Abstract
Background Relaxation of laws and regulations around privacy and billing during the COVID-19 pandemic provide expanded opportunities to use telehealth to provide patient care at a distance. Many health systems have transitioned to providing outpatient care via telehealth; however, there is an opportunity to utilize telehealth for inpatients to promote physical distancing.
Objective This article evaluates the use of a rapidly implemented, secure inpatient telehealth program.
Methods We assembled a multidisciplinary team to rapidly design, implement, and iteratively improve an inpatient telehealth quality improvement initiative using an existing videoconferencing system at our academic medical center. We assigned each hospital bed space a unique meeting link and updated the meeting password for each new patient. Patients and families were encouraged to use their own mobile devices to join meetings when possible.
Results Within 7 weeks of go-live, we hosted 1,820 inpatient telehealth sessions (13.3 sessions per 100 bedded days). We logged 104,647 minutes of inpatient telehealth time with a median session duration of 22 minutes (range 1–1,961). There were 5,288 participant devices used with a mean of 3 devices per telehealth session (range 2–22). Clinicians found they were able to build rapport and perform a reasonable physical exam.
Conclusion We successfully implemented and scaled a secure inpatient telehealth program using an existing videoconferencing system in less than 1 week. Our implementation provided an intuitive naming convention for providers and capitalized on the broad availability of smartphones and tablets. Initial comments from clinicians suggest the system was useful; however, further work is needed to streamline initial setup for patients and families as well as care coordination to support clinician communication and workflows. Numerous use cases identified suggest a role for inpatient telehealth will remain after the COVID-19 crisis underscoring the importance of lasting regulatory reform.
Keywords: COVID-19, coronavirus, telemedicine, inpatients, hospital medicine
Background and Significance
In December 2019 reports of a novel coronavirus emerged from Wuhan, China, from patients with pneumonia. 1 2 Over the following months, the virus (COVID-19) spread uncontrolled and developed into a global pandemic. 3 The rapid spread of COVID-19 and evidence that public health measures such as physical distancing can mitigate pandemic influenza 4 5 has resulted in governments and health systems around the globe working to identify ways to slow the rate of infection to avoid overwhelming hospitals with sick patients. In addition, the pandemic has drastically increased the use of personal protective equipment (PPE) while also threatening the supply chain to replenish hospital stock. 6 7
For decades, telecommunication systems have been used to provide health care (telehealth) to those without access such as rural communities, prisons, and the military. 8 For hospitalized patients there are numerous reports of using telehealth for rapid evaluation for intensive care and subspecialty consults such as dermatology, infectious diseases, and psychiatry, where a thorough chart review, history, and visual exam may provide consultants with sufficient information to make clinical recommendations. 9 10 11 12 13 14 15 16 17 18 Telehealth has also been used to engage patients and families in their care during and after hospitalization. 19 20 21 One major limitation to the widespread adoption of telehealth initiatives has been the lack of payment models 22 however, in response to the COVID-19 pandemic both federal and state governments have loosened restrictions on privacy and billing for telehealth visits in an effort to allow health care providers to continue to care for patients while reducing potential exposure to the virus. 23 24 In particular, the announcement by the Office of Civil Rights at the Department of Health and Human Services means that health care providers may provide care over the telephone or popular consumer grade video chat technology that may not comply with the Health Insurance Portability and Accountability Act (HIPAA) rules without fear of penalty, so long as it is done in good faith to provide necessary care.
The role of telehealth in responding to epidemics and pandemics has been described previously 25 26 27 and health systems around the country have expanded use of telehealth in response to COVID-19 for outpatients, emergency departments, and intensive care units. 28 29 30 Prior to the COVID-19 pandemic our hospital had an established telehealth program for second opinions, select outpatient subspecialty visits, and limited interhospital consultations. Recognizing the need to limit COVID-19 exposure and transmission, 31 we implemented an intrahospital inpatient telehealth (ITH) program with the goals of limiting clinician face-to-face time in the room with patients and to minimize use of PPE.
Objectives
Evaluate the rapid development and implementation of an intrahospital ITH program in response to the COVID-19 pandemic.
Methods
We convened a group of physicians and nursing clinical informatics experts along with information systems specialists to develop, implement, and support an ITH program at Boston Children's Hospital, a 404-bed quaternary care facility in Boston, Massachusetts, United States. We utilized an existing videoconferencing software system (Zoom) used for hospital operations, which was available to nurses, physicians, advanced practice clinicians, and other clinical staff on hospital-provided smartphones. The software was also available on hospital computer workstations and could be downloaded to clinician personal devices if desired. We communicated with our biocontainment and infection control teams to ensure the agreed upon process would be consistent with their best practices. We utilized vendor software to track the number of ITH sessions hosted. Data from our enterprise data warehouse was used to track hospital bedded days. We solicited informal feedback via electronic mail from a convenience sample of eight early adopters including fellows and attending physicians from multiple specialties.
The ITH project team convened initially on March 18, 2020 via videoconference and met remotely multiple times over the subsequent days to design and implement the system. We tested the system with a patient family and bedside nurse on March 19 to compare various hospital and personal devices, assess the audio and video quality, and to ensure the process was intuitive for users. Based on user feedback, we developed educational materials and launched the program on March 21, less than a week after our initial meeting. At the time of this publication data were available for telehealth sessions from March 23 through May 10, 2020.
While any hospital employee could use our videoconferencing system to initiate a meeting using their personal login, our working group sought a unified solution for ITH meetings that would limit the need for staff, patients, and families to exchange meeting information in person, via email, or by phone. We initially developed a central process where an information services department technician created a unique link for each of the 10 available hospital tablets. We provided the tablet and meeting link to the biocontainment team when a patient with suspected or confirmed COVID-19 was admitted. A unique, patient-specific password was created by a clinical informatics specialist and provided to the family and clinical team so that when the patient was discharged the meeting link could remain the same, but the password could be updated. This ensured that patients who were discharged or transferred to a different bed space could not call back into the existing meeting when another patient had taken their place and also prevented patients from utilizing the videoconferencing software for their personal use after discharge. The tablet was then cleaned and prepared for the next patient.
In an effort to maximize the impact of our intervention, we rapidly transitioned to a bring-your-own-device (BYOD) model for patients and families. This allowed us to scale the program quickly and also to minimize the risk of contaminated devices being shared across patients. With this transition, we also needed to create additional meeting links. For simplicity, we opted to create a unique meeting link for each hospital bed space that would be easily remembered by clinicians ( Table 1 ). We continued to make hospital tablets available for patients who did not have a device that would support the videoconferencing software, ultimately deploying multiple devices to each inpatient unit. The anesthesia program also requested meeting link assignments for each operating room to facilitate anesthesia and surgical consultations during surgical procedures. A select number of tablets were implemented for use in other areas as well, such as the emergency department and infusion center.
Table 1. Sample meeting link assignments.
| Unit | Bed | Bed space | Meeting link |
|---|---|---|---|
| 13 North | 1301 | A | Meet1301A |
| 13 North | 1301 | B | Meet1301B |
| 13 North | 1302 | A | Meet1302A |
| 13 North | 1302 | B | Meet1302B |
| 13 North | 1303 | A | Meet1303A |
| 13 North | 1303 | B | Meet1303B |
Note: Meeting links are examples and do not represent actual meeting links used for patients.
We continued the process of clinical informatics specialists updating the meeting password for each bed space whenever a new patient was admitted or changed bed spaces. The meeting link was posted in each patient's room and on the outside of the door, and the password was provided on the dry-erase board in the room. Patient experience representatives on each unit were utilized by patients, families, and clinicians to request an ITH session. Fig. 1 shows the workflow for on- and off-boarding patients and families with the ITH process. Based on anecdotal feedback of patients and families having difficulty onboarding and joining meetings, we utilized available members of the patient experience team working remotely to contact families the morning after admission to support first time setup. Additionally, we created quick response codes for each bed space-specific meeting link to help clinicians, patients, and families join the telehealth meetings without having to input the meeting link manually. Table 2 summarizes the people, process, and technology required for ITH implementation.
Fig. 1.
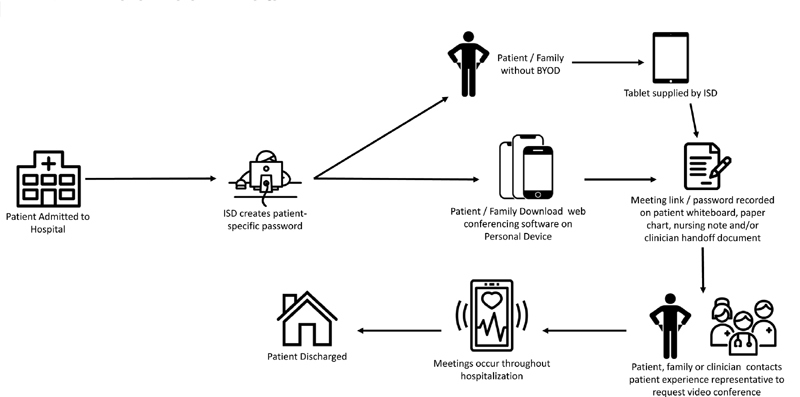
Inpatient telehealth workflow to assign unique meeting link and password to patients based on their hospital bed space. Once provided this link and password allow patients, families, and clinicians to communicate throughout the hospitalization.
Table 2. People, process, and technology requirements for inpatient telehealth.
| People | Process | Technology |
|---|---|---|
| Multidisciplinary group (technical, IT security, admin, clinicians) | Onboarding new clinicians, services, and locations | Vendor for videoconferencing |
| Local champions | Updating passwords with each bed transfer to maintain security | Ability to have a continuous videoconference meeting open at all times |
| Support for hospital devices and BYOD users | Creating and disseminating training materials for staff | Ability to join a videoconference without logging into vendor software |
| Support staff for clinicians | Creating bed space-specific meeting links | Ability to set a meeting link with a “vanity” name |
| Support staff for families | Creating and disseminating training materials for patients and families | Ability to set and update a password for each meeting |
| Generating QR codes | Devices for clinicians including camera and QR code scanning capabilities | |
| Reporting | Devices on inpatient units for patient's without BYOD including camera and QR code scanning capabilities |
Abbreviations: BYOD, bring-your-own-device; IT, information technology; QR, quick response.
Results
From March 23 through May 10, 2020, there were 12,993 bedded patient days including 471 bedded days for patients on COVID-19 precautions (either COVID-19 positive or person under investigation). We hosted 1,820 ITH sessions, including 1,727 on medical, surgical, or critical care units (13.3 sessions per 100 bedded days). Fig. 2 shows the total number of ITH visits over time, stratified by hospital unit type. ITH was used most frequently for patients on medical units. We logged 104,647 minutes of ITH time with a median session duration of 22 minutes (range 1–1,961). There were 5,288 participant devices used with a mean of 3 devices per telehealth session (range 2–22). Table 3 summarizes comments from clinicians.
Fig. 2.
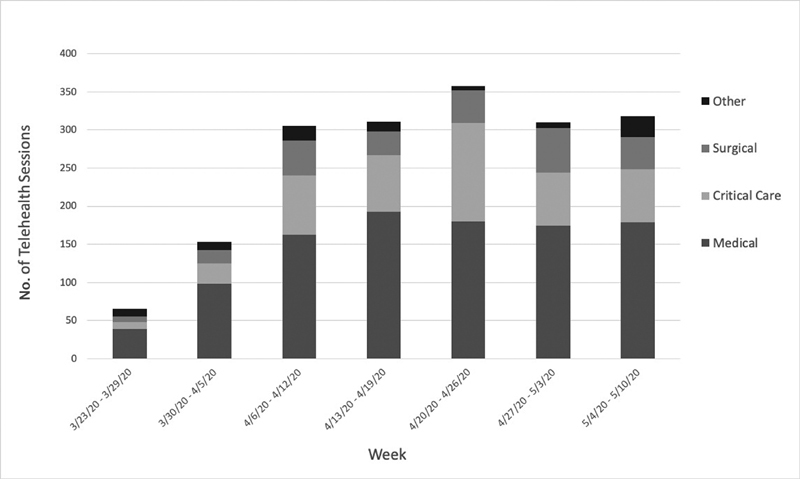
Graph of inpatient telehealth visits over time, stratified by hospital unit type.
Table 3. Feedback about inpatient telehealth provided by clinicians.
| Positive feedback | Negative feedback |
|---|---|
| “It was seamless”-Pediatric hospitalist | “Couldn't figure out how to turn audio on.” -Pediatric hospitalist |
| “Parent used her own device...and already had [the video conferencing app] installed for work.”-Pediatric hospitalist | “At admission, the automatic [meeting links] didn't seem to be set up so I had to create my own.” -Pediatric hospitalist |
| “I was able to get a pretty good history and fairly decent physical and develop good rapport.”-Pediatric hospitalist | “The hospital-assigned [meeting links] didn't work so I set up a personal [meeting identification] and added a password.” -Pediatric hospitalist |
| “Using the families own smartphone...was much easier. I could see/hear better [than using hospital device].”-Pediatric hospitalist | “It was hard to get a good skin exam on [the video conferencing software] but I could tell the skin looked generally more eczematous and that the patient was well appearing and nontoxic.” |
| “Parents very willing to help with exam, including cap refill, ROM testing, etc.” -Pediatric Hospitalist | “[The residents] seemed hesitant to use their own device [in the room].” -Pediatric hospitalist |
| “I think I established great rapport with both families, both of whom had already had telemedicine visit with their PCP btw.” -Pediatric hospitalist | “I didn't ask the nurse to do as many exam maneuvers for me because I sensed she was trying to maintain a distance and I wanted to minimize her exposure.” -Pediatric hospitalist |
| “I think overall it worked quite well. We had really good success with getting the families to download [the app] to their phones and no major technological issues.” -Pediatric gastroenterology fellow | “The main issue is getting [inpatient telehealth] appointments set up is that patients who are NOT under precautions are not consistently trained/set up to use [telehealth] (and challenge to do so during busy rounds/day). For patients in precautions, there appears to be more consistent attention to have them set up [on the video conferencing app]” -Pediatric endocrinologist |
| “I think it is an amazingly important technology for social distancing.” -Pediatric gastroenterologist | “This could be streamlined by helping family's download the app on admission.” -Pediatric endocrinology fellow |
| “My sense was that the families liked it or at least didn't seem to have any big problem with it” -Pediatric gastroenterology fellow | “I was told that the [tablets] were only available for patients on precautions/COVID rule outs. I also felt that nurses seemed surprised that we would even want/need to do a virtual visit for a patient who wasn't on precautions.” -Pediatric endocrinology fellow |
| “Thanks again for the outstanding job of deploying the capabilities of [video conferencing software] for the OR” -Pediatric anesthesiologist | |
| “As typically happens, great success brings new visions and with it more possibilities” -Pediatric anesthesiologist | |
| “We had a very successful [telehealth] visit using the family's personal device and [the assigned meeting link and password].” -Pediatric endocrinology fellow |
Abbreviations: PCP, primary care physician; ROM, range of motion.
Use cases identified for providing ITH visits included (1) telerounding for primary inpatient teams, (2) brief updates on laboratory/test results, (3) teleconsultation for subspecialists, (4) consultation with nutrition, pharmacy, child life services, and other nonphysician providers, (5) team/family meetings, (6) continuous video monitoring of patient for parents quarantined at home, (7) education classroom training, such as for asthma and diabetes care, and (8) operating room consultation with offsite providers. In addition to communicating with the family, providers noted how helpful it was to do visual portions of the exam via telehealth to reduce contact time while in the room. In particular, providers were able to examine patients' general appearance, skin findings, indwelling lines/tubes/drains, and even urine and stool appearance.
Discussion
We rapidly designed and implemented an ITH program in preparation for the COVID-19 pandemic using existing videoconferencing software. In just a few days we scaled the program to support any patient in the hospital and any clinician with access to a hospital device or computer, while providing a consistent workflow to facilitate use for patients, families, and clinicians with minimal training.
Unlike other telehealth programs, this initiative was not meant to overcome the distance between providers and patients but rather to help create distance between patients, families, and staff within the hospital during an unprecedented global pandemic. Notably, while only a small percentage of our patients required COVID-19 precautions, our ITH system was used broadly with clinicians logging over 70 days of telecommunication time over a 7-week period. This likely reflects the efforts of staff to promote physical distancing with all patients as well as with other hospital staff and is particularly important given reports of asymptomatic carriers. 32 33 34 Undiagnosed employees could pose a greater threat to COVID-19 spread within the hospital than infected patients on strict precautions. Additional use-cases also emerged, such as in the intensive care unit where some ITH sessions were left open for 24 hours a day so quarantined parents at home could remain virtually at the bedside with their critically ill child.
While one of our goals was to preserve PPE, we were unable to directly measure PPE use. Rapidly evolving PPE guidelines made it hard to know what protective equipment may have been used on a given day. One could conjecture that each telehealth session saved a set of PPE for each clinician involved; however, we also know that some telehealth sessions still required a follow-up in person exam (e.g., for auscultation of the heart and lungs). In addition, we only counted telehealth sessions logged using the bed space-specific meeting links and not when users independently set up a new meeting identification (either because of challenges with the provided workflow or because they found it easier) so we likely underestimate the total number of sessions.
Prior studies have demonstrated that with encouragement from clinical professionals, patients can have a positive experience using mobile health applications. 35 For this implementation, the BYOD self-service approach was critical to allow us to scale the intervention across our enterprise. Feedback from clinicians and families was largely positive. Clinicians noted the ease of the system and how it enabled them to drastically reduce the amount of time spent in the room with the patient per day by engaging the family in conversation over telehealth and performing some portions of the physical exam remotely. Moreover, we quickly identified additional use cases and received requests from various departments to expand. Anecdotally, providers commented that patients and families also found the system relatively easy to use and appreciated minimizing contact with health care providers during a frightening time.
Challenges encountered when implementing this ITH program included limited availability of support staff in the hospital due to hospital and state social distancing mandates, communication between patients and providers regarding setting up the telehealth visits, as well as disruption of normal rounding and communication practices. Initial setup was especially challenging during off hours when clinicians tended to rely on each other for guidance on how to establish a telehealth session as opposed to reaching out to the help desk. Prior to engaging the patient experience representatives, clinicians did not have a good way to initiate a telehealth session with the patient or family. Workflow challenges highlight the importance of clear and concise training materials, 24/7 support, and role clarity.
There were instances where physician teams or attending providers asked nurses or trainees to help initiate a telehealth session. This led to dissatisfaction, particularly when providers in the room were asked to lend their own hospital-provided or personal devices to the family. Understandably, frontline clinicians may feel apprehensive when asked to prolong their own contact time with a potentially infectious patient to help other clinicians work remotely. They also were appropriately hesitant to bring devices into the patient room to support telehealth encounters, due to concerns for contamination. This underscores the importance of the BYOD self-service model, streamlined workflows, as well as training and support materials that allow patients and families to participate in telehealth sessions seamlessly.
The rapid implementation and adoption of our ITH system was fostered by regulatory changes due to the emergent nature of the COVID-19 pandemic, so it remains unclear how the program may evolve over time. Specifically, the loosening of HIPAA restrictions allowed us to quickly utilize a videoconferencing vendor not initially designed as a stand-alone solution for telehealth. Likewise, parity for billing inpatient evaluation and management codes via telehealth allowed entire teams of providers to work remotely and still generate revenue for their service (e.g., pediatric endocrinology consultations). There appears to be a clear role for intrahospital ITH to facilitate communication between patients, families, and health care provider that will undoubtedly persist beyond the current pandemic 36 ; however, further study is needed to better understand the benefits and potential unintended consequences. Ultimately, if regulatory rules around telehealth return to their pre-COVID-19 state after the pandemic it may be hard to sustain such programs.
Overall, our ITH program was well received by end users and lessons learned during this crisis may help health systems respond more rapidly to future outbreaks and overcome implementation challenges. Our next steps include formal surveys to solicit provider and patient satisfaction, improving access to telehealth sessions, and further evaluating usage patterns to disseminate best practices.
Conclusion
We rapidly implemented and scaled an ITH solution using existing videoconferencing software and encouraging a BYOD self-service model for patients and families. Initial impressions suggest this system is useful for providing care to patients at our hospital during the COVID-19 pandemic; however, further work is needed to improve onboarding and coordination of telehealth sessions. More permanent regulatory reform will help ensure programs like this can continue beyond the nationwide public health emergency.
Clinical Relevance Statement
This quality improvement effort demonstrates how established tools such as telehealth can be rapidly adapted in response to a crisis to support patient care.
Multiple Choice Questions
-
Despite its ability improve access to physicians and specialists, what has historically been a major contributing factor to the limited adoption of inpatient telehealth?
Lack of standardized reimbursement model.
Slow internet bandwidth at many institutions.
High cost of device deployment.
Shortage of health care providers able to use advanced technology.
Correct Answer: The correct answer is option a. In both the inpatient and outpatient setting, lack of a standardized payment model has limited widespread acceptance of telehealth initiatives. Previously, reimbursement for telehealth was limited to rural areas or specific situations, such as telestroke. With the state of emergency introduced by the COVID-19 pandemic, insurers have relaxed payment restrictions, leading to further adoption of telehealth.
-
In response to the COVID-19 pandemic, the Office for Civil Rights (OCR) at the Department of Health and Human Services (HHS) loosened which regulations with the intention to accelerate the adoption of telehealth?
HIPAA Privacy, Security, and Breach Notification Rules (the HIPAA Rules).
Human Subjects Research Protections.
The Health Information Technology for Economic and Clinical Health (HITECH Act).
Freedom of Information Act.
Correct Answer: The correct answer is option a. On March 17, 2020 during the national state of emergency brought forth by the COVID-19 pandemic, the OCR of HHS announced that it would waive potential penalties for HIPAA violations associated with the use of consumer-grade technologies used for virtual patient care. This announcement encouraged remote video communication products such as FaceTime or Skype be used to encourage social distancing, while providing health care during the pandemic. With this directive, institutions were able to quickly scale telehealth offerings to meet many patient care needs during the time of crisis.
Acknowledgments
The authors would like to acknowledge Mark Hourigan, Manager for Network Services at Boston Children's Hospital, for his work configuring the videoconferencing software. We would also like to acknowledge all the front-line providers at Boston Children's Hospital who work tirelessly each day to keep our patients safe.
Funding Statement
Funding None.
Conflict of Interest None declared.
Protection of Human and Animal Subjects
This project was deemed quality improvement by the Boston Children's Hospital Department of Pediatrics Performance Excellence Group. Quality improvement projects that are designed to improve clinical care to better conform to established or accepted standards are considered exempt by our institutional review board.
References
- 1.Zhu N, Zhang D, Wang W et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(08):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Novel Coronavirus (2019-NCoV) SITUATION REPORT - 1 2020. Available at:https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf?sfvrsn=20a99c10_4. Accessed March 30, 2020
- 3.Novel Coronavirus (2019-NCoV) SITUATION REPORT - 51 2020. Available at:https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10. Accessed June 2, 2020
- 4.Markel H, Lipman H B, Navarro J A et al. Nonpharmaceutical interventions implemented by US cities during the 1918-1919 influenza pandemic. JAMA. 2007;298(06):644–654. doi: 10.1001/jama.298.6.644. [DOI] [PubMed] [Google Scholar]
- 5.Rashid H, Ridda I, King C et al. Evidence compendium and advice on social distancing and other related measures for response to an influenza pandemic. Paediatr Respir Rev. 2015;16(02):119–126. doi: 10.1016/j.prrv.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Livingston E, Desai A, Berkwits M.Sourcing personal protective equipment during the COVID-19 pandemic JAMA 2020E1–E3.. Doi: 10.1001/jama.2020.5317 [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization.Rational use of personal protective equipment for coronavirus disease (COVID-19): interim guidance, 27 February 2020 World Health Organization; 2020 [Google Scholar]
- 8.Brown E M. The Ontario Telemedicine Network: a case report. Telemed e-Health. 2013;19(05):373–376. doi: 10.1089/tmj.2012.0299. [DOI] [PubMed] [Google Scholar]
- 9.Kim E W, Teague-Ross T J, Greenfield W W, Keith Williams D, Kuo D, Hall R W. Telemedicine collaboration improves perinatal regionalization and lowers statewide infant mortality. J Perinatol. 2013;33(09):725–730. doi: 10.1038/jp.2013.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robison J, Slamon N BA. A more rapid, rapid response. Pediatr Crit Care Med. 2016;17(09):871–875. doi: 10.1097/PCC.0000000000000855. [DOI] [PubMed] [Google Scholar]
- 11.Georgesen C, Karim S A, Liu R, Moorhead A, Falo L D, English J C.Inpatient eDermatology (teledermatology) can help meet the demand for inpatient skin diseaseTelemed e-Health 2019:tmj.2019.0147. Doi: 10.1089/tmj.2019.0147 [DOI] [PubMed]
- 12.Okita A L, Molina Tinoco L J, Patatas O HG et al. Use of smartphones in telemedicine: comparative study between standard and teledermatological evaluation of high-complex care hospital inpatients. Telemed e-Health. 2016;22(09):755–760. doi: 10.1089/tmj.2015.0086. [DOI] [PubMed] [Google Scholar]
- 13.Coombes C E, Gregory M E. The current and future use of telemedicine in infectious diseases practice. Curr Infect Dis Rep. 2019;21(11):41. doi: 10.1007/s11908-019-0697-2. [DOI] [PubMed] [Google Scholar]
- 14.Young J D, Abdel-Massih R, Herchline T et al. Infectious Diseases Society of America position statement on telehealth and telemedicine as applied to the practice of infectious diseases. Clin Infect Dis. 2019;68(09):1437–1443. doi: 10.1093/cid/ciy907. [DOI] [PubMed] [Google Scholar]
- 15.Assimacopoulos A, Alam R, Arbo M et al. A brief retrospective review of medical records comparing outcomes for inpatients treated via telehealth versus in-person protocols: is telehealth equally effective as in-person visits for treating neutropenic fever, bacterial pneumonia, and infected bacterial wounds? Telemed e-Health. 2008;14(08):762–768. doi: 10.1089/tmj.2007.0128. [DOI] [PubMed] [Google Scholar]
- 16.Shively N R, Moffa M A, Paul K Tet al. Impact of a telehealth-based antimicrobial stewardship program in a community hospital health system Clin Infect Dis 2019ciz878. Doi: 10.1093/cid/ciz878 [DOI] [PubMed] [Google Scholar]
- 17.DeVido J, Glezer A, Branagan L, Lau A, Bourgeois J A. Telepsychiatry for inpatient consultations at a separate campus of an academic medical center. Telemed e-Health. 2016;22(07):572–576. doi: 10.1089/tmj.2015.0125. [DOI] [PubMed] [Google Scholar]
- 18.Dorsey E R, Topol E J. State of telehealth. N Engl J Med. 2016;375(02):154–161. doi: 10.1056/NEJMra1601705. [DOI] [PubMed] [Google Scholar]
- 19.Gray J E, Safran C, Davis R B et al. Baby CareLink: using the internet and telemedicine to improve care for high-risk infants. Pediatrics. 2000;106(06):1318–1324. doi: 10.1542/peds.106.6.1318. [DOI] [PubMed] [Google Scholar]
- 20.O'Connor M, Asdornwised U, Dempsey M L et al. Using telehealth to reduce all-cause 30-day hospital readmissions among heart failure patients receiving skilled home health services. Appl Clin Inform. 2016;7(02):238–247. doi: 10.4338/ACI-2015-11-SOA-0157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Negarandeh R, Zolfaghari M, Bashi N, Kiarsi M. Evaluating the effect of monitoring through telephone (tele-monitoring) on self-care behaviors and readmission of patients with heart failure after discharge. Appl Clin Inform. 2019;10(02):261–268. doi: 10.1055/s-0039-1685167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang T. Health Policy Brief: Telehealth Parity Laws. Health Affairs, August 15, 2016. Doi: 10.1377/hpb2016.12
- 23.Notification of Enforcement Discretion for Telehealth 2020. Available at:https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html. Accessed March 26, 2020
- 24.Order Expanding Access to Telehealth Services and to Protect Health Care Providers Boston: Office of the Governor, Commonwealth of Massachusetts; 2020. Available at:https://www.mass.gov/doc/march-15-2020-telehealth-order/download. Accessed April 1, 2020 [Google Scholar]
- 25.Keshvardoost S, Bahaadinbeigy K, Fatehi F.Role of telehealth in the management of COVID-19: lessons learned from previous SARS, MERS, and Ebola outbreaksTelemed e-Health April 2020:tmj.2020.0105. Doi: 10.1089/tmj.2020.0105 [DOI] [PubMed]
- 26.Chiappelli F, Bakhordarian A, Thames A D et al. Ebola: translational science considerations. J Transl Med. 2015;13(01):11. doi: 10.1186/s12967-014-0362-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosen J M, Kun L, Mosher R E et al. Cybercare 2.0: meeting the challenge of the global burden of disease in 2030. Health Technol (Berl) 2016;6(01):35–51. doi: 10.1007/s12553-016-0132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reeves J J, Hollandsworth H M, Torriani F J et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inf Assoc. 2020 doi: 10.1093/jamia/ocaa037/5811358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Turer R W, Jones I, Rosenbloom S T, Slovis C, Ward M J. Electronic personal protective equipment: a strategy to protect emergency department providers in the age of COVID-19. J Am Med Inf Assoc. 2020 doi: 10.1093/jamia/ocaa048/5815267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grange E S, Neil E J, Stoffel M et al. Responding to COVID-19: the UW medicine information technology services experience. Appl Clin Inform. 2020;11(02):265–275. doi: 10.1055/s-0040-1709715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aroroa V M, Chivu M, Schram A, Meltzer D. Implementing physical distancing in the hospital: a key strategy to prevent nosocomial transmission of COVID-19. J Hosp Med. 2020;15(05):290–291. doi: 10.12788/jhm.3434. [DOI] [PubMed] [Google Scholar]
- 32.Chan J FW, Yuan S, Kok K Het al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster Lancet 2020395(10223):514–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu Z, Song C, Xu C et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020;63(05):706–711. doi: 10.1007/s11427-020-1661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bai Y, Yao L, Wei T et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323(14):1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Farzandipour M, Nabovati E, Heidarzadeh Arani M, Akbari H, Sharif R, Anvari S. Enhancing asthma patients' self-management through smartphone-based application: design, usability evaluation, and educational intervention. Appl Clin Inform. 2019;10(05):870–878. doi: 10.1055/s-0039-1700866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dyrda L.“The genie's out of the bottle on this one”: Seema Verma hints at the future of telehealth for CMS beneficiaries. Becker's Hospital ReviewPublished 2020. Available at:https://www.beckershospitalreview.com/telehealth/the-genie-s-out-of-the-bottle-on-this-one-seema-verma-hints-at-the-future-of-telehealth-for-cms-beneficiaries.html. Accessed May 6, 2020


