Abstract
In this communication, we proposed sustainable preventive measures that may be adopted by the low-income countries to forestall the potential outbreak and transmission of COVID-19 (coronavirus disease 2019) through wastewater. Most low-income countries have poor sanitation and wastewater management policies, which create potential risks of COVID 19 spread. Hence, the proposed measures include decentralization of wastewater treatment facilities, community-wide monitoring and testing of SARS-CoV-2 in wastewater samples, improved sanitation, developing point-of-use devices for wastewater decontamination, and more focused policy interventions. Therefore, this paper adds useful insights into the monitoring and management of ongoing COVID-19 outbreak in low-income countries.
Keywords: COVID-19, Coronavirus transmission, Low-income countries, SARS-CoV-2, Wastewater reuse
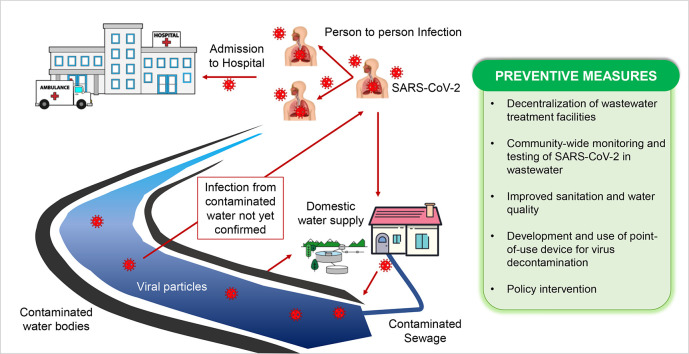
Graphical abstract
1. Introduction
The current global pandemic of novel coronavirus disease 2019 (code-named COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and its potential transmission through wastewater is raising concerns amidst the science community (Amirian, 2020; Venugopal et al., 2020; Randazzo et al., 2020; Ahmed et al., 2020; Nghiem et al., 2020). While studies on the routes through which humans can contract the virus are still evolving, the currently known routes are inhalation of droplets of saliva, sputum, and person-to-person body contacts (WHO, 2020a; Kitajima et al., 2020). Recent studies demonstrate that the SARS-CoV-2 virus is shed in feces from infected patients with severe symptoms (Wang et al., 2020a; Pan et al., 2020), asymptomatic status (Tang et al., 2020), and treated patients with no further sign of the symptoms (Xiao et al., 2020). Lescure et al. (2020) and Ling et al. (2020) also reported the presence of the SARS-CoV-2 viral RNA in the urine samples of infected patients. Similarly, only the SARS-CoV-2 RNA was reported in the hospital sewage and community wastewater (Medema et al., 2020; Lodder and de Roda Husman, 2020). Although the ability of the SARS-CoV-2 to persist in the water medium, including wastewater remains uncertain (Heller et al., 2020), the detection of the SARS-CoV-2 RNA in both untreated and treated wastewater (Ahmed et al., 2020; Venugopal et al., 2020) and the isolation of the infectious SARS-CoV-2 from stool samples (Wang et al., 2020b; Xiao et al., 2020; Zhang et al., 2020b) raise a concern of the risk of the potential spread through this medium (Annalaura et al., 2020; Randazzo et al., 2020; Gupta et al., 2020). However, to date no study could confirm the transmission of SARS-CoV-2 through virus-contaminated water. Also, some studies reported that SARS-CoV-2 loses its infectivity very quickly in wastewater (Venugopal et al., 2020; Annalaura et al., 2020). Nonetheless, other waterborne diseases contracted through the consumption of contaminated water such as diarrhea and gastroenteritis are rampant in low-income countries (Pooi and Ng, 2018).
The current state of the sanitary system in low-income countries, especially in Africa, is critical. The proximity of the pit-latrine sanitation system and groundwater source is very common in many parts of the low-income countries while series of indiscriminate and open defecation close to the surface water has also been reported (Bhallamudi et al., 2019; Back et al., 2018; WHO, 2013). Moreover, the untreated wastewater is often discharged into the environment (Adelodun et al., 2019), which inadvertently could found its way to the groundwater source (Omosa et al., 2012). Since the majority of the population in low-income countries, especially the people in rural and peri-urban communities, largely rely on the surface and groundwater resources to meet their daily water consumption, the potential risk of community spread of COVID-19 disease needs to be taken into consideration.
This communication added to the existing literature on the concerns of possible snowballing transmission of COVID-19 through wastewater (Venugopal et al., 2020; Randazzo et al., 2020; Ahmed et al., 2020; Nghiem et al., 2020; Lodder and de Roda Husman, 2020), with particular interest to propose sustainable measures to mitigate the risk of the potential spread of COVID-19 through wastewater in low-income countries.
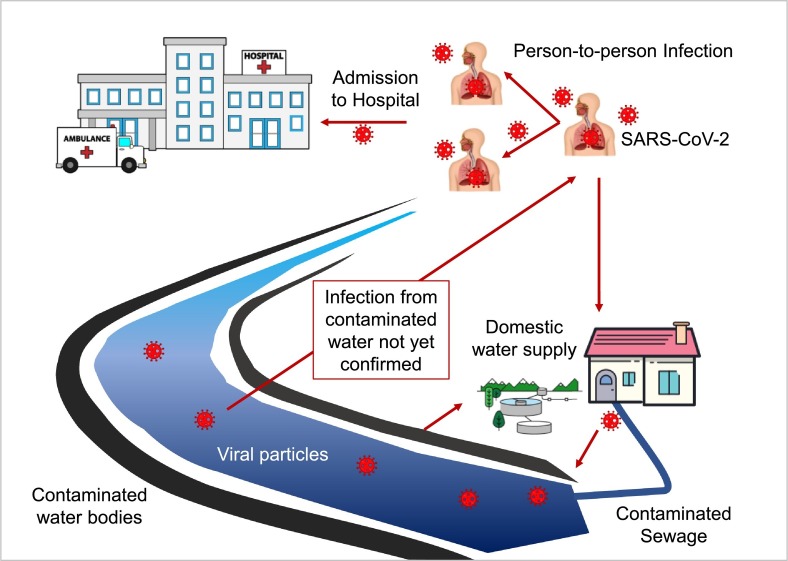
2. Pathways of SARS-CoV-2 RNA in the water systems
The SARS-CoV-2 RNA could enter the water systems through numerous pathways (Fig. 1 ), consequently causing the risk of potential transmission of COVID-19 in the water environment (Annalaura et al., 2020; Venugopal et al., 2020; Lodder and de Roda Husman, 2020). These paths include wastewater discharged from hospitals and isolation and quarantine centers (Wang et al., 2020a; Wang et al., 2020b; Verlicchi et al., 2010). The excreta-related contaminations are found to transmit through the contamination of water systems (Prüss-Ustün et al., 2019). Many water sources can, therefore, be potentially contaminated via varieties of routes. The surface water (streams and lake) where wastewater is often discharged directly without proper treatment can also be a potential vehicle for the SARS-CoV-2 through the water channels into various parts of the communities, where they rely on these water sources for their daily needs in low-income countries.
Fig. 1.
Sources and pathways of SARS-CoV-2 in water systems.
Similarly, groundwater sources are not safe in this regard, as there could be a potential virus-contamination during the groundwater recharge. Also, the hospital wastes when disposed of without proper treatment in water bodies could be a reason for disease transmission (Gupta et al., 2009; Kumar et al., 2020). Hynds et al. (2014) and Kitajima et al. (2018) highlighted several studies where pepper mild mottle virus and other human enteric viruses were detected in both surface and groundwater sources. There is a need to safeguard the water system pathways to prevent unexpected contamination of these water sources from SARS-CoV-2 and other pathogens. Such viruses and pathogens have more potential chances to spread in the areas having inadequate water supply facilities and possible direct infection of employees of wastewater treatment plants (Barcelo, 2020). However, it is reported that half-life of SARS-CoV-2 in wastewater was significantly affected by temperature (Hart and Halden, 2020), UV ozone (Wang et al., 2020c), and chlorine disinfectant (Zhang et al., 2020). The half-life of SARS-CoV-2 in hospital wastewater was estimated to range between 4.8 and 7.2 h at 20 °C, with a 99.9% sequence match in nucleotide and similarity in the spike glycoproteins among the variants of SARS-CoV-2 (Hart and Halden, 2020; Robson, 2020).
The person-to-person contact is the most important factor which enhances the COVID-19 spread rate. A recent example includes the uncontrolled COVID-19 outbreak in the Dharavi place of Mumbai, India. It is South Asia's largest slum area which has nearly 0.65 million population within the 2.5 sq. km area. The person-to-person social distancing measure is not practicable and this led to 3000 confirmed COVID-19 cases. Moreover, water and hygiene practices in slum areas are poorly exercised or adopted, which indicates the reason for annual malaria and dengue fever outbreaks in Dharavi. Hence, it raises a potential concern of SARS-CoV-2 RNA in wastewater and COVID-19 spread (BMC, 2020).
3. Sustainable preventive measures of SARS-CoV-2 in the water systems
The transmissibility of the virus is considered to be from the primary host (bat) to an immediate host, and then to human (host), which can be further widened from human-to-human freely (Tomar and Gupta, 2020). The WHO (2020b) therefore gave the preventive measures to adopt for the mitigation of the spread of the virus, which include maintenance of social distancing, face masking when outdoors, frequent handwashing with soaps or alcohol-based sanitizer, and shunning of touching eyes, nose, and mouth. While these measures are genuine and have been noted to be effective (Australian Academy of Science, 2020), the fear of potential widespread due to community interactions, especially in the low-income countries where many households share sanitary and water systems persists (Amirian, 2020). Therefore, we suggested the following measures, which are not exhaustive and set the tone for further research in this line.
3.1. Decentralization of wastewater treatment facilities
The isolation centers and some of the health care facilities designated for the monitoring and treatment of COVID-19 infected patients share the same sewerage system with the neighboring communities. This arrangement makes people within these communities to likely use the water from the stream or open well (common water sources in low-income countries) within the catchment, and thereby potentially vulnerable to coronavirus diseases. The improper disposal of hospital waste and wastewater without adequate treatment could lead to public health risks and the potential danger of infection (Wang et al., 2020c). Several studies have reported the presence of SARS-CoV-2 in feces and wastewater (Holshue et al., 2020; Wang et al., 2020a; Annalaura et al., 2020). Leakage of sewerage system when conveying wastewater containing contaminated excretes is one of the ways by which sanitary related diseases can be contracted by human beings (Behnke et al., 2020; Gormley et al., 2020). The best way to address this is to create a decentralized wastewater treatment facility. Specifically, separating the wastewater treatment of the health care facilities from the community central systems for proper treatment targeting virus removal.
3.2. Community-wide monitoring and testing of SARS-CoV-2 RNA in wastewater
The low-income countries have been reported to have low testing rates for COVID-19 as compared to developed countries due to lack of adequate testing kits and facilities (Kavanagh et al., 2020; John Nkengasong, 2020). There is currently a significant gap in the testing in many low-income countries, with only 88,432 people tested so far as on June 13, 2020, out of about 200 million in Nigeria, the most populous country in Africa (NCDC, 2020). Therefore, large-scale testing of the huge population would be an arduous task and might not be feasible in these regions. Regrettably, the spread of the virus within a short period among these countries has been attributed to the inability to rapidly detect the infected individual's status before mingling and transmitting the SARS-CoV-2 to others (Mehtar et al., 2020). Since early detection of the virus can be obtained from the feces (Orive et al., 2020), testing of the virus particles in the community wastewater before following it up with individual testing would be an alternative method to contain the spread. The approach of wastewater-based epidemiology is deemed effective and sustainable for the regions of low-income nations to surveil the prevalence of the COVID-19 disease in the population by monitoring the abundance of SARS-CoV-2 in wastewater, then the current scouting for episodic symptoms of the virus from an individual. Daughton (2020) also reiterated the importance of community-wide testing as an inexpensive way to monitor the status and trend of COVID-19 infections. The resourcing of field and laboratory facilities for community-wide monitoring and testing should be one of the major priorities of the governments of low-income countries since it provides significant insight into monitoring the large-scale virus spread within short period and at low-expenses.
3.3. Improved sanitation and water quality
Poor sanitation and lack of adequate water quality have been responsible for many sicknesses and deaths globally. About 829,000 deaths were reported due to water, sanitation, and hygiene-related in 2016 (Prüss-Ustün et al., 2019). The target 6.1 of the Sustainable Development Goal of the United Nations Agenda (SDG 6) was specifically on the provision of clean water and sanitation for all by 2030. However, the lack of improved sanitary and adequate water quality continues in many countries of the low-income nations. Only a few households have separate sanitary systems (bathroom and toilet). At the same time, many still depend on unsafe water sources in the rural communities of low-income nations, where significant populations reside (Armah et al., 2018). Moreover, untreated wastewater management is a major problem in low-income countries with attributable health challenges including respiratory infections, gastroenteritis, lymphatic filariasis, trachoma, schistosomiasis, and many more (Omosa et al., 2012; Prüss-Ustün et al., 2019). The quality of the water system is often judged by a mere appearance using the turbidity level (Massoud et al., 2018), while the testing of the presence of SARS-CoV-2 and other enteric viruses require highly sensitive equipment and facilities in water systems. Some studies have recently reported the use of cheap systems such as paper-based and biosensor devices for the detection of SARS-CoV-2 in wastewater (Mao et al., 2020; Mavrikou et al., 2020). Adequate sanitation and improved water quality are poised to address the potential contamination of water systems by preventing the unexpected transmission of the SARS-CoV-2 and other possible related human enteric viruses that could emanate from feces of an infected person.
3.4. Development and use of the point-of-use device for virus decontamination
The development of a low-cost point-of-use device that could inactivate and remove SARS-CoV-2 and related viruses should be at the forefront of discovery. Previously, some inexpensive point-of-use devices were developed to treat virus-contaminated water. These include iron-oxide bio-sand filters (Bradley et al., 2011), zero-valent iron filter (Shi et al., 2012), gravity-based ultrafilter (Chaidez et al., 2016), nanocellulose-based filter (Mautner, 2020), etc. Such devices will go in no small measure to further mitigate the potential infection of COVID-19 diseases, especially in a setting where there are no effective wastewater treatment systems. Chaidez et al. (2016) developed a low-cost gravity ultrafiltration point-of-use for the treatment of wastewater for the waterborne gastrointestinal pathogen in rural communities of Mexico. Some point-of-use technologies have also been previously developed, especially for developing communities to remove selected waterborne pathogens (Pooi and Ng, 2018) and enteric viruses in the water systems (Gerba et al., 2018). Since preliminary investigations have suggested the oxidants like chlorine, ozonation, and UV irradiation have the potential to inactivate the SARS-CoV-2 in a water environment (Rosa et al., 2020; Wang et al., 2020c; Quevedo-león et al., 2020). This can, therefore, be incorporated into the existing low-cost point-of-use technology for the treatment of wastewater containing feces with possible SARS-CoV-2 (sewage), while further investigations into a specific low-cost technology that can efficiently remove the SARS-CoV-2 from water systems including wastewater is ongoing.
3.5. Policy intervention
The streams serve as recreational waters for people, especially children, in rural communities. The children often have their baths in the streams, which are often used as the primary source of water consumption in many parts of the villages in low-income countries (Garg et al., 2018). The strong policy intervention is required at this critical period of COVID-19 pandemic to ensure adequate compliance with the discharge of wastewater into the environment, especially surface water without proper treatment procedures targeted at removing enteric viruses and other waterborne causing diseases. Sensitization of the populace, especially people in rural villages, on the awareness of the seriousness of the COVID-19 pandemic is essential as many of them do not have access to the happenings in the world. The government and policymakers' roles are very germane to mitigate and prevent the total outbreaks of the ravaging COVID-19. Recognizing the non-existence of standard methodologies to examining the wastewater for the presence of SARS-CoV-2 in terms of both sampling and treatments, there is a need for a rapid process on establishing the standard procedures that could generally be adopted as the COVID-19 is regarded as a pandemic while the employees in the wastewater systems are taking precautionary measures that would prevent them from the possible danger of infections.
4. Conclusion
The potential outbreak of COVID-19 disease in low-income countries due to poor sanitary systems and lack of proper wastewater treatment cannot be ignored as it is related to the quality of personal hygiene. The vast population coupled with low socioeconomic status in these nations could serve as an avenue for the potential spread of COVID-19 disease and other waterborne pathogens. The inexhaustible preventive measures, including decentralization of wastewater treatment facilities, community-wide monitoring and testing of SARS-CoV-2 in wastewater, improved sanitation and water quality, development, and the use of the point-of-use device for virus decontamination, and policy intervention were proffered, especially for the low-income countries to forestall the unexpected outbreaks transmission of the COVID-19 disease via wastewater. The improved sanitation and adequate water quality can significantly address the potential waterborne diseases that could emanate from wastewater.
CRediT authorship contribution statement
Bashir Adelodun: Conceptualization, Investigation, Visualization, Writing - original draft, Writing - review & editing. Fidelis Odedishemi Ajibade: Investigation, Visualization, Writing - review & editing. Rahmat Gbemisola Ibrahim: Investigation, Visualization, Writing - review & editing. Hashim Olalekan Bakare: Investigation, Visualization, Writing - review & editing. Kyung-Sook Choi: Visualization, Resources, Supervision, Project administration.
Declaration of competing interest
All authors declare no conflict of interest.
Acknowledgments
We gratefully acknowledge the assistance of Pankaj Kumar of Agro-ecology and Pollution Research Laboratory, Department of Zoology and Environmental Science, Gurukula Kangri Vishwavidyalaya, Haridwar-249404 (Uttarakhand), India, who thoroughly read the manuscript and offered brilliant suggestions to improve the manuscript.
Editor: Damia Barcelo
References
- Adelodun B., Odedishemi F., Segun M., Choi K.-S. Dosage and settling time course optimization of Moringa oleifera in municipal wastewater treatment using response surface methodology. Desalin. Water Treat. 2019;167:45–56. doi: 10.5004/dwt.2019.24616. [DOI] [Google Scholar]
- Ahmed W., Angel N., Edson J., Bibby K., Bivins A., O’Brien J.W., Choi P.M., Kitajima M., Simpson S.L., Li J., Tscharke B., Verhagen R., Smith W.J.M., Zaugg J., Dierens L., Hugenholtz P., Thomas K.V., Mueller J.F. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amirian E.S. Potential fecal transmission of SARS-CoV-2: current evidence and implications for public health. Int. J. Infect. Dis. 2020;95:363–370. doi: 10.1016/j.ijid.2020.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annalaura C., Federigi I., Dasheng L., Julian R.T., Marco V. Making waves: coronavirus detection, presence and persistence in the water environment: state of the art and knowledge needs for public health. Water Res. 2020;179:115907. doi: 10.1016/j.watres.2020.115907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armah F.A., Ekumah B., Yawson D.O., Odoi J.O., Afitir A.-R., Nyieku Florence Esi. Access to improved water and sanitation in sub-Saharan Africa in a quarter century. Heliyon. 2018;4:e00931. doi: 10.1016/j.heliyon.2018.e00931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Academy of Science Hand sanitiser or soap: making an informed choice for COVID-19 - curious. 2020. https://www.science.org.au/curious/people-medicine/hand-sanitiser-or-soap-making-informed-choice-covid-19
- Back J.O., Rivett M.O., Hinz L.B., Mackay N., Wanangwa G.J., Phiri O.L., Songola C.E., Thomas M.A.S., Kumwenda S., Nhlema M., Miller A.V.M., Kalin R.M. Risk assessment to groundwater of pit latrine rural sanitation policy in developing country settings. Sci. Total Environ. 2018;613–614:592–610. doi: 10.1016/j.scitotenv.2017.09.071. [DOI] [PubMed] [Google Scholar]
- Barcelo D. An environmental and health perspective for COVID-19 outbreak: meteorology and air quality influence, sewage epidemiology indicator, hospitals disinfection, drug therapies and recommendations. J. Environ. Chem. Eng. 2020;8:104006. doi: 10.1016/j.jece.2020.104006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behnke N.L., Cronk R., Shackelford B.B., Cooper B., Tu R., Heller L., Bartram J. Environmental health conditions in protracted displacement: a systematic scoping review. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138234. [DOI] [PubMed] [Google Scholar]
- Bhallamudi S.M., Kaviyarasan R., Abilarasu A., Philip L. Nexus between sanitation and groundwater quality: case study from a hard rock region in India. J. Water, Sanit. Hyg. Dev. 2019;9:703–713. doi: 10.2166/washdev.2019.002. [DOI] [Google Scholar]
- BMC Brihanmumbai Municipal Corporation, official coronavirus cases data website of Mumbai, Maharashtra, India. 2020. https://stopcoronavirus.mcgm.gov.in/
- Bradley I., Straub A., Maraccini P., Markazi S., Nguyen T.H. Iron oxide amended biosand filters for virus removal. Water Res. 2011;45:4501–4510. doi: 10.1016/j.watres.2011.05.045. [DOI] [PubMed] [Google Scholar]
- Chaidez C., Ibarra-Rodríguez J.R., Valdez-Torres J.B., Soto M., Gerba C.P., Castro-del Campo N. Point-of-use unit based on gravity ultrafiltration removes waterborne gastrointestinal pathogens from untreated water sources in rural communities. Wilderness Environ. Med. 2016;27:379–385. doi: 10.1016/j.wem.2016.05.006. [DOI] [PubMed] [Google Scholar]
- Daughton C. The international imperative to rapidly and inexpensively monitor community-wide Covid-19 infection status and trends. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg T., Hamilton S.E., Hochard J.P., Kresch E.P., Talbot J. (Not so) gently down the stream: river pollution and health in Indonesia. J. Environ. Econ. Manage. 2018;92:35–53. doi: 10.1016/j.jeem.2018.08.011. [DOI] [Google Scholar]
- Gerba C.P., Betancourt W.Q., Kitajima M., Rock C.M. Reducing uncertainty in estimating virus reduction by advanced water treatment processes. Water Res. 2018;133:282–288. doi: 10.1016/j.watres.2018.01.044. [DOI] [PubMed] [Google Scholar]
- Gormley M., Aspray T.J., Kelly D.A. COVID-19: mitigating transmission via wastewater plumbing systems. Lancet Glob. Heal. 2020;8:e643. doi: 10.1016/S2214-109X(20)30112-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta P., Mathur N., Bhatnagar P., Nagar P., Srivastava S. Genotoxicity evaluation of hospital wastewaters. Ecotox. Environ. Safe. 2009;72(7):1925–1932. doi: 10.1016/j.ecoenv.2009.05.012. [DOI] [PubMed] [Google Scholar]
- Gupta S., Parker J., Smits S., Underwood J., Dolwani S. Persistent viral shedding of SARS-CoV-2 in faeces – a rapid review. Color. Dis. 2020;22:611–620. doi: 10.1111/codi.15138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart O.E., Halden R.U. Computational analysis of SARS-CoV-2/COVID-19 surveillance by wastewater-based epidemiology locally and globally: feasibility, economy, opportunities and challenges. Sci. Total Environ. 2020;730 doi: 10.1016/j.scitotenv.2020.138875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller L., Mota C.R., Greco D.B. COVID-19 faecal-oral transmission: are we asking the right questions? Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H., Spitters C., Ericson K., Wilkerson S., Tural A., Diaz G., Cohn A., Fox L.A., Patel A., Gerber S.I., Kim L., Tong S., Lu X., Lindstrom S., Pallansch M.A., Weldon W.C., Biggs H.M., Uyeki T.M., Pillai S.K. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hynds P.D., Thomas M.K., Pintar K.D.M. Contamination of groundwater systems in the US and Canada by enteric pathogens, 1990-2013: a review and pooled-analysis. PLoS One. 2014;9 doi: 10.1371/journal.pone.0093301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanagh M.M., Erondu N.A., Tomori O., Dzau V.J., Okiro E.A., Maleche A., Aniebo I.C., Rugege U., Holmes C.B., Gostin L.O. Access to lifesaving medical resources for African countries: COVID-19 testing and response, ethics, and politics. Lancet. 2020;6736:19–22. doi: 10.1016/S0140-6736(20)31093-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitajima M., Sassi H.P., Torrey J.R. Pepper mild mottle virus as a water quality indicator. npj Clean Water. 2018;1 doi: 10.1038/s41545-018-0019-5. [DOI] [Google Scholar]
- Kitajima M., Ahmed W., Bibby K., Carducci A., Gerba C.P., Hamilton K.A., Haramoto E., Rose J.B. SARS-CoV-2 in wastewater: state of the knowledge and research needs. Sci. Total Environ. 2020 doi: 10.1016/J.SCITOTENV.2020.139076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar V., Kumar P., Singh J., Kumar P. Environmental Degradation: Causes and Remediation Strategies. Vol. 1. 2020. Current status of water pollution by integrated industrial hubs (IIHs) in India; p. 104. [Google Scholar]
- Lescure F., Bouadma L., Nguyen D., Parisey M., Wicky P., Behillil S., Gaymard A. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect. Dis. 2020;2:1–10. doi: 10.1016/S1473-3099(20)30200-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling Y., Xu S., Lin Y., Tian D., Zhu Z., Dai F., Wu F., Song Z., Huang W., Chen J., Hu B., Wang S., Mao E., Zhu L., Zhang W., Lu H. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin. Med. J. 2020;133:E007. doi: 10.1097/CM9.0000000000000774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lodder W., de Roda Husman A.M. SARS-CoV-2 in wastewater: potential health risk, but also data source. lancet. Gastroenterol. Hepatol. 2020;1253:30087. doi: 10.1016/S2468-1253(20)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao K., Zhang H., Yang Z. Can a paper-based device trace COVID-19 sources with wastewater-based epidemiology? Environ. Sci. Technol. 2020:3733–3735. doi: 10.1021/acs.est.0c01174. [DOI] [PubMed] [Google Scholar]
- Massoud M.A., Kazarian A., Alameddine I., Al-hindi M. Factors influencing the reuse of reclaimed water as a management option to augment water supplies. Environ. Monit. Assess. 2018;190 doi: 10.1007/s10661-018-6905-y. [DOI] [PubMed] [Google Scholar]
- Mautner A. Nanocellulose water treatment membranes and filters: a review. Polym. Int. 2020 doi: 10.1002/pi.5993. [DOI] [Google Scholar]
- Mavrikou S., Georgia Moschopoulou V.T., Kintzios S. Development of a portable, ultra-rapid and ultra-sensitive cell-based biosensor for the direct detection of the SARS-CoV-2 S1 spike protein antigen. Sensors. 2020;20:3121. doi: 10.3390/s20113121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medema G., Heijnen L., Elsinga G., Italiaander R., Brouwer A. Presence of SARS-Coronavirus-2 in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in the Netherlands. Environ Sci Technol Lett. 2020 doi: 10.1021/acs.estlett.0c00357. acs.estlett.0c00357. [DOI] [PubMed] [Google Scholar]
- Mehtar S., Preiser W., Lakhe N.A., Bousso A., TamFum J.-J.M., Kallay O., Seydi M., Zumla A., Nachega J.B. Limiting the spread of COVID-19 in Africa: one size mitigation strategies do not fit all countries. Lancet Glob. Heal. 2020;0:2019–2021. doi: 10.1016/S2214-109X(20)30212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCDC Nigeria Centre for Disease Control on Coronavirus COVID-19 update 2020. 2020. https://covid19.ncdc.gov.ng/
- Nghiem L.D., Morgan B., Donner E., Short M.D. The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case stud. Chem. Environ. Eng. 2020;1:100006. doi: 10.1016/j.cscee.2020.100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkengasong John. Let Africa into the market for COVID-19 diagnostics. Nature. 2020;580 doi: 10.1038/d41586-020-01265-0. [DOI] [PubMed] [Google Scholar]
- Omosa I.B., Wang H., Cheng S., Li F. Sustainable tertiary wastewater treatment is required for water resources pollution control in Africa. Environ. Sci. Technol. 2012;46:7065–7066. doi: 10.1021/es3022254. [DOI] [PubMed] [Google Scholar]
- Orive G., Lertxundi U., Barcelo Damia. Early SARS-CoV-2 outbreak detection by sewage-based epidemiology. Sci. Total Environ. 2020:183135. doi: 10.1016/j.scitotenv.2020.139298. This. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan X., Chen D., Xia Y. Viral load of SARS-CoV-2 in clinical samples. Lancet Infect. Dis. 2020;20:411–412. doi: 10.1016/S1473-3099(20)30113-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pooi C.K., Ng H.Y. Review of low-cost point-of-use water treatment systems for developing communities. npj Clean Water. 2018;1 doi: 10.1038/s41545-018-0011-0. [DOI] [Google Scholar]
- Prüss-Ustün A., Wolf J., Bartram J., Clasen T., Cumming O., Freeman M.C., Gordon B., Hunter P.R., Medlicott K., Johnston R. Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: an updated analysis with a focus on low- and middle-income countries. Int. J. Hyg. Environ. Health. 2019;222:765–777. doi: 10.1016/j.ijheh.2019.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quevedo-león R., Bastías-Montes J., Espinoza-Tellez T., Ronceros B., Balic I., Muñoz O. Inactivation of coronaviruses in food industry: the use of inorganic and organic disinfectants, ozone, and UV radiation. Scientia Agropecuaria. 2020;11(2):257–266. doi: 10.17268/sci.agropecu.2020.02.14. [DOI] [Google Scholar]
- Randazzo W., Truchado P., Cuevas-Ferrando E., Simón P., Allende A., Sánchez G. SARS-CoV-2 RNA in wastewater anticipated COVID-19 occurrence in a low prevalence area. Water Res. 2020;181 doi: 10.1016/j.watres.2020.115942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robson B. COVID-19 coronavirus spike protein analysis for synthetic vaccines , a peptidomimetic antagonist , and therapeutic drugs , and analysis of a proposed achilles ’ he el conserved region to minimize probability of escape mutations and drug resistance. Comput. Biol. Med. 2020;121 doi: 10.1016/j.compbiomed.2020.103749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa G. La, Bonadonna L., Lucentini L., Kenmoe S., Suffredini E. Coronavirus in water environments: occurrence, persistence and concentration methods - a scoping review. Water Res. 2020;179:115899. doi: 10.1016/j.watres.2020.115899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi C., Wei J., Jin Y., Kniel K.E., Chiu P.C. Removal of viruses and bacteriophages from drinking water using zero-valent iron. Sep. Purif. Technol. 2012;84:72–78. doi: 10.1016/j.seppur.2011.06.036. [DOI] [Google Scholar]
- Tang A., Tong Z., Wang H., Dai Y., Li K., Liu J., Wu W., Yuan C., Yu M., Li P., Yan J. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg. Infect. Dis. J. 2020;26 doi: 10.3201/eid2606.200301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomar A., Gupta N. Prediction for the spread of COVID-19 in India and effectiveness of preventive measures. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venugopal A., Ganesan H., Sudalaimuthu Raja S.S., Govindasamy V., Arunachalam M., Narayanasamy A., Sivaprakash P., Rahman P.K.S.M., Gopalakrishnan A.V., Siama Z., Vellingiri B. Novel wastewater surveillance strategy for early detection of coronavirus disease 2019 hotspots. Curr. Opin. Environ. Sci. Heal. 2020;17:8–13. doi: 10.1016/j.coesh.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verlicchi P., Galletti A., Petrovic M., BarcelÓ D. Hospital effluents as a source of emerging pollutants: an overview of micropollutants and sustainable treatment options. J. Hydrol. 2010;389:416–428. doi: 10.1016/j.jhydrol.2010.06.005. [DOI] [Google Scholar]
- Wang J., Feng H., Zhang S., Ni Z., Ni L., Chen Y., Zhuo L., Zhong Z., Qu T. SARS-CoV-2 RNA detection of hospital isolation wards hygiene monitoring during the Coronavirus Disease 2019 outbreak in a Chinese hospital. Int. J. Infect. Dis. 2020;94:103–106. doi: 10.1016/j.ijid.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., Tan Wenjie. Detection of SARS-CoV-2 in different types of clinical specimens. J. Am. Med. Assoc. 2020:3–4. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Shen J., Ye D., Yan X., Zhang Y., Yang W., Li X., Wang Junqi, Zhang L., Pan L. Disinfection technology of hospital wastes and wastewater: suggestions for disinfection strategy during coronavirus disease 2019 (COVID-19) pandemic in China. Environ. Pollut. 2020 doi: 10.1016/j.envpol.2020.114665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Progress on sanitation and drinking-water: fast facts. 2013. https://www.who.int/water_sanitation_health/monitoring/jmp_fast_facts/en/
- WHO Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. 2020. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations
- WHO Coronavirus disease (COVID-19) advice for the public. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
- Xiao F., Tang M., Zheng X., Liu Y., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158:1831–1833.e3. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang D., Ling H., Huang X., Li J., Li W., Yi C., Zhang T., Jiang Y., He Y., Deng S., Zhang X., Wang X., Liu Y., Li G., Qu J. Potential spreading risks and disinfection challenges of medical wastewater by the presence of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) viral RNA in septic tanks of fangcang hospital. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.140445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Chen C., Zhu S., Shu C., Wang D., Song J., Song Y., Zhen W., Feng Z., Wu G., Xu J., Xu W. Isolation of 2019-nCoV from a stool specimen of a laboratory-confirmed case of the Coronavirus Disease 2019 (COVID-19) China CDC Weekly. 2020;2(8):123–124. doi: 10.46234/ccdcw2020.033. [DOI] [PMC free article] [PubMed] [Google Scholar]