Abstract
Background
Within 4 months of COVID-19 first being reported in the USA, it spread to every state and to more than 90% of all counties. During this period, the US COVID-19 response was highly decentralised, with stay-at-home directives issued by state and local officials, subject to varying levels of enforcement. The absence of a centralised policy and timeline combined with the complex dynamics of human mobility and the variable intensity of local outbreaks makes assessing the effect of large-scale social distancing on COVID-19 transmission in the USA a challenge.
Methods
We used daily mobility data derived from aggregated and anonymised cell (mobile) phone data, provided by Teralytics (Zürich, Switzerland) from Jan 1 to April 20, 2020, to capture real-time trends in movement patterns for each US county, and used these data to generate a social distancing metric. We used epidemiological data to compute the COVID-19 growth rate ratio for a given county on a given day. Using these metrics, we evaluated how social distancing, measured by the relative change in mobility, affected the rate of new infections in the 25 counties in the USA with the highest number of confirmed cases on April 16, 2020, by fitting a statistical model for each county.
Findings
Our analysis revealed that mobility patterns are strongly correlated with decreased COVID-19 case growth rates for the most affected counties in the USA, with Pearson correlation coefficients above 0·7 for 20 of the 25 counties evaluated. Additionally, the effect of changes in mobility patterns, which dropped by 35–63% relative to the normal conditions, on COVID-19 transmission are not likely to be perceptible for 9–12 days, and potentially up to 3 weeks, which is consistent with the incubation time of severe acute respiratory syndrome coronavirus 2 plus additional time for reporting. We also show evidence that behavioural changes were already underway in many US counties days to weeks before state-level or local-level stay-at-home policies were implemented, implying that individuals anticipated public health directives where social distancing was adopted, despite a mixed political message.
Interpretation
This study strongly supports a role of social distancing as an effective way to mitigate COVID-19 transmission in the USA. Until a COVID-19 vaccine is widely available, social distancing will remain one of the primary measures to combat disease spread, and these findings should serve to support more timely policy making around social distancing in the USA in the future.
Funding
None.
Introduction
A cluster of cases of pneumonia of unknown cause in Wuhan, China, was first reported on Dec 31, 2019,1 and a week later identified as the disease now called COVID-19.2 COVID-19 has since spread rapidly around the world, nearing 10 million confirmed cases and more than 500 000 deaths reported in 188 countries and regions as of June 25, 2020.3 The first case of COVID-19 in the USA was reported on Jan 20, 2020, in Snohomish County, WA, and as of June 25, COVID-19 has been reported in every US state and more than 3000 US counties.4, 5 Until the widespread availability of a vaccine, social distancing alongside personal protective measures, such as handwashing and wearing a mask, will remain the primary control mechanisms for mitigating the spread of COVID-19.
In China, a nationally coordinated effort limiting travel and social interaction effectively mitigated the spread of the disease.6, 7 Crucially, by contrast with the nationally mandated directives put in place in China, the US directives to shelter in place and temporarily close non-essential businesses and schools were made at the state and local level throughout March and April, 2020 (appendix pp 2, 12–13). This distributed decision-making process and variable enforcement resulted in an outbreak mitigation response that was highly variable in both space and time. Adding to this complexity is the varying intensities of the outbreak around the USA, with some counties nearing their peak and others remaining in the early stages of an epidemic.5 Together, these issues pose a significant challenge to evaluating the effectiveness of social distancing policies in the USA. To address this issue, we used real-time mobility data derived from cell (mobile) phone data to quantify the progression of social distancing within the USA. Subsequently, we examined the relationship of the data to the rate of emerging COVID-19 cases in 25 US counties, with the highest number of reported cases as of April 16, 2020 (table ; appendix p 3).
Table.
The selected 25 US counties and the associated Pearson correlation coefficient and generalised linear model coefficients (intercept and slope) between 11-day lagged mobility ratio and growth rate ratio
| Correlation coefficient | Intercept | Slope | |
|---|---|---|---|
| Essex, NJ (34013) | 0·90 | 0·86 | 0·26 |
| New York City, NY* (36061) | 0·86 | 0·94 | 0·14 |
| Middlesex, NJ (34023) | 0·85 | 0·89 | 0·24 |
| Cook, IL (17031) | 0·85 | 0·89 | 0·22 |
| Hudson, NJ (34017) | 0·84 | 0·90 | 0·23 |
| Nassau, NY (36059) | 0·84 | 0·89 | 0·22 |
| Union, NJ (34039) | 0·84 | 0·85 | 0·28 |
| Middlesex, MA (25017) | 0·83 | 0·90 | 0·24 |
| Suffolk, NY (36103) | 0·83 | 0·85 | 0·26 |
| Miami-Dade, FL (12086) | 0·83 | 0·86 | 0·28 |
| Bergen, NJ (34003) | 0·82 | 0·87 | 0·24 |
| Passaic, NJ (34031) | 0·81 | 0·87 | 0·26 |
| Suffolk, MA (25025) | 0·81 | 0·90 | 0·27 |
| Philadelphia, PA (42101) | 0·80 | 0·84 | 0·33 |
| Wayne, MI (26163) | 0·80 | 0·82 | 0·32 |
| Westchester, NY (36119) | 0·80 | 0·88 | 0·22 |
| Monmouth, NJ (34025) | 0·76 | 0·83 | 0·28 |
| Rockland, NY (36087) | 0·74 | 0·81 | 0·36 |
| Jefferson, LA (22051) | 0·71 | 0·77 | 0·38 |
| Oakland, MI (26125) | 0·71 | 0·86 | 0·27 |
| Orange, NY (36071) | 0·66 | 0·80 | 0·34 |
| Los Angeles, CA (06037) | 0·62 | 0·89 | 0·22 |
| Fairfield, CT (09001) | 0·61 | 0·85 | 0·27 |
| Orleans, LA (22071) | 0·61 | 0·84 | 0·26 |
| Harris, TX (48201) | 0·53 | 0·78 | 0·38 |
| All counties | 0·71 | 0·88 | 0·24 |
The list is presented by the correlation coefficient in descending order. The last row represents the results of a single model for all 25 US counties. All coefficients are statistically significant at 95% CI. Federal Information Processing Standards code for each county is given.
To be consistent with the Johns Hopkins University Center for Systems Science and Engineering COVID-19 dashboard reporting,5 New York City is used to represent New York County, Queens County, Bronx County, Kings County, and Richmond County in one location.
Research in context.
Evidence before this study
Our study considers the relationship between the emerging dynamics of COVID-19 transmission and mobility in the USA; therefore, we took into consideration the few publications that address this issue from a robust, data-driven perspective. We used Google Scholar, PubMed, and medRxiv to search for articles relating mobility to coronavirus, using the terms “Covid-19,” “SARS-CoV-2,” “coronavirus,” “mobility”, “travel”, and “social distancing”. The studies identified from this search concluded that travel reduction had a positive effect on reducing the transmission of COVID-19. However, the only studies that used data to reach this conclusion were done using information from China; thus, empirical evidence about the efficacy of social distancing is still needed to understand its effect on COVID-19 transmission in the USA.
Added value of this study
Our results are consistent with COVID-19 transmission research to date—namely, that decreased mobility has a significant, positive relationship with reduced case growth. Although social distancing has consistently been shown to have positive effects on COVID-19 transmission in China, our work extends these results to the USA. Our study does not rely on assumed infection rates, assumed compliance aligned with timing of policies, or modelled or synthetic data, but rather uses real-world mobility data and reported case counts to empirically estimate the relationship between the two variables in the USA.
Implications of all the available evidence
Our work shows that social distancing helps to reduce the spread of COVID-19, and should remain part of personal and institutional responses to the pandemic until a vaccine is widely available.
Previous studies have evaluated the connection between travel and transmission of COVID-19, but these studies were restricted to examining the disease in China. In addition to the aforementioned work by Kraemer and colleagues,7 Zhao and colleagues8 found a positive association between confirmed cases and the quantity of domestic passenger travel within ten cities outside of Hubei province. Tian and colleagues9 found evidence that social distancing measures in cities throughout China delayed case transmission. Chinazzi and colleagues10 used a transmission model to project the effect of travel limitations on the spread of COVID-19 in China; they found travel restrictions to the affected areas had modest effects, and that transmission reduction interventions were more effective at mitigating COVID-19 spread. These studies are encouraging, and suggest social distancing measures should successfully mitigate infection transmission outside of China; however, this has not yet been shown. Qualitative studies and projections exist for social distancing helping to reduce the spread of COVID-19 in countries such as Italy and the USA but, to date, a quantitative analysis has not yet been done outside of China.11, 12, 13 We therefore evaluated the effect of social distancing on the spread of COVID-19 in the USA—the country that has reported the most confirmed cases and deaths because of COVID-19 globally.
Methods
Data collection and analysis
To quantify the amount of social distancing in each US county, we defined a mobility ratio (MR) for each day (t) and county (j), which quantified the change in mobility patterns as a proxy for social distancing. MR reflects the change in the number of individual trips made in each county per day, relative to ordinary behavioural patterns (ie, before COVID-19). To compute this measure, we used daily origin–destination trip matrices at the US county level derived from aggregated and anonymised cell phone data obtained from Teralytics (Zürich, Switzerland). This effort aligns with work14 supporting the use of aggregated mobility data to monitor the effectiveness of social distancing interventions. The data consisted of the number of unique daily trips made between origin–destination pairs of US counties, each day, from Jan 1 to April 20, 2020. MR is the sum of the total trips incoming, outgoing, and within each county on a given day, divided by the same measure on a baseline day. The baseline value is specific to each day of the week and taken as the average from Jan 8 to Jan 31, 2020, when travel patterns were stable (appendix p 4). We interpreted this metric as a proxy for social distancing on the basis of the assumption that when individuals make fewer trips, they physically interact less. MR j t was calculated as follows:
where V i t j represents the number of trips from county i to j on day t, and t 0 represents the baseline measure. The trips were all-directional; therefore, the number of trips from i to j did not equal the number of trips from j to i. This metric accounts for movements both between and within counties; thus, it includes changes in typical commuting patterns and microlevel (within county) movements (eg, travel to local grocery stores, shopping centres, gyms, and schools).
Using this function, an MR of 0 indicates no trips were made, and a value of 0·5 indicates half the number of trips relative to baseline were made on a given day. An MR of 1 signifies no change in behaviour relative to the baseline period (Jan 8–31, 2020), before COVID-19 transmission was widely reported in the USA. Any value above 1 means that mobility had increased from baseline.
Epidemiological data from the Johns Hopkins University Center for Systems Science and Engineering COVID-19 dashboard, which includes daily data on cases and deaths for each US county, were used to compute the COVID-19 growth rate ratio (GR) for a given county on a given day.5 The ratio was defined as the logarithmic rate of change (number of newly reported cases) over the previous 3 days relative to the logarithmic rate of change over the previous week. GR for any county j on a day t was calculated as follows:
where C j t is the number of new cases reported in county j on a day t.
GR could take on any non-negative value and is defined only when the average number of reported cases per day is greater than one over any period (3-day or 7-day moving averages). GR equals 0 when an average of one new case per day was reported over the last 3 days, and at least seven new confirmed cases reported over the last week. GR equals 1 when there was no change in the growth rates since last week (ie, the average number of new cases per day over the last 3 days was the same as the average over the last 7 days). A GR below 1 means that the growth rate during the last 3 days was lower than that of the last week, whereas a value greater than 1 represented a growth rate increase in the last 3 days relative to the last week. We used moving averages to smooth volatile case reporting data. This metric, used in conjunction with the social distancing proxy MR, allowed us to grasp the complex and time-dependent dynamics at play between human mobility and COVID-19 spread for each county in the USA.
Using the two aforementioned metrics, we evaluated if and how well social distancing affects the rate of new infections in the 25 counties in the USA with the highest number of confirmed cases on April 16, 2020. King County, WA, was excluded because its initial outbreak preceded the time period considered in our analysis, and was driven by an infection source that differed from other outbreaks in the USA. We fitted a generalised linear model (GLM) for each county, specifically using lagged MR as a predictor of COVID-19 growth rate and tested the correlation of MR and GR at different time lags. The correlation between MR and GR was computed from separate models for each county as well as a combined single model for all counties. Additionally, the most highly correlated lag range was identified based on the (maximum) mean and (minimum) SD of the correlations across all counties, based on the Pearson correlation coefficient.
Role of the funding source
There was no funding source for this study. All corresponding authors had full access to all the data in the study and shared the final responsibility for the decision to submit for publication.
Results
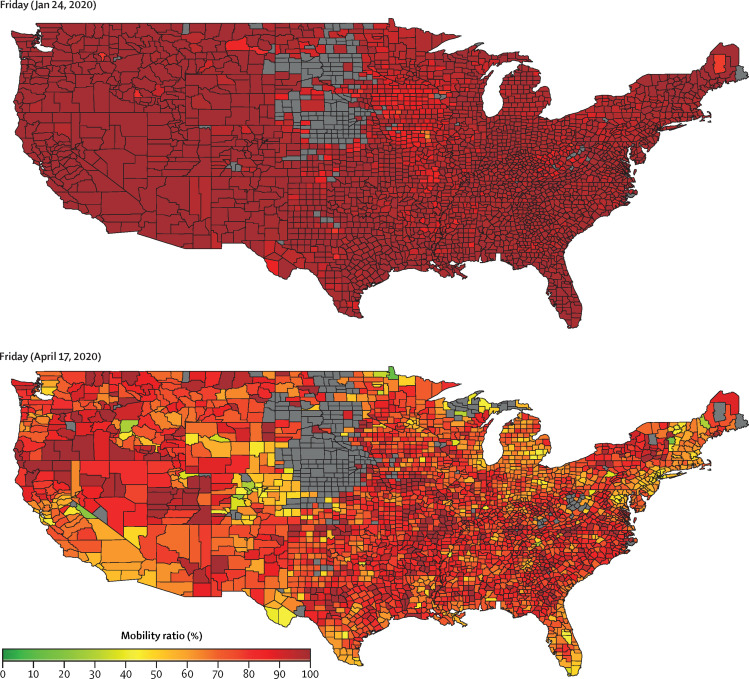
The differences in county-level MR across the USA from Jan 24 to April 17, 2020, are illustrated in figure 1 , and shown at a daily resolution in the video. For the 25 US counties with the highest number of reported cases, the MR as of April 17 are shown in the appendix (p 5). The MR for these 25 counties ranged from 0·35 in New York City to 0·63 in Harris County, TX, which highlights the varying MR measures and associated behavioural changes around the country. Counties with the most social distancing in the first week of April were predominantly in New York, New Jersey, and Massachusetts—the locations that reported the most COVID-19 cases at the time.
Figure 1.
Mobility ratio for each US county on Friday, Jan 24, 2020 (top), and on Friday, April 17, 2020 (bottom)
The greyed-out areas in the Midwest are filtered because of low coverage in the Teralytics dataset.14 This includes all counties with total trip counts less than two SDs below the mean.
For the set of 11 states corresponding to the top 25 counties (appendix p 6), similar MR behaviour was observed at the state level. The complete list of all US states ranked by their respective MR as of April 17 is provided in the appendix (p 7). Consistent with county-level behaviour, there was evidence of different levels of social distancing across states, with only Washington DC reducing trips to below 50% of the baseline rate, and the rest of the 50 states moving around 53–90% of baseline levels. Many of the southern states, which implemented temporary closure of non-essential business later in March or early April, reported higher MRs.
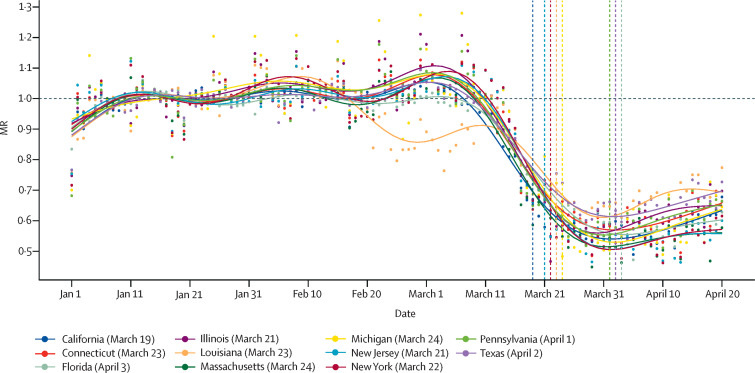
The relationship between the state's MR trends over time and the timing of the state-level social distancing directives are illustrated in figure 2 (appendix pp 12–13). In addition to the timing of the state-level directives, we collected information on the county-level social distancing directives that were implemented in each of the 25 counties of focus. A list of all local directives and respective dates is provided in the appendix (pp 14–18), and includes the time between local-level and state-level actions. Figure 2 illustrates that social distancing began in early March, well before the first US state-level stay-at-home directive (implemented by California on March 19). While the county-level directives partly explain the earlier decline in MR, which began well before the state-level directives were put in place, all states illustrated some level of social distancing before county-level directives were enacted.
Figure 2.
Timeseries of MR for US states and the corresponding dates of stay-at-home orders
The dots represent the raw MR data while the plotted lines are smoothed using a generalised additive model. Vertical dashed lines are stay-at-home orders (dates listed in the appendix pp 12–13). Some orders occurred on the same day; thus, only eight of 11 orders are visible. MR=mobility ratio.
The relationship between state and local directives and MR for each of the selected 25 counties is illustrated in the appendix (p 8). To explore how internal trips (ie, movements within a county) might vary from the total county trips (including incoming and outgoing), within-county trips only are presented in the appendix (p 9). From the results of this county-level breakdown, locations such as Bergen, NJ, Oakland, MI, Orange, NY, and Fairfield, CT, implemented local directives much earlier than their corresponding states, which better align with the start of MR decline in these counties. By contrast, in Orleans and Jefferson, LA, where local-level directives were implemented late or not at all, MR was declining for weeks without directives in place, suggesting this behavioural change was driven by other means. For all 25 counties, except for Jefferson, LA, local directives were implemented at least 3–17 days before the state-level stay-at-home directives, with an average difference of 7·3 days.
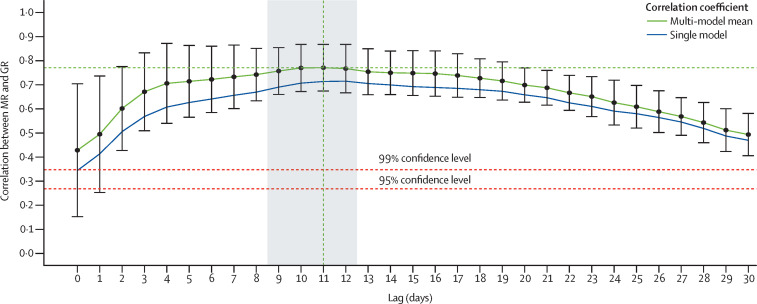
Using MR and GR, we evaluated how social distancing influenced the rate of new infections in the 25 counties with the highest number of confirmed cases on April 16, 2020, by fitting a GLM model for each county (and one for all counties), using lagged MR as a predictor of COVID-19 growth rate. An optimal lag of 11 days, with a window of 9–12 days was identified (figure 3 ; table). Furthermore, the correlation remained above 0·7 for up to 20 days. This lag was the period separating the beginning of social distancing and onset of case growth reduction. An interval of this length was consistent with the estimated 4-day to 5-day (median) incubation period of severe acute respiratory syndrome coronavirus 2 plus additional time for reporting.15, 16, 17 The CIs shown on the curve of figure 3 illustrate that this estimated lag interval was robust and consistent across multiple counties.
Figure 3.
Correlations between MR and GR at different lags (in days) for the single all-county model and the mean and SDs of the county-specific model
All correlations are significant at a 95% CIs. An optimal lag of 11 days is noted by the vertical green dotted line, with the window of 9–12 days highlighted in grey. MR=mobility ratio. GR=growth rate ratio.
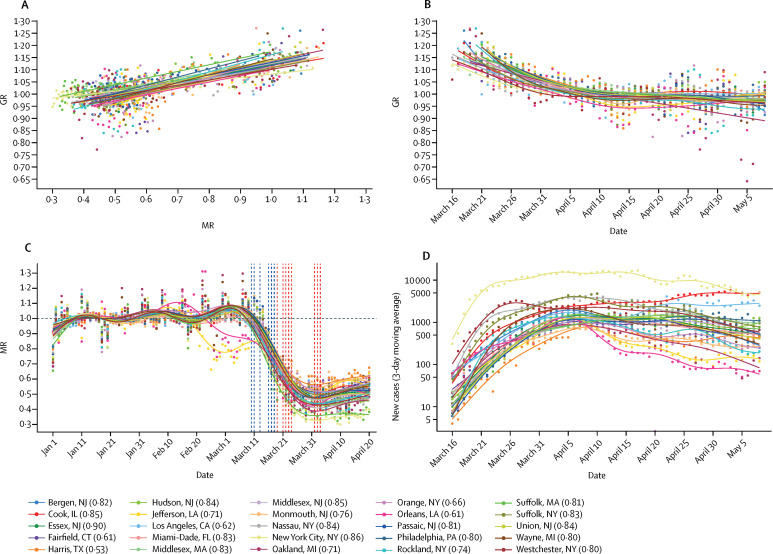
The county-specific correlations between MR and GR, for an 11-day lag, alongside the computed GR, MR, and number of daily COVID-19 cases from March 16 to May 4, are illustrated in figure 4 . The case data show the number of new daily cases for all 25 counties increases through March, then slows in April in many counties, and begins decreasing in some counties. During the same period, MR steadily decreases, specifically during the second half of March, before stabilising for most locations in early April, followed by a slight increase throughout April.
Figure 4.
Relationship between MR and GR given 11-day lag (A), with GR (B), progression of MR (C), and new confirmed cases (D)
Correlations found to be significant at a 95% CI. Dates of state-level stay-at-home orders are shown as vertical dashed red lines, and local-level social distancing orders are shown as dashed blue lines. The dots represent the raw data, and the plotted lines are smoothed using a generalised additive model. GR=growth rate ratio. MR=mobility ratio.
In almost all counties, the initial decline in MR began before any formal regulation was put in place (figure 4; appendix pp 8–9). The GR showed a general decreasing trend for all locations through March, stabilising around 1 in April, which was consistent with the case curves. All correlations were significant at a 95% CI, with Pearson correlation coefficients for 20 of the 25 counties above 0·7 (table). These high correlations suggest that social distancing had a significant effect on the spread of COVID-19. Some exceptions include Orleans, LA (correlation coefficient of 0·61), which can be attributed to an outbreak that emerged before social distancing was common practice, and Harris County, TX (correlation coefficient of 0·53), which was probably underestimated because of limited testing rates in Texas.18 The results of a single model that includes all counties is listed in the table, and is consistent with the individual county-level analysis. The consistency across results suggests the results are robust, and transferable to other locations in the USA, thus providing a more generalised finding about the effect of social distancing on case growth rates within the USA.
We repeated the equivalent evaluation method at the state level, using aggregated case reports from all the counties within each state. The results were consistent with the county-level analysis, revealing a 9–12-day lag window (appendix p 10), and displaying similarly high correlations between MR and GR (appendix p 11). The lowest correlation, 0·7, was observed for Massachusetts, which was likely a result of spatial variability, specifically with regards to the state of the outbreak, testing capabilities, and varied degrees of behavioural change associated with social distancing measures.
Discussion
The USA has enacted a complex combination of responses to COVID-19. Government policy varies in space, scale, and time (table; appendix pp 14–18), resulting in varied patterns of movement and behavioural changes throughout the country. Simultaneously, the progression and intensity of local outbreaks differs markedly by location. This landscape makes quantifying the effect of social distancing on COVID-19 spread a non-trivial task. Nevertheless, our method captured relevant trends in human behaviour as it related to the spread of the disease. Because our analysis used real-time mobility data, we captured the dynamics of social distancing without relying on assumed efficacy of shelter-in-place orders. Additionally, we used the real-world frequency of trips, not extrapolated transmission rates or travel distances, as our mobility indicator. This means our mobility metric was driven by how much people actually moved between and within counties. Because our case data consist of reported cases at the county level, our analysis is a powerful comparison of actual human behaviour and the documented status of COVID-19 in the USA.
Our results used this real-world data to show a strong and statistically significant correlation between social distancing, quantified by mobility patterns, and reduction of COVID-19 case growth. Importantly, our statistical analysis revealed that the effect of social distancing on decreasing transmission is not likely to be perceptible for at least 9–12 days after implementation, and might be longer. This lag time reflects the time for symptoms to manifest after infection, worsen, and be reported. Besides emphasising its necessity, this study also revealed that social distancing (and outbreak growth deceleration) in the counties most affected by COVID-19 was driven primarily by changes in individual-level behaviour and local-level regulations; the state (and federal) actions were implemented either too late (or not at all). The motivation behind the individual-level behavioural changes requires further study, but could possibly be attributed to educational and data-tracking resources, as well as media and information sharing, which might vary substantially by information source, location, and time. These findings show that it is within the power of each US resident, even without government mandates, to help slow the spread of COVID-19. Crucially, if individual-level and local actions were not taken, and social distancing behaviour was delayed until the state-level directives were implemented, COVID-19 would have been able to circulate unmitigated for additional weeks in most locations, inevitably resulting in more infections and deaths. Additionally, the strong relationship between social distancing and reduced case growth rates suggests that a return to baseline mobility poses a significant risk of increased infections, which will probably not appear for up to 3 weeks after the mobility increases. However, practices such as handwashing, face mask use, and self-isolation when sick might help to mitigate future case growth, even under more normal mobility patterns, and these behaviours might be more widespread in the future than they were during the initial months of the pandemic in the USA.
This study has multiple limitations. First, we focused on quantifying the relationship between mobility patterns and case growth rates; therefore, the role of other potential mitigating factors (eg, wearing face masks and handwashing) that could also have contributed to the decline in the case growth rate observed during March are not accounted for. However, without detailed county-level compliance data for each type of mitigating action, we were unable to model the relative effect of each factor. Similarly, our travel data did not enable us to identify trip purpose, and therefore we did not differentiate between low-risk and high-risk trips—eg, multiple trips alone to a park are probably lower risk than a single unmitigated trip to a grocery store. Although these topics are outside the scope of this study, they are critical to our understanding of COVID-19 transmission risk, and require further exploration. Second, we used the GR as our representative variable for the degree of transmission occurring in a region. We believe this variable is an intuitive and representative estimate for the spread of COVID-19 among a local population, but future extensions of this analysis should explore replacing this variable with more traditional transmission indexes commonly used in infectious disease epidemiology. Third, the case data might have errors due to both reporting issues and limited testing capacity, especially in early March before widespread testing was underway. We partly address this issue by starting our analysis on March 16, as well as using a 3-day moving average for the case data. Fourth, the analysis was focused on 25 counties, which might be a biased sample of locations; however, we believe these locations accurately capture the relationship between mobility patterns and case growth rates. The consistency among the estimated model parameters presented in the table suggests that the results are generalisable and might be transferred to other locations in the USA and abroad. In addition, our results are consistent at both the county and state level. Finally, the data used in this analysis do not include sociodemographic information; therefore, it might not representatively capture all groups, such as older adults and individuals with chronic medical disorders and comorbidities, low-income groups, and other traditionally underserved communities, for whom social distancing might be difficult to maintain.
Our results strongly support the conclusion that social distancing played a crucial role in the reduction of case growth rates in multiple US counties during March and April. It might be difficult to recognise the value in safe behaviour when the reward is not obvious, and the danger is not immediate. This is particularly true given the economic and social repercussions of the COVID-19 response. Nevertheless, given the absence of proven antiviral drugs or a vaccine, social distancing is one of the most important and timely ways to combat the spread of COVID-19.19, 20 These findings also highlight the difference in pandemic control policy between the USA and China, and should serve to support more timely policy making in the USA in the future. This finding is particularly relevant as the USA begins to loosen stay-at-home orders, once again doing so in a highly decentralised manner. As we continue to grapple with the ramifications of the COVID-19 pandemic on our health, society, and economy, we hope that our results will motivate both individuals and governments to make safe and data-driven decisions, and acknowledge the effect these choices have on all of our communities.
Contributors
LMG conceived and supervised the study. HSB and LMG designed the experiments and analysed the model results. HSB developed the model, did the computational analysis, and prepared all figures. ED, HD, and MMS collected, processed, analysed, and contributed data. HSB, MM, MMS, and LMG drafted the original Article. All authors contributed to the editing of the Article. All authors read and approved the final Article.
Declaration of interests
We declare no competing interests.
Supplementary Materials
The 7-day moving average of the mobility ratio timeseries until April 20, 2020, for all US counties nationwide
The greyed-out areas in the Midwest are filtered because of low coverage in the Teralytics dataset. This includes all counties with a total trip counts less than two SDs below the mean.
YouTube link: https://youtu.be/w020G4NU0ps
References
- 1.WHO . World Health Organization; Geneva: 2020. Pneumonia of unknown cause–China. Jan 5, 2020.https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china [Google Scholar]
- 2.WHO . World Health Organization; Geneva: 2020. Jan 12, 2020. Novel coronavirus–China; emergencies preparedness, response.https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china [Google Scholar]
- 3.WHO . World Health Organization; Geneva: 2020. Coronavirus disease 2019 (COVID-2019). Situation report 106. May 5, 2020.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [Google Scholar]
- 4.Holshue ML, DeBolt C, Lingquist S, et al. Washington State 2019-nCov case investigation team, first case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–554. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bi Q, Wu Y, Mei S, et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30287-5. published online April 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kraemer MUG, Yang C, Gutierrez B, et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao S, Zhuang Z, Cao P, et al. Quantifying the association between domestic travel and the exportation of novel coronavirus (2019-nCov) cases from Wuhan, China in 2020: a correlational analysis. J Travel Med. 2020;27:1–3. doi: 10.1093/jtm/taaa022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tian H, Liu Y, Li Y, et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368:638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chinazzi M, Davis JT, Ajelli M, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368:395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sjodin H, Wilder-Smith A, Osman S, Farooq Z, Rocklov J. Only strict quarantine measures can curb the coronvirus disease (COVID-19) outbreak in Italy, 2020. Euro Surveill. 2020;25:1–5. doi: 10.2807/1560-7917.ES.2020.25.13.2000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860–868. doi: 10.1126/science.abb5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kucharski AJ, Russell TW, Diamond C, et al. Early dynamics and control of COVID-19: a mathematical modelling study. Lancet Inf Dis. 2020;20:553–558. doi: 10.1016/S1473-3099(20)30144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buckee CO, Balsari S, Chan J, et al. Aggregated mobility data could help fight COVID-19. Science. 2020;368:145–146. doi: 10.1126/science.abb8021. [DOI] [PubMed] [Google Scholar]
- 15.Guan WJ, Ni ZY, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Internal Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.COVID Tracking Project US COVID-19 testing data. 2020. https://covidtracking.com
- 19.US CDC . US Centers for Disease Control and Prevention; 2020. Social distancing. April 4, 2020.https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html [Google Scholar]
- 20.WHO . World Health Organization; Geneva: 2020. Advice for public. March 18, 2020.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The 7-day moving average of the mobility ratio timeseries until April 20, 2020, for all US counties nationwide
The greyed-out areas in the Midwest are filtered because of low coverage in the Teralytics dataset. This includes all counties with a total trip counts less than two SDs below the mean.
YouTube link: https://youtu.be/w020G4NU0ps