Abstract
Purpose
The aim of the study was to quantify the association between perceived everyday discrimination and binge eating among Latinas in the United States.
Methods
Participants included 1014 Latinas from the 2002–2003 National Latino and Asian American Study. Modified Poisson models with robust standard errors were used to estimate sociodemographic-adjusted prevalence ratios (aPRs) and 95% confidence intervals (CIs) of binge eating associated with overall and attribution-specific discrimination.
Results
Approximately 7% of Latinas reported binge eating. Increased frequency of discrimination was associated with a higher prevalence of binge eating (aPR, 1.59; 95% CI, 1.23–2.06), and Latinas reporting frequencies of discrimination in the top tertile had the greatest prevalence elevation (aPR, 3.63; 95% CI, 1.32–10.00). There were important differences by discrimination attribution: Latinas experiencing primarily height/weight-based or skin color–based discrimination had the greatest prevalence elevation relative to those reporting no discrimination (aPR, 10.24; 95% CI, 2.95–35.51; and aPR, 8.83; 95% CI, 2.08–37.54, respectively), whereas Latinas reporting primarily race-based discrimination had the lowest prevalence elevation (aPR, 1.64; 95% CI, 0.47–5.69).
Conclusions
Discrimination may be an important social determinant of Latinas’ binge eating. Future research should incorporate expanded conceptual models that account for Latinas’ complex social environment, focusing on intersecting dimensions of identity.
Keywords: Feeding and eating disorders, Social discrimination, Weight prejudice, Latinas, Health status disparity
Introduction
Latinas report high rates of binge eating (BE) [1], or consuming a large amount of food while feeling a loss of control [2]. Nationally representative data from the National Latino and Asian American Study (NLAAS) indicate that the 12-month and lifetime prevalence estimates of recurrent BE (occurring twice or more per week for ≥6 months) among Latinas are 3.3% and 5.8%, respectively [3]. These estimates are higher than the national average estimates (2.1% and 4.5%) [4] and are significantly higher than those observed among Asian, Black, and non-Hispanic White women and men of all racial/ethnic backgrounds [5]. Such findings are concerning, given the substantial health consequences of BE (e.g., cardiometabolic issues, substance use, and depression) [4,6–8] and its negative impacts on psychosocial functioning and quality of life [9]. There is thus a critical need to understand the factors contributing to Latinas’ elevated rates to inform interventions.
Leading etiologic models of BE (i.e., cognitive behavioral, affect regulation, and dual-pathway models) conceptualize the behavior as a maladaptive coping response to negative affect or low self-esteem, with predisposing factors that are social in origin and often relating to body shape/weight (e.g., cultural/peer pressures to be thin) [10,11]. As feminist scholars routinely point out, however, such models are based on studies with almost exclusively White participants [12–14], and only recently has population-level research considered the unique social stressors affecting racial/ethnic minorities that may additionally contribute to their eating-related pathology. With respect to Latinas, this work is underdeveloped. Most studies focus narrowly on acculturation [1,3,15,16], a construct rightfully critiqued for its individual-level perspective and tendency to obscure the complexity of Latinas’ social environment beyond stressors related to immigration status [17–19]. For instance, as women and racial/ethnic minorities, Latinas report high levels of perceived everyday discrimination or “the belief that one has experienced unfair treatment by individuals and social institutions … based on personal characteristics such as race, gender, or weight” [20] because of social hierarchies and interlocking systems of power/oppression in the United States [21]. Importantly, this may increase BE risk: discrimination is a major social stressor that adversely impacts mental well-being [22,23] and has been described as an important determinant of eating-related pathology in qualitative research with racially/ethnically diverse women [12,24–26].
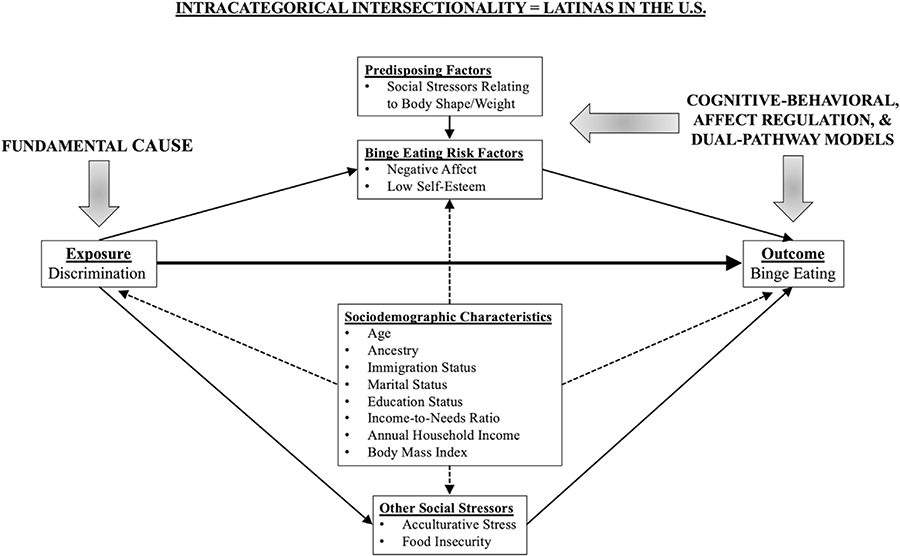
To date, only a few small quantitative studies have examined associations between discrimination and eating-related pathology among Latinas, and most studies have focused on a singular discrimination attribution (typically race/ethnicity) [27–29]. Although these studies suggest a link, there is a need for population-level research examining the relationship between discrimination and BE using large, nationally representative samples and to extend investigations to multiple discrimination attributions to account for the complexity of Latinas’ social environment and the multidimensionality of their identities. To begin addressing these research gaps, our objectives for this descriptive epidemiologic study were to quantify the association between perceived everyday discrimination (henceforth, “discrimination”) and BE among Latinas and to evaluate whether this association differed across discrimination attributions. Theoretical support was drawn from fundamental cause theory from epidemiology, which posits that certain social factors (including discrimination) represent “root causes” of health outcomes [30–32]; intracategorical intersectionality from Black feminist scholarship, which focuses on explaining the unique social factors related to interlocking systems of power/oppression shaping the lives of groups at a particular social location [33–35]; and leading models of BE [10,11] (Fig. 1). We hypothesized that discrimination would be associated with BE within this population [12,24–29], and that discrimination attributions previously linked with eating-related pathology in racially/ethnic diverse samples (gender [36], race/ethnicity [27–29], weight [37–39], and skin color [40–43]) would be most strongly associated. Owing to the cross-sectional nature of our data, we described associations rather than causal effects, with the goal of guiding future work.
Fig. 1.
Conceptual model detailing hypothesized relationship between perceived everyday discrimination and binge eating among Latinas in the U.S. model is informed by fundamental cause theory, in that we conceptualized discrimination as a “root cause” of binge eating (including all mediating pathways); intracategorical intersectionality, in that we focused on a fundamental cause related to interlocking systems of power/oppression shaping the lives of those at a particular social location (while acknowledging important within-group diversity); and cognitive behavioral, affect regulation, and dual-pathway models, leading etiologic models of binge eating that identify negative affect and low self-esteem as important risk factors, with social stressors relating to body shape/weight as upstream predisposing factors. Note: Model is not a directed acyclic graph, as not all arrows/relevant variable are included, and arrows do not necessarily represent causal relationships. For example, we do not mean to imply that sociodemographic characteristics “cause” discrimination but rather are related through macrosocial processes of racialization, immigration policies and so on (hence the dashed lines).
Methods
Data and participants
We used data from the 2002–2003 NLAAS, a nationally representative community household survey of Latinx and Asian adults in the United States. (n = 4649) [44,45]. Importantly, the NLAAS provides the most recent nationally representative data on BE prevalence among Latinas. Conducted as part of the National Institute of Mental Health’s Collaborative Psychiatric Epidemiology Surveys, the NLAAS used a four-stage probability sample design with oversampling of census blocks with greater than 5% density of target ancestry groups (Cuban, Mexican, and Puerto Rican) and attained an overall response rate of 73% [46]. Data were collected via in-person interviews in English or Spanish in the participant’s home unless a telephone interview was requested. The Institutional Review Boards at Cambridge Health Alliance, the University of Washington, and the University of Michigan approved all study procedures, and written informed consent was obtained from all participants [47]; as the present study was a secondary analysis of deidentified data, it was exempt from Institutional Review Board regulation. Further details about the NLAAS are described elsewhere [44,46].
We included 1027 Latinas aged 18–49 years who participated in the NLAAS; the age restriction reflects the critical risk period (young-to-middle adulthood) and age cohort distributions of BE [3,4], as well as shifts in the clinical presentation and social determinants of eating-related pathology across age cohorts [48] (Supplementary Materials provide results from a sensitivity analysis including all participants). Given the low percentage of missingness across all variables (<5%), we used complete case analysis [49,50]. After excluding participants with missing data on discrimination and BE (n = 13), the final analytic sample included 1014 participants.
Measures
Discrimination
Discrimination was assessed using the Everyday Discrimination Scale (EDS), a 9-item self-report scale that measures perceptions of day-to-day discrimination with demonstrated validity among Latinx adults in the United States [51–53]. Participants are asked, “In your day-to-day life, how often have any of the following things happened to you?” (e.g., being treated with less courtesy, being ignored), with six response options ranging from “never” to “almost every day.” We constructed a mean summary score by summing the response options from each item and dividing by nine (range: 0–5, Cronbach’s alpha = 0.90). To evaluate the exposure–outcome relationship by discrete frequencies of discrimination, we constructed three groups based on tertiles: none (score = 0), low (score >0 and <1), and high (score ≥1). We used tertiles to reflect the distribution of scores within our analytic sample and potentially conceptually distinct groups (those unwilling/unable to report discrimination, those reporting low frequencies, and those reporting high frequencies) [54,55], although we consider this parameterization secondary to the continuous summary score, given the former’s constraints on variance.
Discrimination attribution was assessed using a follow-up question to the EDS: “What do you think was the main reason for this/these experience(s)?,” with mutually exclusive options including ancestry/ethnicity, gender, race, age, height/weight, skin color, or other. We categorized participants into one of eight groups, based on their EDS summary score (dichotomized as 0 and >0) and response to this item, with no reported discrimination as the referent. For example, a participant who received an EDS score greater than 0 and selected gender in response to this question would be categorized into the “gender-based discrimination” group. We excluded participants who replied “don’t know” (n = 41) from analyses using this question.
Binge eating
Lifetime history of recurrent BE was defined using previously specified algorithms for assessing eating-related pathology in the NLAAS [4,21], which are based on Diagnostic and Statistical Manual, Fourth Edition (DSM-IV), criteria [56]. We used the “any BE” algorithm, in which participants who replied “yes” to having recurrent BE episodes and endorsed more than one item indicating loss of control (e.g., “Did you often get upset both during and after binges that your eating was out of your control?”) are categorized as ever affected by recurrent BE, and participants who replied “no” to the question about recurrent BE episodes are categorized as never affected.
Covariates
We considered two additional types of variables: (1) adjustment and (2) descriptive; such grouping was used to avoid model overadjustment [57] while still providing sufficient description of the sample’s BE risk profile. The selection of these variables was informed by theories of fundamental causes [30–32] and intracategorical intersectionality [33–35], leading models of BE [10,11] as described, and research on BE etiology [3,58–61] (see Supplementary Materials for details on covariate selection/grouping).
We considered the following sociodemographic characteristics as adjustment variables: age in years (continuous), ancestry (Cuban, Puerto Rican, Mexican, and other Latinx), immigration status (U.S. born to parents born in the United States, U.S. born to one or more parents born outside the United States, born outside the United States and U.S. citizen, and born outside the United States and non-U.S. citizen), marital status (married/cohabitating, divorced/separated/widowed, and never married), employment status (employed, unemployed, and not in labor force), income-to-needs ratio (continuous), annual household income (continuous), and body mass index in kilogram per square meter (<25 and ≥25).
We considered the following BE risk factors as descriptive variables: food/weight-related concerns (binary; yes or no to a question about fear of gaining weight), negative affect (binary; reporting none or one or more of three symptoms of a DSM-IV–defined major depressive episode [56]), acculturative stress (continuous; summed score on a 9-item scale from the Mexican–American Prevalence and Services Survey [62], range 0–9), and past-year food insecurity (binary; often or rarely/never to a question about not having enough money for food). We did not consider these variables as adjustment variables, as they likely represent mediators on the path between discrimination and BE [22,29,63]. For all categorical variables (adjustment and descriptive), we selected the largest group as the referent to increase precision.
Statistical analysis
For all analyses, the complex survey design of the NLAAS was taken into account via weighting, as per analytic guidelines published by Collaborative Psychiatric Epidemiology Surveys [64]; therefore, all estimates describe the population of Latinas in the United States. We described this population with respect to all covariates, overall and by discrimination frequency. We used modified Poisson models with robust standard errors to estimate prevalence ratios (PRs) and 95% confidence intervals (CIs) of BE associated with overall and attribution-specific discrimination. For each, we estimated their crude association with BE. Although we acknowledge the inability to estimate causal effects from cross-sectional data (and note our objectives were not causal), we also adjusted for sociodemographic characteristics to assess the robustness of discrimination’s association with BE; such estimates were interpreted as the association between discrimination and BE among Latinas of the same age, ancestry, and so on. Variables were entered into models one by one, checking for multicollinearity by examining the variance inflation factor of included variables. If detected (variance inflation factor >10), the variable most strongly associated with the outcome was retained (see Results).
Results
Table 1 presents sociodemographic characteristics and prevalence of BE risk factors among Latinas in the United States (2002–2003). The majority of the population were first-generation immigrants of Mexican descent who were not U.S. citizens. More than half were married/cohabitating and employed, and their average annual household income was three times the poverty line at the time of data collection. Most had a body mass index classified as overweight/obese [65]. Overall, the population reported a high prevalence/level of BE risk factors, and Latinas reporting the highest frequency of discrimination had the highest prevalence/level of all BE risk factors relative to those reporting low/no discrimination.
Table 1.
Sociodemographic characteristics and binge eating risk profile of Latinas aged 18–49 years in the United States estimated from the National Latino and Asian American Study, 2002–2003
| Unweighted, n (weighted %) | Overall n = 1014 (100) | Frequency of discrimination |
||
|---|---|---|---|---|
| High 402 (40) | Low 334 (33) | None 278 (27) | ||
| Sociodemographic characteristics* | ||||
| Age in years, mean (SE) | 32.1 (0.4) | 30.2 (0.7) | 32.4 (0.7) | 34.4 (0.4) |
| Ancestry (%) | ||||
| Cuban | 4.6 | 3.3 | 4.8 | 6.5 |
| Mexican | 56.6 | 53.8 | 60.3 | 57.2 |
| Puerto Rican | 10.1 | 13.5 | 9.3 | 5.4 |
| Other | 28.7 | 29.5 | 25.5 | 30.9 |
| Immigration status (%) | ||||
| Born in the United States | 20.2 | 30.0 | 18.2 | 8.6 |
| Born in the United States to one or more parents born elsewhere | 22.4 | 29.8 | 19.4 | 15.6 |
| Born outside the United States, U.S. citizen | 15.1 | 12.2 | 16.0 | 18.1 |
| Born outside the United States, not U.S. citizen | 42.4 | 28.1 | 46.4 | 57.7 |
| Marital status (%) | ||||
| Married/cohabitating | 62.0 | 54.7 | 62.4 | 71.7 |
| Divorced/separated/widowed | 13.8 | 14.8 | 12.7 | 13.9 |
| Never married | 24.2 | 30.5 | 24.9 | 14.4 |
| Employment status (%) | ||||
| Employed | 55.6 | 56.3 | 57.4 | 52.6 |
| Unemployed | 9.3 | 12.3 | 9.0 | 5.3 |
| Not in labor force | 35.1 | 31.4 | 33.6 | 42.1 |
| Income-to-needs ratio, mean (SE) | 2.9 (0.2) | 3.2 (0.2) | 2.4 (0.3) | 3.0 (0.4) |
| Annual household income in $, mean (SE)† | 40,849 (2481) | 45,757 (3014) | 35,077 (3004) | 41,767 (3788) |
| Body mass index ≥25 kg/m2 (%) | 59.1 | 58.0 | 59.2 | 60.7 |
| Binge eating risk factors* | ||||
| Food/weight-related concerns (%) | 41.4 | 50.0 | 40.2 | 30.4 |
| Negative affect (%) | 54.3 | 66.9 | 51.3 | 39.3 |
| Acculturative stress, mean (SE)‡ | 2.8 (0.1) | 3.6 (0.2) | 3.0 (0.2) | 2.0 (0.2) |
| Food insecurity (%) | 5.2 | 8.0 | 4.4 | 2.2 |
All estimates are based on the weighted analytic sample. Percentages are column totals and may not add to 100% due to rounding.
SE = standard error.
Number of participants with missing information: immigration status (n = 10), body mass index (n = 18), acculturative stress (n = 104), and food insecurity (n = 53).
Adjusted for household size.
Asked only of participants born outside the United States.
The population’s average EDS score was 0.8, and among those reporting discrimination, other-based discrimination was the most frequently endorsed attribution, followed by ancestry/ethnicity-based, height/weight-based, and skin color–based discrimination were the least frequently endorsed (Table 2).
Table 2.
Discrimination attribution across levels of perceived everyday discrimination among Latinas in the United States estimated from the National Latino and Asian American Study, 2002–2003
| Unweighted, n (weighted %) | Overall n = 1014 (100) | Frequency of discrimination |
||
|---|---|---|---|---|
| High 402 (40) | Low 334 (33) | None 278 (27) | ||
| Everyday Discrimination Scale summary score, mean (SE) | 0.8 (0.03) | 1.6 (0.04) | 0.5 (0.01) | 0 (0.0) |
| Discrimination attribution (%)* | ||||
| Age | 5.8 | 8.5 | 7.5 | — |
| Ancestry/national origin/ethnicity | 18.3 | 23.3 | 27.5 | — |
| Gender/sex | 5.8 | 10.1 | 5.3 | — |
| Height/weight | 3.1 | 4.3 | 4.4 | — |
| Race | 15.9 | 22.6 | 21.7 | — |
| Skin color | 2.4 | 3.3 | 3.1 | — |
| Other | 21.3 | 29.0 | 30.4 | — |
| No discrimination | 27.6 | — | — | — |
All estimates are based on the weighted analytic sample. Percentages are column totals and may not add to 100% due to rounding.
SE = standard error.
Discrimination attributions are mutually exclusive.
Approximately 7% of the population reported a lifetime history of recurrent BE; among Latinas reporting the highest frequency of discrimination, the prevalence was 11.3% (Table 3). Before adjustment, a 1-unit increase in EDS summary score was associated with a 65% elevation in BE prevalence (95% CI, 37%–99%). Adjusting for sociodemographic characteristics attenuated the estimate to 59% (95% CI, 23%–106%). BE prevalence among Latinas reporting high and low discrimination frequencies was five and three times higher, respectively, than the prevalence among those reporting no discrimination; adjustment slightly attenuated these estimates.
Table 3.
Prevalence and prevalence ratios for binge eating among Latinas in the United States associated with discrimination estimated from the National Latino and Asian American Study, 2002–2003
| Outcome | Prevalence of binge eating, % | Prevalence ratio (95% confidence interval) |
|
|---|---|---|---|
| Crude | Adjusted* | ||
| Everyday Discrimination Scale summary score | 7.1 | 1.65 (1.37–1.99) | 1.59 (1.23–2.06) |
| Frequency of discrimination | |||
| High | 11.3 | 4.79 (1.66–13.86) | 3.63 (1.32–10.00) |
| Low | 5.9 | 2.50 (0.89–7.01) | 2.05 (0.80–5.22) |
| None | 2.4 | 1.00 (reference) | 1.00 (reference) |
| Discrimination attribution† | |||
| Height/weight | 40.8 | 17.31 (4.39–68.32) | 10.24 (2.95–35.51) |
| Skin color | 22.1 | 9.38 (2.14–41.05) | 8.83 (2.08–37.54) |
| Ancestry/national origin/ethnicity | 9.0 | 3.80 (1.16–12.49) | 3.43 (0.95–12.33) |
| Other | 8.0 | 3.40 (1.07–10.81) | 2.66 (0.81–8.69) |
| Gender/sex | 6.6 | 2.82 (0.56–14.32) | 2.37 (0.44–12.73) |
| Age | 6.3 | 2.68 (1.02–7.04) | 2.32 (0.88–6.13) |
| Race | 4.2 | 1.79 (0.52–6.19) | 1.64 (0.47–5.69) |
| No discrimination | 2.4 | 1.00 (reference) | 1.00 (reference) |
All estimates are based on the weighted analytic sample.
Adjusted for age, ancestry, immigration status, marital status, employment status, income-to-needs ratio, annual household income, and body mass index (no multicollinearity detected).
Discrimination attributions are mutually exclusive.
There were large differences in BE prevalence by discrimination attribution (Table 3). Although height/weight-based and skin color–based discrimination were the least frequently endorsed discrimination attributions, they were the most strongly associated with BE. Approximately two-fifths of Latinas who had experienced primarily height/weight-based discrimination reported BE, a 10-fold elevation in prevalence relative to those reporting no discrimination (aPR, 10.24; 95% CI, 2.95–35.51). Similarly, one-fifth of Latinas who had experienced primarily skin color–based discrimination reported BE, a nine-fold elevation in prevalence (aPR, 8.83; 95% CI, 2.08–37.54). Latinas reporting primarily race-based discrimination had the lowest elevation in prevalence (aPR, 1.64; 95% CI, 0.47–5.69).
Discussion
This descriptive epidemiologic study aimed to expand conceptualizations of eating-related pathology among Latinas by examining the role of perceived everyday discrimination as a social determinant of BE within this population. Our primary finding was that discrimination was associated with BE, such that a one-unit increase in EDS score was associated with a ~60% increase in BE prevalence, and prevalence was highest among those reporting frequencies of discrimination in the top tertile. This is consistent with a large body of research documenting the adverse effects of discrimination on mental health in Latinx populations [22,66] and qualitative research exploring social determinants of eating-related pathology in racially/ethnically diverse women [12,24–26]. Although the present study is the first to our knowledge to document the discrimination–BE association among Latinas in a large, nationally representative cohort, similar associations have been reported in several smaller studies using recent data [27,29,67,68]. Thus, although sociodemographic characteristics of Latinas in the United States have shifted and the social stressors affecting this population have increased since 2002–2003 (e.g., postelection discrimination) [69,70], our findings are likely still relevant.
Our secondary finding was that the strength of the discrimination-BE association differed considerably across discrimination attributions, with height/weight-based and skin color-based discrimination having the strongest associations and gender- and race-based discrimination the weakest. There are two interrelated explanations for this. First, weight stigma (societal devaluation of people of higher weight status [71]) and colorism (skin color–based prejudice [72]) may be specific fundamental causes for BE among Latinas. These social stressors deeply shape the ways in which bodies are perceived and people are treated from the individual- to population-level, and feminist scholarship provides qualitative evidence of how women who are further marginalized by race, class, and other dimensions of identity are disproportionately affected in ways that increases BE risk [12,25]. Specifically, this work highlights the links between Western beauty standards, defined by thinness and light skin color, and social capital/mobility in the United States [73–77]. For example, Cheney writes of how “…attaining a slender body–a form of power–is a means by which women of diverse ethnicities and social classes can overcome inequalities in everyday social relationships and interactions” ([25], p. 1349); such efforts to attain a largely unattainable ideal can lead to food/weight-related concerns, negative affect, low self-esteem, and other BE risk factors. Adding to previous research highlighting the roles of weight stigma and colorism in structuring the distribution of mental health outcomes (including eating-related pathology) within Latinx populations [78,79], our findings thus suggest that these social stressors help structure the distribution of BE within Latinas specifically.
Second, our findings on discriminatory attributions may speak to intersectional nature of social identities and their relationships with health. Response options to the discrimination attributions question in this study included several constructs typically collapsed under the umbrella of “race/ethnicity”: race, ancestry/ethnicity, and skin color. Although these constructs are distinct dimensions of identity with potentially differential impacts on health for Latinx populations [79–82], they are also intersectional (along with gender) in ways that often make identity-based oppressions impossibile to disentangle [33,34,83,84]. A central tenet of intersectionality theory is that multiply marginalized groups experience qualitatively unique forms of discrimination on the basis of their intersecting identities, and that such experiences cannot be disaggregated into their component parts. This has important implications for measuring discrimination when scales are designed such that participants are forced to assign discriminatory experiences to a single identity [35,83,85,86]; that other-based discrimination was the most frequently endorsed suggests that for Latinas, individual attributes such as gender or race may not adequately capture their lived experiences. Collectively, our findings reveal an interesting pattern: discrimination based on aspects of identity linked with Western beauty standards (i.e., weight and skin color) were most strongly associated with BE, perhaps because of their specificity, whereas discrimination based on gender, race, and ethnicity may have been difficult to identify as such, diluting their apparent effects.
This study has important implications for future research. First, our findings illustrate the benefit of investigating the fundamental causes of BE, particularly those accounting for complex social environments and intersecting dimensions of identity. Leading etiologic models of BE have yet to incorporate an intersectional perspective, potentially limiting their ability to inform treatment and prevention efforts for diverse groups. Notably, our findings are largely consistent with the mechanisms described by these models, (i.e., social stressors as predisposing factors, with those relating to body shape/weight of preeminent importance), yet they also demonstrate the importance of contextualizing BE risk factors within social hierarchies and interlocking systems of power/oppression to better understand population-level distributions and root causes. Another advantage of investigating fundamental causes is the potential to understand eating-related pathology in relation to other health outcomes engendered by discrimination [30]. Second, although research facilitating causal interpretations is needed before stating practice/policy implications, our findings add empirical support to calls for initiating structural-level eating-related pathology prevention efforts [87,88]. Recent research provides guidance regarding how such efforts can be structured [89–91], although this work has largely focused on addressing gender- and weight-based inequities; analogous work accounting for racial/ethnic inequities (and their intersections) is in its infancy [16].
Limitations
Our findings must be interpreted in light of limitations. First, our use of data from 2002 to 2003 may have resulted in underestimated associations because of increased discrimination directed toward Latinx communities within current sociopolitical climates [70,92–94] and changes to BE criteria from the DSM-IV to DSM-5 involving decreased episode frequency [95]; however, as previously discussed, associations similar in magnitude to ours have been documented using recent data [27,29,67,68]. Second, we acknowledge that our data precluded a more nuanced intracategorical intersectional analysis. Ancestry, immigration status, and other dimensions of identity all shape exposure and responses to discrimination among Latinas [55], and considering this population a homogenous group likely obscured important within-group differences; indeed, the results presented in Table 1 suggest that discrimination frequency differed considerably across categories of most of the included sociodemographic characteristics. Given small subgroup sizes, we were unable to explore whether these differences were associated with BE prevalence. Future research with larger subgroup sample sizes should seek to build upon our findings and include between-population comparisons to facilitate investigations of multiple/compounding forms of discrimination [35,85]. Finally, qualitative research is an invaluable component to intersectional questions and will be necessary for furthering understanding of how intersecting dimensions of identity influence BE rates among Latinas [83,96].
Conclusions
This study adds to an emerging body of literature that adopts an intersectional, social epidemiologic approach to eating-related pathology research [97,98], investigating an important social determinant of Latinas’ BE. Future work should continue to expand upon conceptualizations of eating-related pathology to inform health equity efforts.
Highlights.
Binge eating was prevalent within a nationally representative cohort of Latinas
Everyday discrimination was positively associated with binge eating prevalence
Weight- and skin color-based discrimination were most strongly associated
Weight stigma and colorism may be upstream determinants of Latina’s binge eating
Acknowledgments
The authors would like to acknowledge the contributions of individuals who participated in the National Latino and Asian American Study.
This work was supported by the National Heart, Lung, and Blood Institute (5T32HL120823-05, awarded to A.B.). The opinions expressed in this work are those of the authors and do not necessarily reflect those of the funders.
References
- [1].Perez M, Ohrt TK, Hoek HW. Prevalence and treatment of eating disorders among Hispanics/Latino Americans in the United States. Curr Opin Psychiatry 2016;29(6):378–82. [DOI] [PubMed] [Google Scholar]
- [2].Diagnostic and Statistical Manual (DSM-5). Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- [3].Alegria M, Woo M, Cao Z, Torres M, Meng XL, Striegel-Moore R. Prevalence and correlates of eating disorders in Latinos in the United States. Int J Eat Disord 2007;40:S15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biol Psychiatry 2007;61(3):348–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, et al. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord 2011;44(5):412–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents: Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry 2011;68(7):714–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bulik CM, Sullivan PF, Kendler KS. Medical and psychiatric morbidity in obese women with and without binge eating. Int J Eat Disord 2002;32(1):72–8. [DOI] [PubMed] [Google Scholar]
- [8].Rosenbaum DL, White KS. The relation of anxiety, depression, and stress to binge eating behavior. J Health Psychol 2015;20(6):887–98. [DOI] [PubMed] [Google Scholar]
- [9].Sheehan DV, Herman BK. The psychological and medical factors associated with untreated binge eating disorder. Prim Care Companion CNS Disord 2015;17(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Burton AL, Abbott MJ. Conceptualising binge eating: A review of the theoretical and empirical literature. Behav Chang 2017;34(3):168–98. [Google Scholar]
- [11].Burton AL, Abbott MJ. Processes and pathways to binge eating: Development of an integrated cognitive and behavioural model of binge eating. J Eat Disord 2019;7(18):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Thompson BW. A hunger so wide and so deep: a multiracial view of women’s eating problems. Minneapolis, MN: University of Minnesota Press; 1996. [Google Scholar]
- [13].Katzman MA, Lee S. Beyond body image: the integration of feminist and transcultural theories in the understanding of self starvation. Int J Eat Disord 1997;22:385–94. [DOI] [PubMed] [Google Scholar]
- [14].Harrington EF, Crowther JH, Payne Henrickson HC, Mickelson KD. The relationships among trauma, stress, ethnicity, and binge eating. Cultur Divers Ethnic Minor Psychol 2006;12(2):212–29. [DOI] [PubMed] [Google Scholar]
- [15].Doris E, Shekriladze I, Javakhishvili N, Jones R, Treasure J, Tchanturia K. Is cultural change associated with eating disorders? A systematic review of the literature. Eat Weight Disord 2015;20(2):149–60. [DOI] [PubMed] [Google Scholar]
- [16].Rodgers RF, Berry R, Franko DL. Eating disorders in ethnic minorities: an update. Curr Psychiatry Rep 2018;20:90. [DOI] [PubMed] [Google Scholar]
- [17].Fox M, Thayer ZM, Wadhwa PD. Acculturation and health: the moderating role of sociocultural context. Am Anthropol 2017;119(3):405–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: Structural racism, intersectionality theory, and immigrant health. Soc Sci Med 2012;75:2099–106. [DOI] [PubMed] [Google Scholar]
- [19].Zambrana RE, Carter-Pokras O. Role of acculturation research in advancing science and practice in reducing health care disparities among Latinos. Am J Public Health 2010;100(1):18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Gonzales KL, Noonan C, Goins RT, Henderson WG, Beals J, Manson SM, et al. Assessing the everyday discrimination scale among American Indians and Alaska Natives. Psychol Assess 2016;28(1):51–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Pérez DJ, Fortuna L, Alegría M. Prevalence and correlates of everyday discrimination among U.S. Latinos. J Community Psychol 2008;36(4):421–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, et al. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One 2015;10(9):e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Lee DL, Ahn S. Discrimination against Latina/os: a meta-analysis of individual-level resources and outcomes. Couns Psychol 2012;40(1):28–65. [Google Scholar]
- [24].Franko DL, Coen EJ, Roehrig JP, Rodgers RF, Jenkins A, Lovering ME, et al. Considering J.Lo and Ugly Betty: a qualitative examination of risk factors and prevention targets for body dissatisfaction, eating disorders, and obesity in young Latina women. Body Image 2012;9(3):381–7. [DOI] [PubMed] [Google Scholar]
- [25].Cheney AM. “Most girls want to be skinny”: body (Dis)satisfaction among ethnically diverse women. Qual Health Res 2011;21(10):1347–59. [DOI] [PubMed] [Google Scholar]
- [26].Piran N Embodied possibilities and disruptions: the emergence of the Experience of Embodiment construct from qualitative studies with girls and women. Body Image 2016;18:43–60. [DOI] [PubMed] [Google Scholar]
- [27].Kwan MY, Gordon KH, Minnich AM. An examination of the relationships between acculturative stress, perceived discrimination, and eating disorder symptoms among ethnic minority college students. Eat Behav 2018;28: 25–31. [DOI] [PubMed] [Google Scholar]
- [28].Perez M, Voelz ZR, Pettit JW, Joiner TE. The role of acculturative stress and body dissatisfaction in predicting bulimic symptomatology across ethnic groups. Int J Eat Disord 2002;31:442–54. [DOI] [PubMed] [Google Scholar]
- [29].Velez BL, Campos ID, Moradi B. Relations of sexual objectification and racist discrimination with Latina women’s body image and mental health. Couns Psychol 2015;43(6):906–35. [Google Scholar]
- [30].Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav 1995;Spec No:80–94. [PubMed] [Google Scholar]
- [31].Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health 2013;103(5):813–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Phelan J, Link B. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol 2015;41:311–30. [Google Scholar]
- [33].Crenshaw K Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory, and antiracist politics. Univ Chic Leg Forum 1989;140:139–67. [Google Scholar]
- [34].Collins PH. Black feminist thought: knowledge, consciousness, and the politics of empowerment. New York: Routledge; 1990. [Google Scholar]
- [35].McCall L The complexity of intersectionality. Signs (Chic) 2005;30:1771–800. [Google Scholar]
- [36].Piran N A feminist perspective on risk factor research and on the prevention of eating disorders. Eat Disord 2010;18(3):183–98. [DOI] [PubMed] [Google Scholar]
- [37].Hunger JM, Major B, Blodorn A, Miller CT. Weighed down by stigma: how weight-based social identity threat contributes to weight gain and poor health. Soc Personal Psychol Compass 2015;9(6):255–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Nolan LJ, Eshleman A. Paved with good intentions: paradoxical eating responses to weight stigma. Appetite 2016;102:15–24. [DOI] [PubMed] [Google Scholar]
- [39].Puhl R, Suh Y. Health consequences of weight stigma: implications for obesity prevention and treatment. Curr Obes Rep 2015;4(2):182–90. [DOI] [PubMed] [Google Scholar]
- [40].Watson LB, Lewis JA, Moody AT. A sociocultural examination of body image among black women. Body Image 2019;31:280–7. [DOI] [PubMed] [Google Scholar]
- [41].Mucherah W, Frazier AD. How deep is skin-deep? The relationship between skin color satisfaction, estimation of body image, and self-esteem among women of African descent. J Appl Soc Psychol 2013;43(6):1177–84. [Google Scholar]
- [42].Craddock N, Dlova N, Diedrichs PC. Colourism: a global adolescent health concern. Curr Opin Pediatr 2018;30(4):472–7. [DOI] [PubMed] [Google Scholar]
- [43].Craddock N Colour me beautiful: examining the shades related to global skin tone ideals. J Aesthet Nurs 2016;5(6):287–9. [Google Scholar]
- [44].Alegria M, Takeuchi D, Canino G, Duan N, Shrout P, Meng XL, et al. Considering context, place and culture: the National Latino and Asian American Study. Int J Methods Psychiatr Res 2004;13(4):208–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Alegria M, Jackson JS, Kessler RC, Takeuchi D. Collaborative Psychiatric Epidemiology Surveys (CPES), 2001–2003 [Data set]. Ann Arbor, MI: Interuniversity Consortium for Political and Social Research; 2016. [Google Scholar]
- [46].Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample design and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES). Int J Methods Psychiatr Res 2004;13(4):221–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Pennell BE, Bowers A, Carr D, Chardoul S, Cheung GQ, Dinkelmann K, et al. The development and implementation of the National Comorbidity Survey Replication, the National Survey of American Life, and the National Latino and Asian American Survey. Int J Methods Psychiatr Res 2004;13(4): 241–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Izydorczyk B, Sitnik-Warchulska K. Sociocultural appearance standards and risk factors for eating disorders in adolescents and women of various ages. Front Psychol 2018;9:429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Barzi F, Woodward M. Imputations of missing values in practice: results from imputations of serum cholesterol in 28 cohort studies. Am J Epidemiol 2004;160(1):34–45. [DOI] [PubMed] [Google Scholar]
- [50].Bell BA, Kromrey JD, Ferron JM. Missing data and complex samples: the impact of listwise deletion vs. subpopulation analysis on statistical bias and hypothesis test results when data are MCAR and MAR. Proceedings of the Joint Statistical Meetings, Survey Research Methods Section 2009. p. 4759–70. [Google Scholar]
- [51].Williams DR, Yu Y, Jackson JS, Anderson NB . Racial differences in physical and mental health: socioeconomic status, stress and discrimination. J Health Psychol 1997;2(3):335–51. [DOI] [PubMed] [Google Scholar]
- [52].Reeve BB, Willis G, Shariff-Marco SN, Breen N, Williams DR, Gee GC, et al. Comparing cognitive interviewing and psychometric methods to evaluate a racial/ethnic discrimination scale. Field Methods 2011;23(4):397–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Lewis TT, Yang FM, Jacobs EA, Fitchett G. Racial/ethnic differences in responses to the everyday discrimination scale: a differential item functioning analysis. Am J Epidemiol 2012;175(5):391–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Krieger N Methods for the scientific study of discrimination and health: an ecosocial approach. Am J Public Health 2012;102(5):936–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Viruell-Fuentes EA. Beyond acculturation: Immigration, discrimination, and health research among Mexicans in the United States. Soc Sci Med 2007;65(7):1524–35. [DOI] [PubMed] [Google Scholar]
- [56].Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). 4th ed. Washington, D.C.: American Psychiatric Association; 1994. [Google Scholar]
- [57].Schisterman EF, Cole SR, Platf RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 2009;20(4):488–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Goldschmidt AB, Wall MM, Zhang J, Loth KA, Neumark-Sztainer D. Overeating and binge eating in emerging adulthood: 10-year stability and risk factors. Dev Psychol 2016;52(3):475–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Hilbert A, Pike KM, Goldschmidt AB, Wilfley DE, Fairburn CG, Dohm FA, et al. Risk factors across the eating disorders. Psychiatry Res 2014;220(1–2):500–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Mulders-Jones B, Mitchison D, Girosi F, Hay P. Socioeconomic correlates of eating disorder symptoms in an Australian population-based sample. PLoS One 2017;12(1):e0170603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Lydecker JA, Grilo CM. Food insecurity and bulimia nervosa in the United States. Int J Eat Disord 2019;52(6):735–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, Caraveo-Anduaga J. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California . Arch Gen Psychiatry 1998;55: 771–8. [DOI] [PubMed] [Google Scholar]
- [63].Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull 2002;128(5):825–48. [DOI] [PubMed] [Google Scholar]
- [64].Alegría M, Jackson JS, Kessler RC, Takeuchi D. Collaborative Psychiatric Epidemiology Surveys (CPES), 2001–2003 [United States] User Guide. Ann Arbor, MI: Interuniversity Consortium for Political and Social Research; 2016. [Google Scholar]
- [65].Defining adult overweight and obesity. Washington, D.C.: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- [66].Lo CC, Cheng TC. Social status, discrimination, and minority individuals’ mental health: a secondary analysis of US national surveys. J Racial Ethn Heal Disparities 2018;5(3):485–94. [DOI] [PubMed] [Google Scholar]
- [67].Higgins Neyland MK, Bardone-Cone AM. Tests of escape theory of binge eating among Latinas. Cultur Divers Ethnic Minor Psychol 2017;23(3):373–81. [DOI] [PubMed] [Google Scholar]
- [68].Lin SL. Examining ethnicity-related risk factors for eating disorder symptoms in African American, Asian American, Latina, and Caucasian Women. University of North Carolina at Chapel Hill; 2018. https://cdr.lib.unc.edu/concern/dissertations/7w62fd38k. [Accessed 3 February 2020]. [Google Scholar]
- [69].Flores A How the U.S. Hispanic population is changing. 2017. https://www.pewresearch.org/fact-tank/2017/09/18/how-the-u-s-hispanic-population-is-changing/. [Accessed 28 February 2020].
- [70].Lopez MH, Gonzales-Barrera A, Krogstad JM. More Latinos have serious concerns about their place in America Under Trump. 2018. https://www.pewresearch.org/hispanic/wp-content/uploads/sites/5/2018/10/Pew-Research-Center_Latinos-have-Serious-Concerns-About-Their-Place-in-America_2018-10-25.pdf. [Accessed 28 February 2020].
- [71].Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity 2009;17:941–64. [DOI] [PubMed] [Google Scholar]
- [72].Russell K, Wilson M, Hall R. The color complex (revised): the politics of skin color in a new millennium. New York City, NY: Anchor Books; 2013. [Google Scholar]
- [73].Maralani V, McKee D. Obesity is in the eye of the beholder: BMI and socioeconomic outcomes across cohorts. Sociol Sci 2017;4:288–317. [Google Scholar]
- [74].Nutter S, Russell-Mayhew S, Alberga AS, Arthur N, Kassan A, Lund DE, et al. Positioning of weight bias: moving towards social justice. J Obes 2016;2016: 3753650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Reece RL. Coloring weight stigma: on race, colorism, weight stigma, and the failure of additive intersectionality. Sociol Race Ethn 2019;5(3):1–13. [Google Scholar]
- [76].Hunter ML . “If you’re light you’re alright”: Light skin color as social capital for women of color. Gend Soc 2002;16(2):175–93. [Google Scholar]
- [77].Hunter ML. The persistent problem of colorism: skin tone, status, and inequality. Sociol Compass 2007;1(1):237–54. [Google Scholar]
- [78].Himmelstein MS, Puhl RM, Quinn DM. Intersectionality: an understudied framework for addressing weight stigma. Am J Prev Med 2017;53(4):421–31. [DOI] [PubMed] [Google Scholar]
- [79].Cuevas AG, Dawson BA, Williams DR. Race and skin color in Latino health: an analytic review. Am J Public Health 2016;106(12):2131–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Parker K, Morin R, Horowitz J, Lopez MH, Rohal M. Multiracial in America: proud, diverse, and growing in numbers. Washington, DC: Pew Research Center; 2015. [Google Scholar]
- [81].Borrell LN. Racial identity among Hispanics: Implications for health and well-being. Am J Public Health 2005;95(3):379–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Quiros L, Dawson BA. The color paradigm: the impact of colorism on the racial identity and identification of Latinas. J Hum Behav Soc Environ 2013;23(3): 287–97. [Google Scholar]
- [83].Bowleg L When Black + lesbian + woman s Black lesbian woman: the methodological challenges of qualitative and quantitative intersectionality research. Sex Roles 2008;59:312–25. [Google Scholar]
- [84].Scheim AI, Bauer GR. The Intersectional Discrimination Index: development and validation of measures of self-reported enacted and anticipated discrimination for intercategorical analysis. Soc Sci Med 2019;226:236–45. [DOI] [PubMed] [Google Scholar]
- [85].Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med 2014;110:10–7. [DOI] [PubMed] [Google Scholar]
- [86].Bowleg L, Bauer G. Invited reflection: quantifying intersectionality. Psychol Women Q 2016;40:337–41. [Google Scholar]
- [87].McLaren L, Piran N. Prevention of disordered eating through structural change: the population health framework and lessons from case studies in intensive community-based interventions In: Preventing eating-related and weight-related disorders: collaborative research, advocacy, and policy change. Ontario, Canada: Wilfrid Laurier University Press; 2012. p. 45–70. [Google Scholar]
- [88].Austin SB. A public health approach to eating disorders prevention: it’s time for public health professionals to take a seat at the table. BMC Public Health 2012;12:854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Holmes S ‘Blindness to the obvious’? Treatment experiences and feminist approaches to eating disorders. Fem Psychol 2016;26(4):464–86. [Google Scholar]
- [90].Holmes S, Drake S, Odgers K, Wilson J. Feminist approaches to Anorexia Nervosa: a qualitative study of a treatment group. J Eat Disord 2017;5:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Thapliyal P, Hay P, Conti J. Role of gender in the treatment experiences of people with an eating disorder: a metasynthesis. J Eat Disord 2018;6:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Nichols VC, Lebrón AMW, Pedraza FI. Policing us sick: the health of Latinos in an era of heightened deportations and racialized policing. PS Polit Sci Polit 2018;51(2):293–7. [Google Scholar]
- [93].Vargas ED, Sanchez GR, Juárez M. Fear by association: perceptions of anti-immigrant policy and health outcomes. J Health Polit Policy Law 2017;42(3):459–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Bruzelius E, Baum A. The mental health of Hispanic/Latino Americans following national immigration policy changes: United States, 2014–2018. Am J Public Health 2019;109(12):1786–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Call C, Walsh BT, Attia E. From DSM-IV to DSM-5: changes to eating disorder diagnoses. Curr Opin Psychiatry 2013;26(6):532–6. [DOI] [PubMed] [Google Scholar]
- [96].Syed M. Disciplinarity and methodology in intersectionality theory and research. Am Psychol 2010;65(1):61–2. [DOI] [PubMed] [Google Scholar]
- [97].Beccia AL, Baek J, Jesdale WM, Austin SB, Forrester S, Curtin C, et al. Risk of disordered eating at the intersection of gender and racial/ethnic identity among U.S. high school students. Eat Behav 2019;34:101299. [DOI] [PubMed] [Google Scholar]
- [98].Austin SB, Nelson LA, Birkett MA, Calzo JP, Everett B. Eating disorder symptoms and obesity at the intersections of gender, ethnicity, and sexual orientation in US high school students. Am J Public Health 2013;103(2):e16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]