Abstract
Implementation of telemedicine for patient encounters optimizes personal safety and allows for continuity of patient care. Embracing telehealth reduces the use of personal protective equipment and other resources consumed during in-person visits. The use of telehealth has increased to historic levels in response to the coronavirus disease 2019 (COVID-19) pandemic. Telehealth may be a key modality to fight against COVID-19, allowing us to take care of patients, conserve personal protective equipment, and protect health care workers all while minimizing the risk of viral spread. We must not neglect vascular health issues while the coronavirus pandemic continues to flood many hospitals and keep people confined to their homes. Patients are not immune to diseases and illnesses such as stroke, critical limb ischemia, and deep vein thrombosis while being confined to their homes and afraid to visit hospitals. Emerging from the COVID-19 crisis, incorporating telemedicine into routine medical care is transformative. By leveraging digital technology, the authors discuss their experience with the implementation, workflow, coding, and reimbursement issues of telehealth during the COVID-19 era.
Keywords: Telemedicine, Telehealth, Virtual care, Digital health, COVID-19
The Society for Vascular Surgery (SVS) Town Hall on Telemedicine during the coronavirus disease 2019 (COVID-19) era highlights our conversation around COVID-19 and the use of technology and telemedicine to allow efficient communication among physicians, health care professionals, and patients. Now more than ever, physicians need to stay connected with colleagues, who are facing similar challenges. As of June 7, 2020, the United States had over 1,920,904 COVID cases and 109,901 deaths.1 According to the Centers for Disease Control (CDC), at least 9282 health care workers have tested positive for COVID-19, 723 required hospitalization and 27 died, and many more developed symptoms.2 We have seen the upsurge, devastation, and demise among patients and health care workers. Given the impact of this pandemic on our lives and patient care, the SVS Health Information Technology Task Force recommends implementing telemedicine for patient encounters and teleconference for professional interactions to optimize personal safety and continuity of patient care. Embracing telehealth will also reduce the use of personal protective equipment and other resources consumed in face-to-face encounters.
Implementation, patient satisfaction, cost-saving, travel reduction, and reimbursement of telehealth in an integrated health care system have been published previously in vascular surgery.3, 4, 5, 6, 7 The mission of telehealth is to improve patient access/experience, maintain high-quality care, and reduce the cost of care across a population, which will ultimately improve the value of health care. Using telehealth may be a key modality to fight against COVID-19, while we take care of patients, conserve personal protective equipment, and protect health care workers to minimize the risk of spread. The COVID-19 outbreak has the potential to finally make telemedicine a mainstream modality for health care delivery in the United States.
Overview of virtual care
Telehealth is the umbrella term that encompasses the five major categories of virtual care with varying levels of reimbursement. Mobile health includes provision of public health information through mobile devices. Remote patient monitoring includes the use of connected electronic tool to record personal health and medical data. Wearable technologies send information directly to the medical record though app platforms and include Bluetooth-enabled glucose monitoring systems used in endocrinology or home blood pressure monitors. Virtual check-ins are patient-initiated brief communications that connect with patients through the electronic medical records (EMR) or a secure platform. Telemedicine is a visit with a provider using two-way interactive audio and video so that there is real-time communication between the provider and the patient. There are two main pathways for telemedicine: video visits with a patient who is likely at home and telemedicine clinic with an originating site and distant site. The “originating site” is where the patient is located, and the distant site is where the provider conducting the visit is located.
Implementation
One of the most important things is to set up a private computer workstation with audio-video capability and dual monitors for telemedicine. Having the device on a stand allows you to conduct the visit, check the chart, and type at the same time during the visit. A dual-screen computer setup allows for reviewing images and charting during the telehealth visits. A digital clock to keep track of the length of telemedicine visit may be helpful for billing. Large health systems have the capability to provide Health Insurance Portability and Accountability Act (HIPAA) compliant video visits from within the EMR. Examples include Epic and Cerner. If this capability has not been implemented or if you work in a smaller practice, stand-alone HIPAA compliant telemedicine solutions exist. These include Doxy.me, Google G Suite Hangouts Meet, GoToMeeting, InTouch Health, Mend, Mundaii, Skype for Business, swyMed, Updox, VSee, and Zoom for Healthcare. These secured platforms may be used by providers in their private office to perform telemedicine visits.
Epic EMR allows for an easy-to-use video visit platform for patients through the patients' MyChart application, or it may be called by your hospital's name. Providers may use Haiku on the phone or Cantu on a tablet. Performing a telemedicine visit in Epic is simple, and it can be done by two methods. The first method entails going into the provider's schedule and selecting the appropriate chart. The telemedicine icon is found at the bottom of the screen and selected. The second method is by going into the notifications section of the EPIC app. If the patient has entered his or her video visit, the notification can be selected and the provider is taken into the patient's chart and the appropriate video visit. If the patient has entered the visit, there will be a green display when the patient's video is live, and they are ready. The provider should wait until the patient is in the virtual waiting first to avoid patients hearing conversations with other physicians or nursing staff about potentially private health information.
An additional feature of the Epic platform is for image capture while in the video visit. This is performed using the camera icon displayed at the bottom of the visit interaction screen. Epic can then automatically import images captured for the encounter into a note by using the smart phase images. This is a systems-based phrase and will insert all images from that encounter into the note. These images can be placed in the chart as part of the physical examination. Finally, the Epic platform allows the camera flip option. This allows the provider to show patients computed tomography, ultrasound, or X-ray images for the visit.
Patient selection and logistics
Certain patients are particularly suited to a telemedicine visit. These include postoperative patients having an unremarkable and uncomplicated convalescence. Chronic vascular patients who need surveillance with or without vascular imaging represent another group that can frequently be managed remotely. Established patience exhibiting a new complaint can be initially evaluated with a virtual visit and triaged toward an office visit, hospitalization, or delay visit. New referral patients can be evaluated initially through telehealth to determine whether they need to be seen immediately, urgently, or they can be delayed as well until the risks of the viral pandemic have diminished. Disadvantages include the inability to perform an in-person physical examination (pulse examination, wound probing, etc.) or perform any procedures (wound debridement, drainage, suture removal, etc). The goals of incorporating telemedicine into the community vascular surgeon's practice are to keep the physical office waiting room as empty as possible but to keep the virtual waiting room full. It is also to keep the surgeons, providers, and other staff working and on the payroll. Telemedicine allows the vascular surgery practice to maintain a revenue stream to support these aspirations.
After choosing a telemedicine platform, obtaining the necessary hardware is critical, which includes a computer desktop or laptop, microphone, and camera. Some physicians may use a smartphone primarily or as a backup. The practice will need to have a standardized script regarding telemedicine and a workflow process (Fig 1 ). The patient will also require access to the appropriate computer hardware setup or a smartphone. The appointment schedules are then evaluated well in advance, and the appropriate patients are selected for a possible telemedicine visit. They are then contacted and offered the opportunity for a telemedicine visit if they have the necessary devices. If they provide their consent and have the appropriate equipment, their visit is then flagged in the office scheduling software as a telemedicine visit. If an imaging study is required, this is to be scheduled in advance of the visit if possible. If not, it can be scheduled to follow the visit with another telemedicine visit to discuss the results. Before starting telemedicine, it is important to coordinate with the back office or billing company. This will be necessary to identify which payers are not reimbursing for telemedicine as well as to make sure that these patients visits are appropriately flagged in the system so that the correct modifier can be attached.
Fig 1.
Workflow and script. BP, Blood pressure; MA, medical assistant.
Telemedicine at the veterans administration
As the largest integrated national health care delivery system in the United States, the Veterans Administration (VA) provides care for nearly 9 million veterans by 180,000 medical professionals. The VA uses the Veterans Health Information Systems and Technology Architecture based Computerized Patient Record System as its EHR system. The Computerized Patient Record System has neither secure messaging nor video-conferencing features built directly into the graphical user interface. However, the Office of Connected Care was established in 2016 with the mission to extend access to care beyond the traditional office visit, including the MyHealthyVet patient portal, VA telehealth services, and VA mobile applications. Scaling these foundational programs has been instrumental in response to the increased demands during the current COVID-19 pandemic. The MyHealthyVet patient portal provides asynchronous secure messaging from within the Patient Health Record where the patient can also review results and schedule appointments. Home video visits are conducted through the VA Video Connect system. Because VA Video Connect is a web-based app, it does not require patients to register into a portal to launch. Only Apple iOS devices such as iPhones and iPads require downloading of a mobile application. Patients simply tap the hyperlink in their appointment email that launches a browser to initiate the video visit. Since the COVID-19 pandemic, the number telemedicine visits has increased nearly 200-fold in VA Sierra Pacific Network (VISN 21) and were essential to maintaining patient care while minimizing patient clinic and hospital visitations.
Using vascular health APPS
A digital health revolution is fueled by an increase in the prevalence of both smartphones and connected devices. A valuable digital health use case is for postoperative surgical site infection monitoring. Surgical site infections have been reported to be 8% or higher in vascular surgery patients and a significant cause for readmissions.8 Applications to proactively engage patients at home before their follow-up visit to assess postoperative wound status can be implemented. These are typically asynchronous store and forward communication solutions that include photos or videos. HCPCS code G2010 is used for a virtual check-in when a recorded video and/or photo is submitted by an established patient. This requires an interpretation and a follow-up communication within 24 hours. The encounter may not be originating from a related evaluation and management (E/M) coding service provided within the previous 7 days and may not lead to an E/M service within 24 hours after the virtual check-in.
Remote management of chronic conditions may improve health outcomes and lower costs. Programs to manage hypertension, diabetes mellitus, and congestive heart failure are well established in certain health systems. Established patients with a well-defined diagnosis are asked to purchase a connected device, such as a Bluetooth-connected blood pressure cuff for a digital hypertension program to measure their blood pressure at home. This data automatically syncs to the EMR via the patient's smartphone for the mid-level provider or pharmacist to review and make medication changes. Ochsner Health System's digital hypertension program achieved target blood pressure control in 71% of its digital-medicine program vs 31% of the usual-care patients at 90 days.9 Remote monitoring allows for more frequent patient check-ins with the intent of more rapid achievement of treatment goals and prevention of complications. An added benefit is for health coaches to leverage these programs to address behavioral health by providing health education on smoking cessation, nutrition, and exercise.
Peripheral artery disease (PAD) is poised for remote monitoring, particularly in the early stages when patients suffer from claudication. Studies to clinically validate sensors in smartphones and smartwatches in patients with PAD have been conducted to help set the foundation for remote tracking.10 Despite supervised exercise therapy being a grade 1 and level A recommendation in SVS guidelines for claudicants, utilization is quite poor.11 One solution would be to address this with a smartphone-delivered home-based supervised exercise therapy program to schedule exercise sessions, measure effort, and report compliance while providing PAD, smoking cessation, diet, and exercise education with the support of health coaches. Remote monitoring programs are a form of telehealth and have the advantage of continuing to be effective during periods of COVID-19 lockdown.
Workflow issues to optimize efficiency
The workflow for a regular office visit from referral to billing consists of multiple levels and is comparable to the workflow for telehealth visits. The complexity, however, can cause problems during conversion of a scheduled office visit to a telehealth visit. The number of potential pitfalls is even higher if the conversion process must occur rapidly, as was the case at the beginning of the COVID-19 era. Although many challenges depend on the utilized telehealth platform, and the necessary prerequisites both on the patient and provider side, the presence of an infrastructure and experience with telehealth at the health system cannot be overstated.
Although all steps are logical, implementing the conversion of regular office visits to remote visits depends largely on the close interaction between the provider, medical assistant, and scheduler. The larger obstacles such as restrictions of other departments involved in our patient care must be considered, and the vascular provider will have to make the decision on whether the test or diagnostic imaging is necessary or can be deferred. Lastly, the individual provider's experience, and an understanding of and bias toward the telemedicine approach must be considered. Training in person or via training videos is essential to provide the necessary understanding of the process, including scheduling, and documentation of and billing for the telehealth. In general, although the conversion process to telemedicine during a short period is challenging, the workflow issues can be overcome with adequate training and close collaboration of all involved parties. Best practice would be to schedule traditional in-person visits and telemedicine visits as separate blocks for efficiency. The setup and workflow for each is very different. In addition, telemedicine patients tend to be on time because the 15-minute block locks out after the time is up.
As many challenges as the COVID 19 era poses, it is also a chance for vascular surgeons to adopt and establish an additional modality of patient care that is not only highly appreciated by the patients but also safe and effective without compromising quality of care.
Licensure
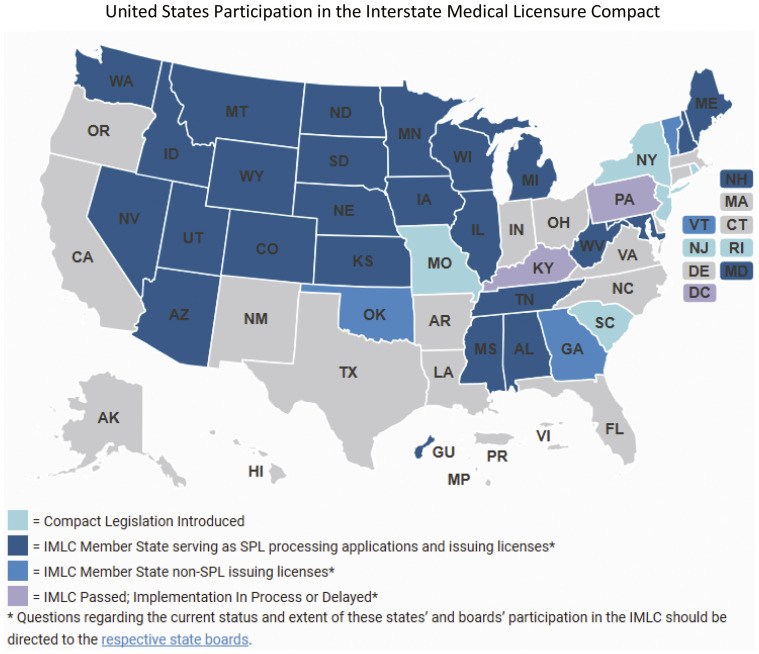
To perform telemedicine, physicians must be licensed in one of the states (Fig 2 ). The Interstate Medical Licensure Compact is an agreement between 29 states, the District of Columbia, and the Territory of Guam. Under this agreement, licensed physicians can qualify to practice medicine across state lines within the Compact if they meet the agreed on eligibility requirements.12 Approximately 80% of physicians meet the criteria for licensure through the Interstate Medical Licensure Compact. During the pandemic, Center for Medicare and Medicaid Services (CMS) has waived the interstate licensing restriction allowing physicians to practice across state lines.
Fig 2.
United States participation in the Interstate Medical Licensure Compact (IMLC). SPL, State of Principal Licensure.
Coding and reimbursement
CMS approved Current Procedural Terminology (CPT) codes for telehealth in 2018 (Table I ). For new patients, use CPT codes 99201-99205, and for established patients, use CPT codes 99211-99215. Some requires you to add point of service POS 02 for Telehealth Medicare and modifier 95 for Commercial Payers. For 2020, CPT codes are separated for online digital visits provided by qualified physician and nonphysician health care professionals (Table II ). Medicare payment for the telephone evaluation and management visits (CPT codes 99441-99443) is equivalent to the Medicare payment for office/outpatient visits with established patients effective March 1, 2020. CMS made major changes to telehealth with over 80 new telehealth codes added, changes in place of service, and fee schedule payment, allowing physician supervision to be done virtually and allowing both new and established patients for virtual check-in.13
Table I.
Telehealth codes
| CPT code | RVU | Minutes |
|---|---|---|
| New patients: CPT codes 99201-99205 for new patients, POS 02 for Telehealth Medicare and modifier 95 for Commercial Payers | ||
| 99201 | 0.48 | 10 |
| 99202 | 0.93 | 20 |
| 99203 | 1.42 | 30 |
| 99204 | 2.43 | 45 |
| 99205 | 3.17 | 60 |
| Established patients: CPT codes 99211-99215 for established patients, POS 02 for Telehealth Medicare and modifier 95 for Commercial Payers | ||
| 99211 | 0.18 | 5 |
| 99212 | 0.48 | 10 |
| 99213 | 0.97 | 15 |
| 99214 | 1.50 | 25 |
| 99215 | 2.11 | 40 |
CPT, Current Procedural Terminology; POS 02, Place of Service 02; RVU, relative value units.
Table II.
New CMS 2020 code updates
| CPT codes | Description |
|---|---|
| Online digital visits: CPT codes 99421-99423. Patient-initiated online digital evaluation and management service provided by qualified physician health care professional | |
| 99421 | For up to 7 days' cumulative time during the 7 days; 5-10 minutes |
| 99422 | For up to 7 days' cumulative time during the 7 days; 11-20 minutes |
| 99423 | For up to 7 days' cumulative time during the 7 days; 21 or more minutes |
| Online digital visits: CPT codes 98970-98972. Patient-initiated online digital evaluation and management service provided by qualified nonphysician health care professional | |
| 98970 | For up to 7 days' cumulative time during the 7 days; 5-10 minutes |
| 98971 | For up to 7 days' cumulative time during the 7 days; 11-20 minutes |
| 98972 | For up to 7 days' cumulative time during the 7 days; 21 or more minutes |
| Remote patient monitoring: CPT codes 99453-99454, 99457-99458, 99091. Collecting and interpreting physiologic data digitally stored and/or caregiver to the physician or qualified health care professional | |
| 99453 | Remote monitoring of physiologic parameters, initial; setup and patient education on use of equipment |
| 99454 | Devices supply with daily recordings or programmed alerts transmission, each 30 days |
| 99457 | Remote physiologic monitoring treatment management services, clinical staff/physician/other qualified health care professional time in a calendar month requiring interactive communication with the patient/caregiver during the month; first 20 minutes |
| 99458 | Each additional 20 minutes |
| 99091 | Collection and interpretation of physiologic data digitally stored and/or transmitted by the patient and/or caregiver to the physician or other qualified health care professional, qualified by education, training, licensure/regulation |
| Telephone evaluation and management service: CPT codes to describe telephone evaluation and management services available since 2008, which are NOT covered by Medicare. Some private payers may pay for these services | |
| 99441 | Telephone evaluation and management service by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment 5-10 minutes of medical discussion |
| 99442 | 11-20 minutes of medical discussion |
| 99443 | 21-30 minutes of medical discussion |
CPT, Current Procedural Terminology; E/M, evaluation and management.
Regardless of coverage, receiving and providing telehealth medicine is not prohibited. Rather, the controversy lies in its reimbursement and coverage. Large commercial insurers, such as Aetna, BlueCross Blue Shield, Cigna, Humana, UnitedHealthcare, and more are moving to expand telehealth coverage. Some states have telemedicine parity laws mandating equal reimbursement for telemedicine and in-person care by commercial payers. CMS has lifted Medicare restrictions on the use of telehealth services during the COVID-19 emergency. Here are the 6 key changes:
-
1.
Effective for services starting March 6, 2020, and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to patients in broader circumstances.
-
2.
These visits are considered the same as in-person visits and are paid at the same rate as regular, in-person visits.
-
3.
Medicare will make payment for professional services furnished to beneficiaries in all areas of the country in all settings.
-
4.
Although they must generally travel to or be located in certain types of originating sites such as a physician's office, skilled nursing facility, or hospital for the visit, Medicare will make payment for telehealth services furnished to beneficiaries in any health care facility and in their home.
-
5.
The Medicare coinsurance and deductible would generally apply to these services. However, the Health and Human Services (HHS) Office of Inspector General is providing flexibility for health care providers to reduce or waive cost-sharing for telehealth visits paid by federal health care programs.
-
6.
To the extent the 1135 waiver requires an established relationship, HHS will not conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency.
Conclusions
At these virtual Town Hall meetings, the panelists learned from each other about their vascular practices, protocols, and preferences through this difficult time. During the pandemic, the use of telemedicine has grown exponentially at many institutions and vascular surgery practices around the country. Our next challenge will be deciding on how to best deploy those limited resources to take care of vascular patients once surgery restrictions are lifted. Although stay-at-home orders have slowed the spread of the virus and flattened the curve, the threat of viral infection will continue until we develop and administer a vaccine. As states ease restrictions, the country will likely experience further regional spikes and waves of infection. Although the risk of dying from COVID-19 may be low in healthy patients, vascular patients are a vulnerable population due to their comorbidities and advanced age. The next step in evidence-based practice would focus on patient-reported satisfaction and clinical outcomes using telemedicine for the management of vascular disease via comparative effectiveness studies. Continuing telemedicine, where appropriate, minimizes viral exposure risk and offers convenience benefits for patients. During these unprecedented times, we encourage everyone to keep open communications and share our best practices.
Author contributions
Conception and design: JL, KH
Analysis and interpretation: JL, MH, WS, OA, UF
Data collection: JL, MH, WS, OA, UF
Writing the article: JL, MH, WS, OA, UF
Critical revision of the article: JL, MH, WS, OA, UF, KH
Final approval of the article: JL, MH, WS, OA, UF, KH
Statistical analysis: Not applicable
Obtained funding: Not applicable
Overall responsibility: JL
From the Society for Vascular Surgery
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Coronavirus Resource Center COVID-19 Case Tracker. Johns Hopkins University & Medicine. https://coronavirus.jhu.edu/ Available at:
- 2.Characteristics of Health Care Personnel with COVID-19—United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477–481. doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin J.C., Kavousi Y., Sullivan B., Stevens C. Analysis of outpatient telemedicine reimbursement in an integrated healthcare system. Ann Vasc Surg. 2019;59:167–172. doi: 10.1016/j.avsg.2019.10.069. [DOI] [PubMed] [Google Scholar]
- 4.Lin J.C., Crutchfield J.M., Zurawski D., Stevens C. Implementation of a virtual vascular clinic with point-of-care ultrasound in an integrated healthcare system: a feasibility pilot study. J Vasc Surg. 2018;68:213–218. doi: 10.1016/j.jvs.2017.11.070. [DOI] [PubMed] [Google Scholar]
- 5.Kavousi Y., Al-Adas Z., Crutchfield J.M., Karamanos E., Swanson C., Lin J.C. Early clinical experience using telemedicine for the management of patients with varicose vein disease. J Telemed Telecare. 2019;25:54–58. doi: 10.1177/1357633X17734580. [DOI] [PubMed] [Google Scholar]
- 6.Lin J.C., McLaughlin D., Zurawski D., Kennedy N., Kabbani L.S. Comparison of virtual visit versus traditional clinic for management of varicose veins. J Telemed Telecare. 2020;26:100–104. doi: 10.1177/1357633X18797181. [DOI] [PubMed] [Google Scholar]
- 7.Paquette S., Lin J.C. Outpatient telemedicine program in vascular surgery reduces patient travel time, cost, and environmental pollutant emissions. Ann Vasc Surg. 2019;59:167–172. doi: 10.1016/j.avsg.2019.01.021. [DOI] [PubMed] [Google Scholar]
- 8.Wiseman J.T., Fernandes-Taylor S., Barnes M.L., Saunders R.S., Saha S., Havlena J., et al. Predictors of surgical site infection after hospital discharge in patients undergoing major vascular surgery. J Vasc Surg. 2015;62:1023–1031.e5. doi: 10.1016/j.jvs.2015.04.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Milani R.V., Lavie C.J., Bober R.M., Milani A.R., Ventura H.O. Improving hypertension control and patient engagement using digital tools. Am J Med. 2017;130:14–20. doi: 10.1016/j.amjmed.2016.07.029. [DOI] [PubMed] [Google Scholar]
- 10.Ata R., Gandhi N., Rasmussen H., El-Gabalawy O., Gutierrez S., Ahmad A., et al. Clinical validation of smartphone-based activity tracking in peripheral artery disease patients. NPJ Digit Med. 2018;1:66. doi: 10.1038/s41746-018-0073-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dua A., Gologorsky R., Savage D., Rens N., Gandhi N., Brooke B., et al. National assessment of availability, awareness, and utilization of supervised exercise therapy for peripheral artery disease patients with intermittent claudication. J Vasc Surg. 2020;71:1702–1707. doi: 10.1016/j.jvs.2019.08.238. [DOI] [PubMed] [Google Scholar]
- 12.Interstate Medical Licensure Compact. https://www.imlcc.org/ Available at:
- 13.CMS list of telehealth services. Centers for Medicare and Medicaid Services. https://www.cms.gov/Medicare/Medicare-General-Information/Telehealth/Telehealth-Codes Available at: