Abstract
Background
The available treatments for frozen shoulder yield variable results. Physical therapy and analgesics are considered as the first-line treatment for this disorder, but the effects are not uniform. There is some evidence to support that alternative medicine may have a role in its management.
Objective(s)
This study was designed to examine the short-term effects of yoga therapy in patients with frozen shoulder of mild to moderate severity.
Materials and methods
A prospective randomized controlled trial was conducted on patients with frozen shoulder between 30 and 60 years of age. They were divided into two groups: yoga (Y) and control (NY). A set of Asana exercises called “Standing Group of Asana” was practiced by the yoga group in addition to the conventional therapy as received by the control group. The patients were reviewed at 1, 2 and 4 weeks. The pain and functional assessment were done at baseline and at each review using the Shoulder Pain and Disability Index (SPADI).
Results
There were 16 male and 20 female participants in the Y group, and 15 males and 21 females in the NY group. There was no statistically significant difference in age, sex, and pre-treatment SPADI score between the groups. At the end of the four weeks, the SPADI pain scores in the Y and NY group were 20.47 and 20.14, respectively (p = 0.666). The SPADI disability scores in the Y and NY group were 20.4 and 19.7, respectively (p = 0.599). Overall SPADI scores were 40.67 and 40.03 in the Y and NY group, respectively (p = 0.736). Both groups had a significant reduction in SPADI pain and disability scores. However, there was no significant difference between the groups in terms of SPADI scores.
Conclusion
The effect of the Standing Group of Asana has no added advantage relative to standard frozen shoulder treatment when practiced for one month.
Keywords: Adhesive capsulitis, Alternative medicine, Frozen shoulder, Standing group of asana, Yoga
1. Introduction
Frozen shoulder (FS) or adhesive capsulitis is a disease of unknown etiology where the glenohumeral joints become painful and stiff because of the loss of joint capsule resilience, possibly with adhesions between its folds [1]. The prevalence ranges from 2 to 5% in general population with a slight preponderance in women [2]. The association is 2–4 times higher in patients with diabetes [1]. In diabetic patients, the risk of involvement of the opposite shoulder also remains high, to an extent of 1 in 5 [3]. Those affected are mainly in the 35–65 age group but the issue can occur in younger people who are involved in repetitive overhead motions in their sports activities, like lawn tennis, basketball, and volley ball [4]. Other predisposing factors include rheumatic disease (gout, rheumatoid arthritis) progression, recent shoulder surgery, thyroid disorders, osteoporosis, Dupuytren's contracture, cardiovascular disease, stroke and parkinsonism [1], [5], [6], [7].
Management of frozen shoulder can be surgical or nonsurgical. Nonsurgical treatment is the first-line therapy, which includes oral anti-inflammatory drugs, physiotherapy, glenohumeral steroid injections, or joint distension and electrotherapy [8], [9], [10]. The existing treatment modalities yield variable results and little evidence exists to support the benefit of one over others.
Yoga has been practiced in India since ancient times and is increasingly being accepted by the Western world. The beneficial effects of medical yoga have been documented in various chronic musculoskeletal diseases [11], [12]. However, there is only one study in reference to yoga and the FS. Kwon et al. who have studied yoga in a small number of middle aged women suffering from FS [13].
The “Standing Group of Asana” (SGA) is a group of stretching postures implemented to promote joint and muscle flexibility [14]. They also promote an increase in stamina and natural positing of joints with a considerable impact on the shoulder joint. Thus, the investigators aim to study the potential benefit of short-term yoga therapy using this group of Asana in a limited number of patients and compare their functional outcomes to the standard treatment. The researchers have hypothesized that this type of yogic posture practiced on a home-based program would reduce pain and disability in this specific condition.
2. Material and methods
A prospective quasi-randomized control trial (RCT) was conducted in our institute between September 2017 and January 2018, where all patients diagnosed with frozen shoulder were evaluated to assess the effects of yoga. The study was conducted by the AYUSH department of a tertiary care center in Eastern India, in collaboration with the Department of Orthopedics and Physical Medicine and Rehabilitation. It was a two-treatment parallel design study with an allocation ratio of 1:1. The study was approved by the institutional ethics clearance committee (T/IM-NF/Ortho/17/12). The patients were recruited after obtaining written consent.
The diagnosis of frozen shoulder was made by the orthopedic surgeons based on shoulder pain and limitation in both active and passive movements of the glenohumeral joint (25% in at least two directions of flexion, abduction, external rotation, internal rotation) [9]. All patients between 30 and 60 years of age with moderate to severe pain and stiffness for six months prior to presentation were included in the study. The standing groups of asana are yogic posture which is difficult to perform in the initial painful period of FS and requires lots of motivation on patient's part especially since they are home based programme. We observed most patients ignore the adjunct therapy (yogic asana) but continue the analgesics. Only after multiple visits, patients realize the importance of yoga and are motivated and willing to adhere to the home based protocol. Six months is optimal for this sensitization and choosing patients who are still clinically painful (phase I). The anteroposterior radiograph of the affected shoulder was performed to rule out other pathology. Patients with prior history of trauma, arthritis (ankylosing spondylitis, psoriatic arthritis, traumatic arthritis, infective arthritis, etc.), bilateral involvement or major psychiatric problems were excluded from the study. Arthritis was ruled on basis of history, prior notes, other joint involvement and also prior doctor notes.
The study involved two arms (Y = Yoga, NY = Non-Yoga/Control) with a quasi-randomization process (consecutive patients coming to Orthopedicoutpatient department were recruited daily until completion) using block technique with 6 blocks of 12 envelopes, each containing equal number of Y and NY patients. The concealment was also ensured through sealed and invisible envelops. The allocation for the group was initially chosen by lottery and the patients followed the same (group) protocol until completion.
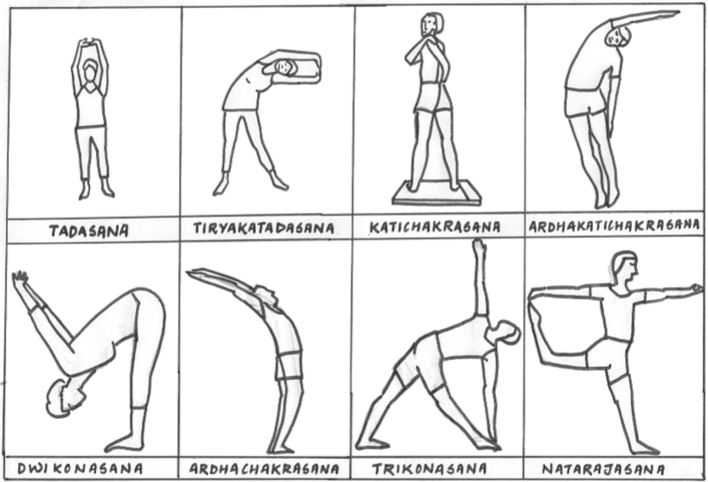
The subjects in the Y group practiced supervised SGA (Table 1) for a period of 30 min as an adjunct therapy to the standard care (NSAIDS and physical therapy). The concept used to develop a specific module of the Standing Group of Asana for frozen shoulder was taken from the reference book titled Asana Pranayama Mudra Bandha authored by Swami Satyananda Saraswati from Bihar School of Yoga that highlights a holistic approach for integral health at physical, mental, emotional, and spiritual levels [14]. Participants were given a diagrammatic instruction to practice the same once daily at home (Fig. 1). The NY group subjects were advised to adhere to the standard care.
Table 1.
Yoga module for Frozen Shoulder.
| S.No. | Asana | Time in min (total = 30) |
|---|---|---|
| 1 | Tadasana | 3.5 |
| 2 | Tiriyakatadasana | 3.5 |
| 3 | Katichakrasana | 3.5 |
| 4 | Trikonasana | 3.5 |
| 5 | Ardhakatichakrasana | 4 |
| 6 | Dwikonasana | 4 |
| 7 | Ardhachakrasana | 4 |
| 8 | Natarajasana | 4 |
Fig. 1.
Diagram depicting the “Standing Group of Asana”.
All subjects in both groups were evaluated at baseline (0) and subsequently, at 1, 2, and 4 weeks for pain and disability using the Shoulder Pain and Disability Index (SPADI) questionnaires filled by the investigator [15]. Patients’ adherence and compliance with the therapy was self-reported.
The sample size was calculated for assuming superiority limit of mean difference 10 with 90% power of the study, 5% significance level, and expected standard deviation 10 for a superiority trail. It was found that the required sample size is 32 in each group. Considering attrition of 10 percent, a total of 36 patients were recruited in each group. Applying the formula of sample size for comparing two means n = (σ12+σ22/k) (z1-α/2 + z1-β/2)/Δ2(n = sample size of Group,σ 1 = standard deviation of Group 1, σ 2 = standard deviation of Group 2, Δ = difference in group means, κ = ratio = n2/n1, Z1-α/2 = two-sided Z value, Z1-β = power = 90%).
The demographic data were analyzed using descriptive statistics. Continuous variables were analyzed using the unpaired t-test among groups and repeated measure ANOVA within the groups. Post-hoc test was applied to compare the mean scores at various time intervals within the group. The data were analyzed using SPSS version 18.0 (PASW) package.
3. Results
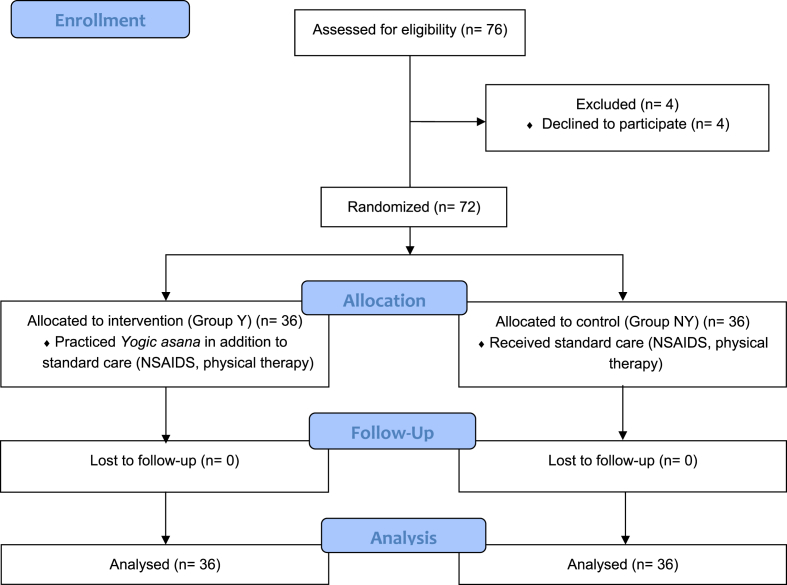
The study involved 72 patients, who were randomly assigned to each group, with 36 in Y and NY each. The study design and patient recruitment strategy are summarized using the CONSORT flow diagram presented in Fig. 2. The two groups were comparable in terms of participants’ demographic characteristics, namely mean age (Y- 49.61 ± 11.27 years, NY- 49.08 ± 11.78 years), sex (male: female in Y-16:20, NY-15:21), and diabetic distribution (male: female in Y-2:3, NY-2:4). The baseline values of the two groups were checked for normal distribution by applying the Kolmogorov–Smirnov test. The pain score of 44.61 (2.32) and 43.94 (2.15) was measured at the time of recruitment for the Y and NY group, respectively, while the corresponding disability scores were 63.53 (4.04) and 61.97 (4.10). Further analyses confirmed that the differences in pain score, disability score, and total SPADI score between the groups at the time of recruitment were not statistically significant. The total SPADI score in each arm was assessed for normality by using Shapiro–Wilk test, focusing on the skewness and kurtosis values.
Fig. 2.
CONSORT diagrams depicting patient recruitment.
At the end of the 4-week study period, the pain score in the Y and NY group was 20.47 (3.37) and 20.14 (3.15), respectively (p = 0.666), whereas the corresponding disability scores were 20.4 (5.84) and 19.7 (5.31) (p = 0.599). However, the difference in the total SPADI scores of the two groups was not statistically significant (40.67 vs. 40.03, p = 0.736). In both groups, the incremental gain in terms of pain and disability reduction was statistically significant (p < 0.05), based on the findings of repeated measure analysis of variance. However, when the scores of the two groups were compared, their difference was not statistically significant, as shown in Table 2. After applying mixed model design (split ANOVA), the difference between the groups were non-significant as shown (Table 3) None of the patients in either group developed any problem/complications.
Table 2.
Pain and disability assessment in both groups after intervention using Repeated measures ANOVA.
| Variables | Standard treatment with yoga (Y) |
Standard treatment (NY) |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| SPADI Pain Score | ||
| Baseline | 44.61 ± 2.32 | 43.94 ± 2.15 |
| Week 1 | 39.42 ± 2.23 | 38.83 ± 1.95 |
| Week 2 | 33.28 ± 3.13 | 32.69 ± 2.62 |
| Week 4 | 20.47 ± 3.37 | 20.14 ± 3.15 |
| SPADI Disability Score | ||
| Baseline | 63.53 ± 4.04 | 61.97 ± 4.10 |
| Week 1 | 52.94 ± 6.1 | 52.92 ± 5.8 |
| Week 2 | 41.75 ± 6.31 | 40.36 ± 5.78 |
| Week 4 | 20.4 ± 5.84 | 19.7 ± 5.31 |
| SPADI Total Score | ||
| Baseline | 107.69 ± 5.18 | 105.78 ± 5.43 |
| Week 1 | 91.78 ± 6.62 | 91.97 ± 6.73 |
| Week 2 | 74.69 ± 7.34 | 73.25 ± 7.55 |
| Week 4 | 40.67 ± 8.10 | 40.03 ± 7.89 |
P value (Repeated measure ANOVA) is 0.0001.
Table 3.
Split ANOVA test to compare the mean scores at various time intervals within the group.
| Group | Mean ± Std. Deviation | F Test mixed model design | P Value | |
|---|---|---|---|---|
| Pain 0 | Non Yoga | 43.94 ± 2.151 | 0.125 | 0.946 |
| Yoga | 44.61 ± 2.321 | |||
| Total | 44.28 ± 2.247 | |||
| Pain 1 week | Non Yoga | 38.83 ± 1.949 | ||
| Yoga | 39.42 ± 2.234 | |||
| Total | 39.13 ± 2.103 | |||
| Pain 2 weeks | Non Yoga | 32.69 ± 2.617 | ||
| Yoga | 33.28 ± 3.132 | |||
| Total | 32.99 ± 2.880 | |||
| Pain 4 weeks | Non Yoga | 20.14 ± 3.146 | ||
| Yoga | 20.47 ± 3.376 | |||
| Total | 20.31 ± 3.244 | |||
| Disability –0 | Non Yoga | 61.97 ± 4.102 | 0.745 | 0.526 |
| Yoga | 63.53 ± 4.046 | |||
| Total | 62.75 ± 4.121 | |||
| Disability –1 week | Non Yoga | 52.92 ± 5.789 | ||
| Yoga | 52.94 ± 6.090 | |||
| Total | 52.93 ± 5.899 | |||
| Disability – 2 weeks | Non Yoga | 40.36 ± 5.778 | ||
| Yoga | 41.75 ± 6.308 | |||
| Total | 41.06 ± 6.047 | |||
| Disability – 4 weeks | Non Yoga | 19.69 ± 5.307 | ||
| Yoga | 20.39 ± 5.842 | |||
| Total | 20.04 ± 5.552 | |||
| SPADI total –0 | Non Yoga | 105.78 ± 5.436 | 0.787 | 0.474 |
| Yoga | 107.69 ± 5.181 | |||
| Total | 106.74 ± 5.360 | |||
| SPADI total – 1 week | Non Yoga | 91.97 ± 6.729 | ||
| Yoga | 91.78 ± 6.625 | |||
| Total | 91.88 ± 6.631 | |||
| SPADI total – 2 weeks | Non Yoga | 73.25 ± 7.557 | ||
| Yoga | 74.69 ± 7.344 | |||
| Total | 73.97 ± 7.434 | |||
| SPADI total – 4 weeks | Non Yoga | 40.03 ± 7.898 | ||
| Yoga | 40.67 ± 8.103 | |||
| Total | 40.35 ± 7.951 | |||
4. Discussion
The FS remains one of the common musculoskeletal problems among patients presenting to orthopaedic clinics. The pain can be sometimes severe enough to disturb the patient's sleep [8]. The natural course of the disease has three clinical stages:- the freezing stage, the frozen stage, and thawing stage [16]. The freezing stage usually lasts for 2–9 months with moderate to severe shoulder pain and stiffness. In the frozen stage, the stiffness increases and pain reduces which lasts for about 4–14 months. The thawing stage continues for the next 5–24 months, wherein the pain subsides and the range of motion (ROM) recovers. All forms of treatment aim to cut short the natural course of the disease.
Recent research has shown that yogic practices positively impact the body in many ways. Unlike the exercises which yield physical benefit, yoga seems to be able to improve body awareness, pain acceptance, and coping [11]. Healthy persons practicing yoga have been found to have better body and mind coordination, anxiety control, breath control, and improved body flexibility [17]. The expansion of its use has given birth to the term “medical yoga” wherein the art and science of yoga is practiced for the prevention and potential treatment of different medical conditions [17].
In multiple studies, yoga has been found to decrease inflammatory markers [18], [19]. The beneficial effect has been documented when yoga is practiced as an additional therapy for people suffering from for back and neck pain [11], [12]. Specific asanas (yoga practices) help in correcting the vertebral curvature, strengthening the thoracic and abdominal cavities, along with supporting respiratory muscles, thus overall improving the posture [20]. In 2015, Moonaz et al. conducted a large trial on rheumatoid and osteoarthritis patients to examine the safety, efficacy, and feasibility of yoga for sedentary patients [21]. After eight weeks of intervention, they observed significant improvements were seen in physical pain, general health, vitality, ability to carry out Activities of Daily Living (ADLs), along with balance, upper body strength and mental health scales (p < 0.05). Interestingly the researchers found that almost all benefits were still observable even after nine months of study completion.
The data on the effect of yoga in the FS is however limited. We hypothesized that yogic asanas will help the patients recover from the FS by increasing flexibility and strengthening muscles via more holistic approach rather than simply managing shoulder pain. The SGA is a group of stretching postures implemented for the treatment of FS. Stretching of the muscles involve the fullest elongation of fibers and improves the muscle's elasticity and reaffirms the comfortable tone. This results in a feeling of improved flexibility, muscle control, and range of motion (ROM). Stretching is also used therapeutically to alleviate cramps. Sleeper Stretches are specific shoulder stretch exercise done in lying down posture that is done to increase shoulder range of motion and flexibility. These are delicate exercises aimed to stretch the back of shoulder and overdoing or doing it wrongly can be harmful like injury to posterior capsule, instability and impingement [22]. Sharma et al. compared sleeper stretches group (n = 20) with yoga group (n = 20) and found that the latter group had better internal rotation and pain reduction than the former [23]. As no patient in either group had received any other treatment in the form of analgesics/physical therapy, the difference was likely attributable to yoga practice. In the present study, reduction over time in the SPADI pain and disability scores was noted in both groups, but the difference between the Y and NY group was not statistically significant. In a study related to acute sleeper stretches in range of movement of the shoulder, Kevin et al. found an improvement in the internal rotation but was not statistically significant [22]. Similarly, Sule et al. compared the conventional treatment group to the sleeper stretches group (sleeper stretches as adjunct therapy to conventional treatment) and realised that while the two groups had some improvement in flexion and extension, the changes in their respective SPADI scores were not statistically significant [24]. The authors attributed the improvement in both groups to the conventional therapy, which was the case in the present study (with both groups having “standard therapy”). In a recent 12-week study comparing middle-aged women practicing yoga (n = 8) with controls (n = 8), Kwon et al. reported decreased SPADI scores and a significant increase in the shoulder pressure threshold, namely in subscapularis and teres minor muscles. It is possible that these beneficial results were obtained due to the greater study duration (50 min for 12 weeks, compared to 30 min for 4 weeks adopted in the present study) [13].
When interpreting the findings reported here, it is important to acknowledge certain limitations to our study. Specifically, our investigations involved a small group of patents and the follow-up period was short (4 weeks only). Given that the natural course of frozen shoulder passes through different stages and at various time intervals, we had purposely selected the group in the initial freezing phase (Phase 1) to minimize the selection bias. However, as the freezing phase is the most resistant to intervention, this may have masked the expected benefits, which could have potentially been more pronounced in the frozen and thawing phases. The experimental group's compliance with the recommended treatment was self-reported, likely introducing an element of social bias to the data and thus adversely affecting the reliability of the final outcome. In yoga, strict adherence to practice is intrinsic to its efficacy. Even with multiple treatment strategies for FS, none seem to work with certitude [25]. Another shortcoming of the present study is that patient perspectives were not evaluated while assessing the treatment effectiveness. They appear bifurcated either as ‘pain predominant’ or as ‘stiffness predominant’. The ideal treatment should consider exploring the experiences and perceptions of people along with the amelioration of anxiety and other living conditions and their priorities for treatment [26], [27]. Nevertheless, no adverse effect was noted. The study conducted by Cramer et al. focusing on neck pain or Sharma et al. in frozen shoulder also showed no serious adverse events of practicing yoga [11], [23]. Hence, this opens up a new horizon for the researchers and directs the future studies to evaluate further on the outcome of yoga as an adjunct therapy.
5. Conclusion
Based on our findings, we conclude that the effect of the “Standing Group of Asana” yogic practices undertaken for a short duration of four weeks on home-based program has no added benefit relative to the standard treatment in the management of frozen shoulder. However, no adverse effects were observed during the intervention period.
Disclaimer
CTRI registration was attempted retrospectively but change of rules did not allow this. It is compulsory to register all trials with the CTRI.
Sources of funding
None.
Conflict of interest
None.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Manske R.C., Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1:180–189. doi: 10.1007/s12178-008-9031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morén-Hybbinette I., Moritz U.S.B. The clinical picture of the painful diabetic shoulder--natural history, social consequences and analysis of concomitant hand syndrome. Acta Med Scand. 1987;221:73–82. doi: 10.1111/j.0954-6820.1987.tb01247.x. [DOI] [PubMed] [Google Scholar]
- 3.Bunker T.D. Frozen shoulder: unravelling the enigma. Ann R Coll Surg Engl. 1997;79:210–213. [PMC free article] [PubMed] [Google Scholar]
- 4.Kugler A. Muscular imbalance and shoulder pain in volleyball attackers. Br J Sports Med. 1996;30:256–259. doi: 10.1136/bjsm.30.3.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith S., Devaraj V., Bunker T. The association between frozen shoulder and Dupuytren's disease. J Shoulder Elbow Surg. 2001;10:149–151. doi: 10.1067/mse.2001.112883. [DOI] [PubMed] [Google Scholar]
- 6.Boyle-Walker K.L., Gabard D.L., Bietsch E.M.V., RB A profile of patients with adhesive capsulitis. J Hand Ther. 1997;10:9268913. doi: 10.1016/s0894-1130(97)80025-7. [DOI] [PubMed] [Google Scholar]
- 7.Riley D., Lang A.E., Blair R.D.G., Birnbaum A., Reid B. Frozen shoulder and other shoulder disturbances in Parkinson ’ s disease. J Neurol Neurosurg Psychiatry. 1989;52:63–66. doi: 10.1136/jnnp.52.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bateman M., McClymont S., Hinchliffe S. The effectiveness and cost of corticosteroid injection and physiotherapy in the treatment of frozen shoulder-a single-centre service evaluation. Clin Rheumatol. 2014;33:1005–1008. doi: 10.1007/s10067-014-2501-x. [DOI] [PubMed] [Google Scholar]
- 9.Arai Y., Shimo K., Inoue M., Sakurai H., Ohmichi Y., Matsubara T. Integration of a kampo medicine , nijutsuto , and western medical treatment in the treatment of long-term frozen shoulder refractory to western medical Treatment : a case series. J Evid Based Complement Altern Med. 2015;20:157–161. doi: 10.1177/2156587214568346. [DOI] [PubMed] [Google Scholar]
- 10.Baig M., Baig U., Naseem A. Pain modulation in frozen shoulder –Electrotherapy versus exercise therapy. Ann King Edward Med. 2011;17:245–250. [Google Scholar]
- 11.Cramer H., Lauche R., Hohmann C., Lüdtke R., Haller H., Michalsen A. Randomized-controlled trial comparing yoga and home-based exercise for chronic neck pain. Clin J Pain. 2013;29:216–223. doi: 10.1097/AJP.0b013e318251026c. [DOI] [PubMed] [Google Scholar]
- 12.Manik R., Mahapatra A., Gartia R., Bansal S., Patnaik A. Effect of selected yogic practices on pain and disability in patients with lumbar spondylitis. Int J Yoga. 2017;10:81–87. doi: 10.4103/0973-6131.205516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kwon I., Oh J., Kim T. Effects of 12 Weeks of yoga program in middle aged women with frozen shoulder. Med Sci Sports Exerc. 2018;1:242–243. [Google Scholar]
- 14.Satyananda S. Gyan Darshan; 2000. Asana Pranayama Mudra Bandha. Munger, Bihar. [Google Scholar]
- 15.Roach K., Budiman-Mak E., Songsiridej N., Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res. 1991;4:143–149. [PubMed] [Google Scholar]
- 16.Reeves B. The natural history of the frozen shoulder. Scand J Rheumatol. 2018;4:1198072. doi: 10.3109/03009747509165255. [DOI] [PubMed] [Google Scholar]
- 17.Stephens I. Medical yoga therapy. Children. 2017;4:1–20. [Google Scholar]
- 18.Vijayaraghava A., Doreswamy V., Narasipur O.S., Kunnavil R., Srinivasamurthy N. Effect of yoga practice on levels of inflammatory markers after moderate and strenuous exercise. J Clin Diagn Res. 2015;9:CC08–CC12. doi: 10.7860/JCDR/2015/12851.6021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nagarathna R., Ram A., Banerjee B., Hosakote V., Rao R. Comparison of lymphocyte apoptotic index and qualitative DNA damage in yoga practitioners and breast cancer patients: a pilot study. Int J Yoga. 2013;6:20–25. doi: 10.4103/0973-6131.105938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross A., Friedmann E., Bevans M., Thomas S. National survey of yoga practitioners: mental and physical health benefits. Complement Ther Med. 2013;21:313–323. doi: 10.1016/j.ctim.2013.04.001. National. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moonaz S., Bingham C., Wissow L., Bartlett S. Yoga in sedentary adults with arthritis: effects of a randomized controlled pragmatic trial. J Rheumatol. 2015;42:1194–1202. doi: 10.3899/jrheum.141129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kevin L., Sipes C., Wilson T. The acute effect of sleeper stretch on shoulder range of motion. J Athl Train. 2008;43:359–363. doi: 10.4085/1062-6050-43.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma N., Chauhan S.K., Kumar A. Effect of yogic asana on Adhesive capsulitis ( frozen shoulder ) to increasing the internal rotation. Int J Phys E Ducation, Sport Heal. 2016;3:192–195. [Google Scholar]
- 24.Sule K., Rathi M., Palekar, Tushar J., Anwer S. Comparison of conventional therapy versus sleeper stretch with conventional therapy in adhesive capsulitis. Int J Health Sci Res. 2015;5:186–192. [Google Scholar]
- 25.Maund E., Craig D., Suekarran S., Neilson A., Wright K., Brealey S. Management of frozen shoulder: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2012;16:1–264. doi: 10.3310/hta16110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanchard N.C.A., Goodchild L., Thompson J., O'Brien T., Davison D., Richardson C. Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of contracted (frozen) shoulder: quick reference summary. Physiotherapy. 2012;98:118–121. doi: 10.1016/j.physio.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 27.Jones S., Hanchard N., Hamilton S., Rangan A. A qualitative study of patients' perceptions and priorities when living with primary frozen shoulder. BMJ Open. 2013;3:1–13. doi: 10.1136/bmjopen-2013-003452. [DOI] [PMC free article] [PubMed] [Google Scholar]