Abstract
Background
Psychological morbidity in both patients and family members related to the intensive care unit (ICU) experience is an often overlooked, and potentially persistent, healthcare problem recognized by the Society of Critical Care Medicine as Post-intensive Care Syndrome (PICS). ICU diaries are an intervention increasingly under study with potential to mitigate ICU-related psychological morbidity, including ICU-related post-traumatic stress disorder (PTSD), depression and anxiety. As we encounter a growing number of ICU survivors, in particular in the wake of the coronavirus pandemic, clinicians must be equipped to understand the severity and prevalence of significant psychiatric complications of critical illness.
Methods
We compared the efficacy of the ICU diary, written by family and healthcare workers during the patient's intensive care course, versus education alone in reducing acute PTSD symptoms after discharge. Patients with an ICU stay >72 h, who were intubated and mechanically ventilated over 24 h, were recruited and randomized to either receive a diary at bedside with psychoeducation or psychoeducation alone. Intervention patients received their ICU diary within the first week of admission into the intensive care unit. Psychological symptom screening with IES-R, PHQ-8, HADS and GAD-7 was conducted at baseline within 1 week of ICU discharge and at weeks 4, 12, and 24 after ICU discharge. Change from baseline in these scores was assessed using Wilcoxon rank sum tests.
Results
From September 26, 2017 to September 25, 2018, our team screened 265 patients from the surgical and medical ICUs at a single large academic urban hospital. 60 patients were enrolled and randomized, of which 35 patients completed post-discharge follow-up, (n = 18) in the diary intervention group and (n = 17) in the education-only control group. The control group had a significantly greater decrease in PTSD, hyperarousal, and depression symptoms at week 4 compared to the intervention group. There were no significant differences in other measures, or at other follow-up intervals. Both study groups exhibited clinically significant PTSD symptoms at all timepoints after ICU discharge. Follow-up phone interviews with patients revealed that while many were interested in getting follow-up for their symptoms, there were many barriers to accessing appropriate therapy and clinical attention.
Conclusions
Results from psychological screening tools demonstrate no benefit of ICU diaries versus bedside education-alone in reducing PTSD symptoms related to the intensive care stay. However, our study finds an important gap in clinical practice – patients at high risk for PICS are infrequently connected to appropriate follow-up care. Perhaps ICU diaries would prove beneficial if utilized to support the work within a program providing wrap-around services and close psychiatric follow up for PICS patients. This study demonstrates the high prevalence of ICU-related PTSD in our cohort of survivors, the high barrier to accessing care for appropriate treatment of PICS, and the consequence of that barrier—prolonged psychological morbidity.
Trial registration
Grant identification
GH-17-022 (Arnold P. Gold Foundation).
1. Background
Patients enduring critical illness carry an increased risk for developing new-onset post-traumatic stress features related to their course in the intensive care unit (ICU). This is largely due to the near-death nature of their medical conditions and complicated hospital courses, which often involve acute stress, delirium, and delusional memories. The prevalence of post-traumatic stress disorder (PTSD) in ICU survivors is estimated at 25–60% after the first month following discharge, and 17–34% during the next 6–12 months [1,2].
ICU-related psychological sequela, such as PTSD, depression, and anxiety, comprise clinically important components of Post-Intensive Care Syndrome (PICS). Both post-ICU PTSD and depression are associated with a significant decrease in patient quality of life after discharge compared to the general population [3,4]. We are thus faced with the challenge of identifying modifiable risk factors in order to prevent the long-term complications of critical care.
Risk factors related to the development of PTSD in the ICU setting include delusional memory formation, poor functional status, use of physical restraints, use of sedation, pre-existing psychiatric history, younger age (<65 years), female gender, sepsis, and treatment with benzodiazepines and neuromuscular blockers [1,[5], [6], [7], [8]]. Early identification of high-risk patients and subsequent interventions in the forms of social support, administration of self-help manuals, and post-discharge psychiatric consultations have all shown to have a protective effect on the incidence of ICU-related PTSD [1,9]. Particular genetic polymorphisms regulating corticotropin-releasing hormone are also associated with significantly fewer post-ICU depressive and post-traumatic stress symptoms [10].
In addition, the use of an ICU diary, where everyday events can be recorded by family members and healthcare workers, has been shown in some studies to reduce new-onset PTSD, anxiety, and depressive symptoms and promote psychological wellbeing in both patients and their families [[11], [12], [13]]. Early interventions, in general, may have the most impact on psychological and cognitive sequela following the ICU course. Thus, early counseling and planned follow-up with mental health providers appears to be critical for at-risk patients.
Previous research has shown that patients exhibiting the most severe PTSD symptoms have no factual recall of their ICU stay and experience vivid delusional memories of their hospital course, such as memories of staff members trying to kill them [14]. The ICU diary's proposed benefit is based on the idea that “one of the strongest and most consistent predictors of subsequent psychological dysfunction is the memory of what may or may not have happened during the course of critical illness” (133) [15]. The early work of Jones, et al. demonstrated benefit of the ICU diary as intervention to improve ICU-related PTSD outcomes [11]; however, subsequent larger multi-centered studies with Randomized Control Trial (RCT) methodology in France have not replicated the early reported benefit [16].
Subjective reports of the secondary benefits of ICU diaries have been recognized, especially among caregivers of patients with PICS. Diaries provide families with a sense of control by allowing them to keep track of general events and to log support and well wishes for their loved one when otherwise unable to communicate. For patients who survive their hospital stay, the diary provides a basic chronology of events and a symbol of the support they received during their ICU stay [17].
Prior studies [11,13] involving ICU diaries have mostly been implemented in Europe, where hospital systems routinely offer diaries to critically ill patients. These trials largely differentiated study groups based on time-to-receiving diaries post-ICU discharge, as opposed to randomizing patients from the onset to diary versus no-diary groups. Our study examines the effect of the diary protocol in a new setting where the culture of ICU diaries had not previously been implemented, and where patients were able to begin reading their diaries as early as one week into their ICU admission if desired. This paper describes our RCT at a large, public, Level One trauma center in the Gulf South to assess the efficacy of a diary versus bedside PTSD education-only on reducing symptoms of new-onset PTSD in patients after their ICU course.
2. Methods
From September 2017 to September 2018, we screened 265 patients at high risk for ICU-related PTSD from both the surgical and medical intensive care units of University Medical Center New Orleans, which holds 60 ICU beds. Inclusion criteria required that patients had an ICU stay >72 h, were sedated and intubated >24 h, and did not have pre-existing PTSD, dementia, intracranial injury, or other debilitating neurocognitive conditions (Supplemental Content, Fig. 2). After screening, 60 patients were enrolled and underwent randomization.
All patients (and available family members) in our study received PTSD education and referrals at the bedside within one week of admission to the intensive care unit (Supplemental Content, 8.2). Patients provided informed consent if able to do so on their own behalf. If not able, a legally authorized representative/surrogate decision-maker provided voluntary written consent for participation into the study for the purpose of initiating the diary intervention while the patient was unconscious. Surrogates were made aware that their consent for the patient could be overridden by the patient when re-consented by our team upon regaining consciousness. Study participants (and respective family members) who received the ICU diary were educated on its purpose by a member of our team. This study was approved by our university and hospital institutional review boards prior to its implementation. Our clinical trial registry is found at https://clinicaltrials.gov/ct2/show/NCT04305353 (with study number NCT04305353).
For the diaries, we used blank journals, into which we encouraged family and ICU healthcare workers write daily events in everyday language. We instructed participants that entries detail daily activities, subjective or hoped for response to treatment, and personal notes of encouragement. This intended to serve as therapeutic for caregivers contributing to the diary writing during hospitalization, as well as for the ICU survivors' understanding of support that was present during their intensive care stay.
While patients were hospitalized, their diaries were always present at the bedside, along with instructions for use for healthcare workers and family. Patients were permitted to read their diaries during their admission if they wished. Diaries remained in the patient's possession after discharge. Our study team did not examine or photocopy contents of the personal diaries. Patients were visited every two to three days until hospital discharge by a member of our study team, who answered questions and encouraged healthcare workers and family members to use the diary during the intensive care course. These visits also served as opportunities for bedside psycho-education and post-discharge mental health resource awareness for family members and patients, in both intervention and control groups. We reminded users of the diaries that they were contributing to a public document and cautioned against including personal or sensitive medical information (e.g.: HIV status, details of treatment, substance use history, and other diagnostic information). Nursing staff also received educational sessions regarding use of the diaries along with written guidelines of best practices. All family members and healthcare staff involved in diary writing received written instructions adapted from prior studies [8,11,18] for consistency (Supplemental Content, 8.3).
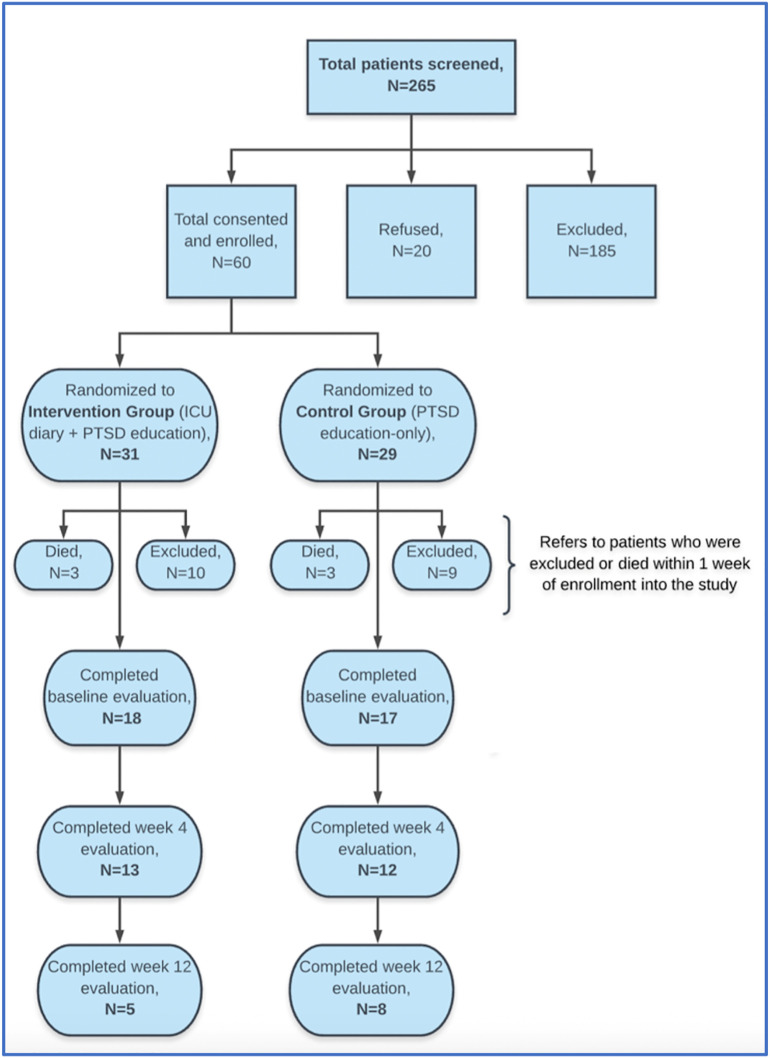
Enrolled patients were randomized to either a diary plus education group (intervention group) or an education-only group (control group) (Fig. 1 ). Randomization was conducted in a 1:1 ratio via a computer-generated algorithm. There was some cross-over between groups during the course of the study due to popularity of the idea of using an ICU diary among family members. We conducted both an intention-to-treat (ITT) analysis maintaining the initial randomization and an as-treated analysis that included the crossover participants originally randomized to the control group in the intervention group. We will present the ITT results and discuss key differences between the ITT results and as-treated results where differences arose.
Fig. 1.
Patient enrollment, randomization, and follow-up. Baseline evaluations were conducted within 1 week of ICU discharge.
Study participants completed the Revised Impact of Event Scales (IES-R), Patient Health Questionnaire (PHQ-8), Hospital Anxiety and Depression Scale (HADS), and Generalized Anxiety Disorder 7-item (GAD-7) within one week of ICU discharge (baseline) and again at the following time points after ICU discharge: week 4, week 12, and week 24. These psychological symptom screenings were administered over the phone. The IES-R assesses the presence and intensity of new-onset PTSD symptoms (range, 0–88; higher scores indicate more severe symptoms), related to a recent inciting event, and we chose to use this for consistency with prior studies [11,16]. The IES-R also includes sub-scores that reflect the severity of hyperarousal, intrusion, and avoidance symptoms. The PHQ-8 identifies the presence and severity of depressive symptoms (range, 0–24; higher scores correspond to more severe symptoms). The question regarding suicidality on the PHQ-8 was omitted due to screening response resource limitations, since the implementation of an appropriate contingency plan would surpass the scope of our team's capabilities. The HADS screens for anxiety and depression symptoms in the acute hospital setting (range, 0–21; higher scores indicate more severe symptoms). The GAD-7 assesses the presence and severity of anxiety symptoms (range, 0–21; higher scores indicate more severe symptoms). If patients demonstrated clinically significant symptoms (e.g.: Total IES-R > 22, HADS sub-score > 8, PHQ-8 score > 10, or GAD-7 score > 10), we arranged clinic referrals for them, which included options for free care. In addition, patient demographic data was collected at baseline: age, sex, race, past medical and psychiatric conditions, reasons for ICU admission, hospital diagnosis, length of ICU stay in days, duration of mechanical ventilation, duration of continuous sedation, and type of sedation administered. Our primary outcome was change in total IES-R score from baseline at week 4. Secondary outcomes included: changes in the other measures and IES-R sub-scores at week 4, changes in all measures at week 12, and length of stay (LOS). Moreover, the prevalence of clinically significant PTSD, defined by IES-R total score >22 [16,19,20], was calculated for both groups at all time points.
The recruitment target was n = 100 which accounted for a 10% withdrawal and loss rate, 80% study power, p-value of 0.05, and 8-point clinically significant reduction in post-traumatic stress symptoms via the IES-R [21,22]. Wilcoxon rank sum tests were used to test group differences in continuous variables, Fisher's exact tests were used for categorical variables, and log rank tests were used for time-to-event variables. All data analyses were conducted using SAS 9.4.
3. Results
The screening and enrollment procedures and randomization scheme are summarized in Fig. 1. Enrolled patients who completed baseline follow-up included 11 women and 24 men, with a mean age of 42 (range: 22–65) years old. Chief complaints were varied due to recruitment from both medical and surgical ICUs, and included the following (along with corresponding number of cases): abdominal aortic aneurysm rupture (3), acute heart failure (2), angioedema (1), post-cardiac arrest (1), diabetic ketoacidosis (3), gunshot wounds (5), motor vehicle accident (9), necrotizing fasciitis (1), palliative radiation therapy and oncologic surgery (1), acute respiratory failure (6), and septic shock (3). Control and intervention patients do not show statistically significant differences with respect to age, sex, or baseline IES-R, GADS, PHQ-8, or GAD-7 scores (Table 1 ).
Table 1.
Summary of baseline characteristics of enrolled patients. Baseline psychologic symptom measures are obtained within one week of ICU discharge.
| Control (n = 17) | Intervention (n = 18) | P value | |
|---|---|---|---|
| Percent male [n (%)] | 13 (76.47%) | 11 (61.11%) | 0.327a |
| Age [med (Q1, Q3)], years | 40 (31, 51) | 43 (32, 54) | 0.781b |
| Length of stay [med (Q1, Q3)], days | 9 (5, 24) | 9.5 (7, 16) | 0.338c |
| Duration of mechanical ventilation [med (Q1, Q3)], days | 5 (3, 6) | 5.5 (2, 7) | 0.686c |
| Duration of continuous sedation [med (Q1, Q3)], days | 4 (2, 5) | 4 (2, 5) | 0.945c |
| Sedation with benzodiazepines [n (%)] | 7 (41.18%) | 9 (50.00%) | 0.738a |
| Sedation with dexmedetomidine [n (%)] | 5 (29.41%) | 8 (44.44%) | 0.489a |
| Sedation with Opioids [n (%)] | 16 (94.12%) | 18 (100.00%) | 0.489a |
| Sedation with Propofol [n (%)] | 10 (58.82%) | 10 (55.56%) | 1.000a |
| Baseline psychologic symptom measures | |||
| PHQ-8 [med (Q1, Q3)] | 7 (2,12) | 3.5 (2, 9) | 0.216b |
| GAD 7 [med (Q1, Q3)] | 3 (0, 6) | 4 (1, 10) | 0.467b |
| HADS total [med (Q1, Q3)] | 9 (3,11) | 13 (5, 16) | 0.328b |
| HADS anxiety [med (Q1, Q3)] | 5 (1, 8) | 8.5 (3, 12) | 0.200b |
| HADS depression [med (Q1, Q3)] | 3 (2, 4) | 3 (1, 5) | 0.987b |
| IESR total [med (Q1, Q3)] | 19 (8, 32) | 25 (13, 39) | 0.249b |
| IESR hyperarousal [med (Q1, Q3)] | 5 (3, 8) | 5.5 (1, 10) | 0.987b |
| IESR intrusion [med (Q1, Q3)] | 6 (1,13) | 9.5 (3, 15) | 0.313b |
| IESR avoidance [med (Q1, Q3)] | 4 (0, 8) | 9 (4, 15) | 0.080b |
Fisher's exact test.
Wilcoxon rank sum test.
Log rank test.
25 patients were withdrawn from our study before baseline evaluation, most often due to mortality. Reasons for withdrawal included: death, new-onset strokes, hospital elopement, and loss to follow-up after discharge. These patients were withdrawn within one week of enrollment into the study, and complete baseline data was unable to be obtained on these subjects. Six participants randomized to the control group were subsequently found to have started diaries on their own, effectively crossing over into the intervention group. Five patients randomized to the intervention group never successfully started a diary, thus crossing over into the control group. The results presented below reflect the initial randomization, and key differences with the as-treated analysis will be discussed.
3.1. IES-R outcomes
Changes in IES-R and sub-scores at 4 and 12 weeks can be seen in Table 2 . The use of a diary during the ICU course was associated with a smaller reduction in PTSD symptoms, as measured by the IES-R, compared to the control group (p = 0.035). Participants in the control group also experienced significantly greater improvements in IES-R hyperarousal sub-scores compared to the intervention group at week 4 (p = 0.022). Changes in other sub-scores and scores at week 12 did not differ significantly between groups. When crossovers were accounted for in an as-treated analysis, there was no longer a significant difference in change from baseline total IES-R score at week 4 between groups. However, the change from baseline in hyperarousal sub-score remained significantly better in the control group than the intervention group (p = 0.032).
Table 2.
Change in IES-R total (and its sub-scores) at weeks 4 and 12, compared to baseline (week 1 after discharge).
| Control (n = 17) | Intervention (n = 18) | P valuea | |
|---|---|---|---|
| IESR total week 4 | |||
| Median [Q1, Q3] | −12.5 [−29, −4] | −2 [−5, 4] | 0.035 |
| Missing (n) | 5 | 5 | |
| IESR total week 12 | |||
| Median [Q1, Q3] | −9.5 [−21.5, 14.5] | 19 [−8, 25] | 0.668 |
| Missing (n) | 9 | 13 | |
| IESR hyperarousal week 4 | |||
| Median [Q1, Q3] | −5 [−7.5, −2.5] | 0 [−1, 7] | 0.022 |
| Missing (n) | 5 | 5 | |
| IESR hyperarousal week 12 | |||
| Median [Q1, Q3] | −1.5 [−7.5, 2] | 11 [−1,13] | 0.237 |
| Missing (n) | 9 | 13 | |
| IESR avoidance week 4 | |||
| Median [Q1, Q3] | −1.5 [−12, 2.5] | 0 [−4, 2] | 0.501 |
| Missing (n) | 5 | 5 | |
| IESR avoidance week 12 | |||
| Median [Q1, Q3] | 0 [−6.5, 8.5] | 1 [−8, 4] | 0.943 |
| Missing (n) | 9 | 13 | |
| IESR intrusion week 4 | |||
| Median [Q1, Q3] | −4.5 [−12.5, −2.5] | −1 [−4, 2] | 0.055 |
| Missing (n) | 5 | 5 | |
| IESR intrusion week 12 | |||
| Median [Q1, Q3] | −4.5 [−7.5, 3] | 1 [−3, 8] | 0.522 |
| Missing (n) | 9 | 13 |
Wilcoxon rank sum test.
3.2. Secondary outcome analyses
Changes from baseline in GAD-7, PHQ-8, and HADS-Total score and anxiety and depression sub-scores at weeks 4 and 12 are summarized in Table 3 . We found a statistically significant reduction in depressive symptoms (as measured by the PHQ-8) in the control group, compared to the intervention group, at week 4 (p = 0.049). This difference was not observed in an as-treated analysis, however. Our study finds no other significant difference between groups with respect to these secondary measures.
Table 3.
Change in secondary outcome measures (GAD-7, PHQ-8, HADS-Total/Anxiety/Depression) at weeks 4 and 12, compared to baseline week 1 after discharge. Wilcoxin rank sum test performed. Change in PHQ-8 scores, between groups, at week 4 is statistically significant (p = 0.049).
| Control (n = 17) | Intervention (n = 18) | P valuea | |
|---|---|---|---|
| GAD-7 week 4 | |||
| Median [Q1, Q3] | −1.5 [−4.0, 5.0] | 0.0 [−4.0, 10.0] | 0.437 |
| Missing (n) | 5 | 5 | |
| GAD-7 week 12 | |||
| Median [Q1, Q3] | −0.5 [−5.0, 2.5] | 6.0 [−1.0, 18.0] | 0.396 |
| Missing (n) | 9 | 13 | |
| PHQ-8 week 4 | |||
| Median [Q1, Q3] | −3.5 [−9.0, 0.0] | 1.0 [0.0, 5.0] | 0.049 |
| Missing (n) | 5 | 5 | |
| PHQ-8 week 12 | |||
| Median [Q1, Q3] | −1.5 [−5.5, −1.0] | 6.0 [−3.0, 6.0] | 0.259 |
| Missing (n) | 9 | 13 | |
| HADS total week 4 | |||
| Median [Q1, Q3] | −6.0 [−12.5, 1.5] | 0.0 [−9.0, 4.0] | 0.392 |
| Missing (n) | 5 | 5 | |
| HADS total week 12 | |||
| Median [Q1, Q3] | 2.0 [−3.5, 10.0] | 4.0 [−1.0, 27.0] | 0.566 |
| Missing (n) | 9 | 13 | |
| HADS anxiety week 4 | |||
| Median [Q1, Q3] | −3.0 [−9.0, 1.0] | −1.0 [−9.0, 3.0] | 0.453 |
| Missing (n) | 5 | 5 | |
| HADS anxiety week 12 | |||
| Median [Q1, Q3] | −0.5 [−2.5, 2.5] | 5.0 [−2.0, 13.0] | 0.359 |
| Missing (n) | 9 | 13 | |
| HADS depression week 4 | |||
| Median [Q1, Q3] | −1.0 [−4.0, 1.0] | 1.0 [−2.0, 2.0] | 0.185 |
| Missing (n) | 5 | 5 | |
| HADS depression week 12 | |||
| Median [Q1, Q3] | 0.5 [−1.0, 7.5] | 1.0 [−1.0, 13.0] | 0.720 |
| Missing (n) | 9 | 13 |
Wilcoxon rank sum text.
Length of ICU stay did not significantly differ between diary and control groups (Table 1). However, the diary group trended towards greater length of stay (Supplemental Content, Fig. 4). The diary intervention group was found to have clinically significant PTSD (defined by IESR Total > 22) at week 4 post-ICU discharge. Both diary and control groups showed clinically significant PTSD at weeks 12 and 24 after discharge. The prevalence of clinically significant PTSD in our sample was 36.0% by week 4, and 70.2% by week 12.
4. Discussion
Our analysis indicates that further investigation is warranted before arriving at conclusions regarding the efficacy of diaries in treating ICU-related PTSD symptoms. We found no significant benefit attributable to the intervention, consistent with the results of a 2014 Cochrane Review [23] and a 2019 multicenter randomized control trial [16] studying the use of diaries across ICUs in France. In our sample, the difference in changes of IES-R scores seems to be driven by an effect in the hyperarousal sub-score. This may be due to the particular sample we had, especially given its small size. It may also signal that those with significant hyperarousal have a more severe form of ICU-related PTSD which may prove to be more persistent and possibly treatment-resistant.
Both study groups trended towards worsening, clinically significant PTSD symptoms by 12 weeks after ICU discharge. We must consider the potentially worse psychological outcomes that exist in the treatment as usual ICU survivor cohort, in the absence of psycho-education alone. Our data demonstrates no benefit to ICU-related PTSD with use of an ICU diary, but it does suggest that PICS is a clinically significant phenomenon that merits attention and improved access to care.
4.1. Limitations
Our study has several important limitations. We experienced a significant participant withdrawal rate (42.0%) within one week of patient enrollment, largely due to loss to follow-up and ICU-related morbidity and mortality, which is not uncommon for this study population. Initiating practice habits regarding voluntary clinician use of a diary in a hospital without a prior institutional culture of a diary intervention stymied staff involvement, and momentum to participate in a novel therapy without direct incentive was difficult to generate. We saw inconsistent family investment at the bedside in utilizing the diary, inconsistent participation among clinicians, and little use of the diary among patients after discharge. For instance, 5 patients who were initially randomized to the intervention group never successfully started a diary, due to lack of family presence and failure to recruit healthcare team involvement.
We also note that patients in both study groups received educational pamphlets (as part of their psycho-education), which reviews ICU diaries as treatment (Supplemental Content, 8.2). Therefore, patient and family member awareness of ICU diaries, particularly among control group participants, likely contributed to our study's crossover effect. Several patients' relatives began bedside diaries of their own, and our team did not discourage this process from happening.
ICU diaries are a non-invasive and low-cost intervention, and when adopted by critical care settings, are widely considered to be a way of humanizing an otherwise chaotic, impersonal and sterilized critical care environment. ICU diaries are more common in Europe where some hospital systems routinely offer diaries to critically ill patients [11,13]. Our study endeavored to implement the diaries intervention within a hospital system that was previously not enculturated with the practice of administering ICU diaries, and despite efforts at training nurses and clinicians, some diaries received very little attention from staff. If there was no family at bedside for a patient, the intervention for that individual may have been no better than control, which may have contributed to the lack of significant difference we saw between the two groups in the majority of our secondary outcomes.
In most other clinical trials of ICU diaries, the intervention patients receive their diary one month after ICU discharge [11,24], or close to the day of ICU discharge [16]. These previous studies took place in hospital systems already privy to the use of diaries, and some utilized post-discharge nursing visits and established follow up services to dispense the diaries. During our study, ICU diaries were present at the patient's bedside, for use by healthcare providers and family members, within the first week of ICU admission. Patients were able to begin reading their diaries as soon as they became available for use in their hospital rooms, if so desired. The early introduction of the diary into the intensive care setting sought to promote awareness and utilization of the diary, especially for the contributing writers, in an environment that had not yet experienced this therapeutic modality. However, due to this difference in methodology, many of our study's ICU patients may have still been experiencing periods of delirium or severe illness during their initial encounters with the diary and baseline psychological measures. Additionally, post-discharge support and ongoing direction for use of the diary was limited to the medium of phone interviews, due to our available resources. Therefore, early exposure to the diary intervention, in conjunction with a lack of comprehensive follow-up and guidance for use following discharge, may have resulted in the increase in hyperarousal and total IES-R scores seen at the 4 week follow up.
Other limitations include our small sample size, which likely explain some of our unexpected results, as small studies are at higher risk of selecting non-representative samples. Our study was originally powered for 100 patients to be recruited, which was not achieved during our enrollment period. This may account for the lack of difference between groups at the 12 week follow up.
With regard to baseline psychologic measures, our intervention group does show clinically significant anxiety (HADS-anxiety sub-score > 8) [25] and PTSD symptoms (IESR-R total score > 22), compared to control subjects, within one week of ICU discharge (Table 1). This may be due to the nature of the particular small sample size we had. Therefore, compared to the control arm, our intervention group trends towards more severe PTSD and anxiety symptoms, which are more difficult to treat, and may explain the lack of efficacy of the diary intervention in this cohort. Moreover, those patients with greater anxiety and PTSD symptomatology, in particular avoidance, may be more resistant to utilize the diary in the discharge setting – which entails revisiting the potentially triggering narrative of the illness course and its trauma.
Although a considerable portion of our cohort exhibited hospital delirium and post-intensive care delusional memories, this information was not collected in a standardized manner during our study. This data would have been useful to report and is certainly relevant for our population that showed such a high prevalence of PTSD symptoms. However, our ICU does not have a systematic way of screening patients for delirium, and we chose not to include this additional assessment due to several concerns: lack of sensitivity and specificity with the Confusion Assessment Method (CAM)-ICU score and the time burden on nursing of a more specific measure like the Stanford Proxy Test for Delirium (S-PTD), which would need to be administered at minimum every 12 h [26,27]. Our study team lacked the resources to conduct such frequent evaluations while patients were hospitalized. We chose not to abstract data on the delirium status of patients given the lack of standardization among ICU teams for patient delirium assessments.
In addition, the outcomes we measured do not represent all aspects of wellness. It is likely that diaries have benefit in other ways that we did not capture, particularly as patients and families responded positively to them. Due to loss to follow-up and our specific study design, we were not able to study the long-term effects that may be associated with the diaries. For instance, diaries may be effective tools in outpatient therapy long term, leading to faster recovery, rather than preventing PTSD symptoms. Our study would not be able to demonstrate this. We also suspect that psycho-education alone leads to improved psychologic outcomes compared to a treatment as usual (or no intervention) group, which our study did not include for comparison.
Moreover, we did not look at measures in family members. After an ICU experience, family members comprise such an important support system for patients, and the critical illness course can have detrimental mental health effects on them as well [28]. The ICU diary may have been beneficial for family members and caregivers with regard to certain psychometric outcomes, as shown by Jones et al. [12], and our study did not account for this.
4.2. Barriers to care
Many patients and family members in our study population were hesitant towards interacting with mental health providers, largely due to misconceptions about the role and intentions of psychiatrists. This was mostly observed by our study team in the ICU rooms during the initial process of consenting patients into our study. Multiple patients elicited negative associations, such as forced medications and experimentation, related to the field of mental health. This posed a challenge towards recruitment into our study, along with attempts at bedside education on ICU-related psychological complications. In part, these sentiments likely derive from longstanding mistrust towards healthcare providers (due to historical injustices in the medical field in the southern United States and beyond) and the stigmatization of mental illness [29]. We suspect that underlying mistrust with the mental health care system also affected the willingness of our study participants to present for aftercare.
Moreover, nearly all of our participants were unaware of their risk for PICS that might manifest following an intensive care unit stay when consenting for the study. All of our participants received education on PICS, which was explained as a constellation of psychological, physical, and cognitive impairments that could emerge in the post-recovery setting and persist up to five years after discharge [3]. We also discussed general prevention and treatment strategies, with an emphasis on family support, early rehabilitation, and mental health referrals if indicated. Many of our patients who were interviewed after ICU discharge required prompting to connect their post-traumatic stress symptoms (e.g.: nightmares, flashbacks, delusional memories) to a mental health condition attributable to their ICU course, and many did not recall having been educated about the syndrome while in the ICU. This highlights the importance of following up with patients who survive the ICU to re-educate about psychological morbidity, which is currently not a routine practice at our institution but perhaps should be.
Despite follow-ups by phone, only 10% of our ICU survivors in the study presented for mental health follow-up appointments, which is striking given that almost 70% were reporting impairing symptoms at 12 weeks after discharge.
The onus to direct patients towards resources and follow-up care for ICU-related psychiatric sequela should not be on the patient and the patient's family alone, but should ideally be absorbed by a system designed to prevent and treat PICS. Few Level One Trauma centers in the United States have dedicated PICS clinics and case managers, but the awareness of PICS as an ongoing disabling syndrome appears to be shifting more research and funding resources towards improving care for those who survive critical illness.
As we encounter a growing number of ICU survivors, in particular in the wake of the coronavirus pandemic, clinicians must be equipped to understand the severity and prevalence of significant long-term psychiatric complications of critical illness – in an effort to mitigate ICU-related symptoms and improve the quality of life of ICU survivors [7].
5. Conclusions
Our ICU diary intervention promoted a culture of compassion, collaboration, and humanism among healthcare workers and their critically ill patients and changed the conversation around what can be done, aside from medical care, to improve the psychological health of those who endure and survive the ICU. Despite finding no significant improvement in symptoms with use of the diary, our intervention increased awareness of the psychological support available to ICU survivors and family members. In fact, we suspect there are significant benefits with regard to post-intensive care outcome measures in use of bedside psycho-education, which is not routinely implemented in our healthcare system. The intervention also offered a way for staff in a busy teaching hospital to concretize positive sentiments felt towards patients and offer lasting messages of hope.
Our data demonstrates no benefit in using an ICU diary versus bedside education-alone in reducing PTSD symptoms related to the intensive care stay. While our findings with regard to psychological symptom measures are largely consistent with the available literature [16,23] as a whole, our ICU diary intervention for the critically ill proved to be worthwhile to patients and families, and subjectively aided in the recovery process per the feedback of participants and family members. The prevalence of post-intensive care PTSD was staggering in our population. While some patients were connected with PICS resources and treatment, this remains an area for improvement: how best to connect patients suffering from symptoms of ICU-related PTSD to services?
Consultant-liaison psychiatrists have a potential role to bridge services in hospitals with ICU patients, helping to identify patients at risk for ICU-related PTSD, educating patients and families regarding psychological morbidity of ICU survival, and building networks of outpatient PICS providers for referral. Future research with ICU diaries may demonstrate benefit in hospital systems with established PICS clinics facile in making therapeutic clinical use of these totems from the ICU experience. We suspect the true benefit of ICU diaries is not in simply making them in the first place but in using them for progressive exposure therapy in the outpatient setting.
It remains unclear how diaries may attend to the prevalent and predictive symptoms of delusional traumatic memories, and whether the diaries have the power to replace delusion with factual narrative. Further research is required to assess the clinical utility of the ICU diary in patients who survive the ICU. What is clear from our work is that the psychological needs and PICS symptoms of the ICU survivor post-discharge are chronic and prevalent and merit improved efforts at prevention, education, treatment, and access to care.
Funding
This work was supported by The Arnold P. Gold Foundation, Englewood Cliffs, NJ (grant number GH-17-022).
Author statement
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript. All authors have approved the final version of the manuscript to be published.
George E. Sayde MD, MPH: Conceptualization, Methodology, Investigation, Data Acquisition & Curation, Writing – Original Draft, Writing – Review & Editing, Funding acquisition.
Andrei Stefanescu MS: Statistical Analysis, Data Curation, Writing – Original Draft, Writing – Review & Editing.
Erich Conrad MD, FAPM: Supervision, Writing – Review & Editing.
Nathan Nielsen MD, MSc, FCCM: Supervision, Writing – Review & Editing.
Rachel Hammer MD, MFA: Supervision, Conceptualization, Methodology, Investigation, Data Acquisition, Writing – Original Draft, Writing – Review & Editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.genhosppsych.2020.06.017.
Appendix A. Supplementary data
The supplementary material includes three additional figures, PTSD educational content, and ICU diary instructions used in the study.
References
- 1.Parker A.M., Sricharoenchai T., Raparla S., Schneck K.W., Bienvenu O.J., Needham D.M. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med. 2015;43:1121–1129. doi: 10.1097/CCM.0000000000000882. [DOI] [PubMed] [Google Scholar]
- 2.Wintermann G.B., Brunkhorst F.M., Petrowski K. Stress disorders following prolonged critical illness in survivors of severe sepsis. Crit Care Med. 2015;43:1213–1222. doi: 10.1097/CCM.0000000000000936. [DOI] [PubMed] [Google Scholar]
- 3.Vlake J.H., van Genderen M.E., Schut A. Patients suffering from psychological impairments following critical illness are in need of information. J Intensive Care. 2020;8:6. doi: 10.1186/s40560-019-0422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang S., Mosher C., Perkins A.J. Post-intensive care unit psychiatric comorbidity and quality of life. J Hosp Med. 2017;12:831–835. doi: 10.12788/jhm.2827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Myhren H., Ekeberg O., Toien K., Karlsson S., Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Crit Care. 2010;14:R14. doi: 10.1186/cc8870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Girard T.D., Shintani A.K., Jackson J.C. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care. 2007;11:R28. doi: 10.1186/cc5708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai S.V., Law T.J., Needham D.M. Long-term complications of critical care. Crit Care Med. 2011;39:371–379. doi: 10.1097/CCM.0b013e3181fd66e5. [DOI] [PubMed] [Google Scholar]
- 8.Jones C., Backman C., Capuzzo M., Flaatten H., Rylander C., Griffiths R.D. Precipitants of post-traumatic stress disorder following intensive care: a hypothesis generating study of diversity in care. Intensive Care Med. 2007;33:978–985. doi: 10.1007/s00134-007-0600-8. [DOI] [PubMed] [Google Scholar]
- 9.Jensen J.F., Thomsen T., Overgaard D., Bestle M.H., Christensen D., Egerod I. Impact of follow-up consultations for ICU survivors on post-ICU syndrome: a systematic review and meta-analysis. Intensive Care Med. 2015;41:763–775. doi: 10.1007/s00134-015-3689-1. [DOI] [PubMed] [Google Scholar]
- 10.Davydow D.S., Kohen R., Hough C.L., Tracy J.H., Zatzick D., Katon W.J. A pilot investigation of the association of genetic polymorphisms regulating corticotrophin-releasing hormone with posttraumatic stress and depressive symptoms in medical-surgical intensive care unit survivors. J Crit Care. 2014;29:101–106. doi: 10.1016/j.jcrc.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones C., Backman C., Capuzzo M. Intensive care diaries reduce new onset post traumatic stress disorder following critical illness: a randomised, controlled trial. Crit Care. 2010;14:R168. doi: 10.1186/cc9260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones C., Backman C., Griffiths R.D. Intensive care diaries and relatives' symptoms of posttraumatic stress disorder after critical illness: a pilot study. Am J Crit Care. 2012;21:172–176. doi: 10.4037/ajcc2012569. [DOI] [PubMed] [Google Scholar]
- 13.Knowles R.E., Tarrier N. Evaluation of the effect of prospective patient diaries on emotional well-being in intensive care unit survivors: a randomized controlled trial. Crit Care Med. 2009;37:184–191. doi: 10.1097/CCM.0b013e31819287f7. [DOI] [PubMed] [Google Scholar]
- 14.Jones C., Griffiths R.D., Humphris G., Skirrow P.M. Memory, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Crit Care Med. 2001;29:573–580. doi: 10.1097/00003246-200103000-00019. [DOI] [PubMed] [Google Scholar]
- 15.Karnatovskaia L.V., Johnson M.M., Benzo R.P., Gajic O. The spectrum of psychocognitive morbidity in the critically ill: a review of the literature and call for improvement. J Crit Care. 2015;30:130–137. doi: 10.1016/j.jcrc.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 16.Garrouste-Orgeas M., Flahault C., Vinatier I. Effect of an ICU diary on posttraumatic stress disorder symptoms among patients receiving mechanical ventilation: a randomized clinical trial. JAMA. 2019;322:229–239. doi: 10.1001/jama.2019.9058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergbom I., Svensson C., Berggren E., Kamsula M. Patients' and relatives' opinions and feelings about diaries kept by nurses in an intensive care unit: pilot study. Intensive Crit Care Nurs. 1999;15:185–191. doi: 10.1016/s0964-3397(99)80069-x. [DOI] [PubMed] [Google Scholar]
- 18.Beg M., Scruth E., Liu V. Developing a framework for implementing intensive care unit diaries: a focused review of the literature. Aust Crit Care. 2016;29:224–234. doi: 10.1016/j.aucc.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rash C.J., Coffey S.F., Baschnagel J.S., Drobes D.J., Saladin M.E. Psychometric properties of the IES-R in traumatized substance dependent individuals with and without PTSD. Addict Behav. 2008;33:1039–1047. doi: 10.1016/j.addbeh.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Miranda S., Pochard F., Chaize M. Postintensive care unit psychological burden in patients with chronic obstructive pulmonary disease and informal caregivers: a multicenter study. Crit Care Med. 2011;39:112–118. doi: 10.1097/CCM.0b013e3181feb824. [DOI] [PubMed] [Google Scholar]
- 21.Horowitz M., Wilner N., Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Beck J.G., Grant D.M., Read J.P. The impact of event scale-revised: psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord. 2008;22:187–198. doi: 10.1016/j.janxdis.2007.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ullman A.J., Aitken L.M., Rattray J. Diaries for recovery from critical illness. Cochrane Database Syst Rev. 2014;12:1–37. doi: 10.1002/14651858.CD010468.pub2. Cd010468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kredentser M.S., Blouw M., Marten N. Preventing posttraumatic stress in ICU survivors: a single-center pilot randomized controlled trial of ICU diaries and psychoeducation. Crit Care Med. 2018;46:1914–1922. doi: 10.1097/CCM.0000000000003367. [DOI] [PubMed] [Google Scholar]
- 25.Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 26.Alosaimi F.D., Alghamdi A., Alsuhaibani R. Validation of the Stanford Proxy Test for Delirium (S-PTD) among critical and noncritical patients. J Psychosom Res. 2018;114:8–14. doi: 10.1016/j.jpsychores.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Maldonado J.R., Sher Y.I., Benitez-Lopez M.A. A study of the psychometric properties of the “Stanford Proxy Test for Delirium” (S-PTD): a new screening tool for the detection of delirium. Psychosomatics. 2020;61:116–126. doi: 10.1016/j.psym.2019.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Davidson J.E., Jones C., Bienvenu O.J. Family response to critical illness: postintensive care syndrome-family. Crit Care Med. 2012;40:618–624. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 29.Hussain-Gambles M., Atkin K., Leese B. Why ethnic minority groups are under-represented in clinical trials: a review of the literature. Health Soc Care Community. 2004;12:382–388. doi: 10.1111/j.1365-2524.2004.00507.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The supplementary material includes three additional figures, PTSD educational content, and ICU diary instructions used in the study.