Abstract
Background
Low-dose computed tomography (LDCT) scan for lung cancer screening is underutilized. Studies suggest that up to one-third of providers do not know the current lung cancer screening guidelines. Thus, identifying the barriers to utilization of LDCT scan is essential.
Methods
Primary care providers in three different healthcare settings in the United States were surveyed to assess provider knowledge of LDCT scan screening criteria, lung cancer screening practices, and barriers to the utilization of LDCT scan screening. Fisher’s Exact, Chi-Squared, and Kruskal-Wallis tests were used to compare provider responses. Multivariable logistic regression was used to test the association between provider characteristics and the likelihood of utilizing LDCT scan for lung cancer screening.
Results
The survey was sent to 614 providers, with a 15.7% response rate. Overall, 29.2% of providers report never ordering LDCT scans for eligible patients. Providers practicing at a community or academic hospital more frequently order LDCT scans than those practicing at a safety net hospital. Academic- and community-based providers received a significantly higher mean knowledge score than safety net-based providers [academic 6.84 (SD 1.33), community 6.72 (SD 1.46), safety net 5.85 (SD 1.38); P<0.01]. Overall, only 6.2% of respondents correctly identified all six Centers for Medicare and Medicaid Services eligibility criteria when challenged with three incorrect criteria. Common barriers to utilization of LDCT scan included failure of the electronic medical record (EMR) to notify providers of eligible patients (54.7%), patient refusal (37%), perceived high false-positive rate leading to unnecessary procedures (18.9%), provider time constraints (16.8%), and lack of insurance coverage (13.7%).
Conclusions
Provider knowledge of lung cancer screening guidelines varies, perhaps contributing to underutilization of LDCT scan for lung cancer screening. Improved provider education at safety net hospitals and improving EMR-based best practice alerts may improve the rate of lung cancer screening.
Keywords: Lung cancer, screening, CT scan
Introduction
Lung cancer is the leading cause of cancer-related death in both men and women in the United States, accounting for nearly one-quarter of all cancer mortality (1). The 5-year survival rate for lung cancer is low because 79% of lung cancers are diagnosed as regional or distant disease (2). Thus, routine implementation of a screening test that effectively detects lung cancer at an early stage is paramount. Screening with chest x-ray has not been shown to reduce lung cancer mortality (3). In 2011, the National Lung Screening Trial (NLST) reported a 20% reduction in cancer-related mortality with low-dose computed tomography (LDCT) scan compared to chest radiography (4). Subsequently, the United States Preventive Services Task Force (USPSTF), the American Cancer Society (ACS), the National Comprehensive Cancer Network (NCCN) and several other professional societies made recommendations for annual LDCT scan for lung cancer screening in high-risk patients (5-10). Accordingly, in 2015 the Centers for Medicare and Medicaid Services (CMS) approved coverage for LDCT scan screening for high-risk Medicare beneficiaries (11).
Despite broad support amongst multiple professional societies and analyses demonstrating a smaller number needed to screen to save a life compared to mammography and colonoscopy combined, utilization of LDCT scan for lung cancer screening has been limited (12). Since the release of the NLST findings in 2011, the rate of LDCT has only increased by 0.6% (13). The underutilization of LDCT scan by primary care providers for lung cancer screening may be due in part to concerns raised by the American Academy of Family Physicians (AAFP) (14), providers’ unfamiliarity with the indications, risks and benefits of screening with LDCT scan, or regional variation due to the distribution of approved lung cancer registry sites (15). To date, no study has examined primary care provider lung cancer screening knowledge and barriers to ordering LDCT scan for lung cancer screening across various healthcare settings.
By surveying primary care providers in three different healthcare settings, this study aimed to measure knowledge of current guidelines for lung cancer screening after approval by CMS. In addition, this study investigates the specific reasons primary care providers choose to recommend or not recommend LDCT scan for lung cancer screening, giving further insight into the barriers to implementation of LDCT scan for lung cancer screening in the United States.
Methods
An anonymous survey was sent via e-mail to primary care providers (PCPs) in three different types of healthcare settings in the United States: a university tertiary care center, a public safety net hospital, and three community hospitals. The five hospitals included in this study were chosen based on author affiliation. Primary care provider e-mail listservs were then acquired in order to distribute our survey to all primary care providers employed at each hospital. All surveys returned were used for analysis, although some provider demographic data were missing. Physicians, physician assistants (PA), and advanced nurse practitioners (APN) who specialize in Internal Medicine or Family Practice were included. Employment was defined as employed or in private practice. Responses were compiled using Survey Monkey® software. The survey is included in the Supplementary file.
Data pertaining to provider demographics and clinical practice were collected using multiple choice questions. Likert scale was used to assess providers’ perception regarding barriers to the utilization of LDCT scan. Respondents were asked to identify the CMS beneficiary eligibility criteria for the utilization of LDCT scan for lung cancer screening (11). Each provider was presented with six correct criteria (the patient must be 55–77 years age; the patient must be asymptomatic; the patient must have a smoking history of at least 30 pack-years; the patient must be a current smoker or has quit smoking within the last 15 years; there must be a documented smoking cessation counseling and face-to-face shared decision making visit; there must be a written order for LDCT scan provided by a licensed provider) and three incorrect criteria (the patient must have no prior abnormal chest X-ray; the patient must have no cancer history; and the patient must be able to tolerate a lung resection if a malignancy is detected). Respondents were asked to select all that are correct. For each correct criterion selected, the respondent received one point. For each incorrect criterion not selected, the respondent received one point. The respondent’s possible total score ranged from 0–9 points. Differences in mean scores were compared using Dunn’s test with P values adjusted using Bonferonni method.
Categorical data were presented as percentage frequencies, with continuous data presented as mean values and standard deviation. Categorical outcomes were analyzed using χ2 or the Fisher exact test, as appropriate. Continuous outcomes were analyzed by the Kruskal-Wallis test. A multivariable logistic regression model was constructed to investigate the relationship between provider characteristics and the likelihood of utilizing LDCT for lung cancer screening. Provider characteristics (independent variables) included hospital affiliation, specialty, title, employment, and CMS eligibility provider knowledge scores. Utilization of LDCT scan (dependent variable) was classified according to PCP’s responses regarding average monthly orders placed for LDCT (0; ≥1). Two-tailed tests were used and statistical significance was defined as P<0.05.
Results
Provider characteristics
The survey was sent to 614 providers, with a 15.7% (n=96) response rate. Respondent characteristics are listed in Table 1. Respondents were primarily physicians (91.7%), practiced Internal Medicine (78.7%), and were employees of the hospital at which they practice (89.6%). Of the total respondents, 33% were community-based, 39.2% were university-based, and 27.8% were safety net-based. On average, providers saw 200 patients (SD 156) in clinic per month [community 237 (SD 131), academic 150 (SD 79), safety net 240 (SD 237)].
Table 1. Provider demographics compared across hospital settings.
| Total, n (%) | Primary affiliation | P value | |||
|---|---|---|---|---|---|
| Community, n (%) | Academic, n (%) | Safety Net, n (%) | |||
| Title | 0.17 | ||||
| Advanced practice nurse | 5 (5.2) | 0 | 3 (7.9) | 0 | |
| Physician assistant | 3 (3.1) | 1 (3.2) | 0 | 1 (3.2) | |
| Physician | 88 (91.7) | 30 (96.8) | 35 (92.1) | 30 (96.8) | |
| Specialty | 0.01 | ||||
| Family practice | 20 (21.3) | 8 (27.6) | 2 (5.3) | 8 (27.6) | |
| Internal medicine | 74 (78.7) | 21 (72.4) | 36 (94.7) | 21 (72.4) | |
| Employment | 0.34 | ||||
| Employed | 86 (89.6) | 26 (83.9) | 34 (89.5) | 26 (83.9) | |
| Private practice | 10 (10.4) | 5 (16.1) | 4 (10.5) | 5 (16.1) | |
Provider practice
Overall, 29.2% of providers never ordered LDCT scans for eligible patients. Of the providers who order LDCT scans, 80.9% stated that they only order 1–3 per month. The rate of providers who utilize LDCT scan at least once per month was similar across healthcare settings (community 77.4%, academic: 68.4%, safety net: 66.7%; P=0.637).
Examining patient inquiry, 61.5% of providers stated that zero patients ask them about lung cancer screening per month. Of the providers who are asked about lung cancer screening, 91.9% stated that only 1–3 patients ask per month. Providers practicing at a community or academic hospital were more commonly asked about lung cancer screening than providers practicing at a safety net hospital (community 48.4%; academic: 39.5%; safety net: 25.9%).
Knowledge of CMS beneficiary eligibility criteria
Providers demonstrated variation in knowledge of CMS eligibility criteria for lung cancer screening. Overall, providers received a mean score of 6.53 (SD 1.44). Academic- and community-based providers received a significantly higher mean score than safety net-based providers [academic: 6.84 (SD 1.33); safety net: 5.85 (SD 1.38); P=0.01] [community: 6.72 (SD 1.46); safety net: 5.85 (SD 1.38); P=0.02]. Overall, only 6.2% of respondents received a knowledge score of 9, i.e., correctly identified all six CMS eligibility criteria when challenged with three incorrect criterion (Table 2). Pertaining specifically to correct eligibility criteria, only 23.7% of providers correctly identified all six CMS eligibility criteria. Of the 32 community-based providers, 59.3% correctly identified five or more CMS criteria. Of the 38 academic-based providers, 52.6% correctly identified 5 or more CMS criteria. Of the 27 safety net-based providers, 33.3% correctly identified 5 or more CMS criteria.
Table 2. Provider knowledge score of CMS beneficiary eligibility compared across hospital settings.
| Knowledge score | Total, n (%) | Primary affiliation | ||
|---|---|---|---|---|
| Community, n (%) | Academic, n (%) | Safety Net, n (%) | ||
| 3 | 3 (3.1) | 2 (6.3) | 0 | 1 (3.7) |
| 4 | 3 (3.1) | 0 (0) | 2 (5.3) | 1 (3.7) |
| 5 | 19 (19.6) | 5 (15.6) | 3 (7.9) | 11 (40.7) |
| 6 | 22 (22.7) | 4 (12.5) | 11 (29.0) | 7 (25.9) |
| 7 | 21 (21.7) | 8 (25.0) | 9 (23.7) | 4 (14.8) |
| 8 | 23 (23.7) | 13 (40.6) | 9 (23.7) | 1 (3.7) |
| 9 | 6 (6.2) | 0 | 4 (10.5) | 2 (7.4) |
CMS, Centers for Medicare and Medicaid Services.
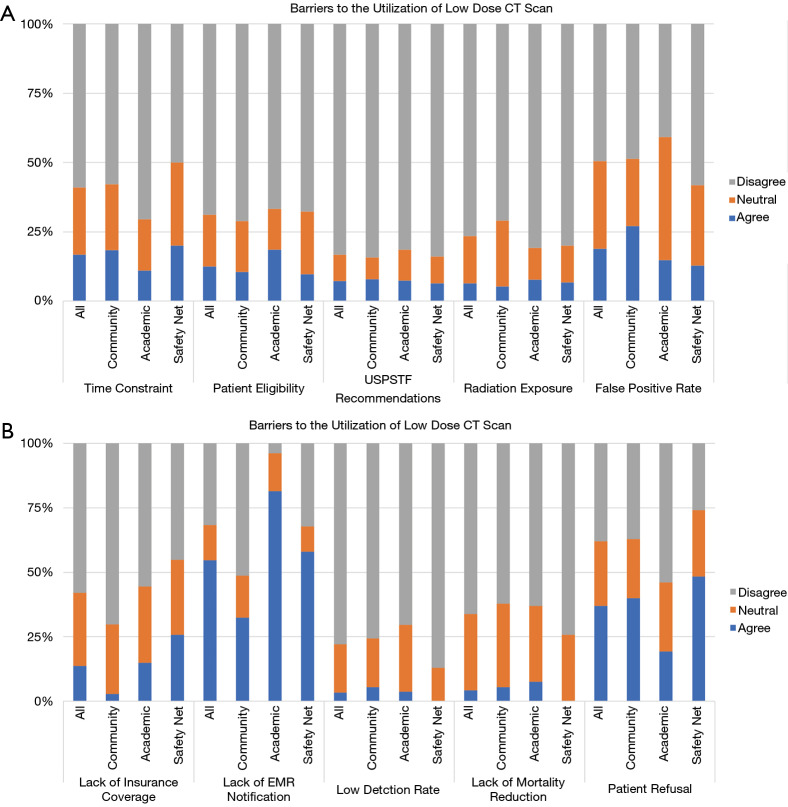
Barriers to utilization of LDCT for lung cancer screening
Common barriers to utilization of LDCT scan included failure of the electronic medical record (EMR) to notify providers of eligible patients (54.7%), patient refusal (37%), perceived high false-positive rate leading to unnecessary procedures (18.9%), provider time constraints (16.8%), and lack of insurance coverage (13.7%). Community-based providers reported lack of EMR notifications (58.1%), patient refusal (48.4%) and lack of insurance coverage (25.8%) as the most significant barriers. Academic-based providers reported patient refusal (40%), lack of EMR notifications (32.4%), and high rate of false positives (27%) as the most significant barriers. Safety net-based providers reported lack of EMR notifications (81.5%), patient refusal (19.2%), and uncertainty of patient eligibility (18.5%) as the most significant barriers (Figure 1).
Figure 1.
Barriers to the utilization of low dose CT scan. (A) Barriers to the utilization of low-dose CT scan; (B) barriers to the utilization of low-dose CT scan continued. USPSTF, United States Preventive Services Task Force; EMR, electronic medical record.
Likelihood of the utilization of LDCT
Controlling for provider characteristics (hospital affiliation, specialty, title, employment) and CMS eligibility provider knowledge scores, a higher provider knowledge score was associated with a higher likelihood of ordering a LDCT scan. For every one point increase in knowledge score, the likelihood of the provider ordering a LDCT scan increased by 13%. Several other covariates trended toward a higher likelihood of ordering a LDCT scan, although none reached statistical significance (Table 3).
Table 3. Likelihood of ordering low-dose computerized tomography scan for lung cancer screening.
| Odds ratio | 95% CI | |
|---|---|---|
| 1-Point Increase in Knowledge Score | 1.13 | 0.78–1.64 |
| Affiliation | ||
| Safety Net Hospital | ref | – |
| Community Hospital | 2.28 | 0.56–9.31 |
| Academic Hospital | 1.16 | 0.34–3.92 |
| Specialty | ||
| Family Practice | ref | – |
| Internal Medicine | 0.59 | 0.15–2.34 |
| Employment | ||
| Private practice | ref | – |
| Employed | 2.38 | 0.56–10.07 |
| Title | ||
| Advanced Nurse Practitioner | ref | – |
| Physician’s Assistant | 1.04 | 0.03–34.15 |
| Physician | 1.76 | 0.26–11.93 |
Discussion
The American Lung Association predicts that widespread screening of smokers who are currently at high risk of developing lung cancer could save approximately 24,000 lives (16). Despite the landmark National Lung Screening Trial (4), which demonstrated a 20% reduction in cancer-related mortality, and broad support from several medical professional societies, LDCT scan for lung cancer screening is significantly underutilized. This study emphasizes the challenge of translating lung cancer screening evidence into clinical practice. In this study, we demonstrate that primary care providers have limited knowledge of lung cancer screening guidelines, significantly underutilize LDCT scan, and face similar barriers across healthcare settings. In order to implement an effective national lung cancer screening initiative and reduce the high mortality associated with lung cancer, such barriers and knowledge gaps must be addressed so that LDCT scan can be integrated into primary and preventive care.
Provider knowledge gap
The current study demonstrates that primary care providers have varying knowledge of the current CMS beneficiary eligibility criteria for lung cancer screening. Although over two-thirds of providers reported that a lack of knowledge of the CMS beneficiary eligibility criteria is not a barrier to the utilization of LDCT scan, less than one-quarter of providers were able to accurately identify all six CMS criteria, and when challenged with incorrect eligibility criteria, only 6% could distinguish correct from incorrect CMS eligibility criteria. These findings are consistent with prior studies that examined provider knowledge of current screening guidelines (17-20). Surveying family practitioners in South Carolina, one study reported that nearly two-thirds of providers could not correctly state the current guidelines and did not know that Medicare covers LDCT scan for lung cancer screening (17). Other studies have shown that less than one-half of surveyed providers knew that the USPSTF, the ACS and the NCCN support the utilization of LDCT scan for lung cancer screening (17,19,20) and that many providers believed that the USPSTF recommends screening with chest X-ray (18,19).
Further examining the overall gap in knowledge across healthcare settings, the current study demonstrates that academic-based providers achieved similar knowledge scores to community-based providers, both of which were significantly higher than the knowledge scores of safety net-based providers. Further, safety net providers not only ordered LDCT scan least frequently, but also reported uncertainty of patient eligibility criteria as a major barrier to the utilization of LDCT scan. Although the current data are not equipped to determine if a lack of knowledge of the CMS beneficiary eligibility criteria for lung cancer screening led to an underutilization of LDCT scan, these findings suggest an association. For every one point increase in provider knowledge score, the likelihood of ordering a LDCT scan increased by 13%. To our knowledge, no prior study has examined the variation of provider knowledge of lung cancer screening guidelines across healthcare settings. Such variation suggests an opportunity for quality improvement initiatives focused on lung cancer screening education for healthcare providers.
Barriers and underutilization
This study demonstrates that LDCT scan is underutilized. Nearly two-thirds of providers stated that patients do not ask them about lung cancer screening. Further, providers infrequently order LDCT scan. Despite 83% of providers agreeing with the statement, “The USPSTF recommends annual screening with LDCT scan,” nearly one-third of respondents reported that they do not order LDCT scan and of those who do, 80% of providers only order 1–3 per month. These findings add to the mounting evidence that LDCT scan is underutilized in the United States. For example, from 2010 to 2015, during which time the NLST released its findings and the ACS and USPSTF both released recommendations for the utilization of LDCT scan for lung cancer screening, the proportion of eligible patients who received a LDCT scan increased by only 0.6% (13). In addition, in 2016, 7.6 million patients were eligible for lung cancer screening; however, only 1.9% of eligible patients were actually screened (21).
A failure of the electronic medical record to notify providers of eligible patients and patient refusal were the most frequently endorsed barriers to the utilization of LDCT scan across all three healthcare settings. Although only safety net-based providers cited uncertainty of eligibility criteria as a major barrier to utilizing LDCT scan for lung cancer screening, our results suggest that a knowledge gap exists across all three healthcare settings. Such a knowledge gap may be the true driving force behind the two main barriers to utilization that were identified (e.g., lack of EMR notifications and patient refusal). Perhaps primary care providers rely on EMR notifications because they are unfamiliar with eligibility criteria. However, EMR notifications are reliant on tobacco history which is often not collected for each patient or is inaccurate. In addition, it remains unclear if eligible patients refuse screening with LDCT scan because they are uninformed of the indications and benefits of screening. Identifying the root cause of the knowledge gap may facilitate the implementation of an effective national screening initiative.
Prior studies have found that provider uncertainty of screening criteria arose from the presence of multiple screening recommendations, each with slightly different guidelines regarding whom to screen, how frequently, and for how long (19,22). Further, the AAFP (14) has stated that “there is not enough evidence to either recommend or discourage the use of LDCT for lung cancer screening in high risk patients” and the USPSTF has only issued a B rating for lung cancer screening with LDCT (5). Studies have suggested that primary care providers only strongly advocate for USPSTF A-rated preventive services (19). If primary care providers prioritize the AAFP as their predominant source of current guidelines, they may be unaware of changes made to national screening guidelines as they arise (19,20), which may prevent primary care providers from facilitating conversations regarding the potential harms, benefits and indications for lung cancer screening with their patients. For example, one survey of high-risk patients found that the majority of patients were unaware of LDCT scan because no healthcare provider had ever discussed screening with them (20). However, patients are generally receptive to learning more about screening with LDCT scan (22). Recommendations provided by PCPs have been shown to have a significant influence on patient screening behaviors (23). Despite patient anxiety about a potential cancer diagnosis and cost of LDCT scan, studies have demonstrated that if educated on the risks, benefits, and current recommendations, high-risk patients would willingly undergo LDCT scan for screening if advised to do so by their PCP (20,24). Further, a designated counseling and shared decision-making clinic appointment, one of the CMS beneficiary eligibility criterion, has been shown to significantly improve patients’ understanding of lung cancer screening with LDCT (25). Thus, enhancing provider knowledge of lung cancer screening may translate into improved patient understanding, further empowering high-risk patients to make value-based decisions regarding lung cancer screening with LDCT scan.
Implications for LDCT screening
From these findings, we propose three initiatives to improve the utilization of LDCT scan for lung cancer screening. First, providers should be made aware of designated Screening Centers of Excellence, as well as the American College of Radiology Lung Cancer Screening Registry (26), which provides data that can validate the findings from the NLST. This may aid professional medical societies, including the AAFP, the USPSTF and CMS reach a consensus regarding lung cancer screening best practices, and release uniform, evidence-based national recommendations. Second, additional efforts are necessary to increase provider and patient awareness of lung cancer screening with LDCT scan. Primary care providers have shown to be highly receptive to educational webinars regarding lung cancer screening, how to best incorporate it into their practice, and how to facilitate conversations with their high-risk patients (22). Educational materials and videos, posters in clinic waiting rooms, and decision aids could be made available to high-risk patients. Such materials not only increase knowledge and awareness, but will further facilitate necessary communication regarding lung cancer screening. Third, alerts for eligible high-risk patients, auto-populated referral tools, and lists of certified lung cancer screening centers could be incorporated into the EMR. Prior studies have shown that such pop-up reminders in the EMR with subsequent referral have been effective (22). Applying these three measures may facilitate the implementation of an effective national lung cancer screening initiative and reduce the high mortality associated with lung cancer.
Some limitations should be considered in interpreting the findings of this study. Response rates for web-based surveys of healthcare professionals have been shown to be highly variable, and often quite low (27,28). Although the survey was sent to healthcare providers in multiple hospital settings, the low response rate perhaps limits the generalizability of our findings. Second, due to the anonymous and voluntary nature of the survey, we were unable to identify responders and non-responders in order to gather further data to analyze non-responder bias. Third, because providers worked at hospitals located in a single region, our findings may not reflect the patterns of care of providers located in other parts of the country. Fourth, providers may have felt uncomfortable answering questions regarding a personal knowledge gap, which could have influenced their responses. Lastly, due to the cross-sectional nature of a survey study, our findings represent the practices of providers at only one point in time.
In conclusion, LDCT scan is underutilized as a lung cancer screening modality in the United States. Common barriers to the utilization of LDCT scan, such as failure of the EMR to notify providers of eligible patients and patient refusal, may be due to provider and patient unfamiliarity with lung cancer screening current guidelines. In order to better incorporate lung cancer screening into practice, we propose that (I) patients continue to be enrolled in the American College of Radiology Lung Cancer Screening Registry; (II) educational initiatives and public screening campaigns are broadly implemented to foster provider and patient awareness of lung cancer screening; and (III) high-risk patient eligibility and referral tools be incorporated into the EMR and utilized by providers.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: None.
Supplementary
-
Tell us about your practice!
-
What is the primary hospital that you are affiliated with?
Rush University Medical Center
Rush Oak Park Hospital
Rush Copley
John H. Stroger, Jr. Hospital of Cook County
Northwest Community Hospital
-
What is your title?
Physician
Physician’s assistant
Advanced practice nurse
-
What is your specialty?
Internal Medicine
Family Practice
-
Are you employed or in private practice?
Employed B. Private practice
-
What percentage of your patients are: (0–25%; 26–50%; 51–75%; 76–100%)
-
Asian B. African-American
Hispanic D. Caucasian
-
On average, approximately how many individual patients do you see per month? (Fill in box)
-
On average, how many times per month does a patient ask about lung cancer screening?
-
None B. 1–3
-
4–7 D. 8–10
>10
-
-
-
On average, how many times per month do you order a LDCT for an eligible patient?
-
None B. 1–3
-
4–7 D. 8–10
>10
-
-
Knowledge about LDCT Screening Which of the following are necessary requirements to receive reimbursement from Medicare/Medicaid for a LDCT screening exam? (Select all that apply)
Patient is 55–77 years of age
Patient has no prior abnormal chest X-ray
-
Patient is asymptomatic
Patient has a smoking history of at least 30 pack-years
Patient is a current smoker or quit smoking within the last 15 years
Patient must have no cancer history
Documented smoking cessation counseling and face-to-face shared decision-making visit
Written order for LDCT was provided by a licensed provider
The patient must be able to tolerate a lung resection if a malignancy is found
-
Barriers to LDCT Screening (Strongly Agree, Agree, Neutral, Disagree, Strongly Disagree)
It takes too much time to educate patients, order the test, and follow up on the results.
I am not sure which patients qualify for low-dose CT scan.
Low-dose CT is not recommended by USPSTF.
I am concerned about the risk of radiation exposure.
Low-dose CT scan has a high false positive rate leading to unnecessary procedures.
Low-dose CT scan is not covered by insurance.
The EMR does not notify me of eligible patients.
Low-dose CT scan has a low likelihood of detecting lung cancer.
Low-dose CT scan does not decrease mortality.
Patients refused LDCT even though it was offered to them.
Other (Please specify).
-
-
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.03.66). CWS serves as an unpaid editorial board member of Journal of Thoracic Disease from Jul 2017 to Jun 2021. The other authors have no conflicts of interest to declare.
References
- 1.Siegel R, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7-34. 10.3322/caac.21551 [DOI] [PubMed] [Google Scholar]
- 2.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2016, National Cancer Institute. Bethesda, MD, Available online: https://seer.cancer.gov/csr/1975_2016/, based on November 2018 SEER data submission, posted to the SEER web site, April 2019.
- 3.Oken MM, Hocking WG, Kvale PA, et al. Screening by chest radiograph and lung cancer mortality: the Prostate, Lung, Colorectal, and Ovarian (PLCO) randomized trial. JAMA 2011;306:1865-73. 10.1001/jama.2011.1591 [DOI] [PubMed] [Google Scholar]
- 4.Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. 10.1056/NEJMoa1102873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clinical Summary: Lung Cancer: Screening. U.S. Preventive Services Task Force. October 2014. Available online: https://www.uspreventiveservicestaskforce.org/Page/Document/ClinicalSummaryFinal/lung-cancer-screening
- 6.Wender R, Fontham E, Barrera E, et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin 2013;63:107-17. 10.3322/caac.21172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wood DE, Kazerooni E, Baum S, et al. Lung cancer screening, version 3.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 2018;16:412-41. 10.6004/jnccn.2018.0020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaklitsch MT, Jacobson FL, Austin JH, et al. The American Association for Thoracic Surgery guidelines for lung cancer screening using low-dose computed tomography scans for lung cancer survivors and other high-risk groups. J Thorac Cardiovasc Surg 2012;144:33-8. 10.1016/j.jtcvs.2012.05.060 [DOI] [PubMed] [Google Scholar]
- 9.Lung Cancer Screening Guidelines [Internet]. The Society of Thoracic Surgeons. 2019. Available online: https://www.sts.org/resources/lung-nodule-resources/lung-cancer-screening-guidelines
- 10.American Thoracic Society and American Lung Association. Lung cancer screening implementation guide. Available online: https://www.lung.org/assets/documents/lung-cancer/implementation-guide-for-lung.pdf
- 11.Centers for Medicare & Medicaid Services. Decision Memo for Screening for Lung Cancer with Low Dose Computed Tomography (LDCT). Available online: https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=274
- 12.Richardson A. Screening and the number needed to treat. J Med Screen 2001;8:125-7. 10.1136/jms.8.3.125 [DOI] [PubMed] [Google Scholar]
- 13.Jemal A, Fedewa SA. Lung Cancer Screening With Low-Dose Computed Tomography in the United States—2010 to 2015. JAMA Oncol 2017;3:1278-81. 10.1001/jamaoncol.2016.6416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Armstrong C. Lung Cancer Screening Recommendations from the AAFP. Am Fam Physician 2018;98:688-9. [PubMed] [Google Scholar]
- 15.Okereke IC, Nishi S, Zhou J, et al. Trends in lung cancer screening in the United States, 2016-2017. J Thorac Dis 2019;11:873-81. 10.21037/jtd.2019.01.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Lung Association. Lung cancer screening could save your life. April 2018. Available online: https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/lung-cancer/patient-resources-and-videos/videos/lung-cancer-screening-could-save-life.html
- 17.Ersek JL, Eberth JM, McDonnell KK, et al. Knowledge of, attitudes toward, and use of low-dose computed tomography for lung cancer screening among family physicians. Cancer 2016;122:2324-31. 10.1002/cncr.29944 [DOI] [PubMed] [Google Scholar]
- 18.Lewis JA, Petty WJ, Tooze JA, et al. Low-dose CT Lung Cancer Screening Practices and Attitudes Among Primary Care Providers at an Academic Medical Center. Cancer Epidemiol Biomarkers Prev 2015;24:664-70. 10.1158/1055-9965.EPI-14-1241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoffman RM, Sussman AL, Getrich CM, et al. Attitudes and beliefs of primary care providers in New Mexico about lung cancer screening using low-dose computed tomography. Prev Chronic Dis 2015;12:E108. 10.5888/pcd12.150112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simmons VN, Gray JE, Schabath MB, et al. High-risk community and primary care providers knowledge about and barriers to low-dose computed topography lung cancer screening. Lung Cancer 2017;106:42-9. 10.1016/j.lungcan.2017.01.012 [DOI] [PubMed] [Google Scholar]
- 21.Pham D, Bhandari S, Oechsli M, et al. Lung cancer screening rates: Data from the lung cancer screening registry. J Clin Oncol 2018;36:6504. 10.1200/JCO.2018.36.15_suppl.6504 [DOI] [Google Scholar]
- 22.Kanodra NM, Pope C, Halbert CH, et al. Primary care provider and patient perspectives on lung cancer screening. a qualitative study. Ann Am Thorac Soc 2016;13:1977-82. 10.1513/AnnalsATS.201604-286OC [DOI] [PubMed] [Google Scholar]
- 23.Zapka JG, Lemon SC. Interventions for patients, providers, and health care organizations. Cancer 2004;101:1165-87. 10.1002/cncr.20504 [DOI] [PubMed] [Google Scholar]
- 24.Delmerico J, Hyland A, Celestino P, et al. Patient willingness and barriers to receiving a CT scan for lung cancer screening. Lung Cancer 2014;84:307-9. 10.1016/j.lungcan.2014.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mazzone PJ, Tenenbaum A, Seeley M, et al. Impact of a lung cancer screening counseling and shared-decision-making visit. Chest 2017;151:572-8. 10.1016/j.chest.2016.10.027 [DOI] [PubMed] [Google Scholar]
- 26.Lung CT Screening Reporting and Data System. American College of Radiology. 2014. Available online: http://www.acr.org/Quality-Safety/Resources/LungRADS.
- 27.Dykema J, Jones NR, Piche T, et al. Surveying clinicians by web: current issues in design and administration. Eval Health Prof 2013;36:352-81. 10.1177/0163278713496630 [DOI] [PubMed] [Google Scholar]
- 28.McLeod CC, Klabunde CN, Willis GB, et al. Health care provider surveys in the United States, 2000-2010: a review. Eval Health Prof 2013;36:106-26. 10.1177/0163278712474001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as