%), regular web-based teaching was reportedly attended by 67.7% of the respondents. A strong agreement was found regarding the worthwhile role of web-based case-presentations in clinical training (91.7%), web-based discussion of edited surgical videos (85.7%) and simulation-based practice (86.9%) in surgical training.
Conclusions
This survey, focusing on trainees’ perspective, strongly reinforces the need to promptly include new technology-based training tools, such as web-based teaching, virtual surgical simulators, and telementoring, in long-term reorganisation of ophthalmology training to ensure its continuity and effectiveness, which would remain available even in the face of another unpredictable crisis within the health system.
Subject terms: Education, Events
Introduction
The current coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), led to a global crisis within health systems, which had a knock-on effect on all aspects of graduate medical education (GME), including residency and fellowship programs [1, 2]. Over the last 2 months, in response to the rapid spread of the virus in Asia, Europe, Middle East, North and South America, the majority of countries took drastic containment measures [3]. With regard to the ophthalmology departments, all elective clinical and surgical activities were suspended indefinitely and, where necessary, healthcare personnel, including trainees, were redeployed to COVID-19 wards. Moreover, ophthalmology is considered a high-risk subspecialty due to both the compounded risk of virus exposure to patients’ conjunctival and respiratory secretions during the close proximity ophthalmic examination and the typical high-volume outpatient clinics and theatre lists [4]. It follows that, once the strict restrictions of the first phase have been overcome, the subsequent phase of coexistence with the virus cannot be managed as a rapid and complete “return to normal”. Further and long-term rearrangements of ophthalmology protocols will be required to minimize unnecessary contact, including the reduction of the volume of both outpatient and operating lists. Ophthalmology residents and fellows are, therefore, highly likely to experience significant restrictions in clinical and surgical opportunities for several more months. Furthermore, another crucial area of GME, such as the didactic teaching, has also been heavily impacted by the COVID-19 pandemic that resulted in the suspension or cancellation of traditional lecturing sessions, educational courses, and meetings/conferences.
It appears evident that the above outlined situation could cause a gap of unpredictable duration in ophthalmology training impairing its effectiveness. An effective reorganization of ophthalmology training will be required and should be undertaken promptly. However, it should also be sustainable in the long-term as, on the one hand, training time is a crucial issue in fixed-term programs, such as residency or fellowship, and, on the other hand, social distancing and restrictions to practical activities could be required for an indefinite period.
Although there are plenty of papers and reviews describing the impact of the current health emergency on ophthalmology practice with suggestions as to how it could be reorganised, we found a lack of studies focused on ophthalmology training and trainees’ experience and perspective. Specifically, to the best of our knowledge, there is one editorial reporting common practices to adopt in academic ophthalmology departments [2] and one letter reporting the experience of New York Area Ophthalmology Residents during the pandemic from the program directors’ perspective [5]. In addition, potentially beneficial adaptations have been suggested for general medical students educational programs, but not specifically for ophthalmology trainees [6–8].
In view of this, we created an online survey, specifically addressed to ophthalmology residents and fellows, aiming to assess the changes they have experienced in ophthalmology training related to the current COVID-19 pandemic, and based on their responses, propose potentially beneficial long-term changes.
Materials and methods
An anonymous web-survey was created on Google Forms and distributed by email and/or WhatsApp messenger to ophthalmology residents and fellows worldwide over a period of 10 days, from May 2, 2020 to May 11, 2020. The survey followed the principles of Declaration of Helsinki. The data analysis included only the responses of participants who consented to the use of the data contained in the survey for scientific and statistical purposes.
Initial questions aimed to characterize the sample in terms of professional qualifications and country of training attendance. Then, a set of closed-ended questions investigated the changes experienced by the trainees in three areas (clinical activity, surgical practice, and didactic teaching), their perception of the impact that the current situation has had on their training and could have in the future as well as the potential modifications from which they could benefit. Finally, the survey ended with an open-ended question about any additional suggestions to improve the quality and the effectiveness of training in view of the pandemic.
Categorical variables were summarized by percentages.
Results
A total of 525 responses were collected from 32 different countries. Thirteen respondents did not consent to the use of data and 8 submitted a blank survey, thus these 21 responses were excluded from the data analysis. Of the remaining 504 respondents, 414 (82.1%) were residents and 90 (17.9%) fellows in different subspecialties.
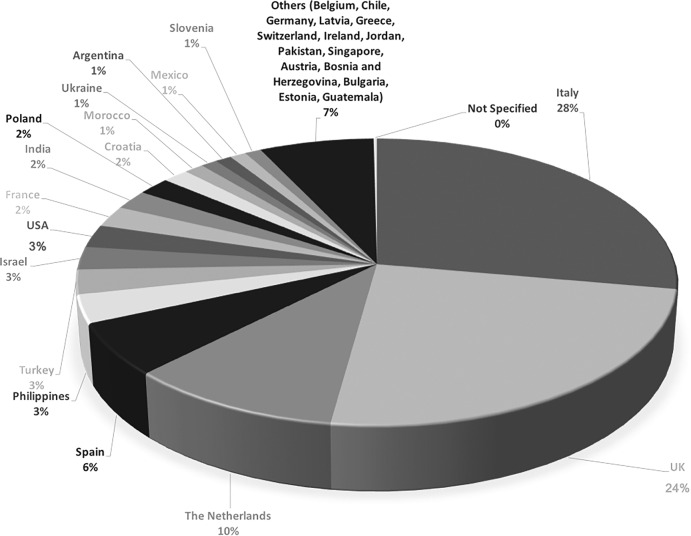
The geographical distribution of the responses is shown in Fig. 1. Table 1 summarises the changes in the training experienced over the preceding 2 months secondary to the COVID-19 pandemic. About one fifth of the trainees were redeployed (25.4%). Both clinical and surgical activity massively decreased with 52.6% and 74.6% of trainees reported a reduction of >75% of their clinical and surgical practice, respectively; in particular, about half of respondents declared that they have suspended surgical practice completely. More than half of the residents (53.1%) and 34.4% of fellows, reported that they were not able to perform cataract surgery routinely anymore. Didactic teaching has reportedly been less impacted by the pandemic. Indeed, although most trainees experienced a gap, web-based teaching has been arranged on a regular basis in the majority of cases (Table 1).
Fig. 1. Chart showing the proportion of country of training attendance of the respondents.
Geographical distribution of the respondents.
Table 1.
Changes of ophthalmology training during COVID-19 pandemic.
| Question | Residents n (%) | Fellows n (%) |
|---|---|---|
| Have you been redeployed due to COVID-19 pandemic? | ||
| Yes | 115 (27.78) | 13 (14.44) |
| No | 295 (71.26) | 76 (84.44) |
| On average, how many days per week have you worked in your ophthalmology department in the last 2 months? | 2.81 ± 1.73 | 3.24 ± 1.85 |
| How much has your clinical activity decreased? | ||
| <25% | 51 (12.32) | 8 (8.89) |
| 25–50% | 46 (11.11) | 13 (14.44) |
| 50–75% | 89 (21.49) | 31 (34.44) |
| >75% | 193 (46.62) | 27 (30) |
| 100% | 34 (8.21) | 11 (12.22) |
| Do you feel confident with telephone consultations? | ||
| Yes | 180 (43.48) | 52 (57.78) |
| No | 230 (55.56) | 37 (41.11) |
| Are you performing any virtual clinic/telemedicine? | ||
| Yes | 141 (34.06) | 40 (44.44) |
| No | 269 (64.97) | 50 (55.56) |
| How much has your surgical activity decreased? | ||
| <25% | 61 (14.73) | 10 (11.11) |
| 25–50% | 14 (3.38) | 6 (6.67) |
| 50–75% | 15 (3.62) | 7 (7.78) |
| >75% | 97 (23.43) | 28 (31.11) |
| 100% | 213 (51.45) | 38 (42.22) |
| How many surgeries did you perform in the last 2 months? | 2.22 ± 5.67 | 7.92 ± 15.6 |
| According to your training, do you feel that there is any surgical procedure that you are not able to carry out anymore on regular basis? (choose one or more) | ||
| Intravitreal injection | 70 (16.91) | 5 (5.56) |
| Cataract surgery | 220 (53.14) | 31 (34.44) |
| Filtering surgeries | 128 (30.92) | 9 (10) |
| Macular surgery | 122 (29.47) | 12 (13.33) |
| Retinal detachment repair | 108 (26.08) | 10 (11.11) |
| Squint surgeries | 128 (30.92) | 8 (8.89) |
| Dacryocystorhinostomy | 137 (33.09) | 6 (6.67) |
| Eyelid position repair | 141 (34.06) | 5 (5.56) |
| Other | 2 (0.48) | 5 (5.56) |
| In your hospital is there any simulation-based tool available for surgical training? | ||
| Yes | 182 (43.96) | 44 (48.89) |
| No | 232 (56.04) | 46 (51.11) |
| Have you experienced any gap in the didactic teaching? | ||
| Yes | 232 (56.04) | 47 (52.22) |
| No | 181 (43.72) | 43 (47.78) |
| Are you attending any web-based teaching regularly? | ||
| Yes | 278 (67.15) | 63 (70) |
| No | 134 (32.37) | 27 (30) |
The responses related to the trainees’ perception of the influence of COVID-19 pandemic are shown in Table 2. Most trainees reported that COVID-19 has currently impacted severely on ophthalmology training (54.2%), but only a third (33.1%) responded that this gap could be irreversible. The majority of them described the perspective of the long-term impact as “moderate” (37.3%), “mild” (14.1%) of “slight” (4.2%) suggesting a more optimistic outlook (Table 2). Although the institutional guidance on working during the pandemic was largely recognized as appropriate (66.7%), less than half of the trainees responded to feeling safe in the work environment (47.2%) (Table 2). Half the trainees (49.8%) considered appropriate the measures taken to preserve the effectiveness of training (Table 2).
Table 2.
Ophthalmology trainees’ perception related to COVID-19 pandemic.
| Question | Residents n (%) | Fellows n (%) |
|---|---|---|
| How would you describe the impact of COVID-19 pandemic on your training program? | ||
| Slight | 8 (1.93) | 1 (1.11) |
| Mild | 36 (8.69) | 7 (7.78) |
| Moderate | 113 (27.29) | 19 (21.11) |
| Severe | 216 (52.17) | 57 (63.33) |
| Catastrophic | 40 (9.66) | 6 (6.67) |
| Do you think that COVID-19 pandemic will result in an irreversible gap in your training? | ||
| Yes | 142 (34.29) | 25 (27.78) |
| No | 122 (29.47) | 28 (31.11) |
| Not sure | 150 (36.23) | 37 (41.11) |
| Do you think that your institution has provided you appropriate guidance on working during the pandemic? | ||
| Yes | 267 (64.49) | 69 (76.67) |
| No | 147 (35.51) | 21 (23.33) |
| Do you feel safe and well protected against SARS-CoV-2 working in the hospital? | ||
| Yes | 191 (46.13) | 47 (52.22) |
| No | 220 (53.14) | 43 (47.78) |
| Do you think that the measures taken by your institution to preserve the effectiveness of your training have been appropriate? | ||
| Yes | 195 (47.1) | 56 (62.22) |
| No | 216 (52.17) | 34 (37.78) |
| Considering the future long-term restrictions in clinical and surgical activities related to the phase of coexistence with the virus, how do you think will be the impact on your training? | ||
| Slight | 15 (3.62) | 6 (6.67) |
| Mild | 59 (14.25) | 12 (13.33) |
| Moderate | 149 (35.99) | 39 (43.33) |
| Severe | 162 (39.13) | 31 (34.44) |
| Catastrophic | 28 (6.76) | 1 (1.11) |
Table 3 summarises the outcomes of the questions investigating trainees’ opinion on the effectiveness of some changes proposed to improve the training. For most residents the ideal ratio for trainer/trainees supervision during clinical activities ranged from 1:2 to 1:1 (66.2%), whereas the fellows preferred a ratio between 1:3 and 1:2 (64.4%). With regard to surgical practice, the vast majority of trainees agreed in identifying 1:1 as the ideal ratio trainer/trainees (77.8%). Web-based case-presentations, web-based discussion of edited surgical videos and simulation-based training were largely considered effective educational tools (Table 3), even if, so far, the web-based teaching is perceived as complimentary and not a replacement of traditional lecture presentations (Table 3). With regard to the need for an extension of training program to recover the current gap, the majority of trainees did not express a definite opinion, as the preferred options were “reasonable” (34.1%) and “not sure” (21.4%).
Table 3.
Trainees’ perception of potential implementations for ophthalmology training.
| Question | Residents n (%) | Fellows n (%) |
|---|---|---|
| Please, suggest the ideal ratio trainer/trainees in outpatient clinic: | ||
| 1:4 | 45 (10.87) | 9 (10) |
| 1:3 | 79 (19.08) | 25 (27.78) |
| 1:2 | 159 (38.41) | 33 (36.67) |
| 1:1 | 115 (27.78) | 18 (20) |
| 2:1 | 9 (2.17) | 2 (2.22) |
| Do you believe that telementoring could be effective to improve your clinical skills? | ||
| Yes | 186 (44.93) | 43 (47.78) |
| No | 62 (14.97) | 17 (18.89) |
| Not sure | 164 (39.61) | 27 (30) |
| Do you believe that virtual clinic and telemedicine may help you to retain and/or improve your clinical skills? | ||
| Yes | 267 (64.49) | 52 (57.78) |
| No | 146 (35.26) | 36 (40) |
| The increase of web-based teaching sessions including case-presentations could be helpful to your clinical training? | ||
| Yes | 380 (91.78) | 82 (91.11) |
| No | 31 (7.48) | 5 (5.56) |
| Please, suggest the ideal ratio trainer/trainees in the operating room: | ||
| 1:4 | 5 (1.21) | 1 (1.11) |
| 1:3 | 13 (3.14) | 0 (0) |
| 1:2 | 63 (15.21) | 17 (18.89) |
| 1:1 | 323 (78.02) | 69 (76.67) |
| 2:1 | 5 (1.21) | 0 (0) |
| Do you believe that telementoring could be effective to improve your surgical skills? | ||
| Yes | 113 (25.45) | 24 (26.67) |
| No | 149 (35.99) | 37 (41.11) |
| Not sure | 153 (36.95) | 25 (27.78) |
| Do you believe that a simulator training may help you to retain and/or improve your surgical skills? | ||
| Yes | 367 (88.65) | 71 (78.89) |
| No | 47 (11.35) | 17 (18.89) |
| The increase of web-based teaching sessions including live discussion of edited surgical videos could be helpful to your surgical training? | ||
| Yes | 353 (85.26) | 79 (87.78) |
| No | 59 (14.25) | 9 (10) |
| Can the web-based teaching sessions entirely replace the traditional lecturing? | ||
| Yes | 70 (16.91) | 19 (21.11) |
| Only partially | 236 (57.01) | 51 (56.67) |
| No | 108 (26.08) | 19 (21.11) |
| What do you think about an extension of your training program? | ||
| Pointless | 90 (21.73) | 12 (13.33) |
| Reasonable | 127 (30.67) | 45 (50) |
| Necessary | 91 (21.98) | 17 (18.89) |
| Not sure | 106 (25.6) | 15 (16.67) |
In the open-ended question at the end of the survey most respondents reinforced their support for one or more of the suggested changes, and one respondent proposed sessions of discussion on scientific literature consistent with journal club format.
Discussion
We conducted the first survey specifically investigating the trainees’ perspective on both the impact of COVID-19 pandemic on their clinical, surgical and didactic activity, and the potential of modern technology-based educational tools for a long-term reshaping of ophthalmology training. The effectiveness and continuity of GME are crucial for the competence of future ophthalmologists and should be ensured, despite any challenging environment. Ophthalmology residency provides extensive training to fulfill comprehensive core ophthalmology competence over a period varying from 4 to 7 years according to the country of training. Whereas, a fellowship is focused on the development of clinical and surgical skills specific to a subspecialty area over a short period, commonly from 6 to 24 months [9]. Thus, a prolonged delay in practical and didactic training might not be recovered and result in the failure to acquire the necessary surgical and clinical skills for both residents and fellows without an extension of training. In this regard, the COVID-19 pandemic, whose duration and magnitude are still unknown, might be compared with other catastrophic events, such as wars or natural disasters, having a dramatic impact on the economy, society, health systems and, therefore, medical education [10, 11]. As has happened in countries ravaged by wars, the crisis within GME should be mitigated and facilitators should take this opportunity to introduce structural and targeted changes, sustainable over time, leading to an improvement and a greater flexibility in the preexisting system [10, 12]. This amelioration would not only overcome the current COVID-19-related restrictions but also any future situational barriers. Moreover, working in “health emergency mode” constitutes a learning opportunity itself contributing to trainees’ professional and personal enrichment [11]. In this survey, focused on ophthalmology training, we chose to identify the concerns of residents and fellows, highlighting their opinions on the suggested educational tools. Indeed, audience acceptance is a fundamental prerequisite for the effectiveness of any teaching method. We found that, despite a significantly negative perception of the current impact of the pandemic on training, most trainees consider favorably the role that emerging teaching methods could have.
In our survey, clinical activity was reportedly reduced by at least 50% by more than three-quarters of trainees. The need for social distancing and the minimization of in-person evaluation of the patients is likely to lead to the increased use of virtual clinics and telemedicine as well as telephone consultations [2]. The importance of the acquisition of appropriate communication skills in ophthalmology and the need to implement targeted educational activities have been already highlighted, mainly related to difficult conversations [13]. Our survey highlighted this need, showing that the majority of trainees lacked confidence in telephone consultations. A good level of acceptance of telemedicine, virtual clinics, and telementoring as helpful educational tools for learning clinical skills has been noted. It is worth noting that trainees’ acquisition of skills in telemedicine and remote monitoring could facilitate the long-term use of virtual clinics in future routine practice [14]. Finally, the increase of teaching sessions including case-presentations has been widely reported by trainees as a helpful tool for clinical training. This result is consistent with the recent literature reporting that case-based learning is effective in improving two primary clinical skills, such as critical thinking and decision-making [15].
With regard to surgical activity, the impact was reported to be even greater. The majority of residents have stopped practical surgical training completely. Furthermore, in an attempt to bring in social distancing measures, the number of people physically present in the operating rooms, including trainees, has been limited. Therefore, the pandemic has impacted two fundamental aspects of surgical training, such as the practice for the acquisition of technical surgical skills and observational surgical learning. In this regard, we asked trainees to evaluate if simulator training and web-based teaching sessions, including live discussion of edited surgical videos, could be helpful for surgical training. An affirmative response was registered in the vast majority of cases for both. Simulation-based tools have been increasingly used in ophthalmology to acquire and retain surgical technical skills, at the trainees’ convenience in an entirely safe environment [16]. In particular, it has recently been reported that, among the available simulation-based models, the Eyesi Surgical Simulator received the best effectiveness rating for cataract surgery, resulting in improved theatre performance and lower rates of complications [16]. This finding appears even more relevant considering that half of the residents and one third of the fellows stated that they feel to be not able to carry out cataract surgery routinely anymore. In addition, the demonstration of surgical procedures through live-surgery and edited video-recordings has been gaining popularity in ophthalmology as it is known that the acquisition of both motor and cognitive skills can be achieved through observation [17, 18]. Specifically, surgical video-recordings are recognized as a safe and effective teaching tool that can be implemented with post hoc interactive discussion aiming to acquire crucial surgical n non-technical skills, such as decision-making, surgical planning, situational awareness, and understanding of surgical steps [17, 19]. Clearly, the forthcoming resumption of trainees’ surgical practice remains highly desirable and surgical telementoring may help to accelerate this process. Indeed, supervising and guiding the trainees from a remote location could be a convenient and effective solution to avoid crowded operating rooms. In our survey, surgical telementoring was mostly considered of uncertain or no usefulness. Contrarily, a recent systematic review suggested that telementoring is as safe and effective as on-site mentoring [20]. It might be argued that the results of our survey can be explained by the fact that, so far, the use of telementoring has been limited in ophthalmology [21, 22].
Differently from practical training protocols, the didactic teaching appeared to be less impacted by the COVID-19 pandemic as many academic centers rapidly switched from traditional lecturing to web-based teaching. Indeed, despite a common initial gap, most trainees were attending web-based teaching sessions on a regular basis at the time of distribution of our survey. Several e-learning formats, such as webcasts, webinars, podcasts, and vodcasts, have been used in medical education and, specifically, in ophthalmology, with promising results [23–26]. These technology-based tools have established advantages impacting positively on both learning effectiveness and audience satisfaction, such as the possibility to be recorded and/or stored online and the availability at a time and location convenient to the attendee [24]. In particular, webinars offer the advantage of real-time interaction between mentor and trainees and have been associated with increased knowledge retention and active audience participation [27]. Moreover, e-learning sessions could facilitate trainees’ attendance at lessons shared among multiple institutions and/or lectures given by national and international experts [2]. Traditional lecturing, however, still appeared to be appreciated by the trainees, thus the most desirable scenario may be long-term integration of web-based coupled with traditional teaching.
Finally, the unpredictable course and duration of the current COVID-19 pandemic has raised the concern of a potential prolongation of the training program if competency cannot be gained in the remaining training period and the perspective of the trainees appeared open to this possibility.
In conclusion, in response to the COVID-19-related restrictions and the consequent potentially devastating impact on GME, a huge effort is required to optimize ophthalmology training. A prompt and appropriate reshaping of ophthalmology training, taking advantage of new technological educational tools, may result not only in increasing our capacity to cope successfully with the current situation but, above all, in a substantial amelioration of the effectiveness of training programs in the long term. Moreover, in view of the unpredictable course of the pandemic and the unlikelihood of a complete “return to normal”, the suggested implementations could provide ophthalmology training with the flexibility necessary to react properly and promptly to any further restrictions as well as other potentially future devastating events.
What was known before
The coronavirus disease 2019 (COVID-19) pandemic and the resulting global crisis within health systems impacted severely on graduate medical education, including ophthalmology training
What this study adds
Trainees’ perspective strongly reinforced the need to introduce new technology-based educational tools for a prompt and long-term reshaping of ophthalmology training to preserve its effectiveness and improve its sustainability and flexibility despite any challenging situations.
Ophthalmology trainees largely agreed to consider web-based case-presentations, web-based discussion of edited surgical videos, and simulation-based training effective educational tools for their clinical and surgical training.
Acknowledgements
The authors thank Hannah Levis for proofreading this paper.
OphthaTraining Group
Mariantonia Ferrara1, Vito Romano2,3, Davis H Steel4,5, Rajen Gupta1, Claudio Iovino6, Elon H. C. van Dijk7, Carlos Rocha-de-Lossada8, Ernesto Bali9, Xavier Valldeperas10, Davide Romano11, Kunal A. Gadhvi2, Francesco Matarazzo12, Argyrios Tzamalis13, Piergiacomo Grassi14, Rahul Rachwani15, Giulia Coco2,16, Catherine Dianne Reyes-Delfino17, Francesca Amoroso18, Nakhoul Nakhoul19,20, Francesco Sabatino21, Sufiyan Shaikh1, Adrian Au22, Emiliano Di Carlo23, Bernhard Steger24, Andrea Govetto25, Mario Toro26, Michela Cennamo27, Sibel Demirel28, Pasquale Napolitano29, Cristian Cartes30, Raffaele Raimondi31, Alessio Montericcio31, Giancarlo Dell’Aversana Orabona32, Chiara Comune33, Davide Borroni34, Luca Pagano2,31, Clara Montalbano31, Danilo Iannetta35, Martina Angi36
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Members of the OphthaTraining Group are listed below Acknowledgements.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mariantonia Ferrara, Email: mariantonia.ferrara@gmail.com.
for the OphthaTraining Group:
Mariantonia Ferrara, Vito Romano, Davis H Steel, Rajen Gupta, Claudio Iovino, Elon H. C. van Dijk, Carlos Rocha-de-Lossada, Ernesto Bali, Xavier Valldeperas, Davide Romano, Kunal A. Gadhvi, Francesco Matarazzo, Argyrios Tzamalis, Piergiacomo Grassi, Rahul Rachwani, Giulia Coco, Catherine Dianne Reyes-Delfino, Francesca Amoroso, Nakhoul Nakhoul, Francesco Sabatino, Sufiyan Shaikh, Adrian Au, Emiliano Di Carlo, Bernhard Steger, Andrea Govetto, Mario Toro, Michela Cennamo, Sibel Demirel, Pasquale Napolitano, Cristian Cartes, Raffaele Raimondi, Alessio Montericcio, Giancarlo DellʼAversana Orabona, Chiara Comune, Davide Borroni, Luca Pagano, Clara Montalbano, Danilo Iannetta, and Martina Angi
References
- 1.Li OJ, Shantha J, Wong TY, Wong EY, Mehta J, Lin H, et al. Preparedness among ophthalmologists: during and beyond the COVID-19 pandemic. Ophthalmology. 2020;127:569–72.. doi: 10.1016/j.ophtha.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong TY, Bandello F. Academic ophthalmology during and after the COVID-19 pandemic. Ophthalmology. 2020:S0161-6420:30406-1. [DOI] [PMC free article] [PubMed]
- 3.Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobingeret G, et al. COVID-19: towards controlling of a pandemic. Lancet. 2020;395:1015–8. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Romano MR, Montericcio A, Montalbano C, Raimondi R, Allegrini D, Ricciardelli G, et al. Facing COVID-19 in ophthalmology department. Curr Eye Res. 2020;45:653–8. doi: 10.1080/02713683.2020.1752737. [DOI] [PubMed] [Google Scholar]
- 5.Chen RWS, Abazari A, Dhar S, Fredrick DR, Friedman IB, Dagi Glass LR, et al. Living with COVID-19: a perspective from New York area ophthalmology residency program directors at the epicenter of the pandemic. Ophthalmology. 2020:S0161-6420(20)30430-9. [DOI] [PMC free article] [PubMed]
- 6.Hodgson JC, Hagan P, et al. Medical education adaptations during a pandemic: transitioning to virtual student support. Med Educ. 2020;54:662–3. doi: 10.1111/medu.14177. [DOI] [PubMed] [Google Scholar]
- 7.Eva KW, Anderson MB, et al. Medical education adaptations: really good stuff for educational transition during a pandemic. Med Educ. 2020;54:494. doi: 10.1111/medu.14172. [DOI] [PubMed] [Google Scholar]
- 8.Alsafi Z, Abbas AR, Hassan A, Ali MA. The coronavirus (COVID-19) pandemic: adaptations in medical education. Int J Surg. 2020;78:64–5. doi: 10.1016/j.ijsu.2020.03.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang G, Fang CH, Lopez SA, Bhagat N, Langer PD, Eloy JA. Impact of fellowship training on research productivity in academic ophthalmology. J Surg Educ. 2015;72:410–7. doi: 10.1016/j.jsurg.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Hodgetts G, Brown G, Batić-Mujanović O, Gavran L, Jatić C, Racić M, et al. Twenty-five years on: revisiting Bosnia and Herzegovina after implementation of a family medicine development program. BMC Fam Pr. 2020;21:7. doi: 10.1186/s12875-020-1079-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Espana-Schmidt C, Ong EC, Frishman W, Bergasa NV, Chaudhari S. Medical residency training and hospital care during and after a natural disaster: Hurricane Sandy and its effects. Am J Med. 2013;126:944–5. doi: 10.1016/j.amjmed.2013.03.031. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz AM, Wilson JM, Boden SD, Moore TJ, Jr, Bradbury TL, Jr, Fletcher ND. Managing resident workforce and education during the COVID-19 pandemic. JBJS Open Access. 2020;5:e0045. doi: 10.2106/JBJS.OA.20.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mishra A, Browning D, Haviland MJ, Jackson ML, Luff D, Meyer EC, et al. Communication skills training in ophthalmology: results of a needs assessment and pilot training program. J Surg Educ. 2018;75:417–26.. doi: 10.1016/j.jsurg.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Ting DSW, Lin H, Ruamviboonsuk P, Wong TY, Sim DA. Artificial intelligence, the internet of things, and virtual clinics: ophthalmology at the digital translation forefront. Lancet Digital Health. 2020;2:e8–9. doi: 10.1016/S2589-7500(19)30217-1. [DOI] [PubMed] [Google Scholar]
- 15.McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3:JMECD.S20377. doi: 10.4137/JMECD.S20377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee R, Raison N, Lau WY, Aydin A, Dasgupta P, Ahmed K, et al. A systematic review of simulation-based training tools for technical and non-technical skills in ophthalmology. Eye. 2020. [DOI] [PMC free article] [PubMed]
- 17.Hollick EJ, Allan BD. Live surgery: national survey of United Kingdom ophthalmologists. J Cataract Refract Surg. 2008;34:1029–32. doi: 10.1016/j.jcrs.2008.02.023. [DOI] [PubMed] [Google Scholar]
- 18.van Gog T, Paas F, Marcus N, Ayres P, Sweller J. The mirror neuron system and observational learning: implications for the effectiveness of dynamic visualizations. Educ Psychol Rev. 2008;21:21–30. [Google Scholar]
- 19.Youngson GG. Teaching and assessing non-technical skills. Surgeon. 2011;9:S35–7. doi: 10.1016/j.surge.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 20.Erridge S, Yeung DKT, Patel HRH, Parkayastha S. Telementoring of surgeons: a systematic review. Surg Innov. 2019;26:95–111. doi: 10.1177/1553350618813250. [DOI] [PubMed] [Google Scholar]
- 21.Ye Y, Wang J, Xie Y, Jiang H, Zhong J, He X, et al. Global teleophthalmology with the smartphone for microscopic ocular surgery. Eye Contact Lens. 2016;42:275–9. doi: 10.1097/ICL.0000000000000215. [DOI] [PubMed] [Google Scholar]
- 22.Camara JG, Zabala RR, Henson RD, Senft SH. Teleophthalmology: the use of real-time telementoring to remove an orbital tumor. Ophthalmology. 2000;107:1468–71. doi: 10.1016/S0161-6420(00)00211-6. [DOI] [PubMed] [Google Scholar]
- 23.Bandhu SD, Raje S. Experiences with E-learning in ophthalmology. Indian J Ophthalmol. 2014;62:792–4. doi: 10.4103/0301-4738.138297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Backhaus J, Huth K, Entwistle A, Homayounfar K, Koenig S. Digital affinity in medical students influences learning outcome: a cluster analytical design comparing vodcast with traditional lecture. J Surg Educ. 2019;76:711–9. doi: 10.1016/j.jsurg.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Kapoor S, Catton R, Khalil H. An evaluation of medical student-led podcasts: what are the lessons learnt? Adv Med Educ Pr. 2018;9:133–8. doi: 10.2147/AMEP.S148513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petrarca CA, Warner J, Simpson A, Petrarca R, Douiri A, Byrne D, et al. Evaluation of eLearning for the teaching of undergraduate ophthalmology at medical school: a randomised controlled crossover study. Eye. 2018;32:1498–503. doi: 10.1038/s41433-018-0096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mayorga EP, Bekerman JG, Palis AG. Webinar software: a tool for developing more effective lectures (online or in-person) Middle East Afr J Ophthalmol. 2014;21:123–7. doi: 10.4103/0974-9233.129756. [DOI] [PMC free article] [PubMed] [Google Scholar]