Abstract
Background
Anterior mediastinal tumours account for 50% of all mediastinal masses. Surgical intervention is the standard approach for their diagnosis or treatment. Minimally invasive techniques have gained significant popularity in the last few decades due to the obvious advantages that they offer. We will describe a series composed of the first 20 patients who were submitted to a new minimally invasive video-assisted technique, which uses an inframammary incision approach involving a Thoratrak rib spreader and a Rultract Skyhook retractor.
Methods
A retrospective study was undertaken, involving all the patients in our department who were submitted to a resection of their anterior mediastinal masses by inframammary incision, using a Thoratrak rib spreader, a Rultract Skyhook retractor and video assistance.
Results
A total of 20 patients were included, with a mean age of 52.6. The mean surgery duration was 47 minutes, with an intraoperative blood loss of 70 mL. The mean period of hospitalisation was 2.9 days. No patients underwent conversion to open surgery, and there were no major complications. The mean size of the masses that were excised was 13.9 cm, with a mean weight of 77.3 g. The surgical margins were all free of tumour tissue, and no early recurrence was observed during the postoperative follow-up period.
Conclusions
Video-assisted thoracoscopic surgery (VATS) and robot assisted thoracic surgery (RATS) account for most of the minimally invasive procedures. However, VATS has certain limitations in terms of deep perception and manoeuvrability, and RATS has the disadvantage of lacking tactile and force feedback for the surgeon. The inframammary technique allows for safe direct dissection around the vascular and nervous structures, ensuring a complete observation of the anterior mediastinum and its structures. The findings in the present study suggest that this technique is useful. We had good surgical results, short surgery times and very low blood loss, and all tumours were totally resected, with tumour-free surgical margins. The size and the right lateralisation of the mass did not present any contraindications, and the learning curve and investment were minimal. In conclusion, the inframammary approach could be a safe and useful approach for treating anterior mediastinal pathology.
Keywords: Mediastinal tumours, mini-invasive surgery, inframammary incision, thymoma, myasthenia gravis
Introduction
The mediastinum is small space that contains key structures such as major vessels and the heart (1). Mediastinal tumours represent 3% of all tumours seen within the chest (2), and anterior mediastinal tumours account for 50% of all mediastinal masses, including thymoma, teratoma, thyroid disease and lymphoma (3).
Surgical intervention is the standard approach for the diagnosis or treatment of mediastinal tumours (4). Improved techniques and technologies have made minimally invasive approaches increasingly popular over the last two decades. When compared to conventional surgery, minimally invasive techniques are associated with reduced postoperative pain, morbidity and hospitalisation days and a faster return to active life (5,6).
Several techniques and variations have been reported, each with specific advantages and disadvantages, but the struggle for the perfect approach remains. We will describe a series composed of the first 20 patients submitted to undergo a new video-assisted technique utilising an inframammary incision and employing a Thoratrak rib spreader (Medtronic, Inc., Minneapolis, Minn) and a Rultract Skyhook retractor (Rultract Inc., Cleveland, Ohio, USA).
Methods
This is a retrospective study of all the patients submitted for the resection of their anterior mediastinal masses by inframammary incision, using a Thoratrak rib spreader, a Rultract Skyhook retractor and video assistance.
Between June 1st, 2017 and July 1st, 2019, 20 patients underwent the resection of their mediastinal masses through this mini-invasive approach. The diagnostic workup for all patients included a clinical examination, full haematological investigations, posteroanterior and lateral chest radiographs, a chest CT scan and, in some cases, an MRI.
Endotracheal intubation was performed using a double lumen tube, to allow for left lung exclusion. All patients were placed in a supine position, with the arms along the body and the left half-body elevated between 15–30º.
An incision of approximately 5 cm was made in the left inframammary line, in the 4th or 5th intercostal space (Figure 1). An additional port for a 30° camera was used at the anterior axillary line in the same intercostal space. We used the Thoratrak rib spreader fitted to the Rultract Skyhook retractor to expose the anterior mediastinum (Figure 2).
Figure 1.

Surgical incision in the left inframammary line, in the 4th or 5th intercostal space.
Figure 2.

Thoratrak fitted to the Rultract Skyhook retractor to expose the anterior mediastinum.
Dissection was performed using endoscopic instruments. A thoracic drain was let through the port of the camera in all the patients (Figure 3), and the patients were awakened and extubated in the operation room.
Figure 3.

Final incision, with the thoracic drain left through the port of the camera.
Results
From June 1st, 2017 to July 1st, 2019, the patients with anterior mediastinal masses who were submitted for resection through mini-invasive surgery were studied and analysed. The preoperative characteristics of this group of patients are shown in Table 1. A total of 20 patients, including 9 males and 11 females, were involved. Their ages ranged from 21 to 72, with a mean age of 52.6. The mean BMI was 26. In total, 35% of the patients had myasthenia gravis.
Table 1. Preoperative characteristics of the group of patients submitted to anterior mediastinal masses resection through mini-invasive surgery.
| Variable | Number (n=20) |
|---|---|
| Gender (male/female) (n) | 9/11 |
| Age (y) | 52.6±15.6 |
| BMI | 26 |
| MG (n) | 7 |
y, years; BMI, body mass index; MG, myasthenia gravis.
The surgical outcomes are shown in Table 2. The mean duration of the surgery was 47 minutes, and the mean volume of intraoperative blood loss was 70 mL. Total thymectomy was performed in all the procedures. In one patient, the resection of the mass was combined with pericardium and lung resection, due to focal invasion.
Table 2. Surgical outcomes of the patients submitted to anterior mediastinal masses resection through mini-invasive surgery.
| Variable | Number (n=20) |
|---|---|
| Duration of surgery (min) | 47±6.3 |
| Blood loss (mL) | 70±28.3 |
| Postoperative pleural drainage (mL) | 168±216.2 |
| Postoperative UCI stay (days) | 0.8±0.1 |
| Postoperative hospital stay (days) | 2.9±1.2 |
| Converted to open surgery (n) | 0 |
| Blood transfusion (n) | 0 |
| Surgical complications (n) | 0 |
| Postoperative complications (n) | 1 |
The mean postoperative intensive care unit stay was 0.8 days, and the mean total period of hospitalisation was 2.9 days. No patient needed blood products, and the chest tubes were removed when the drainage output volume declined to <100 mL in a 24 h period. The mean postoperative pleural drainage volume was 168 mL.
No patient underwent the conversion to open surgery. There were no surgical complications in the postoperative days. One patient had an episode of atrial fibrillation, which was controlled with oral medication after clinical and echocardiographic assessment.
All the patients were discharged home with their pain controlled through an oral analgesic. In the one-month follow-up, all the patients had already returned to active life. One patient required thoracentesis due to asymptomatic pleural effusion, as shown in the thoracic X-ray, which was compatible with transudate and did not require hospitalisation.
The mean size of the masses excised was 13.9 cm (3–35 cm), with a mean weight of 77.3 g (24–168 g) (Figure 4). The pathology of the tumours is shown in Table 3. Overall, 35% were thymomas, 30% were thymic hyperplasia, 20% were simple thymic cysts, 5% were bronchogenic cysts, 5% were lipoma and 5% were pericardium cysts.
Figure 4.
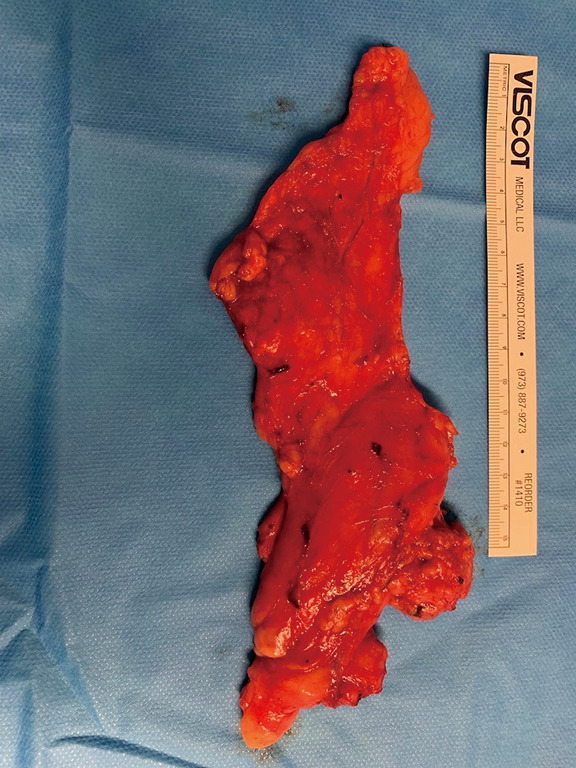
One of the masses surgically excised.
Table 3. Characteristics and pathological diagnoses of the resected masses.
| Variable | Number (n=20) |
|---|---|
| Mass size (cm) | 13.9±8.0 |
| Mass weight (g) | 77.3±47.4 |
| Thymomas (%) | 35 |
| Thymic hyperplasia (%) | 30 |
| Simple thymic cyst (%) | 5 |
| Bronchogenic cyst (%) | 5 |
| Lipoma (%) | 5 |
| Pericardium cyst (%) | 5 |
In patients with thymoma, 71% required radiotherapy as adjuvant therapy. The patients were able to receive this treatment one month after the surgery. According to the Masaoka-Koga stage classification, the thymomas were classified into the following stages: I (29%), II (43%), III (14%) and IV (14%). The surgical margins were free of tumour tissue in all the patients. No early recurrence was observed during the postoperative follow-up period.
Discussion
Minimally invasive techniques allow for a shorter postoperative hospital stay, lower perioperative complications, faster recovery and better cosmetic results than the classical sternal approach. Nowadays, video-assisted thoracoscopic surgery (VATS) and robot assisted thoracic surgery (RATS) account for most of the procedures, even though the perfect approach remains to be set, mainly due to the space restrictions of the anterior mediastinum.
VATS has obvious limitations in terms of deep perception and manoeuvrability, which dissuades its use for anterior mediastinum lesions (6,7) and RATS, although it offers excellent 3D visualisation of structures and the use of articulating instruments. It is also associated with high acquisition and maintenance costs, plus the necessary training and extensive learning curve. Additionally, another disadvantage of RATS is the lack of tactile and force feedback for the surgeon (8). Both have limits for mass size and use carbon dioxide insulation to widen the working space, the impact of which on the cardiopulmonary system is still controversial.
When compared with VATS or RATS, the inframammary technique using the Thoratrak rib spreader and Rultract Skyhook retractor allows for safe direct dissection around the vascular and nervous structures, ensuring complete observation of the anterior mediastinum and its structures. The use of an auxiliary camera allows for better visualisation of the most cephalic area of the mediastinum and for a cervical extension if necessary.
Some previous studies with VATS thymectomy have described the weight of the resected samples with values ranging from 59.6 to 72.5 g (9). In our study, the mean weight of the resected tissue was 77.2 g, suggesting that our technique apparently is not inferior to the other lateral approaches. The size and right lateralisation of the mass are not contraindications for its use, since the complete anterior phrenic and even the cervical area can be easily addressed. The only contraindication seems to be the invasion of major vessels (innominate vein not included).
Although no numeric data regarding postoperative pain were obtained, since there was no actual rib spread but instead an anterior displacement of the upper rib, its level was certainly low, as was the impact on respiratory function. These aspects justify the reduced hospital stay period (2.9 days), with pain controlled only through oral non-opioid analgesics.
The learning curve and investment are minimal, especially if this device is already implemented in other procedures, such as mini-invasive coronary grafting.
Conclusions
In conclusion, inframammary approach seems to be a safe and useful approach for treating anterior mediastinal pathology. The findings in the present study suggest the usefulness of thymectomy via the inframammary approach for anterior mediastinal tumours. We had good surgical results, with short surgery times and very low blood loss, with no patient needing transfusional support. All the tumours were totally resected, with tumour free surgical margins.
Our study has several limitations, including its small sample size, short follow-up and retrospective nature.
Future investigations with more patients and a longer follow-up will be required to confirm the oncological outcomes of this new technique.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethics Committee of Hospital de Santa Maria, Lisbon (No. 391/19). Written consent was obtained from the patient for publication of this case and the accompanying images.
Footnotes
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-19-3310b). The authors have no conflicts of interest to declare.
References
- 1.Vohra A, Narula H, Bindra G. Spectrum of CT findings in posterior mediastinal masses. Int J Adv Res 2016;4:546-56. 10.21474/IJAR01/162 [DOI] [Google Scholar]
- 2.Junqueira N, Ferreira R, Sena A, et al. An alternative approach for addressing mediastinal tumours through mini-invasive surgery. Int J Surg Case Rep 2018;42:158-60. 10.1016/j.ijscr.2017.11.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tomiyamaa N, Hondaa O, Tsubamoto M, et al. Anterior mediastinal tumors: Diagnostic accuracy of CT and MRI. Eur J Radiol 2009;69:280-8. 10.1016/j.ejrad.2007.10.002 [DOI] [PubMed] [Google Scholar]
- 4.Stremmel C, Passlick B. Surgery of mediastinal tumors. Chirurg 2008;79:9-10, 12-7. 10.1007/s00104-007-1438-x [DOI] [PubMed] [Google Scholar]
- 5.Cheng YJ, Wu HH, Chou SH, et al. Video-assisted thoracoscopic management of mediastinal tumors. JSLS 2001;5:241-4. [PMC free article] [PubMed] [Google Scholar]
- 6.Melfi FM, Fanucchi O, Mussi A. Minimally invasive mediastinal surgery. Ann Cardiothorac Surg 2016;5:10-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Radkani P, Joshi D, Barot T, et al. Robotic video-assisted thoracoscopy: minimally invasive approach for management of mediastinal tumors. J Robot Surg 2018;12:75-9. 10.1007/s11701-017-0692-2 [DOI] [PubMed] [Google Scholar]
- 8.Morris B. Robotic surgery: applications, limitations, and impact on surgical education. MedGenMed 2005;7:72. [PMC free article] [PubMed] [Google Scholar]
- 9.Numanami H, Yano M, Yamaji M, et al. Thoracoscopic Thymectomy Using a Subxiphoid Approach for Anterior Mediastinal Tumors. Ann Thorac Cardiovasc Surg 2018;24:65-72. 10.5761/atcs.oa.17-00128 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as


