Abstract
Background
Vasovagal syncope is a common clinical occurrence during routine outpatient dermatology procedures, such as injections and biopsies. Despite its prevalence, many medical students and health care professionals do not know how to respond appropriately to a syncopal episode.
Objective
The aim of this study was to determine the efficacy of a health education video in teaching medical students and health care professionals the appropriate management steps for vasovagal syncope and its prodromal symptoms in a clinical setting.
Methods
With input from dermatologists and an anesthesiologist, an instructional video was developed to demonstrate basic management for a presyncopal and syncopal patient. A pre- and post-video quiz was used to assess comprehension. A total of 124 medical students and health care professionals were enrolled in this study.
Results
After viewing the video, the proportion of respondents who were able to correctly identify how long to monitor a patient after a syncopal episode increased from pre- to post-intervention (44% vs. 71%; p < .001). Participants expressed higher levels of agreement with the statement “I am aware of the appropriate steps in managing a patient during an episode of vasovagal syncope” after the intervention (p < .001). Respondents reported increased confidence in managing a patient during a syncopal episode after this intervention (p < .001).
Conclusion
These results suggest that this health education video is a useful tool for educating medical students and nursing professionals about the management of vasovagal syncope in a clinical setting. We propose the use of video education as an efficient means of increasing recognition and standardizing therapeutic response to the prodromal symptoms of syncope and syncopal episodes.
Keywords: Vasovagal syncope, Video education, Medical education, Vasovagal management
Introduction
Vasovagal syncope (VVS) is a common clinical syndrome with complex pathophysiology that can be difficult to manage. VVS is thought to be due to a combination of decreased preload, decreased sympathetic with increased parasympathetic activity, vasodilation, and cardio-inhibition (Aydin et al., 2010). VVS is challenging to recognize and treat because the patient population is highly heterogeneous. Patients of all ages have different triggers and prodromal symptoms that make its incidence difficult to predict (Fenton et al., 2000).
Although many therapeutic options exist for the long-term management of VVS, the choice of therapy in the acute setting is often empiric and its efficacy unsubstantiated (Fenton et al., 2000). A knowledge gap exists in the management of prodromal VVS symptoms because few large-scale clinical trials have been conducted due to the sporadic nature of VVS (Vaddadi et al., 2010). Teaching health care professionals standardized steps for responding to the prodromal symptoms of VVS is a preventive health strategy for managing these patients.
The impact of syncope on the health care system is significant. Each year, 1 million patients are evaluated for syncope at a cost of $2.4 billion for syncope-related hospitalizations (Jowett et al., 2007, Sun et al., 2005). Training health care providers to recognize the prodromal symptoms of VVS may potentially reduce medical workups for syncope and alleviate the associated economic and emotional costs.
The primary objective of this study was to determine the efficacy of video education in teaching clinical providers to recognize and manage prodromal symptoms of syncope as well as syncope itself in the diverse patient population affected. The ultimate purpose is to assess whether an intervention, such as video education, could be integrated into medical education and dermatology training programs alike to address the lack of standardized protocols in place for responding to VVS episodes.
Video education was chosen because it has been shown to be an efficient adjunct to conventional clinical training (Eisenburger and Safar, 1999). Educational videos are a useful tool for presenting new information in addition to reinforcing previous learning (Mehrpour et al., 2013, Salina et al., 2012). However, there are few educational videos on managing vasovagal episodes and its prodromal symptoms. Given the effectiveness of this method, this study aimed to assess the use of an educational video to prepare health care trainees and professionals to manage VVS in a systematic way.
Methods
After approval by the institutional review board, 124 medical, nursing, MD/PhD students, graduate-level registered nurses (RNs), and practicing RNs were enrolled in the study. Participants were selected by voluntary participation, without any exclusions. Each study participant was shown an instructional video demonstrating the basic steps for managing a symptomatic pre-syncopal and syncopal patient. In addition to management steps, the video also covered known pathophysiology of VVS, common clinical scenarios, prodromal symptoms, and prevention techniques.
The video was developed and produced with the supervision of two dermatologists and an anesthesiologist. Standard-of-care practices, including changing gloves between injection and VVS management, were performed but not explicitly described in the video. Pre- and post-tests consisting of three content-based multiple-choice questions and four questions on a Likert scale were given to study participants immediately after the video. Comprehension of the material and confidence in management of syncope were assessed by comparing the results of the pre- and post-test scores using a Wilcox signed rank test. The video can be found online at https://youtu.be/WAoVTgz4QyM (Loyola Derm, 2018).
Results
After viewing the video, participants expressed higher levels of agreement with the statement “I am aware of the appropriate steps in managing a patient during an episode of VVS” (p < .001; Table 1). Participants reported increased confidence levels about managing a patient during a syncopal episode after this intervention (p < .001; Table 1). The proportion of respondents able to correctly identify how long to monitor a patient after a syncopal episode increased from pre- to post-intervention (55 individuals answered correctly [44%] vs. 87 individuals [71%]; p < .001; Table 2).
Table 1.
Wilcoxon signed-rank test result of agreement rate increased from pre- to post-intervention.
| Pre-intervention, n (%) | Post-intervention, n (%) | p-value | |
|---|---|---|---|
| I am aware of the appropriate steps in managing a patient during an episode of vasovagal syncope | <0.001 | ||
| Strongly disagree | 61 (49) | 0 | |
| Disagree | 19 (15) | 3 (2.4) | |
| Neither agree nor disagree | 20 (16) | 19 (15) | |
| Agree | 19 (15) | 53 (43) | |
| Strongly agree | 5 (4.0) | 49 (40) | |
| I feel confident about managing a patient during an episode of vasovagal syncope | <0.001 | ||
| Strongly disagree | 64 (52) | 3 (2.4) | |
| Disagree | 21 (17) | 7 (5.7) | |
| Neither agree nor disagree | 18 (15) | 17 (14) | |
| Agree | 18 (15) | 60 (48) | |
| Strongly agree | 3 (2.4) | 37 (30) | |
Valid N = 124.
Table 2.
McNemar’s test results show the proportion of respondents correctly answering in before the test compared with after.
| Pre-intervention, n (%) (n = 124) |
Post-Intervention, n (%) (n = 123) |
p-value | |
|---|---|---|---|
| In what situation should you give a patient with vasovagal symptoms something to drink? | <0.001 | ||
| If the patient is nauseous | 4 (3.2) | 6 (4.9) | |
| Only when they are sitting upright | 27 (22) | 7 (5.7) | |
| Immediately when symptoms begin | 13 (10) | 4 (3.3) | |
| If the patient is fully conscious and not nauseous* | 80 (65) | 106 (86) | |
| How long should you monitor a patient after experiencing vasovagal symptoms to ensure they are stable? | <0.001 | ||
| 5 minutes | 0 (0) | 5 (4.1) | |
| 10 minutes | 31 (25) | 14 (11) | |
| 30 minutes* | 55 (44) | 87 (71) | |
| 1 hour | 38 (31) | 17 (14) | |
Correct response to the questions.
The fraction of respondents able to determine situations where a syncopal patient should be given something to drink also increased from pre- to post-intervention (80 individuals answered correctly [65%] vs. 106 individuals [86%]; p < .001; Table 2). The percentage of participants correctly answering the item “What is the most important technique to prevent syncopal episodes when performing procedures?” increased from pre- to post-intervention (76% vs. 85%; p = .10) but was not statistically significant (Table 2).
No meaningful difference in knowledge improvement from pre- to post-intervention was found by student type (medical student, nursing, other) or clinical training year (preclinical vs. clinical years; Table 3, Table 4).
Table 3.
Change in total knowledge from pre- to post-intervention, by student type.
| Points | Medical student, n (%) (n = 110) |
Nursing student, n (%) (n = 13) |
Total (N = 123) |
|---|---|---|---|
| –3 | 1 (0.9) | 0 | 1 (0.8) |
| –2 | 1 (0.9) | 0 | 1 (0.8) |
| –1 | 12 (11) | 1 (7.7) | 13 (11) |
| No change | 41 (37) | 4 (31) | 45 (37) |
| +1 | 40 (36) | 4 (31) | 44 (36) |
| +2 | 10 (9.1) | 3 (23) | 13 (11) |
| +3 | 5 (4.6) | 1 (7.7) | 6 (4.9) |
Wilcoxon Z = 1.20; p = .24.
Table 4.
Change in total knowledge from pre- to post-intervention, by year in medical school.
| Points | Year of medical school |
Total, n (%) (N = 110) |
|||
|---|---|---|---|---|---|
| First year, n (%) (n = 49) |
Second year, n (%) (n = 10) |
Third year, n (%) (n = 30) |
Fourth year, n (%) (n = 21) |
||
| –3 | 0 | 0 | 1 (3.3) | 0 | 1 (0.9) |
| –2 | 0 | 0 | 0 | 1 (4.8) | 1 (0.9) |
| –1 | 6 (12) | 0 | 5 (17) | 1 (4.8) | 12 (11) |
| No change | 16 (33) | 4 (40) | 13 (43) | 8 (38) | 41 (37) |
| +1 | 19 (39) | 4 (40) | 10 (33) | 7 (33) | 40 (36) |
| +2 | 6 (12) | 1 (10) | 0 | 3 (14) | 10 (9.1) |
| +3 | 2 (4.1) | 1 (10) | 1 (3.3) | 1 (4.8) | 5 (4.6) |
Kruskal-Wallis χ2 (df = 3) = 5.03; p = .17.
Discussion
VVS is the most common cause of recurrent syncope, with a lifetime incidence of 35% (Ganzeboom et al., 2006). Diagnosis and treatment of VVS is limited by the number of randomized control trials investigating VVS. Although efforts have been made to investigate the clinical management of prodromal symptoms and acute VVS episodes, the sporadic nature of VVS makes conducting large-scale clinical trials and determining best practices challenging (Vaddadi et al., 2007). Guidelines have been developed to evaluate a patient presenting with recurrent vasovagal episodes and for the long-term management of syncopal patients (Parry et al., 2009). However, limited research has evaluated techniques for managing a patient immediately preceding and during a vasovagal episode in clinic.
The recommended long-term management of a patient with VVS includes educating the patient, avoiding precipitating factors, and maintaining hydration. Patients should be educated on potential injury due to collapse in a VVS attack (Giada et al., 2005). Reassuring the patient of the benign nature of VVS is also important. Pharmacotherapy is rarely used but can include fludrocortisone, alpha‐agonists (e.g., midodrine and dihydroergotamine), and selective serotonin reuptake inhibitors (Liao et al., 2009, Olver et al., 1980, Raj et al., 2006, Sheldon et al., 2016). Permanent cardiac pacing has not been supported for the treatment of VVS (Sheldon and Connolly, 2003).
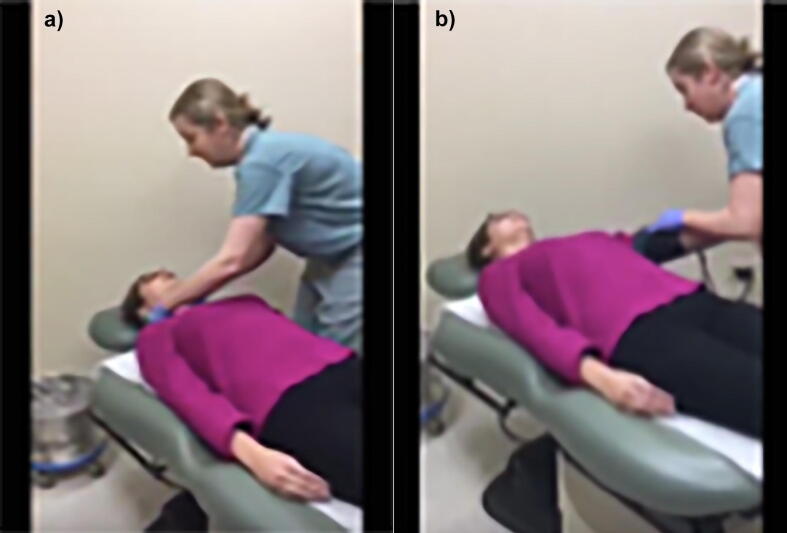
In the setting of an acute VVS episode, physical maneuvers have been shown to be an effective treatment. Placing the patient in a supine position, preferably with the head lowered in the Trendelenburg position, has been shown to effectively halt an acute vasovagal episode (van Dijk et al., 2006). This strategy helps the patient resume normotension after the hypotension of VVS. The patient’s blood pressure should be recorded and monitored immediately after the episode and every 10 minutes for up to 30 minutes while the patient remains in the supine position until symptoms resolve. The video used in this study demonstrated techniques of placing the patient in a supine position and monitoring blood pressure for up to 30 minutes for the acute management of a patient experiencing VVS (Fig. 1).
Fig. 1.
Video demonstration of physical manuver technique for immediate response to a vasovagal episode, including (A) lying in the supine position and (B) monitoring blood pressure for 10 minutes after the episode.
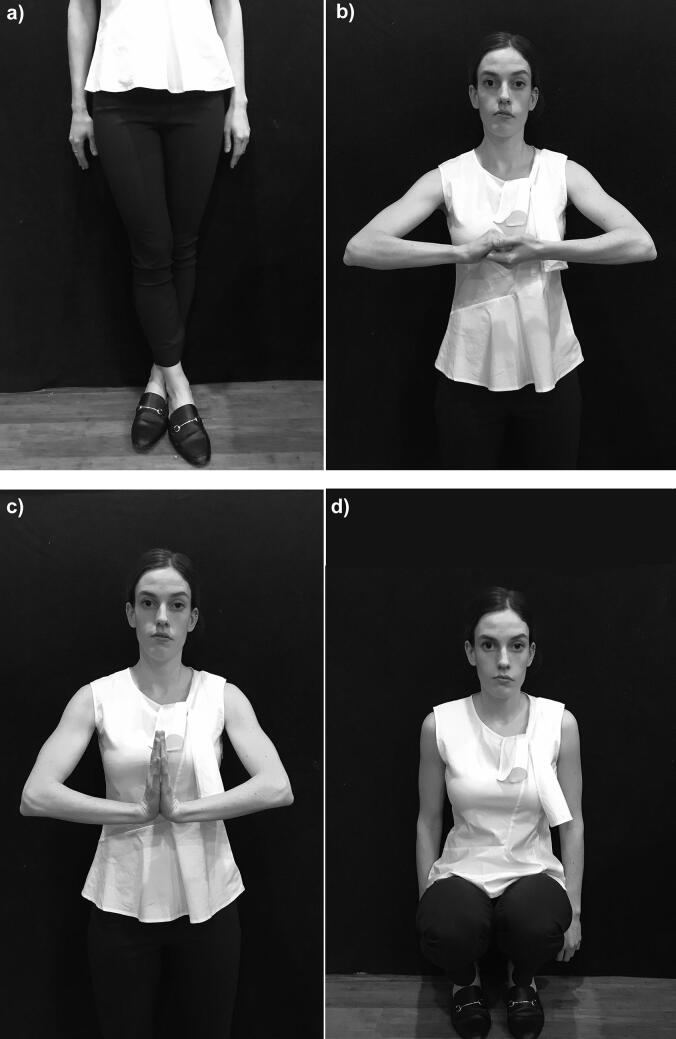
Physical maneuvers that have been shown to reduce the incidence of vasovagal episodes include sitting on the floor with the head between the knees, assuming a squat position, leg crossing, and hand grip techniques (Fig. 2; Vaddadi et al., 2010). One study found that training patients with recurrent VVS in physical maneuver techniques led to a 36% reduction in syncopal episodes with a number needed to treat of 5 (Vaddadi et al., 2010, van Dijk et al., 2006). Physicians can teach patients these muscle tensing and physical counterpressure maneuvers to prevent imminent syncope. However, of note, this technique may be challenging for patients who are already prepared for surgery and may be unable to assume these positions. An alternative for these patients could be ammonia (smelling salts), which has also been shown to be effective at stopping prodromal symptoms from progressing and at rousing a patient after syncope (Wu et al., 2018).
Fig. 2.
Techniques for aborting a vasovagal episode by physical counterpressure techniques. (A) Leg crossing with muscle tensing; (B) isometeric forearm grip; (C) isometric forearm press; and (D) squatting.
Despite the variety in treatment options, no therapy has been proven to be consistently effective for recurrent VVS. In the absence of clear-cut guidelines for a VVS response, having a standardized procedure in place to manage the prodromal symptoms of VVS and syncopal episodes has the potential benefits of immediate action, reduced risk of injury, and increased cohesion among the medical team.
Educational videos are a concise means of delivering clinical information to a large number of health care providers. The use of videos to teach clinicians has been successfully employed across many disciplines, including anesthesiology, nephrology, and pediatrics (Bessmann et al., 2019, Kapell Brown et al., 2018, Wang et al., 2016). Notably, the American Red Cross has successfully used video education for years in conjunction with hands-on practice to train health care providers in cardiopulmonary resuscitation (Eisenburger and Safar, 1999). Cardiopulmonary resuscitation training by video education alone has been found to be superior to instruction alone (Eisenburger and Safar, 1999, Todd et al., 1998). Video education leads to improved clinical skills performance compared with traditional lectures (Mehrpour et al., 2013, Salina et al., 2012). These studies suggest that videos are an effective means of educating health care providers about clinical techniques. The video developed and used in this study similarly demonstrated that this educational technique has the potential to teach medical students and nursing professionals the basic steps for managing symptoms of syncope and syncopal episodes in the clinic.
The study video also highlighted techniques to prevent VVS. Prevention techniques featured in the video include draping a towel over patients’ eyes so they cannot see surgical instruments, encouraging patients to be well-hydrated beforehand, and having them lie down for the procedure. A large percentage of participants (76%) preintervention were able to correctly identify steps to prevent VVS. Although the difference was not statistically significant, this percentage increased after the intervention (85%), suggesting video education is a useful tool for teaching prevention strategies, such as the prodromal signs of VVS, to prevent syncopal episodes.
There are several limitations to this study. One limitation is the lack of hands-on learning to practice and reinforce the techniques demonstrated in the video. Future studies could incorporate hands-on simulation of management steps. Skills performance could then be assessed after the combined video/simulated learning versus video education alone. Another limitation was the administration of the test immediately after the training. Follow-up assessments would have to be done to assess long-term knowledge retention, which would be critical in determining the validity and generalizability of this educational program.
Conclusion
This study investigated the use of a health education video to train medical and nursing students to manage episodes of VVS in a clinical setting. In the field of dermatology, vasovagal episodes commonly occur with minor procedures. Therefore, clinicians should be knowledgeable in prevention techniques and prodromal recognition and should have a basic response algorithm for a vasovagal event. This study indicates that a video education program has the potential to standardize clinical response to VVS and improve patient outcomes.
Acknowledgments
Acknowledgement
The authors thank William Adams for his work on the biostatistics portion of this paper.
Financial disclosures
None.
Funding
None.
Study approval
The author(s) confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies.
References
- Aydin M.A., Salukhe T.V., Wilke I., Willems S. Management and therapy of vasovagal syncope: a review. World J Cardiol. 2010;2(10):308–315. doi: 10.4330/wjc.v2.i10.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessmann E.L., Ostergaard H.T., Nielsen B.U., Russell L., Paltved C., Østergaard D. Consensus on technical procedures for simulation-based training in anaesthesiology: a Delphi-based general needs assessment. Acta Anaesthesiol Scand. 2019;63(6):720–729. doi: 10.1111/aas.13344. [DOI] [PubMed] [Google Scholar]
- Eisenburger P., Safar P. Life supporting first aid training of the public–review and recommendations. Resuscitation. 1999;41(1):3–18. doi: 10.1016/s0300-9572(99)00034-9. [DOI] [PubMed] [Google Scholar]
- Fenton A.M., Hammill S.C., Rea R.F., Low P.A., Shen W.K. Vasovagal syncope. Ann Intern Med. 2000;133(9):714–725. doi: 10.7326/0003-4819-133-9-200011070-00014. [DOI] [PubMed] [Google Scholar]
- Ganzeboom K.S., Mairuhu G., Reitsma J.B., Linzer M., Wieling W., van Dijk N. Lifetime cumulative incidence of syncope in the general population: a study of 549 Dutch subjects aged 35–60 years. J Cardiovasc Electrophysiol. 2006;17(11):1172–1176. doi: 10.1111/j.1540-8167.2006.00595.x. [DOI] [PubMed] [Google Scholar]
- Giada F., Silvestri I., Rossillo A., Nicotera P.G., Manzillo G.F., Raviele A. Psychiatric profile, quality of life and risk of syncopal recurrence in patients with tilt-induced vasovagal syncope. Europace. 2005;7(5):465–471. doi: 10.1016/j.eupc.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Jowett N., LeBlanc V., Xeroulis G., MacRae H., Dubrowski A. Surgical skill acquisition with self-directed practice using computer-based video training. Am J Surg. 2007;193(2):237–242. doi: 10.1016/j.amjsurg.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Kapell Brown C., Kryworuchko J., Martin W. Evaluation of the CPR video decision aid with patients with end stage renal disease. BMC Nephrol. 2018;19(1):226. doi: 10.1186/s12882-018-1018-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao Y., Li X., Zhang Y., Chen S., Tang C., Du J. Alpha-adrenoceptor agonists for the treatment of vasovagal syncope: a meta-analysis of worldwide published data. Acta Paediatr. 2009;98(7):1194–1200. doi: 10.1111/j.1651-2227.2009.01289.x. [DOI] [PubMed] [Google Scholar]
- Loyola Derm. Vasovagal education video [Internet]. 2018 [cited xxx]. Available from https://youtu.be/WAoVTgz4QyM.
- Mehrpour S.R., Aghamirsalim M., Motamedi S.M.K., Ardeshir Larijani F., Sorbi R. A supplemental video teaching tool enhances splinting skills. Clin Orthop Relat Res. 2013;471(2):649–654. doi: 10.1007/s11999-012-2638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olver I.N., Jennings G.L., Bobik A., Esler M. Low bioavailability as a cause of apparent failure of dihydroergotamine in orthostatic hypotension. Br Med J. 1980;281(6235):275–276. doi: 10.1136/bmj.281.6235.275-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry S.W., Reeve P., Lawson J., Shaw F.E., Davison J., Norton M. The Newcastle protocols 2008: an update on head-up tilt table testing and the management of vasovagal syncope and related disorders. Heart. 2009;95(5):416–420. doi: 10.1136/hrt.2007.136457. [DOI] [PubMed] [Google Scholar]
- Raj S.R., Rose S., Ritchie D., Sheldon R.S., POST II Investigators The Second Prevention of Syncope Trial (POST II)–a randomized clinical trial of fludrocortisone for the prevention of neurally mediated syncope: Rationale and study design. Am Heart J. 2006;151(6) doi: 10.1016/j.ahj.2006.03.013. 1186.e1–17. [DOI] [PubMed] [Google Scholar]
- Salina L., Ruffinengo C., Garrino L., Massariello P., Charrier L., Martin B. Effectiveness of an educational video as an instrument to refresh and reinforce the learning of a nursing technique: a randomized controlled trial. Perspect Med Educ. 2012;1(2):67–75. doi: 10.1007/s40037-012-0013-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheldon R., Connolly S. Vasovagal Pacemaker Study II. Second vasovagal pacemaker study (VPS II): Rationale, design, results, and implications for practice and future clinical trials. Card Electrophysiol Rev. 2003;7(4):411–415. doi: 10.1023/B:CEPR.0000023157.37745.76. [DOI] [PubMed] [Google Scholar]
- Sheldon R., Raj S.R., Rose M.S., Morillo C.A., Krahn A.D., Medina E. Fludrocortisone for the prevention of vasovagal syncope: a randomized, placebo-controlled trial. J Am Coll Cardiol. 2016;68(1):1–9. doi: 10.1016/j.jacc.2016.04.030. [DOI] [PubMed] [Google Scholar]
- Sun B.C., Emond J.A., Camargo C.A., Jr. Direct medical costs of syncope-related hospitalizations in the United States. Am J Cardiol. 2005;95:668–671. doi: 10.1016/j.amjcard.2004.11.013. [DOI] [PubMed] [Google Scholar]
- Todd K.H., Braslow A., Brennan R.T., Lowery D.W., Cox R.J., Lipscomb L.E. Randomized, controlled trial of video self-instruction versus traditional CPR training. Ann Emerg Med. 1998;31(3):364–369. doi: 10.1016/s0196-0644(98)70348-8. [DOI] [PubMed] [Google Scholar]
- Vaddadi G., Corcoran S.J., Esler M. Management strategies for recurrent vasovagal syncope. Intern Med J. 2010;40(8):554–560. doi: 10.1111/j.1445-5994.2010.02295.x. [DOI] [PubMed] [Google Scholar]
- Vaddadi G., Lambert E., Corcoran S.J., Esler M.D. Postural syncope: mechanisms and management. Med J Aust. 2007;187(5):299–304. doi: 10.5694/j.1326-5377.2007.tb01248.x. [DOI] [PubMed] [Google Scholar]
- van Dijk N., Quartieri F., Blanc J.J., Garcia-Civera R., Brignole M., Moya A. Effectiveness of physical counterpressure maneuvers in preventing vasovagal syncope: the Physical Counterpressure Manoeuvres Trial (PC-Trial) J Am Coll Cardiol. 2006;48(8):1652–1657. doi: 10.1016/j.jacc.2006.06.059. [DOI] [PubMed] [Google Scholar]
- Wang V., Cheng Y.T., Liu D. Improving education: Just-in-time splinting video. Clin Teach. 2016;13(3):183–186. doi: 10.1111/tct.12394. [DOI] [PubMed] [Google Scholar]
- Wu W.J., Goldberg L.H., Rubenzik M.K., Zelickson B.R. Review of the evaluation and treatment of vasovagal reactions in outpatient procedures. Dermatol Surg. 2018;44(12):1483–1488. doi: 10.1097/DSS.0000000000001598. [DOI] [PubMed] [Google Scholar]