Abstract
Emotion dysregulation is a transdiagnostic risk factor for many mental health disorders and develops in the context of early trauma exposure. Research suggests intergenerational risk associated with trauma exposure and trauma-related disorders, such that maternal trauma experiences and related symptoms can negatively impact child outcomes across development. The goals of the present study were to examine child and mother correlates of PTSD symptoms in the child and the unique roles of child and maternal emotion dysregulation in understanding child PTSD symptoms among African American mothers and their 8–12 year-old children. Subjects were recruited from an urban hospital serving primarily low-income minority individuals. Correlational results showed that child trauma exposure, child emotion dysregulation, maternal depressive symptoms, maternal emotion dysregulation and potential for maternal child abuse all were significantly associated with child PTSD symptoms (p’s<.05). Hierarchical linear regression models revealed that child trauma exposure, maternal depression, and maternal abuse potential accounted for 29% of the variance in child PTSD symptoms (p<.001). Both child emotion dysregulation (R2change=0.14, p<.001) and maternal emotion dysregulation (R2change=0.04, p<.05) were significantly associated with child PTSD symptoms independent of other risk factors and potential for maternal abuse was no longer a significant predictor. These results suggest that maternal emotion dysregulation may be an important factor in influencing their child’s PTSD symptoms above and beyond child-specific variables. Both maternal and child emotion dysregulation could be valuable treatment targets for improving maternal mental health and parenting behaviors and bolstering child health outcomes, thus reducing intergenerational transmission of risk associated with trauma.
Keywords: posttraumatic stress disorder, trauma, emotion dysregulation, intergenerational risk, abuse
The long-term negative effects of trauma on psychological health across the lifespan are well established (Breslau, 2009; Holt, Buckley, & Whelan, 2008; Schilling, Aseltine, & Gore, 2008). While approximately 70% of the United States population experiences at least one traumatic event in their lifetime (Breslau, 2009), only approximately 6% develop posttraumatic stress disorder (PTSD) (Pietrzak, Goldstein, Southwick, & Grant, 2011). Rates of chronic trauma exposure and the subsequent development of PTSD are substantially higher in low-income African American communities, with rates of lifetime PTSD as high as 30–50% (Gillespie et al., 2009; Powers, Fani, Carter, Cross, & Bradley, 2017). The disproportionate levels of trauma exposure and trauma-related disorders in low-income urban African American communities contribute to the disparities in health outcomes observed for African Americans (Baum, Garofalo, & Yali, 1999; Jackson, Knight, & Rafferty, 2010; Myers et al., 2015). In addition, maternal trauma exposure in African Americans contributes to negative health outcomes in their children (Cross et al., 2017; Jovanovic et al., 2011) and thus it is critical to understand factors involved in intergenerational transmission of trauma-related risk in children
Maternal trauma exposure and PTSD increase intergenerational risk for trauma and trauma-related psychopathology, including both PTSD and depressive symptoms, in their children (Yehuda et al., 2005; Yehuda, Halligan, & Bierer, 2001). This may be particularly true for mothers with a history of exposure to child abuse (Bifulco et al., 2002; Jovanovic et al., 2011; Möhler et al., 2009). There are many pathways through which maternal trauma exposure and PTSD may lead to negative mental health outcomes in the child (e.g., Chemtob et al., 2010; van Ee, Kleber, & Mooren, 2012; Yehuda & Bierer, 2007). Research focusing on environmental contributors to this pathway has shown the effects of maternal disorder (e.g. PTSD) (Koen et al., 2017; Yehuda, Halligan, & Bierer, 2001) and the mediating impact of parenting behaviors in the context of PTSD (for reviews see Berg-Nielsen, Vikan, & Dahl, 2002; Christie, Hamilton-Giachritsis, Alves-Costa, Tomlinson, & Halligan, 2019; Van Ee, Kleber, & Jongmans, 2016). In a study with Holocaust survivors, maternal PTSD predicted child PTSD, whereas parental trauma exposure and depression were not predictive (Yehuda, Halligan, & Bierer, 2001). Another study with Holocaust survivors showed that risk for the development of PTSD in children of mothers with PTSD may be driven in part through parental engagement in negative parenting behaviors, such as abuse (Möhler et al., 2009; Yehuda, Halligan, & Grossman, 2001). In a study of African American children, a previous study by our group showed that maternal child abuse potential was associated with higher levels of PTSD symptoms in the children, although maternal trauma exposure and PTSD were not (Cross et al., 2017). DSM-based boundaries between mental health disorders may unnecessarily complicate models of intergenerational transmission of trauma. Thus, to enhance our understanding of how maternal psychopathology and parenting behavior interrelate to increase risk in children, underlying transdiagnostic mechanisms of risk should be considered.
One such transdiagnostic risk factor is emotion dysregulation, which reflects deficits in one’s awareness and acceptance of emotions and one’s ability to regulate and manage intense negative emotional states (Gross, 2007). Emotion dysregulation is a risk factor for the development and maintenance of many psychological disorders in adulthood, including PTSD (Kring, 2008; McLaughlin, Hatzenbuehler, Mennin, & Nolen-Hoeksema, 2011; Messman‐Moore & Bhuptani, 2017; Weissman et al., 2019). Similarly, traumatized children are more likely than their non-traumatized counterparts to manifest emotion regulation difficulties, which can then increase risk for trauma-related psychopathology (Burns, Jackson, & Harding, 2010; McLaughlin et al., 2011). However, the association between problems with emotion regulation and PTSD have yet to be examined among African American children with high rates of trauma exposure. Importantly, maternal PTSD can increase risk for emotional reactivity and difficulty with emotion regulation in children as early as infancy (Enlow et al., 2011). Although substantial evidence supports emotion dysregulation as a risk factor for the development of PTSD in the same individual, to our knowledge, no research has examined the unique role of maternal emotion dysregulation in the development of PTSD symptoms in their children.
To date, much of the research on intergenerational trauma and psychopathology risk has focused on Holocaust survivors or the children of mothers who experienced the World Trade Center attacks on September 11. It is imperative to better understand contributors to intergenerational transmission of trauma-related psychopathology within communities at high risk for chronic exposure to trauma and neighborhood violence: these individuals are at greatest risk for negative mental health outcomes and represent a significant proportion of the US population, with almost 16% of individuals (16.2 million people) in major US cities living below the poverty line (Fontenot, Semega, & Kollar, 2018). The present study focuses on a sample of primarily low-income urban-dwelling African American mothers and their children. The goals of this study are to examine the unique associations of both maternal and child emotion regulation difficulties with child PTSD symptoms independent of the potential effects of child and maternal trauma exposure and maternal PTSD and depressive symptoms. Maternal abuse potential was included based on previous findings in this sample showing an association between maternal abuse potential and child PTSD symptoms (Cross et al., 2017). While there is mounting attention on the negative impact of children’s exposure to adverse childhood experiences (ACEs) more broadly (Mersky, Topitzes, & Reynolds, 2013), we were interested in traumatic experiences since these are a required precursor to PTSD. This study will move this field of research forward by elucidating the differential effects of maternal and child emotion dysregulation in the context of trauma exposure and PTSD to show the potential intergenerational impacts of emotion dysregulation from mother to child and may identify valuable treatment targets for an at-risk, underserved population.
Method
Procedure
Participants were drawn from an NICHD-funded study of intergenerational transmission of trauma and PTSD risk in mothers and their school-aged children in a low socioeconomic, primarily African American urban population. Participants were first enrolled in a larger project, the Grady Trauma Project, which was initiated as an NIMH-funded study examining genetic and trauma-related risk factors for the development of PTSD among non-psychiatric treatment seeking individuals within an urban hospital setting (Gillespie et al., 2009). Participants were recruited from the primary care, obstetrics and gynecology, diabetes, and pharmacy waiting rooms of a public, not-for profit hospital treating primarily underserved, low socioeconomic status minorities (>90% African American) in urban Atlanta, GA. We approached any individual in the waiting room. To be eligible for participation in the parent study, subjects had to be 18–65 years of age and able to give informed consent. After signing the informed consent, an initial interview was administered with questionnaires regarding trauma history, PTSD symptoms, and psychological variables in mothers. For the current study, mothers had to self-identify as African American and have custody of their children, and the children had to fall in the age range of 8 to 12; this age range includes the period when pubertal development typically begins in children. Participants, mother or child, with self-reported intellectual disability, active psychotic disorder, and autism spectrum disorder were excluded. Participants were not required to have experienced trauma to be eligible for the study. Informed consent for self and child participation was obtained from mothers and assent was obtained from children. All study procedures were approved by the institutional review boards of Emory University School of Medicine and Grady Memorial Hospital in Atlanta, Georgia. Data were collected on these participants between 2013 and 2018.
Participants
The sample consisted of 105 African American mother-child dyads who had complete data for maternal trauma, psychiatric symptoms, and emotion dysregulation and child trauma and PTSD symptoms. The sample was predominately low income, with 61.9% of individuals unemployed and 76.9% coming from households with a monthly income of less than $2,000. Maternal education level was as follows: 23% had less than a high school education, 33.2% had a high school degree or GED, 20% had some college or technical school education, and 23.8% had a higher education degree (technical school, college, or graduate school).
Measures
The Childhood Trauma Questionnaire (CTQ) (Bernstein et al., 2003) is a 25-item, brief, reliable and valid self-report instrument that was used to assess maternal exposure to sexual, physical, emotional abuse, and neglect in childhood. Researchers created a continuous variable to represent overall severity of exposure to childhood abuse and neglect. Higher scores on the measure indicated higher levels of reported abuse or neglect. Internal consistency of this measure in the current study was high, α = 0.90.
The Traumatic Events Inventory (TEI) is a 14-item screening instrument for lifetime history of traumatic events, assessing both type and frequency of trauma(s) experienced. Consistent with prior research (Gillespie et al., 2009), total level of trauma exposure was measured by a sum score reflecting the total number of trauma types (e.g., serious accident or injury, sexual assault, and natural disaster) to which a participant had been exposed over the course of their life. For this study, the TEI was used to measure trauma exposure over the lifetime for mothers.
The Modified Posttraumatic Stress Disorder Symptom Scale (mPSS; Coffey, Dansky, Falsetti, Saladin, & Brady, 1998) is a reliable and well-validated 18-item self-report measure that was used to assess maternal PTSD symptoms based on DSM-IV-TR (American Psychiatric Association, 2000) criteria. Internal consistency of this measure in the current study was high, α = 0.91. PTSD symptoms were totaled to create an overall measure of PTSD symptom severity in the mothers. The presence/absence of a probable PTSD diagnosis was determined based on if participants met for at least 1 re-experiencing symptom, 3 avoidance and/or numbing symptoms, 2 hyperarousal symptoms, and if the duration of symptoms was greater than one month.
The Beck Depression Inventory-II (BDI-II) (Beck, Steer, & Brown, 1996) is a reliable and well validated 21-item self-report measure used to assess maternal depressive symptoms. Internal consistency of this measure in the current study was high, α = 0.93. Depression symptoms were totaled to create an overall measure of depression symptom severity in the mothers. Depression severity scores were coded as follows: none or minimal depression = 0–13, mild depression = 14–19, moderate depression = 20–28, and severe depression = 29–63 based on previously identified cutoffs (Beck et al., 1996). In the present study, presence/absence of probable depression included moderate-or-severe levels of depressive symptoms.
The Child Abuse Potential Inventory, Second Edition (CAPI) (Milner, 1994) is a 160-item self-report measure of risk for perpetration of physical child abuse. Items include statements based on attitudes and parenting behavior that have been previously observed in parents identified as physically abusive. Seventy-seven items contribute to an overall Abuse Potential score and the remaining items contribute to validity indices including the Faking Good Validity Index. Child Abuse Potential scores were analyzed continuously. Internal consistency for the Child Abuse Potential scale in this study was high, α = 0.92.
The Traumatic Events Screening Inventory, Child Report (TESI-C) (Ribbe, 1996) is an 18-item structured clinical interview that assesses a child’s experience of a variety of potential traumatic events including current and previous injuries, hospitalizations, domestic violence, community violence, disasters, accidents, physical abuse, and sexual abuse. As outlined in the measure, a trained interviewer probed additional questions to determine the nature of the traumatic experience and whether it met DSM-5 (American Psychiatric Association, 2013) criteria for a criterion A trauma.
The Children’s Emotion Management Scale (CEMS) (J. Zeman, Shipman, & Penza-Clyve, 2001; J. L. Zeman, Cassano, Suveg, & Shipman, 2010) is a 33-item self-report measure that assesses children’s perception of emotion regulation abilities in the context of anger, sadness, and worry. Items are answered on a three-point Likert scale (1 = hardy ever, 2 = sometimes, and 3 = often). For the present analyses, we focused on the dysregulation subscale that assesses over and under-controlled expression or inappropriate expression of emotions (e.g., screaming). Internal consistency of the CEMS dysregulation scale in our sample was high, α = 0.76.
The UCLA PTSD Reaction Index, Child Version (UCLA PTSD-RI) (Steinberg & Beyerlein, 2013; Steinberg, Brymer, Decker, & Pynoos, 2004) is a 20-item semi-structured interview to assess for PTSD symptoms in school-aged children and adolescents. The symptom scale assesses the frequency of PTSD symptoms during the past month (0 = none to 4 = most of the time). The UCLA PTSD-RI has shown good reliability and validity in assessing child PTSD symptoms (Elhai et al., 2013; Steinberg et al., 2013). Participants either completed the DSM-IV-TR version (Association & Association, 2000) or the DSM-5 version (Association, 2013). Since the number of items changed from DSM-IV-TR to DSM-5, individual scores were z-scored to combine across the two measures to create a total PTSD score. Diagnosis was based on DSM-IV-TR (American Psychiatric Association, 2000) or DSM-5 (American Psychiatric Association, 2013) diagnostic criteria.
Data Analysis
All statistical analyses were conducted using SPSS Version 24.0 (Armonk, NY: IBM Corp.). First, descriptive statistics on all variables of interest were run and are included in Table 1. We examined the distributions of all key predictor and outcome variables; level of skewness (range 0.48 to 0.95) and kurtosis (range −0.91 to 1.13) for all variables of interest fell within acceptable parameters for the sample size on all variables (Tabachnick & Fidell, 2001). Second, correlational analyses were performed to determine associations of maternal child maltreatment severity, maternal trauma history, maternal PTSD, maternal depression, maternal emotion dysregulation, maternal child abuse potential, and child trauma exposure and child emotion regulation difficulties with child PTSD symptom severity. A correlation between child age and child PTSD symptoms was conducted to determine if age should be included in the regression model; the correlation was not significant (r=−0.13, p=0.17) and was therefore not included in the model. Finally, based on the results of correlational analyses, a series of hierarchical linear regression models were conducted to determine the unique associations between maternal emotion dysregulation and child PTSD symptoms independent of other significant variables of interest (p<.05 cutoff was used for correlations). The unique impact of child emotion dysregulation also was examined within the final model. The decision to use a series of models was chosen due to smaller sample sizes for maternal child abuse potential (n=91) and child emotion regulation difficulties (n=68).
Table 1.
Descriptive Details of Variables of Interest
| Variables | Mean | SD | Range |
|---|---|---|---|
| Maternal child maltreatment severity (CTQ) | 44.08 | 20.55 | 25–105 |
| Maternal trauma exposure (TEI) | 5.16 | 3.34 | 0–16 |
| Maternal PTSD symptoms (mPSS) | 13.58 | 12.38 | 0–47 |
| Maternal depression symptoms (BDI-II) | 15.05 | 12.13 | 0–58 |
| Maternal emotion dysregulation (DERS) | 70.32 | 24.35 | 36–157 |
| Maternal child abuse potentialΔ (CAPI) | 176.74 | 109.99 | 24–437 |
| Child trauma exposure (TESI) | 4.67 | 2.72 | 0–12 |
| Child PTSD symptoms (UCLA PTSD-RI) | |||
| DSM-IV | 17.19 | 12.72 | 0–52 |
| DSM-5 | 14.40 | 18.57 | 0–62 |
| Child emotion dysregulation† (CEMS) | 16.29 | 4.35 | 10–29 |
Note: CTQ = Childhood Trauma Questionnaire, TEI = Traumatic Events Inventory, mPSS = Modified PTSD Symptom Scale for DSM-IV, BDI-II = Beck Depression Inventory, II, DERS = Difficulty in Emotion Regulation Scale, CAPI = Child Abuse Potential Index, TESI = Traumatic Events Screening Index, UCLA PTSD-RI = UCLA PTSD Reaction Index, and CEMS = Child Emotion Management Scale.
n=91
n=68
Results
This was a highly traumatized sample of mothers and their children, with the mean number of types of traumas for both mothers and children greater than four (See Table 1). Levels of depressive and PTSD symptoms in mothers also were high, with 35.2% endorsing moderate or severe levels of current depressive symptoms and 32.4% meeting probable criteria for current PTSD. Twenty-one percent of the children met criteria for a PTSD diagnosis.
Correlational analyses (Table 2) showed significant positive associations between child trauma exposure, maternal depression symptoms, and maternal child abuse potential with child PTSD symptoms (p<.001, p<.05, and p=.001, respectively). There also were significant positive associations between child PTSD symptom and both child emotion dysregulation symptoms and maternal emotion dysregulation symptoms (p<.001 and p=.001, respectively). Maternal trauma exposure and PTSD symptom severity were not associated with child PTSD symptoms, ps > .05.
Table 2.
Correlations between variables of interest and child PTSD symptoms
| Variables of Interest | Child PTSD Symptoms | |
|---|---|---|
| r | p | |
| Maternal child maltreatment severity | 0.15 | 0.12 |
| Maternal trauma exposure | 0.18 | 0.07 |
| Maternal PTSD symptoms | 0.09 | 0.36 |
| Maternal depression symptoms | 0.22 | 0.02* |
| Maternal emotion dysregulation | 0.32 | 0.001** |
| Maternal child abuse potentialΔ | 0.35 | 0.001** |
| Child trauma exposure | 0.49 | <0.001*** |
| Child emotion dysregulation† | 0.50 | <0.001*** |
Note:
p<.05,
p<.01,
p<.001
n=91
n=68
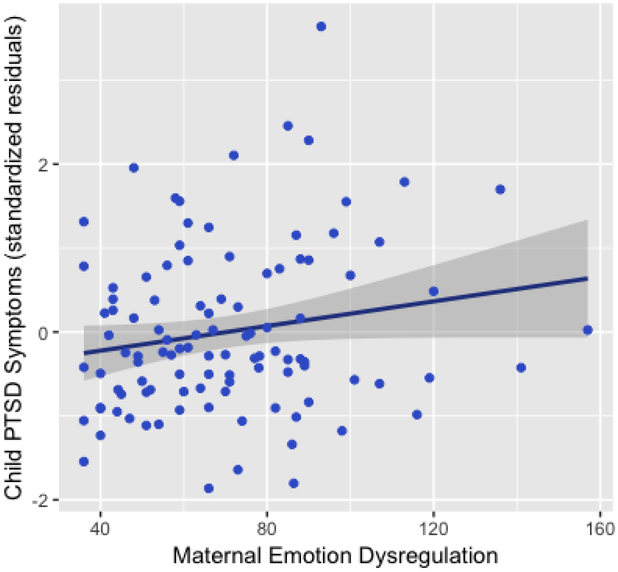
Based on the significant correlations found in the overall sample, the first hierarchical linear regression model included child trauma exposure and maternal depressive symptoms (Step 1), and maternal emotion dysregulation (Step 2). As shown in Table 3, Step 1 was significant (p<.001) and child trauma exposure and maternal depressive symptoms accounted for 25% of the variance in child PTSD symptoms. When both variables were included together in this model, however, only child trauma exposure was associated significantly with child PTSD symptoms (p<.001). When maternal emotion dysregulation was included in the model, emotion dysregulation accounted for an additional 6% of variance in child PTSD symptoms (p=.004) and was independently associated with child PTSD above and beyond effects of child trauma exposure (see Figure 1).
Table 3.
Hierarchical linear regression model predicting child PTSD symptoms by child trauma exposure, maternal depression symptoms, and maternal emotion dysregulation
| Predicting child PTSD symptoms | β | t | R | R2 Change | F-change | p-change |
|---|---|---|---|---|---|---|
| Step 1 | 0.50 | 0.25 | 17.04 | <.001*** | ||
| Child trauma exposure | 0.46 | 5.24*** | ||||
| Maternal depression symptoms | 0.11 | 1.24 | ||||
| Step 2 | 0.56 | 0.06 | 8.85 | .004** | ||
| Child trauma exposure | 0.47 | 5.51*** | ||||
| Maternal depression symptoms | −0.19 | −1.44 | ||||
| Maternal emotion dysregulation | 0.39 | 2.98** |
Note:
p<.01,
p<.001
Figure 1.
The relation between total maternal emotion dysregulation and child PTSD symptoms (controlling for maternal depression and child trauma exposure, t = 2.98, p = .004).
A second hierarchical linear regression model included child trauma exposure, maternal depressive symptoms, and maternal child abuse potential in the model as Step 1 in a smaller sample size with CAPI data available (n=91). Similar results emerged although now Step 1 accounted for 31% of variance in child PTSD symptoms (F = 13.14, p<.001) and child abuse potential was a significant predictor (t = 3.19, p=.002). In Step 2, maternal emotion dysregulation remained a significant predictor although the relation was slightly attenuated (t = 2.67, p=.009).
Finally, as shown in Table 4, a third hierarchical linear regression model was performed using the subsample of children that completed the child emotion regulation measure (n=68). In this model, child emotion dysregulation was associated significantly with child PTSD symptoms independent of trauma exposure, maternal depressive symptoms, and maternal abuse potential (R2change = 0.14, p<.001). Again, maternal emotion dysregulation also was a significant predictor of child PTSD symptoms independent of child trauma and emotion dysregulation, as well as maternal depressive symptoms or abuse potential (R2change = 0.04, p<.05).
Table 4.
Hierarchical linear regression model predicting child PTSD symptoms by child trauma exposure, maternal depression symptoms, maternal child abuse potential, child emotion dysregulation, and maternal emotion dysregulation
| Predicting child PTSD symptoms | β | t | R | R2 Change | F-change | p-change |
|---|---|---|---|---|---|---|
| Step 1 | 0.54 | 0.29 | 8.59 | <.001*** | ||
| Child trauma exposure | 0.42 | 3.87*** | ||||
| Maternal depression symptoms | −0.18 | −1.27 | ||||
| Maternal child abuse potential | 0.42 | 3.10** | ||||
| Step 2 | 0.65 | 0.14 | 15.16 | <.001*** | ||
| Child trauma exposure | 0.36 | 3.68*** | ||||
| Child emotion dysregulation | 0.39 | 3.89*** | ||||
| Maternal depression symptoms | −0.13 | −1.00 | ||||
| Maternal child abuse potential | 0.30 | 2.33* | ||||
| Step 3 | 0.68 | 0.04 | 4.43 | 0.039* | ||
| Child trauma exposure | 0.36 | 3.74*** | ||||
| Child emotion dysregulation | 0.39 | 3.98*** | ||||
| Maternal depression symptoms | −0.30 | −2.04 | ||||
| Maternal child abuse potential | 0.20 | 1.54 | ||||
| Maternal emotion dysregulation | 0.32 | 2.10* |
Note: n=68;
p<.05,
p<.01,
p<.001
Discussion
This study highlights the unique relevance of both maternal and child emotion dysregulation to child PTSD symptoms in a highly traumatized and low-income sample of African American mother-child dyads. The results add to the growing evidence that emotion dysregulation in children is associated with negative mental health outcomes – in this case PTSD – above and beyond trauma exposure. Our findings expand upon this line of research to show the intergenerational impacts of emotion dysregulation from mother to child. More specifically, we found that maternal emotion dysregulation was significantly associated with greater PTSD symptoms in the child independent of the child’s own trauma exposure or emotion regulation difficulties as well as independent of the mother’s trauma history and psychiatric symptoms.
Emotional development begins as early as infancy and is strongly influenced by maternal responsiveness and care, which highlights how important the maternal role may be in addressing the cycle of intergenerational risk associated with trauma (Enlow et al., 2011; Van Ee et al., 2016). Developmental research has established that negative experiences within the home, including potential maltreatment by caregivers or negative parenting behaviors, can lead to problems with emotion regulation in children from preschool through adolescence (Bifulco et al., 2002; Weissman et al., 2019). Thus, emotion dysregulation, a critical transdiagnostic risk factor for many trauma-related disorders and problems, often develops during childhood (Aldao, Nolen-Hoeksema, & Schweizer, 2010; McLaughlin et al., 2011). This development of emotion dysregulation occurs in part through learned behaviors and modeling in the home environment; when caregivers or family environments are harsh and unsupportive, children are less likely to be exposed to appropriate regulatory behavior and more likely to experience emotional invalidation which then leads to the development of emotion dysregulation in themselves (Alink, Cicchetti, Kim, & Rogosh, 2009; Kim & Cicchetti, 2010). As previous research in our lab has shown, abuse potential in mothers is a significant predictor of PTSD symptoms in children (Cross et al., 2017). However, in the present study, when maternal emotion dysregulation was included in our model, maternal abuse potential was no longer associated with child PTSD symptoms. Maternal emotion dysregulation may be an important underlying factor that mediates negative parenting behaviors such as abuse potential. This suggests that directly targeting emotion dysregulation in psychological treatment could reduce psychiatric symptoms in the mother and in turn decrease mothers’ potential for negative parenting behaviors and improve outcomes in their children.
The results also demonstrated the key role that childhood trauma exposure plays in children’s PTSD symptom manifestation. Specifically, we found that both child trauma exposure and child emotion dysregulation had strong associations with child PTSD symptoms, independent of one another. The number of traumas experienced is an important predictor of the development of PTSD (Breslau, 2009) and this was substantiated in the present study with school-aged children. It is certainly true that limiting children’s exposure to traumatic events would decrease the risk for the development of PTSD and importantly, may also decrease the levels of emotion dysregulation in the child. However, because reducing child’s exposure to violence or other traumatic experiences in the community is a complex and resource-intensive problem that requires system-wide change, focusing on addressing the child’s difficulties with emotion regulation to may be a useful initial target for combating childhood PTSD.
Several study limitations are worth noting. First, the data collected were cross-sectional and therefore causality cannot be determined. It is possible that child PTSD symptoms caused increased maternal emotion dysregulation, although prior research shows that emotion regulation abilities develop in childhood and thus it seems less likely that such a causal pattern is the case. Additionally, it is possible that child emotion dysregulation is a result of child PTSD symptoms rather than vice versa. However, multiple longitudinal research studies have shown that prior presence of emotion dysregulation predicts development of psychopathology in adolescence (McLaughlin et al., 2011). Another limitation was the use of only self-report measures for trauma, emotion dysregulation, and psychiatric symptoms (with the exception of child PTSD symptoms). There is value in including clinician rating assessments and additional objective measures of these constructs. Finally, this sample included all African American women and their 8–12 year-old children and the specificity of the sample could limit generalizability of the results. However, this sample was chosen because the mother-child dyads are at high risk for exposure to multiple traumatic experiences and critical health disparities exist among African Americans. It is essential to better understand the intergenerational transmission of risk from trauma and trauma-related psychopathology to improve outcomes for African American children and work to reduce health disparities in low-income communities.
In summary, while evidence supports that emotion dysregulation emerging in development increases risk for negative mental health outcomes like PTSD, this is the first study to demonstrate the intergenerational association of maternal emotion dysregulation with child PTSD symptoms, in a well-powered sample. Our results further emphasize the importance of considering emotion dysregulation as a transdiagnostic treatment target across the lifespan and highlight the potential value of treating maternal emotion dysregulation - not only to improve the health and well-being of the mother - but also to reduce the intergenerational effects of trauma and trauma-related disorders on children of women exposed to chronic trauma. There are a number of emotion regulation-focused skills training interventions that could be beneficial in this context. Specifically, both Dialectical Behavior Therapy (DBT) and Skills Training in Affective and Interpersonal Relationships (STAIR) are treatments that can be used transdiagnostically with individuals with a history of trauma (Cloitre, Koenen, Cohen, & Han, 2002; Neacsiu, Eberle, Kramer, Wiesmann, & Linehan, 2014; Sloan et al., 2017). Incorporating such skills-based protocols with early parenting interventions in high risk trauma populations could be particularly beneficial as we work to reduce health disparities and improve health outcomes across the lifespan in urban African American communities with high trauma exposure.
Clinical Impact Statement.
Difficulties with emotion regulation are a core problem in post-traumatic stress disorder (PTSD) and often develop in the context of early life trauma exposure. This study showed that both maternal and child emotion regulation difficulties were related to the child’s PTSD symptoms following trauma exposure, suggesting that treating emotion regulation difficulties in both mothers and their children could be helpful in reducing the negative consequences of trauma exposure during development.
Acknowledgments
This article was supported in part by the National Institute of Health: K23AT009713 (AP), HD085850 (JSS) and HD071982 (BB).
Appendix
Data Transparency Narrative Description
The data reported in this manuscript were collected as part of a larger data collection. Findings from the data collected have been reported in separate manuscripts. MS 1 (published) focused on maternal and child trauma exposure and PTSD, maternal child abuse potential, and parenting stress; MS 2 (published) focused on maternal emotion dysregulation, parenting stress, and child psychophysiological outcomes via dark-enhanced startle response. MS 3 (the current manuscript) uniquely focuses on the association of maternal and child emotion dysregulation with child PTSD symptoms, including child trauma and maternal child abuse potential as covariates to account for findings from MS1 and previous literature. Data using the child emotion dysregulation variable has not previously been published in any studies from our laboratory.
Footnotes
The authors declare no conflict of interest.
References
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30, 217–237. [DOI] [PubMed] [Google Scholar]
- Alink L, Cicchetti D, Kim J, & Rogosh F (2009). Mediating and moderating processes in the relation between maltreatment and psychopathology: Mother-child relationship quality and emotion regulation. Journal of Abnormal Child Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association AP (2013). Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub. [DOI] [PubMed] [Google Scholar]
- Association AP, & Association AP (2000). Diagnostic and statistical manual-text revision (DSM-IV-TRim, 2000): American Psychiatric Association. [Google Scholar]
- Baum A, Garofalo J, & Yali AM (1999). Socioeconomic status and chronic stress: does stress account for SES effects on health? Ann N Y Acad Sci, 896(1), 131–144. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R, & Brown G (1996). Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Berg-Nielsen TS, Vikan A, & Dahl AA (2002). Parenting related to child and parental psychopathology: A descriptive review of the literature. Clinical child psychology and psychiatry, 7(4), 529–552. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, … Desmond D. (2003). Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child abuse & neglect, 27(2), 169–190. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Moran PM, Ball C, Jacobs C, Baines R, Bunn A, & Cavagin J (2002). Childhood adversity, parental vulnerability and disorder: Examining inter‐generational transmission of risk. Journal of Child Psychology and Psychiatry, 43(8), 1075–1086. [DOI] [PubMed] [Google Scholar]
- Breslau N (2009). The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, Violence, & Abuse, 10(3), 198–210. [DOI] [PubMed] [Google Scholar]
- Burns EE, Jackson JL, & Harding HG (2010). Child maltreatment, emotion regulation, and posttraumatic stress: The impact of emotional abuse. Journal of Aggression, Maltreatment & Trauma, 19(8), 801–819. [Google Scholar]
- Chemtob CM, Nomura Y, Rajendran K, Yehuda R, Schwartz D, & Abramovitz R (2010). Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children’s behavior. Child Development, 81(4), 1129–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie H, Hamilton-Giachritsis C, Alves-Costa F, Tomlinson M, & Halligan SL (2019). The impact of parental posttraumatic stress disorder on parenting: a systematic review. European journal of psychotraumatology, 10(1), 1550345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, & Han H (2002). Skills training in affective and interpersonal regulation followed by exposure: a phase-based treatment for PTSD related to childhood abuse. Journal of consulting and clinical psychology, 70(5), 1067. [DOI] [PubMed] [Google Scholar]
- Cross D, Vance LA, Kim YJ, Ruchard AL, Fox N, Jovanovic T, & Bradley B (2017). Trauma exposure, PTSD, and parenting in a community sample of low-income, predominantly African American mothers and children. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Layne CM, Steinberg AM, Brymer MJ, Briggs EC, Ostrowski SA, & Pynoos RS (2013). Psychometric properties of the UCLA PTSD reaction index. Part II: investigating factor structure findings in a national clinic‐referred youth sample. Journal of traumatic stress, 26(1), 10–18. [DOI] [PubMed] [Google Scholar]
- Enlow MB, Kitts RL, Blood E, Bizarro A, Hofmeister M, & Wright RJ (2011). Maternal posttraumatic stress symptoms and infant emotional reactivity and emotion regulation. Infant Behavior and Development, 34(4), 487–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontenot K, Semega J, & Kollar M (2018). Income and poverty in the United States: 2017. Retrieved from Washington, DC: [Google Scholar]
- Gillespie C, Bradley B, Mercer K, Smith A, Conneely K, Gapen M, & Ressler K (2009). Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry, 31, 505–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt S, Buckley H, & Whelan S (2008). The impact of exposure to domestic violence on children and young people: A review of the literature. Child abuse & neglect, 32(8), 797–810. [DOI] [PubMed] [Google Scholar]
- Jackson JS, Knight KM, & Rafferty JA (2010). Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. American journal of public health, 100(5), 933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jovanovic T, Smith A, Kamkwalala A, Poole J, Samples T, Norrholm SD, … Bradley B (2011). Physiological markers of anxiety are increased in children of abused mothers. Journal of Child Psychology and Psychiatry, 52(8), 844–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychol Psychiatry, 51(6), 706–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koen N, Brittain K, Donald KA, Barnett W, Koopowitz S, Maré K, … Stein DJ (2017). Maternal posttraumatic stress disorder and infant developmental outcomes in a South African birth cohort study. Psychological Trauma: Theory, Research, Practice, and Policy, 9(3), 292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring A (2008). Emotion disturbances as transdiagnostic processes in psychopathology. In Lewis M, Hayiland-Jones J, & Barrett L(Eds.), Handbook of emotion (pp. 691–705). New York: Guilford Press. [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Mennin DS, & Nolen-Hoeksema S (2011). Emotion dysregulation and adolescent psychopathology: A prospective study. Behaviour research and therapy, 49(9), 544–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky JP, Topitzes J, & Reynolds AJ (2013). Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the US. Child abuse & neglect, 37(11), 917–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman‐Moore TL, & Bhuptani PH (2017). A review of the long‐term impact of child maltreatment on posttraumatic stress disorder and its comorbidities: An emotion dysregulation perspective. Clinical psychology: Science and practice, 24(2), 154–169. [Google Scholar]
- Milner JS (1994). Assessing physical child abuse risk: The child abuse potential inventory. Clinical Psychology Review, 14(6), 547–583. [Google Scholar]
- Möhler E, Matheis V, Poustka L, Marysko M, Finke P, Kaufmann C, … Resch F (2009). Mothers with a history of abuse tend to show more impulsiveness. Child abuse & neglect, 33(3), 123–126. [DOI] [PubMed] [Google Scholar]
- Myers HF, Wyatt GE, Ullman JB, Loeb TB, Chin D, Prause N, … Liu H (2015). Cumulative burden of lifetime adversities: Trauma and mental health in low-SES African Americans and Latino/as. Psychological Trauma: Theory, Research, Practice, and Policy, 7(3), 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neacsiu AD, Eberle JW, Kramer R, Wiesmann T, & Linehan MM (2014). Dialectical behavior therapy skills for transdiagnostic emotion dysregulation: A pilot randomized controlled trial. Behaviour research and therapy, 59, 40–51. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of anxiety disorders, 25(3), 456–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers A, Fani N, Carter S, Cross D, & Bradley B (2017). Differential predictors of DSM-5 PTSD and ICD-11 complex PTSD among African American women. European journal of psychotraumatology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribbe D (1996). Psychometric review of traumatic event screening instrument for children (TESI-C). Measurement of stress, trauma, and adaptation, 386–387. [Google Scholar]
- Schilling EA, Aseltine RH, & Gore S (2008). The impact of cumulative childhood adversity on young adult mental health: Measures, models, and interpretations. Soc Sci Med, 66(5), 1140–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan E, Hall K, Moulding R, Bryce S, Mildred H, & Staiger PK (2017). Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clinical Psychology Review, 57, 141–163. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, & Beyerlein B (2013). UCLA PTSD reaction index: DSM-5 version: Los Angeles, CA: The National Child Traumatic Stress Network. [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, & Pynoos RS (2004). The University of California at Los Angeles post-traumatic stress disorder reaction index. Current psychiatry reports, 6(2), 96–100. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Kim S, Briggs EC, Ippen CG, Ostrowski SA, … Pynoos RS (2013). Psychometric properties of the UCLA PTSD reaction index: part I. Journal of traumatic stress, 26(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2001). Using multivariate statistics. [Google Scholar]
- Van Ee E, Kleber RJ, & Jongmans MJ (2016). Relational patterns between caregivers with PTSD and their nonexposed children: A review. Trauma, Violence, & Abuse, 17(2), 186–203. [DOI] [PubMed] [Google Scholar]
- van Ee E, Kleber RJ, & Mooren TT (2012). War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent–child interaction, and child development. Infant mental health journal, 33(5), 459–468. [DOI] [PubMed] [Google Scholar]
- Weissman DG, Bitran D, Miller AB, Schaefer JD, Sheridan MA, & McLaughlin KA (2019). Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Development and Psychopathology, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R, & Bierer LM (2007). Transgenerational transmission of cortisol and PTSD risk. Progress in brain research, 167, 121–135. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Engel SM, Brand SR, Seckl J, Marcus SM, & Berkowitz GS (2005). Transgenerational effects of posttraumatic stress disorder in babies of mothers exposed to the World Trade Center attacks during pregnancy. The Journal of Clinical Endocrinology & Metabolism, 90(7), 4115–4118. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Halligan SL, & Bierer LM (2001). Relationship of parental trauma exposure and PTSD to PTSD, depressive and anxiety disorders in offspring. Journal of psychiatric research, 35(5), 261–270. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Halligan SL, & Grossman R (2001). Childhood trauma and risk for PTSD: Relationship to intergenerational effects of trauma, parental PTSD, and cortisol excretion. Development and Psychopathology, 13(3), 733–753. [DOI] [PubMed] [Google Scholar]
- Zeman J, Shipman K, & Penza-Clyve S (2001). Development and initial validation of the Children’s Sadness Management Scale. Journal of Nonverbal Behavior, 25(3), 187–205. [Google Scholar]
- Zeman JL, Cassano M, Suveg C, & Shipman K (2010). Initial validation of the children’s worry management scale. Journal of Child and Family Studies, 19(4), 381–392. [Google Scholar]