Abstract
Background
The primary aim of this review was to establish whether health literacy interventions, in adults, are effective for improving health literacy. Two secondary aims assessed the impact of health literacy interventions on health behaviours and whether health literacy interventions have been conducted in cardiovascular patients.
Methods
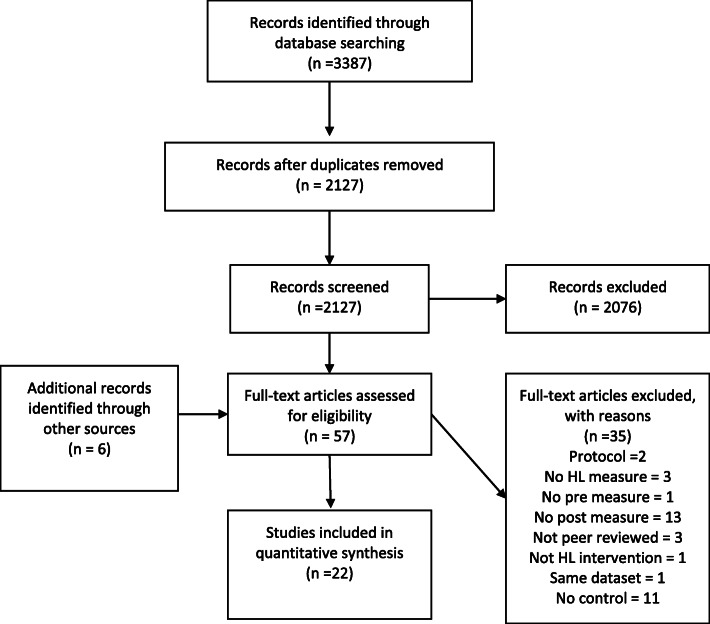
A systematic review (Prospero registration: CRD42018110772) with no start date running through until April 2020. Eligible studies were conducted in adults and included a pre/post measure of health literacy. Medline, Embase, Eric, PsychINFO, CINAHL, Psychology and Behavioural Science, HMIC, Web of Science, Scopus, Social Care Online, NHS Scotland Journals, Social Policy and Practice, and Global Health were searched. Two thousand one hundred twenty-seven papers were assessed, and 57 full text papers screened to give 22 unique datasets from 23 papers. Risk of bias was assessed regarding randomisation, allocation sequence concealment, blinding, incomplete outcome data, selective outcome reporting and other biases. Intervention reporting quality was assessed using the TIDieR checklist.
Results
Twenty-two studies were included reporting on 10,997 participants in nine countries. The majority of studies (14/22) were published in 2018 or later. Eight studies (n = 1268 participants) also reported on behavioural outcomes. Health literacy interventions resulted in improvements in at least some aspect of health literacy in 15/22 studies (n = 10,180 participants) and improved behavioural outcomes in 7/8 studies (n = 1209 participants). Only two studies were conducted with cardiovascular patients. All studies were at risk of bias with 18 judged as high risk. In addition, there was poor reporting of intervention content with little explication of the theoretical basis for the interventions.
Conclusions
Health literacy interventions can improve health literacy and can also lead to changes in health behaviours. Health literacy interventions offer a way to improve outcomes for populations most at risk of health inequalities. Health literacy is a developing field with very few interventions using clear theoretical frameworks. Closer links between health literacy and behaviour change theories and frameworks could result in higher quality and more effective interventions.
Prospero registration
Prospero registration: CRD42018110772
Keywords: Health literacy, Behaviour change, Cardiovascular disease, Systematic review, Interventions
Background
Health literacy as a concept first emerged in the 1970’s [1] and the definition further refined in 2000 by Nutbeam [2] who added interactive health literacy and critical health literacy to the existing focus on functional health literacy. These three aspects have endured throughout the subsequent developments of health literacy and are conceptualised as representing different levels of skills and understanding that move progressively towards greater autonomy and empowerment. They start from a base of functional health literacy (basic ability to read and understand health information [2, 3]) through interactive health literacy (more advanced cognitive and social skills that demonstrate greater engagement with a wider variety of health information, improved self-efficacy, and decision making [2–6]) and finally critical health literacy (higher order cognitive and critical decision making skills, alongside social, political and organisational level actions to improve wider determinants of health [2–7]).
In 2012 the European Health Literacy Consortium [6] conducted a major review of the literature and developed a new definition of health literacy - “Health literacy is linked to literacy and entails people’s knowledge, motivation and competences to access, understand, appraise, and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life during the life course.” (Pg.3). Applying this definition suggests that health literacy pervades patient’s encounters with healthcare services at every level. For a while the focus was on health literacy as a skill or asset that the patient was required to improve [8]. More recently there has been a recognition of the responsibility that healthcare services have to ensure they are providing information in a way that patients can understand [9].
Health literacy and cardiovascular disease
The European health survey found that almost half of adults in eight countries had inadequate or problematic health literacy [10]. Weak health literacy competencies can result in increased rates of hospital readmission, low health related quality of life (HRQOL), higher anxiety levels and lower social support [11], less healthy choices, and poorer self-reported health status [12]. Health literacy is also a key predictor of self-assessed health second only to age [13].
Other studies have shown that patients with chronic conditions have lower levels of health literacy, and amongst this sector, cardiovascular patients have the highest number of problems understanding health information [14, 15]. Given this limitation, it is possible that interventions to improve health literacy may be important to support and facilitate subsequent behaviour change.
Cardiovascular diseases are the leading cause of mortality worldwide, responsible for 31% of deaths in 2015 [16]. Cardiovascular diseases are predominantly the result of lifestyle behavioural factors such as poor diet, inadequate physical activity, smoking or harmful alcohol consumption. Other physiological factors include high blood pressure, high cholesterol, high blood sugar or glucose. Both the physiological and the behavioural factors are linked with socio-economic and societal drivers such as ageing, income, location, education and housing [17].
Following a cardiac diagnosis there is a need for patients to learn to self-manage their condition, and for many a change in lifestyle could reduce the risk of further cardiovascular events. This can be supported through a course of cardiac rehabilitation offered through the national health service (NHS), though uptake is low [18]. Whilst there are many reasons why this may be the case [19–22], some of it may be due to inadequate levels of health literacy.
There has been a significant increase in the amount of research conducted into health literacy in recent years, including a much higher proportion with a European focus, however, much of this has been focused on identifying definitions, prevalence and associations [23]. Less research has been conducted into possible interventions for health literacy – in any health condition, and particularly within cardiac populations [24].
Limitations with previous reviews
From a pool of 96 reviews in the field of health literacy none focused specifically on health literacy interventions in cardiac patients. Four reviews focused on health literacy in cardiac populations [25–28] and covered aspects such as prevalence, adherence to medication and measurement tools. Whilst some of these did include interventions, none required pre-post measures as an inclusion criterion. To be certain that a specified intervention has made a change to the outcome of interest (in this case health literacy) measuring before and after the intervention is an essential requirement. Including a control condition, increases the likelihood that outcomes are a result of the intervention content, rather than the contact the intervention brought. Both of these requirements are missing in all reviews identified by the search team.
Aim
Many chronic or long-term health conditions such as cardiovascular disease, benefit from behavioural changes to support lifestyle modification. Improving health literacy skills is believed to result in patients being better able to manage lifestyles, seek information and have the confidence to apply it. As a consequence, improved health literacy may result in improved behavioural outcomes such as smoking cessation, increased physical activity, improved diet quality, successful weight management and reduced alcohol consumption.
The primary aim of this review is to establish whether controlled health literacy interventions, in adults, are effective for improving health literacy. Two secondary aims, using the studies identified for the primary aim, are to explore whether 1) health literacy interventions lead to a change in health behaviours and 2) which of the eligible studies were conducted with cardiovascular patients and examine the outcomes in this population.
Methods
The protocol was registered with PROSPERO (registration number: CRD42018110772).
Eligibility criteria
Inclusions
Eligible papers included any full text articles published in peer reviewed journals with adults (aged 18 or over) as the subject of the intervention (as opposed to parents/caregivers). Searches were restricted to English language only due to the capacity of the review team to translate or work with other language texts. Eligible interventions included any intervention evaluated in a controlled trial that included a pre-post measure of health literacy. Eligible control conditions include any usual care or alternative approach to the intervention. Primary outcomes were self-reported or objectively measured health literacy measured at baseline and post-intervention (either directly after intervention completion or at follow up, regardless of the duration). Secondary outcomes of interest for this study are changes in behavioural outcomes such as health screening, smoking, nutrition, alcohol or physical activity behaviours. In common with Nutbeam et al. (2018) we excluded mental health literacy interventions as the field is conceptually distinct from health literacy.
Exclusions
Papers were excluded if they were not available in English to allow the review team to effectively review them, if they did not report full peer reviewed results of an intervention (for example abstracts, unpublished studies, protocols), or if they did not report both pre and post measures of health literacy. It is worth noting that many of the excluded papers were either observational/correlational studies, or they only used health literacy to segment the intervention population, or the intervention was designed to improve health literacy but they did not measure health literacy as an outcome of interest. None of these studies were eligible for this review.
Information sources
Searches were conducted on electronic databases with no start date restriction through to 10th April 2020. The following databases were searched: Medline, Embase, Eric, PsychINFO, CINAHL, Psychology and Behavioural Science, HMIC, Web of Science, Scopus, Social Care Online, NHS Scotland Journals, Social Policy and Practice, Global Health. Full search strategies for each database can be found in additional file 1. In addition, the references of the papers included in the systematic review were searched, along with several published systematic reviews in related areas to make sure no relevant articles were missed.
Search strategy
Initial scoping searches to develop the search strategy included cardiology specific terms. The search strategy was then broadened and the results backchecked to ensure the strategy was still retrieving the cardiology related materials. Searches included a combination of terms from MESH headings and keywords in the title and abstract. The search included multiple terms for health literacy (e.g. health literacy, functional health literacy), intervention (e.g. intervention, pre-post, trial) and health literacy measurements (e.g. health literacy screen, health literacy measurement, REALM, TOFHLA). All terms within each category were combined with “OR” and then the three categories were combined with “AND”. The search strategy was created by RW, TG and RP (an experienced information specialist) and run by RW. Detailed search strategies can be found in supplementary Table 1 (additional file 1).
Study selection
Search results were imported into Endnote X9 reference management software and duplicates were removed. The remaining papers were exported to RAYYAN [29] (a systematic review web application) and titles and abstracts screened through application of the inclusion/exclusion criteria by RW, with a random 10% screened independently (TG) with 100% concordance. Full texts of potentially relevant studies were screened independently by two reviewers (RW, TG). All included texts had the references hand searched to check for additional eligible papers.
Data extraction
All data from included studies were extracted into Word independently by two reviewers (RW, TG). Details extracted included study details, (design, population), health literacy details (definition, measure of health literacy used, aspects of health literacy measured), intervention details (intervention content, contact time, aspect of health literacy targeted in the intervention) and outcomes (health literacy and secondary behavioural outcomes).
Data analysis
All papers were assessed using the template for intervention description and replication (TIDieR) independently by RW and TG with 84% initial concordance, rising to 100% following discussion. Quality appraisal was conducted independently using risk of bias in non-randomised studies of interventions (ROBINS-1) for non-randomised controlled trials and the appropriate version of risk of bias 2 (RoB 2.0) for individual randomised, cluster randomised and cross-over trials. Earlier versions were adjusted in domain 5 to provide consistency with the questions in the latest version for randomised controlled trial (RCT) studies. Initial inter-rater agreement was 91% for overall risk of bias and 83% for sub-domains. After discussion all differences were resolved with 100% agreement.
Results are presented using a narrative synthesis as the variation in definitions and measurements rendered a meta-analysis unsuitable.
Results
Study characteristics
This systematic review identified 3387 papers. After the removal of duplicates 2127 unique publications were screened and 2076 excluded based on title or abstract because they did not meet the inclusion criteria (see additional file 1 for detailed breakdown). Fifty-seven papers were retrieved for full text assessment, of which 35 failed to meet the inclusion criteria. Twenty-three papers [30–52] exploring 22 data sets (summarised in Table 1) were included in the final review (see Fig. 1). The two papers by Mas et al. [45, 46] were confirmed by the authors to relate to the same data set. Information from both papers was extracted to complete the review, however for clarity the reference for the latest paper will be used [45].
Table 1.
Summary of studies
| Reference, 1st author, year, country | Study design | Population: (Age, ethnic/migrant focus, n (f = %) | Measure [Objective/Subjective] | Health condition | Domain | Intervention content [Total in-person contact timea (where applicable)] |
Secondary Behavioural Outcomes measured |
|---|---|---|---|---|---|---|---|
| Domain | Health Care | ||||||
| [30] Calderon, 2014 USA | RCT |
Adults, Latino/Hispanic 240 (f = 81.66) |
Diabetes Health Literacy Scale [Subjective] | Diabetes | Health care |
13-min animation [n/a] |
None |
| [31] Tai, 2016 USA | RCT |
> 55 None 118 (f = 62.71) |
STOFHLA [Objective] | Taking 2 or more medications | Health care |
A single one-to-one 10-min education session plus leaflets and sample labels for self-assessment [10 min] |
None |
| [32] Gharachourlo, 2018 Iran | RCT |
18–35, None, 100 (f = 100) |
Iranian Health Literacy Questionnaire [Subjective] | Gestational diabetes | Health care |
Counselling with a health literacy approach (6 X 1.5 h weekly sessions) [540 min] |
Health lifestyle behaviours |
| [33] Knudsen, 2019 Denmark | Quasi-experimental |
Adults, None, 77 (f = 9) |
HLQ [Subjective] |
PCI, CABG, or left heart valve surgery | Health care |
12 weeks of supervised exercise training, dietary advice, educational sessions and psychosocial support [unclear] |
None |
| [34] Tavakoly Sany, 2019 Iran | RCT |
30–75, None, 80 (f = 73.75%) |
TOFHLA [Objective] |
Heart failure | Health care |
Three educational group workshops [200 min] |
Self-care behaviours |
| [35] Banbury, 2020 Australia | Quasi-experimental |
> 50, None 111 (f = 64.86) |
HLQ [Subjective] |
One or more chronic conditions | Health care |
5 facilitative learning video-conference self-management group sessions [337.5 min] |
None |
| [36] Handa, 2020 Japan | RCT |
Adults, None 102 (f = 100) |
HLS-14 [Subjective] |
Breast cancer | Health care |
Smartphone app for self-directed use to record symptoms and manage chemotherapy side-effects [n/a] |
None |
| [37] Kim, 2020 USA | RCT |
> 35, Korean American 209 (f = 40.9) |
REALM, DM-REALM, TOFHLA, NVS [Objective] |
Type 2 Diabetes | Health care |
6 × 2 h weekly education sessions, monthly motivational interviewing counselling sessions and daily self-monitoring of blood glucose levels [1050 minb] |
None |
| Domain | Disease prevention | ||||||
| [38] Li, 2016 Niger | RCT |
Working age adults, Chinese, 1441 (f = 2.98) |
Malaria Health Literacy Questionnaire [Unclear] | Malaria | Disease prevention |
Malaria prevention and treatment messages via WeChat 3xweek for 4 months [n/a] |
None |
| [39] Han, 2017 USA | Cluster RCT |
21–65, Korean American, 560 (f = 100) |
Assessment of health literacy in cancer screening [Objective] | Cancer screening behaviours | Disease prevention |
CHW provided education (Single 1.5–2-h small group session), monthly telephone counselling and navigation assistance over 6 months [155 min] |
Cancer screening |
| Domain | Health promotion | ||||||
| [40] Otilingam 2015, USA | RCT |
> 40, Latino, 100 (f = 100) |
NVS [Objective] | None | Health promotion (nutrition) |
Two 2 h workshops (1 week apart) with culturally relevant nutrition education techniques and 3 behaviour change principles [240 min] |
Nutrition |
| [41] Zhuang, 2016 China | Cluster RCT |
Adults, None 6413 (f = unknown) |
RAHL [Objective] | None | Health promotion (general) |
Health education SMS message once a week for 1 year [n/a] |
None |
| [42] Mas, 2017 USA | Quasi-experimental |
21 or over, Hispanic, 97 (f = 81.44) |
STOFHLA [Objective] | None | Health promotion (general) |
ESL curriculum (180 h) with HL content (5 × 2 h sessions) [600 minc] |
None |
| [43] Parekh, 2017 USA | Pilot RCT |
Adults, None, 59 (f = 100) |
NVS [Objective] | Cancer survivors | Health promotion (nutrition) |
6 Small group nutrition education sessions (2 h duration) delivered fortnightly [720 min] |
Nutrition |
| [44] Liu, 2018 China | Cluster RCT |
60 and above, None, 260 (f = 49.23) |
Chinese Citizen health literacy questionnaire [Unclear] |
None | Health promotion (general) |
Teach back educational classes 40 min long once a month for 6 months [240 min] |
None |
| [45, 46] Mas, 2018 (and 2015) USA | RCT |
Adults, Hispanic, 155 (f = 80.65) |
TOFHLA [Objective] | None | Health promotion (general) |
ESL curriculum with HL content. 12 units over 6 weeks for total of 36 h (6 h sessions) [2160 min] |
Cardiovascular health behaviours |
| [47] Panahi, 2018 Iran | Cluster RCT |
University Students, None, 130 (f = 60) |
Health Literacy in Iranian Adults [Subjective] | Smoking prevention | Health promotion (smoking) |
Six educational sessions via telegram Social media application [n/a] |
Smoking |
| [48] Tsai, 2018 Taiwan | Quasi-experimental |
Adults, Vietnamese/Indonesian 223 (f = 100) |
Bespoke [Subjective] | None | Health promotion (general) |
10 session (2 h per session) every other week, problem-based learning HL program [1200 min] |
None |
| [49] Uemura, 2018 Japan | RCT |
> 65, None 84 (f = 70.23) |
HLS-EU-Q16 and HLS-14 [Subjective] | None | Health promotion (nutrition and physical activity) |
Weekly 90-min active learning program for 24 weeks [2160 min] |
Nutrition and physical activity |
| [50] Fiedler, 2019 Germany | Crossover RCT |
Adults, None 72 (f = 19.44) |
German Health Literacy Questionnaire [Subjective] | None | Health promotion (general) |
5-month training program. Three modules delivered over 3-day classroom training, peer coaching and practice material. [1260 min] |
None |
| [51] McCaffery, 2019 Australia | Cluster RCT |
> 16, None, 213 (f = 70) |
HLQ [Subjective] |
None | Health promotion (general) |
18 week health literacy focused adult education curriculum [6480 min] |
None |
| [52] Smith, 2019 Australia | RCT |
> 55, None, 153 (f = 66.66) |
HLQ [Subjective] |
None | Health promotion (general) |
DVD/web based multi-media education on complementary medicine [n/a] |
None |
aIn-person contact time is calculated through description provided in the original paper. Number of sessions x duration of sessions gives total in-person contact time over the duration of the intervention. If a range is given (e.g. 1.5–2 h) then the midpoint is taken
bThis reflects 720 min of group education sessions and an average of 30 min per counselling session for 11 months
cThis reflects active health literacy content, but was embedded within a wider ESL intervention of 10,800 min
Fig. 1.
PRISMA Flow Diagram
Of the 22 included studies, the earliest study was from 2014 [30], the latest from 2020 [35–37] with the majority (fourteen) being published since 2018 [32–37, 44, 45, 47–52]. Eighteen studies were randomised and included 1 cross over design [50], 5 cluster randomised [39, 41, 44, 47, 51] and 12 individually randomised trials [30–32, 34, 36–38, 40, 43, 45, 49, 52]. The remaining four were quasi-experimental pre-post controlled trials [33, 35, 42, 48]. Studies took place in nine countries –USA [30, 31, 37, 39, 40, 42, 43, 45], Australia [35, 51, 52], Iran [32, 34, 47], China [41, 44], Japan [36, 49], Taiwan [48], Niger [38], Germany [50] and Demark [33].
Two studies focused on the domain of disease prevention (cancer screening [39] and malaria health literacy [38]), eight focused on healthcare (diabetes [30, 37], gestational diabetes [32], breast cancer [36], cardiac conditions [33, 34], one or more chronic conditions [35] and people taking two or more medications daily [31]). The remaining 12 studies focused on health promotion with eight focusing on general health promotion [41, 42, 44, 45, 48, 50–52], two focusing on nutrition [40, 43], one on nutrition and physical activity [49] and one on smoking prevention [47]. Studies are summarised in Table 1.
TIDieR assessment
Reporting was adequate for 58% of the intervention conditions and 57% of the control conditions. Six studies planned to tailor the intervention but only two reported adequately. Only one study modified the delivery of the intervention.
Across the 22 studies only seven reported on planned fidelity checks (reporting was adequate for four of the studies and unclear for the other three). Of these seven only two reported on actual fidelity, with only one being sufficiently clear to be considered adequate. Studies were generally good at providing a descriptive name or phrase (95%), rationale (100%), and details of how (86% for intervention, 69% for control) and frequency and intensity (73% for intervention, 64% for control). Planned fidelity (18%) and actual fidelity (5%) were the most poorly described. It should also be noted that whilst materials were described in 95% of intervention conditions and 69% of control conditions the percentage that were adequately reported was much lower (41% of intervention, 38% of control). See supplementary Tables 2 & 3 (additional files 2 & 3) for TIDieR reporting and percentage summary tables.
Risk of Bias
No studies were rated at a low risk of bias overall, with 18 being at a high or serious risk of bias and just four being rated at some concerns (see supplementary Table 4 (additional file 4)). Studies were generally poorly rated in the randomisation process with only three being at low risk of bias. The majority of studies showed low risk of bias for the deviations from intended intervention (20 studies). Thirteen studies had low risk of bias for measurement of the outcome and 12 studies for missing outcome data domains. No study analysed data in accordance with a pre-published statistical analysis plan (SAP) causing all studies to be rated with some concerns for the risk of selection bias.
Participant characteristics
The studies included 10,997 participants. Six studies focused exclusively on women [32, 36, 39, 40, 43, 48], the remaining 16 included both genders. One study did not provide a gender split [41] but the remaining 15 studies had an average of 55.6% female participants (range 2.98–81.7%).
Eight studies focused on specific ethnic groups or migrants from either Asia (Korea [37, 39], China [38], Vietnam or Indonesia [48]), or Mexico [30, 40, 42, 45]. All participants were adults and most studies covered the whole age spectrum however one study only included people aged 18–35 [32], two specified working age adults [38, 39], and six focused on the later years in life with minimum age of 40 [40], 50 [35], 55 [31, 52], 60 [44] and 65 [49] respectively.
Health literacy definitions and measures
There was considerable variation in how health literacy was defined and measured (see Table 2). Six studies [36, 40, 42, 43, 45, 47] did not provide a definition, two [31, 34] gave a definition but no clear reference to identify it, and the remaining 14 studies referenced 10 different definitions (three studies [30, 35, 48] gave multiple definitions) with Ratzan and Parker [54] used in five studies [30, 35, 37, 39, 51] and Sorensen [6] cited in four studies [33, 48–50].
Table 2.
Definitions and measures
| 1st author, year | Definition | Measure | Subjective /Objective | Culture specific | Condition specific |
|---|---|---|---|---|---|
| [30] Calderon, 2014 | American Medical Association, 1999 [53], Ratzan and Parker, 2000 [54], World HealthOrganisation, 1998 [55] | Diabetes Health Literacy Scale [30] | Subjective | √ | |
| [50] Fiedler, 2019 | Sorensen, 2012 [6] | German Health Literacy Questionnaire [56] | Subjective | √ | |
| [32] Gharachourlo, 2018 | Berkman, 2010 [57] | Iranian Health Literacy Questionnaire [58] | Subjective | √ | |
| [39] Han, 2017 | Ratzan and Parker, 2000 [54] | Assessment of Health Literacy in Cancer Screening [59] | Objective | √ | |
| [44] Liu, 2018 | Mark, 2009 [60] | Chinese Citizen Health Literacy Questionnaire [61] | Subjective | √ | |
| [42] Mas, 2017 | None | STOFHLA [62] | Objective | ||
| [45, 46] Mas, 2018 (and 2015) | None | TOFHLA [63] | Objective | ||
| [38] Li, 2016 | Baker, 2006 [64] | Malaria Health Literacy Questionnaire [38] | Unclear | √ | |
| [40] Otilingam, 2015 | None | NVS [65] | Objective | ||
| [47] Panahi, 2018 | None | Health Literacy for Iranian Adults [66] | Subjective | √ | |
| [43] Parekh, 2017 | None | NVS [65] | Objective | ||
| [31] Tai, 2016 | Unclear | STOFHLA [62] | Objective | ||
| [48] Tsai, 2018 | Kimbrough, 2007 [67], Nutbeam, 2008 [2], Sorensen, 2012 [6] | Bespoke | Subjective | ||
| [49] Uemura, 2018 | Sorensen, 2012 [6] | HLS-EU-Q16 [68] and HLS-14 [69] | Subjective | ||
| [41] Zhuang, 2016 | American Medical Association [53] | Rapid Assessment of Health Literacy [41] | Objective | ||
| [35] Banbury, 2019 | Australian Bureau of statistics, 2006 [70] Berkman et al., 2011 [11] Ratzan and Parker, 2000 [54] | Health Literacy Questionnaire [71] | Subjective | ||
| [36] Handa, 2020 | None | HLS-14 [69] | Subjective | ||
| [37] Kim, 2020 | Ratzan and Parker, 2000 [54] | REALM, DM-REALM, TOFHLA, NVS [37, 63, 65, 72] | Objective | √ (DM-REALM) | |
| [33] Knudsen, 2019 | Sorensen, 2012 [6] | Health Literacy Questionnaire [71] | Subjective | ||
| [51] McCaffery, 2019 | Ratzan and Parker, 2000 [54] | Health Literacy Questionnaire [71] | Subjective | ||
| [34] Tavakoly Sany, 2019 | Unclear | TOFHLA [63] | Objective | ||
| [52] Smith, 2019 | Nutbeam, 2000 [2] | Health Literacy Questionnaire [71] | Subjective |
A variety of health literacy measures were used across the 22 studies. Four studies used condition specific measures [30, 37–39], four used culture specific measures [32, 44, 47, 50], and three created measures for use in the studies [30, 41, 48]. The rest used validated general instruments such as newest vital sign -NVS [37, 40, 43], test of functional health literacy in adults / short test of functional health literacy in adults -TOFHLA/STOFHLA [31, 34, 37, 42, 45], Health Literacy Questionnaire – HLQ [33, 35, 51, 52], HLS-EU-Q16 [49], and HLS14 [49]. Two studies used multiple measures [37, 49].
Studies did not always clearly describe measures used to assess health literacy. Nine studies used clearly objective measures [31, 34, 37, 39–43, 45], 12 used clearly subjective measures [30, 32, 33, 35, 36, 44, 47–52]. In addition one [38] was more difficult to determine and appears to be a mixed measure. The author has not responded to requests for clarification. With regards to the different aspects of health literacy (functional, interactive, critical) as shown in Table 3, all but one [48] measured functional health literacy, nine measured interactive health literacy [32, 33, 35, 36, 48–52] with a further two [38, 47] providing insufficient information to determine, and just six [32, 35, 36, 48, 49, 52] measured critical health literacy, with an additional three being unclear for this aspect [38, 47, 50].
Table 3.
Aspects of Health Literacy covered by measure and intervention content
| Reference, 1st author, year | Measure | Intervention | Measure/Intervention matches | ||||
|---|---|---|---|---|---|---|---|
| Functional | Interactive | Critical | Functional | Interactive | Critical | Insufficient/Matches/Exceeds | |
| [30] Calderon, 2014 | yes | no | no | yes | no | no | matches |
| [50] Fiedler, 2019 | yes | yes | unclear | yes | yes | yes | insufficient |
| [32] Gharachourlo, 2018 | yes | yes | yes | yes | yes | no | exceeds |
| [39] Han, 2017 | yes | no | no | yes | yes | no | insufficient |
| [44] Liu, 2018 | yes | no | no | yes | no | no | matches |
| [42] Mas,2017 | yes | no | no | yes | unclear | no | insufficient |
| [45, 46] Mas, 2018 (and 2015) | yes | no | no | yes | yes | no | insufficient |
| [38] Li, 2016 | yes | unclear | unclear | yes | yes | unclear | insufficient |
| [40] Otilingam, 2015 | yes | no | no | yes | yes | no | insufficient |
| [47] Panahi, 2018 | yes | unclear | unclear | yes | no | no | matches |
| [43] Parekh, 2017 | yes | no | no | yes | yes | no | insufficient |
| [31] Tai, 2016 | yes | no | no | yes | no | no | matches |
| [48] Tsai, 2018 | no | yes | yes | yes | yes | yes | insufficient |
| [49] Uemura, 2018 | yes | yes | yes | yes | yes | unclear | exceeds |
| [41] Zhuang, 2016 | yes | no | no | yes | no | no | matches |
| [35] Banbury, 2020 | yes | yes | yes | yes | yes | yes | matches |
| [36] Handa, 2020 | yes | yes | yes | yes | yes | no | exceeds |
| [37] Kim, 2020 | yes | no | no | yes | yes | no | insufficient |
| [33] Knudsen, 2019 | yes | yes | no | yes | yes | no | matches |
| [51] McCaffery, 2019 | yes | yes | no | yes | yes | unclear | insufficient |
| [34] Tavakoly Sany, 2019 | yes | no | no | yes | yes | no | insufficient |
| [52] Smith, 2019 | yes | yes | yes | yes | yes | yes | matches |
Intervention characteristics
All interventions targeted functional aspects of health literacy (see Table 3), in addition sixteen [32–40, 43, 45, 48–52] also targeted interactive aspects (with a further one [42] providing insufficient information to determine) and four of these [35, 48, 50, 52] also targeted critical health literacy (with a further three [38, 49, 51] being unclear). Intervention designs (as shown in Table 1) included small group sessions [32, 34, 35, 37, 39, 40, 42–45, 48–51], text or social media messages [38, 41, 47], animation [30], multi-media learning [52], app [36] and one to one education [31, 33]. The most common approach was for small group educational classes (14 studies).
Of the text/social media interventions the frequency of messages ranged from 3x/week for 4 months [38] through to once a week for a year [41]. One study used social media for health education counselling for a total of 6 sessions [47], but there was insufficient detail to identify length, duration or content of the sessions.
The 14 small group studies ranged from 40 min [44] to full day sessions [50], with a frequency ranging between twice a week [51], weekly [32, 35, 37, 40, 42, 45, 49] fortnightly [43, 48] and monthly [44]. The intervention duration period ranged from 2 weeks [40] to 12 months [37] of active content. One study did not specify frequency or total intervention duration, just individual session lengths [34]. Across all studies follow-up ranged from the same day [30] to 12 months [37, 41, 50]. The time lag between intervention end and follow up ranged from none [30, 36–38, 41–43, 45, 49] to 6 months [39, 48, 50].
Intervention effects on main outcomes
Table 4 summarises the effect of intervention on both health literacy and behavioural outcomes.
Table 4.
Summary of health literacy and behavioural outcome results
| Reference, 1st author, year, country | Health Literacy | Behavioural outcomes | |||
|---|---|---|---|---|---|
| Significant result found? | Summary result | Behavioural outcome measured | Significant result found? | Summary result | |
| Domain | Health Care | ||||
| [30] Calderon, 2014 USA | Yes | I > C: p = 0.03 | None | ||
| [31] Tai, 2016 USA | Yes | After adjusting for pre-score, I > C: p = 0.011 | None | ||
| [32] Gharachourlo, 2018 Iran | Yes | I > C: p < 0.001 | 10 dimensions of health, physical health, sports and fitness, weight management and nutrition, disease prevention, mental health, spiritual health, social health, avoidance of drugs, alcohol and opiates, accident prevention and environmental health. | Yes for 8/10 dimensions (not environmental health and spiritual health) | I > C: p < 0.001 (Overall lifestyle, physical health, sports & fitness, weight management & nutrition, disease prevention, mental health, social health, avoidance of drugs, alcohol and opiates, accident prevention) |
| [33] Knudsen, 2019 Denmark | For HLQ6 only | HLQ6: I > C p = 0.003 | None | ||
| [34] Tavakoly Sany, 2019 Iran | Yes | I > C: p < 0.05 | Self-care behaviours for heart failure | Yes | I > C: p < 0.05 |
| [35] Banbury, 2020 Australia | No | I vs C: p > 0.05 | None | ||
| [36] Handa, 2020 Japan | No | I vs C: p > 0.05 | None | ||
| [37] Kim. 2020 USA | Yes |
REALM: I > C: 3, 6 months p < 0.01, 12 months p < 0.001 DM-REALM: I > C: 3,6,12 months p < 0.001 TOFHLA: I > C: 3 months p < 0.05 NVS: I > C: 3,6,12 months p < 0.05 |
None | ||
| Domain | Disease prevention | ||||
| [38] Li 2016, Niger | Yes | I > C: p < 0.01 | None | ||
| [39] Han, 2017 USA | Yes | HL change T1 to T2 I > C (p < .05) | Self-reported mammogram at baseline and medical record review at post-test | Yes | I > C, OR 18.5 (95% confidence interval [CI] = 9.2, 37.4) |
| Self-reported pap test at baseline and medical record review at post-test | Yes | I > C, OR 13.3 (95% CI = 7.9, 22.3) | |||
| Self-reported mammogram and pap test at baseline and medical record review at post-test | Yes | I > C, OR 17.4 (95% CI = 7.5, 40.3) | |||
| Domain | Health promotion | ||||
| [40] Otilingam 2015, USA | Yes |
(Combined intervention groups) I > C: p = 0.0103. HL change T1 to T2 I > C: 0.039 HL change T1 to T3 n.s |
Behaviours to reduce dietary fats | Yes | T1 to T3 I > C: p = 0.0140. |
| [41] Zhuang, 2016 China | Yes | I > C: p < 0.001 | None | ||
| [42] Mas, 2017 USA | No | I vs C: p > 0.05 | None | ||
| [43] Parekh, 2017 USA | No | I vs C: p > 0.05 | Nutrition literacy | No | I vs C: p > 0.05 |
| Fruit and vegetable intake | No | I vs C: p > 0.05 | |||
| [44] Liu, 2018 China | Yes | I > C: p < 0.05 | None | ||
| [45, 46] Mas, 2018 (and 2015) USA | Yes | Change score I > C: p = 0.01 | 34 item questionnaire measuring nutrition & physical activity behaviours | Yes, in adjusted model | I > C: p = 0.049. |
| [47] Panahi, 2018 Iran | Yes | HL change T1 –T2 -T3 I > C: p = 0.014 | Smoking behaviour | Yes | I > C: p < 0.0001 |
| [48] Tsai, 2018 Taiwan | No | I vs C: p > 0.05 | None | ||
| [49] Uemura, 2018 Japan | For some but not all domains |
HLS-EU-Q16 I > C: disease prevention score p = 0.04 HLS-14 I > C: Total score p = 0.03, Communicative score p = 0.01, critical score, p = 0.02 |
Dietary habits – food frequency | Yes | I > C p = 0.001 |
| Dietary habits – dietary variety | Yes | I > C p = 0.04 | |||
| Steps per day | Yes | I > C: p < 0.001 | |||
| Total energy expenditure (physical activity level x basal metabolic rate) | Yes | I > C: p = 0.01 | |||
| [50] Fiedler, 2019 Germany | Mixed and inconclusive | A significant effect was only seen for proactive help for the intervention group at T1. | None | ||
| [51] McCaffery 2019, Australia | HLQ3 only | HLQ3: I > C p = 0.01 | None | ||
| [52] Smith, 2019 Australia | No | I vs C: p > 0.05 | None | ||
Note: I Intervention, C Control
Health literacy
Twelve of the studies showed a significant increase in health literacy in the intervention group compared to the control group [30–32, 34, 37–41, 44, 45, 47]. Six showed no significant difference [35, 36, 42, 43, 48, 52], three showed an increase in health literacy for some but not all domains or subscales [33, 49, 51] and one was inconclusive due to mixed results in a crossover design [50]. Four out of the six with no change employed subjective measures [35, 36, 48, 52].
Behavioural outcomes
Many of the studies included additional outcomes such as knowledge [39, 40, 47], self-efficacy [34, 37, 52] morbidity [38], perceptions [39, 47], physical and cognitive function [49], health education impact [35], patient activation [33] and behavioural outcomes [32, 34, 39, 40, 43, 45, 47, 49]. Behaviour was measured in smoking prevention behaviours [47], nutrition related behaviours [40, 43, 49], physical activity behaviours [49], cancer screening behaviours [39], and some measures which encompassed a variety of domains (lifestyle [32], self-care [34] and cardiovascular health [45]).
Smoking prevention behaviours, physical activity and cancer screening were measured in a single study each, and all showed significant changes in favour of the intervention group [39, 47, 49]. Nutrition and diet related behaviours were measured in three studies. Two [40, 49] showed significant results in favour of the intervention group (fat related diet habits, food frequency and dietary variety). The third study [43] measured nutrition literacy and fruit and vegetable intake and found no significant effect of intervention.
Lifestyle factors were measured in one study [32]. This measure considered 10 dimensions of health and found a statistically significant effect of the intervention for overall lifestyle, and for 8 out of 10 sub-dimensions. Cardiovascular health was measured in one study [45] by measuring nutrition and physical activity behaviours and found a significant change in intervention group compared to control. Finally one study [34] found a significant change in intervention compared to control for self-care behaviours in heart failure patients.
Cardiac patients
Two studies focused on cardiac patients [33, 34] and a further two of the studies used a cardiovascular health curriculum within healthy adults to reduce the risk of cardiovascular disease [40, 45]. Tavakoly Sany [34] focused on heart failure patients and ran three educational group workshops using techniques such as teach back and role playing. The study measured health literacy, self-efficacy and self-care behaviours and found a significant effect of intervention in all three aspects – both immediately post intervention and at the three month follow up. Knudsen [33] compared tele-rehabilitation with usual care cardiac rehabilitation for both health literacy and patient activation. They found that neither method of rehabilitation improved patient activation and only one of the HLQ subscales (ability to engage with healthcare providers) showed a significant effect in the intervention group.
Two studies focused on reducing cardiovascular risk in health adults. Both studies were conducted in America and targeted Spanish speaking immigrants. Mas [45] used a combined health literacy and standard English as a second language (ESL) curriculum which used “Salud para su Corazon” (health for your heart) as the main resource. The study measured both health literacy and cardiovascular health behaviours and found a significant effect of intervention in both (although they were not correlated). Otilingam [40] used specifically designed content in two 2-h workshops designed to improve heart health and brain health in Latina’s. The paper measured health literacy and dietary fat reduction behaviours and found significant effects of intervention in both.
Discussion
This systematic review included 22 studies from nine countries involving almost 11,000 participants. In 68% of studies a significant improvement in health literacy was seen. Additionally, eight studies measured behavioural outcomes and in seven of the studies a significant effect in favour of the intervention group was found. Only two studies have been carried out with cardiovascular patients.
Quality appraisal found that no studies were at low risk of bias. This was largely influenced by the lack of pre-published SAP protocols and issues with effective randomisation, allocation concealment and blinding which can be more challenging in this type of interventional study, though not impossible [73]. Analysis of intervention reporting showed that studies were generally poor at reporting sufficient detail of the intervention content to allow replication (and in some cases, effective categorisation of intervention focus).
Notwithstanding this, this systematic review has highlighted the growth in the health literacy field. This review set no lower limit date yet the oldest study including a pre-post measure of health literacy in a controlled trial was 2014. The number of studies has steadily increased (with over half being published since 2018) suggesting a growth in work to establish the evidence base for health literacy interventions. Whilst the most commonly used approach was small group educational interventions it is worth noting that other methods that are less time/resource intensive show promise. A short animation [30], a single 10 min training session [31], remote videoconferencing/tele-rehabilitation [33, 35] and three studies that used social media or SMS messages [38, 41, 47] were all effective at increasing health literacy.
The search for this systematic review captured studies that were not available when the review of community-based interventions was conducted by Nutbeam et al. in 2018 [74]. As Nutbeam [74] indicated, there is a move towards the inclusion of wider aspects of health literacy, with 16 of the interventions in the current review now clearly including interactive aspects but only four interventions clearly including aspects of critical health literacy. It is promising to see more interactive content, but there is an evident lag in including aspects of critical health literacy. This could reflect difficulties in operationalising critical health literacy in measures. For example, a recent study into health literacy interventions in Europe [75] found seven studies (not eligible for this systematic review) with critical health literacy content, but in common with this review, only three of the interventions included any form of critical health literacy measure, and even then it was measured via skills lists, interview or decision-making skills rather than specific health literacy instruments.
This mismatch between measures and intervention content can have significant effects. Half of the studies in this review did not have measures capable of measuring all aspects of health literacy targeted in the intervention [34, 37–40, 42, 43, 45, 48, 50, 51]. Notably four out of the seven studies that did not find an increase in health literacy as a result of the intervention fell within this group [42, 43, 48, 50]. In addition, only 12 of the studies [35, 37, 38, 40, 41, 43, 45, 47–49, 51, 52] included an indication of their intervention’s theoretical underpinnings. Whilst there is debate as to whether theory contributes to the efficacy of interventions [76, 77], in a field which is striving to develop an evidence base, theory allows for the systematic development, comparison and refinement of interventions and is something that should be encouraged [78].
As a determinant of health, health literacy may offer a way to improve outcomes for populations most at risk of health inequalities. Whilst several studies focus on migrants, other at-risk populations have not been similarly targeted for intervention. This is particularly noticeable with regards to gender. Recent studies have suggested men have lower health literacy than women [79–81], and are more likely to have multiple lifestyle risks [68, 82, 83] yet from our pool of 22 studies six focused exclusively on women and no study focused solely on men.
Only two studies (both within the past year) have been conducted with cardiac patients. One of these compared two different modes of cardiac rehabilitation, and the other conducted three education sessions with heart failure patients. It is surprising that more interventions have not been conducted with cardiac patients as yet, given that evidence shows they are at higher risk for health literacy issues [14, 15] and that they can benefit from behavioural interventions. The evidence in this review suggests that health literacy interventions are effective at influencing behaviour, though as no study conducted mediation analysis, we are unable to confirm the direction of this influence.
This review has highlighted rapid growth in intervention studies with just five studies published up until 2016 and then a rapid increase with three in 2017, six in 2018, five in 2019 and three in the first quarter of 2020. We can also see evidence of improved methodological designs in later studies – perhaps as a result of comments by Brainard et al. [84] regarding methodological challenges in health literacy research. A key observation was that there is not enough focus on patient-centred outcomes, and interventions could be more useful if they involved patients in the design - rather than assuming that simply telling people what they need to do is sufficient to bring about change. Three studies [34, 35, 37] in 2019 and 2020 involved participants in intervention content and design. In addition, the only four studies [34, 36, 37, 52] with lower risk of bias (some concerns) were from 2019 to 2020.
The ultimate aim of health literacy interventions is to bring about behaviour change in order to make an individual/agent/organisation behave in a health literate way. In recent years we can see the behaviour change field has developed a considerable number of frameworks, theories, components and techniques. Whilst this review started out asking if health literacy interventions influenced behaviour change, it has become apparent that heath literacy interventions can both influence behaviour change but could also learn from behaviour change theory. Interventions designed along behaviour change principles have the potential to be more robust, effective and applicable – at all levels.
Limitations
This review is the first (to the best of our knowledge) to focus on controlled trial health literacy interventions with pre and post measures, in adults across all health conditions and domains. It adds to the body of knowledge by demonstrating that controlled trial health literacy interventions are increasing rapidly and can be an effective method of both improving health literacy and changing health behaviours. Nevertheless, there are limitations. It is known that there are close links between the concept of health literacy and other concepts such as activation, empowerment and education. By restricting the search terms to studies which identify themselves as health literacy interventions and include a pre-post health literacy measure it is possible we have missed other studies which may have demonstrated effects on health literacy. In addition, we have restricted the search to full peer reviewed and published English language quantitative papers only, and there may well be qualitative studies, or studies in other languages that can contribute to the review question. In addition, it should be noted that all included studies were at risk of bias with 18 judged at high risk. This may impact on ability to draw reliable conclusions from the included studies.
Given health literacy has been around as a concept with dedicated measures for over 30 years it is essential that health literacy begins to operate as a clearly defined concept, with its own terms, measures and dedicated interventions. By restricting the search terms to health literacy specific studies, we begin to demarcate the field and strengthen the evidence base for health literacy interventions.
Conclusions
Even allowing for the strict inclusion criteria applied, 22 studies were found with health literacy interventions. Fifteen of these studies demonstrated that interventions targeting health literacy can improve health literacy. In addition, seven out of eight studies with a behavioural outcome found that the health literacy intervention had a significant effect on behaviour. The health literacy field is growing rapidly, with all studies published since 2014 and over half since 2018. In order to continue to develop the evidence base, health literacy interventions should begin to consider the wider aspects of health literacy and make better use of behaviour change theory to more effectively change the health literacy behaviour of participants – which in turn may help behaviour change interventions be more effective.
Supplementary information
Additional file 1: Supplementary Table 1. PRISMA-S, search results, screening decisions and search strategies.
Additional file 2: Supplementary Table 2. Coding for the 12 TIDieR items for individual studies, divided into intervention and control conditions.
Additional file 3: Supplementary Table 3. Percentage of studies scoring at each reporting grade for the 12 TIDieR items for individual studies, divided into intervention and control conditions.
Additional file 4: Supplementary Table 4. Risk of bias.
Acknowledgements
Not applicable
Abbreviations
- ESL
English as a second language
- HLQ
Health literacy questionnaire
- HRQOL
Health related quality of life
- NHS
National health service
- NVS
Newest vital sign
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
- RCT
Randomised controlled trial
- RoB 2
Risk of Bias 2
- ROBINS-I
Risk of bias in non-randomised studies of interventions
- SAP
Statistical analysis plan
- STOFHLA
Short test of functional health literacy in adults
- TIDieR
Template for intervention description and replication
- TOFHLA
Test of functional health literacy in adults
Authors’ contributions
RW, TG and RP designed the search strategy. RW and TG conducted the search, screening, data-extraction and analysis. TC and SL assisted with data interpretation. RW drafted the manuscript and all authors contributed to revisions. All authors have approved the submitted version and agree to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Funding
This project has been funded by the EU’s INTERREG VA programme, managed by the Special EU Programmes Body (SEUPB). The funding body played no role in the design, collection, analysis, interpretation or writing of the manuscript.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12889-020-08991-0.
References
- 1.Simonds SK. Health Education as Social Policy. Health Educ Monogr. 1974;2(1_suppl):1–10. [Google Scholar]
- 2.Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259–267. [Google Scholar]
- 3.Nutbeam D, McGill B. International Handbook of Health Literacy: Research, practice and policy across the lifespan. Bristol: Policy press; 2019. Improving health literacy in clinical and community populations. [Google Scholar]
- 4.Marks DF, Murray M, Evans B, Willig C, Sykes CM, Woodall C. Health psychology: theory, research and practice. London: Sage; 2005. [Google Scholar]
- 5.Nutbeam D. Defining, measuring and improving health literacy. Health Eval Promot. 2015;42(4):450–456. [Google Scholar]
- 6.Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sykes S, Wills J, Rowlands G, Popple K. Understanding critical health literacy: a concept analysis. BMC Public Health. 2013;13(1):150. doi: 10.1186/1471-2458-13-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67(12):2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 9.Trezona A, Dodson S, Osborne RH. Development of the Organisational health literacy responsiveness (org-HLR) self-assessment tool and process. BMC Health Serv Res. 2018;18(1):694. doi: 10.1186/s12913-018-3499-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sørensen K, Pelikan JM, Röthlin F, Ganahl K, Slonska Z, Doyle G, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU) Eur J Pub Health. 2015;25(6):1053–1058. doi: 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 12.Taggart J, Williams A, Dennis S, Newall A, Shortus T, Zwar N, et al. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Fam Pract. 2012;13(1):12. doi: 10.1186/1471-2296-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Apfel F, Tsouros AD. Health literacy: the solid facts. 2013. [Google Scholar]
- 14.Friis K, Lasgaard M, Osborne RH, Maindal HT. Gaps in understanding health and engagement with healthcare providers across common long-term conditions: a population survey of health literacy in 29 473 Danish citizens. BMJ Open. 2016;6(1):e009627. doi: 10.1136/bmjopen-2015-009627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rowlands GP, Mehay A, Hampshire S, Phillips R, Williams P, Mann A, et al. Characteristics of people with low health literacy on coronary heart disease GP registers in South London: a cross-sectional study. BMJ Open. 2013;3(1) Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3549254/. [cited 2019 Nov 19]. [DOI] [PMC free article] [PubMed]
- 16.World Health Organisation. Cardiovascular diseases (CVDs) World Health Organization/Fact sheets/Cardiovascular Diseases. 2017. [Google Scholar]
- 17.Jakab M, Farrington J, Bogermans L, Mantingh F. Health systems respond to noncommunicable diseases: time for ambition. Copenhagen: WHO Regional Office for Europe; 2018. [Google Scholar]
- 18.British Heart Foundation . Turning back the Tide. 2018. [Google Scholar]
- 19.Resurrección DM, Moreno-Peral P, Gómez-Herranz M, Rubio-Valera M, Pastor L, Caldas de Almeida JM, et al. Factors associated with non-participation in and dropout from cardiac rehabilitation programmes: a systematic review of prospective cohort studies. Eur J Cardiovasc Nurs. 2019;18(1):38–47. doi: 10.1177/1474515118783157. [DOI] [PubMed] [Google Scholar]
- 20.Pedersen M, Overgaard D, Andersen I, Baastrup M, Egerod I. Mechanisms and drivers of social inequality in phase II cardiac rehabilitation attendance: a convergent mixed methods study. J Adv Nurs. 2018;74(9):2181–2195. doi: 10.1111/jan.13715. [DOI] [PubMed] [Google Scholar]
- 21.Herber OR, Smith K, White M, Jones MC. ‘Just not for me’ – contributing factors to nonattendance/noncompletion at phase III cardiac rehabilitation in acute coronary syndrome patients: a qualitative enquiry. J Clin Nurs. 2017;26(21–22):3529–3542. doi: 10.1111/jocn.13722. [DOI] [PubMed] [Google Scholar]
- 22.Murray J, Craigs CL, Hill KM, Honey S, House A. A systematic review of patient reported factors associated with uptake and completion of cardiovascular lifestyle behaviour change. BMC Cardiovasc Disord. 2012;12(1):120. doi: 10.1186/1471-2261-12-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geboers B, Reijneveld SA, Koot JAR, de Winter AF. Moving towards a Comprehensive Approach for Health Literacy Interventions: The Development of a Health Literacy Intervention Model. Int J Environ Res Public Health. 2018;15(6):1268–1279. doi: 10.3390/ijerph15061268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albus C. Health literacy: is it important for cardiovascular disease prevention? Eur J Prev Cardiolog. 2018;25(9):934–935. doi: 10.1177/2047487318770519. [DOI] [PubMed] [Google Scholar]
- 25.de Melo Ghisi GL, da Silva Chaves GS, Britto RR, Oh P. Health literacy and coronary artery disease: a systematic review. Patient Educ Couns. 2018;101(2):177–184. doi: 10.1016/j.pec.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 26.Loke YK, Hinz I, Wang X, Salter C. Systematic review of consistency between adherence to cardiovascular or diabetes medication and health literacy in older adults. Ann Pharmacother. 2012;46(6):863–872. doi: 10.1345/aph.1Q718. [DOI] [PubMed] [Google Scholar]
- 27.Cabellos-Garcia AC, Martinez-Sabater A, Castro-Sanchez E, Kangasniemi M, Juarez-Vela R, Gea-Caballero V. Relation between health literacy, self-care and adherence to treatment with oral anticoagulants in adults: a narrative systematic review. BMC Public Health. 2018;18(1):1157. doi: 10.1186/s12889-018-6070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chan A. Health literacy screening instruments in adults with cardiovascular disease and their importance to the nursing profession. Aust J Adv Nurs. 2014;32(2):14–23. [Google Scholar]
- 29.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Calderon JL, Shaheen M, Hays RD, Fleming ES, Norris KC, Baker RS. Improving diabetes health literacy by animation. Diabetes Educ. 2014;40(3):361–372. doi: 10.1177/0145721714527518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tai BWB, Bae YH, La Rue CE, Law AV. Putting words into action: a simple focused education improves prescription label comprehension and functional health literacy. J Am Pharmacists Assoc. 2016;56(2):145–152. doi: 10.1016/j.japh.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 32.Gharachourlo M, Mahmoodi Z, Akbari Kamrani M, Tehranizadeh M, Kabir K. The effect of a health literacy approach to counselling on the lifestyle of women with gestational diabetes: A clinical trial. F1000Res. 2018;7:282. doi: 10.12688/f1000research.13838.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Knudsen MV, Petersen AK, Angel S, Hjortdal VE, Maindal HT, Laustsen S. Tele-rehabilitation and hospital-based cardiac rehabilitation are comparable in increasing patient activation and health literacy: a pilot study. Eur J Cardiovasc Nurs. 2019;1474515119885325 10.1177/1474515119885325. [DOI] [PubMed]
- 34.Tavakoly Sany BS, Peyman N, Zadehahmad Z, Ferns G, Doosti H. Effect of educational interventions on health literacy in patients with heart failure. Int J Health Promot Educ. 2019;57(1):23–36. [Google Scholar]
- 35.Banbury A, Nancarrow S, Dart J, Gray L, Dodson S, Osborne R, et al. Adding value to remote monitoring: co-design of a health literacy intervention for older people with chronic disease delivered by telehealth-the telehealth literacy project. Patient Educ Couns. 2020;103(3):597–606. doi: 10.1016/j.pec.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 36.Handa S, Okuyama H, Yamamoto H, Nakamura S, Kato Y. Effectiveness of a smartphone application as a support tool for patients undergoing breast cancer chemotherapy: a randomized controlled trial. Clin Breast Cancer. 2020; 10.1016/j.clbc.2020.01.004. [DOI] [PubMed]
- 37.Kim MT, Kim KB, Ko J, Murry N, Xie B, Radhakrishnan K, et al. Health literacy and outcomes of a community-based self-help intervention: a case of Korean Americans with type 2 diabetes. Nurs Res. 2020;69(3):210–218. doi: 10.1097/NNR.0000000000000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li W, Han L, Guo Y, Sun J. Using WeChat official accounts to improve malaria health literacy among Chinese expatriates in Niger: an intervention study. Malar J. 2016;15(1):567. doi: 10.1186/s12936-016-1621-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Han HR, Song Y, Kim M, Hedlin HK, Kim K, Lee HB, et al. Breast and cervical Cancer screening literacy among Korean American women: a community health worker-led intervention. Am J Public Health. 2017;107(1):159–165. doi: 10.2105/AJPH.2016.303522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Otilingam PG, Gatz M, Tello E, Escobar AJ, Goldstein A, Torres M, et al. Buenos Hábitos Alimenticios Para Una Buena Salud: evaluation of a nutrition education program to improve heart health and brain health in Latinas. J Aging Health. 2015;27(1):177–192. doi: 10.1177/0898264314549660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhuang R, Xiang Y, Han T, Yang G, Zhang Y. Cell phone-based health education messaging improves health literacy. Afr Health Sci. 2016;16(1):311–318. doi: 10.4314/ahs.v16i1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mas FS, Jacobson HE, Olivarez A. Adult education and the health literacy of Hispanic immigrants in the United States. J Latinos Educ. 2017;16(4):314–322. [Google Scholar]
- 43.Parekh N, Jiang J, Buchan M, Meyers M, Gibbs H, Krebs P. Nutrition literacy among Cancer survivors: feasibility results from the healthy eating and living against breast Cancer (HEAL-BCa) study: a pilot randomized controlled trial. J Cancer Educ. 2018;33(6):1239–1249. doi: 10.1007/s13187-017-1238-z. [DOI] [PubMed] [Google Scholar]
- 44.Liu Y-B, Li Y-F, Liu L, Chen Y-L. Effectiveness of the teach-back method for improving the health literacy of senior citizens in nursing homes. JJNS. 2018;15(3):195–202. doi: 10.1111/jjns.12192. [DOI] [PubMed] [Google Scholar]
- 45.Mas FS, Schmitt CL, Jacobson HE, Myers OB. A cardiovascular health intervention for Spanish speakers: the health literacy and ESL curriculum. J Community Health. 2018;43(4):717–724. doi: 10.1007/s10900-018-0475-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mas FS, Ji M, Fuentes BO, Tinajero J. The health literacy and ESL study: a community-based intervention for Spanish-speaking adults. J Health Commun. 2015;20(4):369–376. doi: 10.1080/10810730.2014.965368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Panahi R, Ramezankhani A, Tavousi M, Niknami S. Adding health literacy to the health belief model: effectiveness of an educational intervention on smoking preventive behaviors among university students. Iran Red Crescent Med J. 2018;20(2):12. [Google Scholar]
- 48.Tsai TI, Lee SYD, Yu WR. Impact of a problem-based learning (PBL) health literacy program on immigrant Women’s health literacy, health empowerment, navigation efficacy, and health care utilization. J Health Commun. 2018;23(4):340–349. doi: 10.1080/10810730.2018.1445798. [DOI] [PubMed] [Google Scholar]
- 49.Uemura K, Yamada M, Okamoto H. Effects of active learning on health literacy and behavior in older adults: a randomized controlled trial. J Am Geriatr Soc. 2018;66(9):1721–1729. doi: 10.1111/jgs.15458. [DOI] [PubMed] [Google Scholar]
- 50.Fiedler S, Pfaff H, Petrowski K, Pförtner T-K. Effects of a classroom training program for promoting health literacy among IT managers in the workplace: a randomized controlled trial. J Occup Environ Med. 2019;61(1):51–60. doi: 10.1097/JOM.0000000000001471. [DOI] [PubMed] [Google Scholar]
- 51.McCaffery KJ, Morony S, Muscat DM, Hayen A, Shepherd HL, Dhillon HM, et al. Evaluation of an Australian health literacy program delivered in adult education settings. Health Lit Res Pract. 2019;3(3):S42–S57. doi: 10.3928/24748307-20190402-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Smith CA, Chang E, Gallego G, Khan A, Armour M, Balneaves LG. An education intervention to improve decision making and health literacy among older Australians: a randomised controlled trial. BMC Geriatr. 2019;19(1):129. doi: 10.1186/s12877-019-1143-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ad Hoc Committee on Health Literacy Health literacy - report of the council on scientific affairs. JAMA-J Am Med Assoc. 1999;281(6):552–557. [PubMed] [Google Scholar]
- 54.Ratzan SC, Parker RM. Health literacy. Bethesda: National Institutes of Health: US Department of Health and Human Services; 2000. [Google Scholar]
- 55.World Health Organisation . Health Promotion Glossary. Geneva: World Health Organisation; 1998. p. 36. [Google Scholar]
- 56.Lenartz N. Gesundheitskompetenz und Selbstregulation: V&R unipress GmbH. 2012. [Google Scholar]
- 57.Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun. 2010;15(S2):9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- 58.Haghdoost AA, Rakhshani F, Aarabi M, Montazeri A, Tavousi M, Solimanian A, et al. Iranian Health Literacy Questionnaire (IHLQ): An Instrument for Measuring Health Literacy in Iran. Iran Red Crescent Med J. 2015;17(6) Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4537788/. [cited 2019 Jul 11]. [DOI] [PMC free article] [PubMed]
- 59.Han H-R, Huh B, Kim MT, Kim J, Nguyen T. Development and Validation of the Assessment of Health Literacy in Breast and Cervical Cancer Screening. J Health Commun. 2014;19(sup2):267–284. doi: 10.1080/10810730.2014.936569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mark L. Health literacy and the elderly. Osteopath Fam Physician. 2009;1(3):64–69. [Google Scholar]
- 61.Li Z, Sun Z. Research on the status of health literacy among residents in Hunan Province and its influencing factors (PhD thesis). Central South University. 2010. [Google Scholar]
- 62.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 63.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults. J Gen Intern Med. 1995;10(10):537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 64.Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21(8):878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Montazeri ALI, Tavousi M, Rakhshani F, Azin SA, Jahangiri K, Ebadi M, et al. Health literacy for Iranian adults (HELIA): development and psychometric properties. 2014. [Google Scholar]
- 67.Kimbrough JB. Health literacy as a contributor to immigrant health disparities. J Health Dispar Res Pract. 2007;1(2):6. [Google Scholar]
- 68.Buck D, Frosini F. Clustering of unhealthy behaviours over time: implications for policy and practice. London: The Kings Fund; 2012. p. 24. [Google Scholar]
- 69.Suka M, Odajima T, Kasai M, Igarashi A, Ishikawa H, Kusama M, et al. The 14-item health literacy scale for Japanese adults (HLS-14) Environ Health Prev Med. 2013;18(5):407. doi: 10.1007/s12199-013-0340-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.ABS Adult Literacy . Life Skills Survey, Summary Results. Canberra: Australian Bureau of Statistics: Australian Government Publishing Service Cat; 2006. p. 4228.0. [Google Scholar]
- 71.Osborne RH, Batterham RW, Elsworth GR, Hawkins M, Buchbinder R. The grounded psychometric development and initial validation of the health literacy questionnaire (HLQ) BMC Public Health. 2013;13(1):658–675. doi: 10.1186/1471-2458-13-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25(6):391–395. [PubMed] [Google Scholar]
- 73.Friedberg JP, Lipsitz SR, Natarajan S. Challenges and recommendations for blinding in behavioral interventions illustrated using a case study of a behavioral intervention to lower blood pressure. Patient Educ Couns. 2010;78(1):5–11. doi: 10.1016/j.pec.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 74.Nutbeam D, McGill B, Premkumar P. Improving health literacy in community populations: a review of progress. Health Promot Int. 2018;33(5):901–911. doi: 10.1093/heapro/dax015. [DOI] [PubMed] [Google Scholar]
- 75.Visscher BB, Steunenberg B, Heijmans M, Hofstede JM, Devillé W, van der Heide I, et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health. 2018;18(1):1414. doi: 10.1186/s12889-018-6331-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hagger MS, Weed M. DEBATE: do interventions based on behavioral theory work in the real world? Int J Behav Nutr Phys Act. 2019;16(1):36. doi: 10.1186/s12966-019-0795-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Prestwich A, Webb T, Conner M. Using theory to develop and test interventions to promote changes in health behaviour: evidence, issues, and recommendations. Curr Opinion Psyschol. 2015;5:1–5. [Google Scholar]
- 78.Dalgetty R, Miller CB, Dombrowski SU. Examining the theory-effectiveness hypothesis: a systematic review of systematic reviews. Br J Health Psychol. 2019;24(2):334–356. doi: 10.1111/bjhp.12356. [DOI] [PubMed] [Google Scholar]
- 79.van der Heide I, Rademakers J, Schipper M, Droomers M, Sorensen K, Uiters E. Health literacy of Dutch adults: a cross sectional survey. BMC Public Health. 2013;13:11. doi: 10.1186/1471-2458-13-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Christy SM, Gwede CK, Sutton SK, Chavarria E, Davis SN, Abdulla R, et al. Health literacy among medically underserved: the role of demographic factors, social influence, and religious beliefs. J Health Commun. 2017;22(11):923–931. doi: 10.1080/10810730.2017.1377322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Oliffe JL, McCreary DR, Black N, Flannigan R, Goldenberg SL. Canadian Men’s health literacy: a nationally representative study. Health Promot Pract. 2019;19:1524839919837625. doi: 10.1177/1524839919837625. [DOI] [PubMed] [Google Scholar]
- 82.Noble N, Paul C, Turon H, Oldmeadow C. Which modifiable health risk behaviours are related? A systematic review of the clustering of smoking, nutrition, alcohol and physical activity (‘SNAP’) health risk factors. Prev Med. 2015;81:16–41. doi: 10.1016/j.ypmed.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 83.OECD . Health at a Glance 2019: OECD Indicators. Paris: OECD; 2019. [Google Scholar]
- 84.Brainard J, Wilsher SH, Salter C, Loke YK. Methodological review: quality of randomized controlled trials in health literacy. BMC Health Serv Res. 2016;16(1):246. doi: 10.1186/s12913-016-1479-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplementary Table 1. PRISMA-S, search results, screening decisions and search strategies.
Additional file 2: Supplementary Table 2. Coding for the 12 TIDieR items for individual studies, divided into intervention and control conditions.
Additional file 3: Supplementary Table 3. Percentage of studies scoring at each reporting grade for the 12 TIDieR items for individual studies, divided into intervention and control conditions.
Additional file 4: Supplementary Table 4. Risk of bias.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.