Abstract
We report a case of a 53-year-old woman admitted to the emergency department with left hemiplegia, tinnitus and palpitations. A cerebral and cervical computed tomography angiography revealed an acute large ischemic stroke on the right Sylvian territory, which was related to a dissection of the right internal carotid. Moreover, a left internal carotid pseudo-aneurysm was observed.
These two injuries were presumably imputable to a bilateral Eagle Syndrome.
Indeed, the temporal styloid processes were measured at 31mm on both sides.
To support our hypothesis of a stylocarotid impingement, a cervical CTA with hyperflexion (45°) of the neck was performed. It clearly revealed the bilateral impingement between the styloid processes and internal carotids.
It seems important to know that Eagle syndrome may lead to disabling diseases or even death as well as an ischemic stroke. The vascular impingement with bilateral vascular injuries was never described.
To our knowledge, our “neck flexion cervical CTA” to reveal the stylocarotid impingement has never been described before. This approach could lead to a new investigation technique, to better identify this underestimated pathology in the medical doctors community.
Keywords: Eagle syndrome, Carotid artery dissection, Carotid artery aneurysm, Carotid artery pseudo-aneurysm, Stroke in young adults, Neck flexion CTA
Background
Eagle syndrome, first described by Watt W. Eagle in 1937, refers to the symptomatic elongation of the temporal styloid process and/or calcification of the stylohyoid ligament [1]. It is divided into 2 types: classic and stylocarotid syndrome respectively identified by cranial nerve and arterial impingement by the elongated styloid process. The syndrome provides a range of unspecific symptoms as dysphagia, toothache, earache, migraine, cervicofacial pain, syncope or even stroke related to nearby vulnerable neurovascular structures (internal and external carotid, jugular vein and cranial nerves) [2]. Extended styloid process, defined as longer than 3 cm, affects around 4% of the population but only a minority is symptomatic (2/1000). Eagle syndrome can be treated both medically and surgically. The latter consists mainly of an intraoral or a cervical approach to obtain a sub- or complete resection of the styloid process.
In our case, bilateral elongated styloid processes provoked right internal carotid dissection and left internal carotid pseudo-aneurysm.
Case report
A 53-year-old woman was admitted to the emergency department with left hemiplegia, tinnitus, and palpitations. Dyslipidemia was her only cardiovascular risk factor.
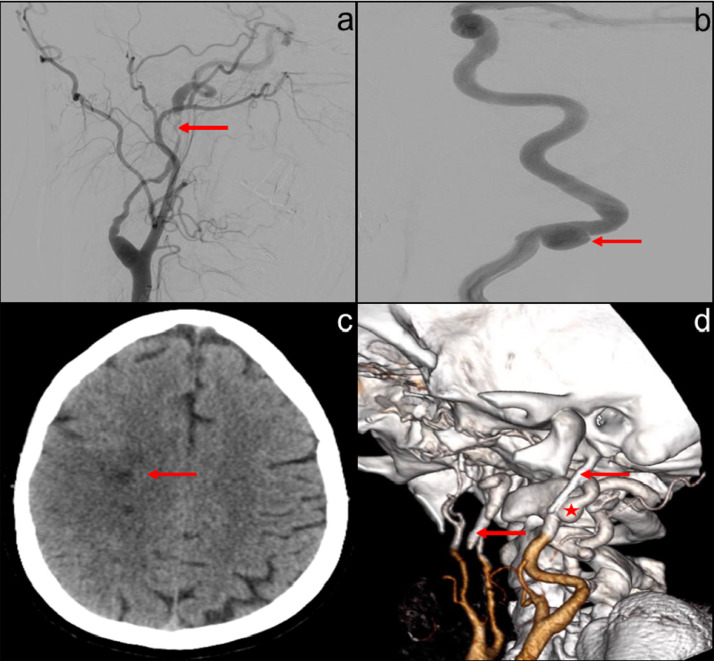
A nonenhanced brain computed tomography (CT) showed 3 small right frontal ischemic lesions related to a previous episode 2 weeks earlier when she presented a left brachiofacial paresis with spontaneous good recovery (Fig. 1).
Fig. 1.
(a) Right internal carotid dissection (red arrow) and (b) left internal carotid pseudo-aneurysm (red arrow) confirmed with angiography. (c) Axial nonenhanced brain CT showing several right frontal sequel ischemic lesions with sulci effacement. (d) 3D reconstruction CT with both elongated styloid processes (red arrows) and left pseudoaneurysm (red star).
On the cervical computed tomography angiography (CTA), a right internal carotid dissection and a left internal carotid pseudoaneurysm were observed with an acute large ischemic stroke on the right sylvian territory, without mismatch on the perfusion CT.
These injuries were confirmed by arteriography (Fig. 1). Doppler-ultrasound of the supra-aortic trunk showed a parietal hematoma with no atheromatous lesions nor fibromuscular dysplasia.
In the standard CT acquisition, in supine decubitus, we did not clearly demonstrate a close anatomical relationship between the temporal styloid and the vascular structures.
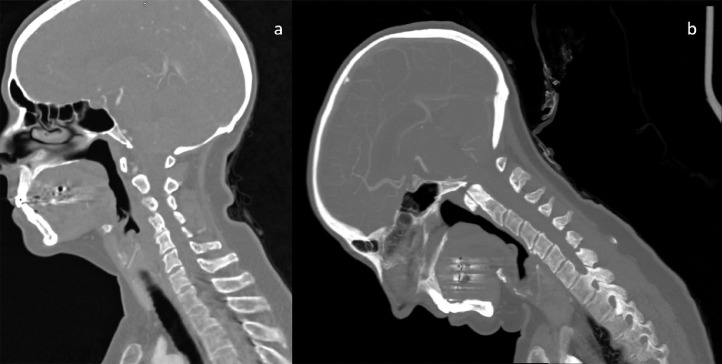
The styloid process being a spiny protuberance of the temporal bone oriented downward and forward, we imagined the head movement that would pointed it toward the vascular structures. As the tip of the styloid process was anterior to the carotid, we suggested a CT with a head flexion. Therefore, to support our hypothesis, we placed the patient in supine position with 2 pillows behind her head in order to obtain a 45° angulation (Fig. 2). This new “Stress-acquisition” technique was never described before.
Fig. 2.
(a) Classical CTA dorsal decubitus acquisition in sagittal. (b) Stress CTA (+/− 45° neck flexion) in sagittal.
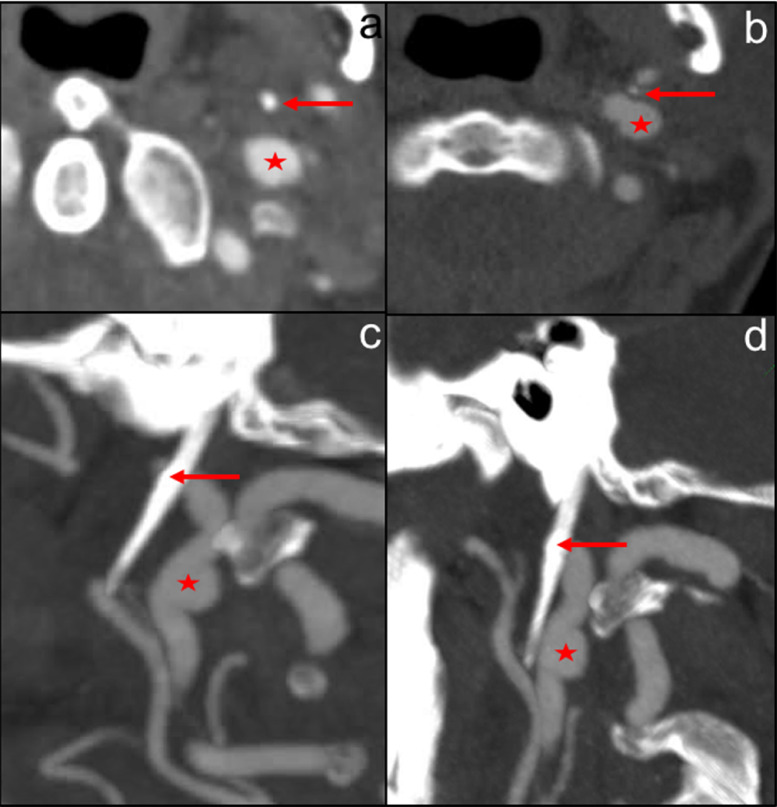
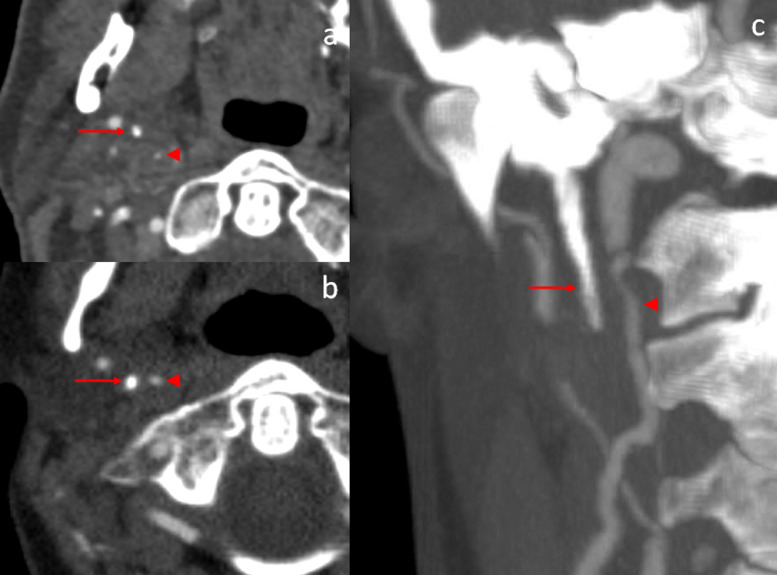
It clearly showed a bilateral impingement between the styloid processes (both measured at 31 mm) and internal carotids. Indeed, the right styloid tip projected exactly on the flap dissection and the left styloid tip was in front of the pseudoaneurysm (Figs. 3-4).
Fig. 3.
Left elongated styloid process tip (red arrow) and pseudoaneurysm (red star). Classical CTA dorsal decubitus acquisition without clear conflict in axial (a) & sagittal (c). Stress CTA (+/− 45° neck flexion) with impingement in axial (b) and sagittal (d). (Color version available online.)
Fig. 4.
Right elongated styloid process tip (red arrow) and true lumen of internal carotid dissection (red arrow head). Classical CTA dorsal decubitus acquisition without clear conflict in axial (a). Stress CTA (+/− 45° neck flexion) with impingement in axial (b). Dissection of the right internal carotid artery in coronal on maximal intensity projection (c).
In addition, the dissection of the right internal carotid was responsible for the acute ischemic stroke due to an insufficient residual flow. Retrospectively, the first episode 2 weeks earlier, could be secondary to a nonocclusive dissection with release of microemboli. This pauci-symptomatic dissection then worsened in the absence of adequate treatment.
Anticoagulation therapy was administered and a 6 months follow-up was suggested.
Functional recanalization was obtained on the 3 months control CTA. On the other side, the pseudoaneurysm remained stable at 3 and 6 months. Surgery was considered, with an experimented team, but was delayed to a 1-year follow up to evaluate the stability of the pseudoaneurysm.
Discussion
Eagle syndrome is rare. Moreover, the vascular impingement with bilateral vascular injuries was never described.
It seems important to know that Eagle syndrome may lead to disabling diseases or even death as well as an ischemic stroke [3].
Eagle syndrome is diagnosed by anamnesis, a thorough clinical examination and imaging.
CTA with 3D reconstructions demonstrates the relationship between the styloid process and the surrounding structures.
One of the potential causes of this clinical presentation is repeated anteroposterior movements resulting in an impingement of the styloid processes against the internal carotids.
While pseudoaneurysm is related to chronic traumatisms, the dissection appears to be a consequence of an acute traumatism secondary to severe coughing related to an acute bronchitis (with violent anteroposterior movements of the head).
In our case, ischemic stroke was caused by the right internal carotid dissection and was treated by anticoagulation.
Treatment should be discussed only if the aneurysm grows. Indeed, there are no large data on extracranial stenting of the internal carotid and furthermore stent fractures were described [4]. Surgical styloidectomy must be considered to reduce the risk of new vascular events [5]. Intraoral and external cervical approaches are both acceptable techniques with a better exposure, a better bleeding control and fewer postoperative airway edema for the latter, but with the disadvantage of leaving a scar and the risk of a facial nerve branch injury [2,6].
Conclusions
Identifying patients at risk of vascular impingement is important considering the potential complications.
To our knowledge, our “stress-acquisition CTA” to reveal the stylocarotid impingement has never been described before. This approach could lead to a new investigation technique, to better identify this underestimated pathology in the medical doctors’ community.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Eagle WW. Elongated styloid process: symptoms and treatment. AMA Arch Otolaryngol. 1958;(67/2):172–176. doi: 10.1001/archotol.1958.00730010178007. [DOI] [PubMed] [Google Scholar]
- 2.Badhey A, Jategaonkar A, Anglin Kovacs AJ. Eagle syndrome: a comprehensive review. Clin Neurol Neurosurg. 2017;159(May):34–38. doi: 10.1016/j.clineuro.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Fusco DJ, Asteraki S, Spetzl RF. Eagle's syndrome: embryology, anatomy, and clinical management. Acta Neurochir (Wien) 2012;154(7):1119–1126. doi: 10.1007/s00701-012-1385-2. [DOI] [PubMed] [Google Scholar]
- 4.Hooker J, Joyner DA, Farley EP, Khan M. Carotid Stent fracture from stylocarotid syndrome. J Radiol Case Rep. 2016;10(6):1–8. doi: 10.3941/jrcr.v10i6.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogura T, Mineharu Y, Todo K, Kohara N, Sakai N. Carotid artery dissection caused by an elongated styloid process: three case reports and review of the literature. NMC Case Rep J. 2015;2(1):21–25. doi: 10.2176/nmccrj.2014-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Papadiochos I, Papadiochou S, Sarivalasis ES, Goutzanis L, Petsinis V. Treatment of Eagle syndrome with transcervical approach secondary to a failed intraoral attempt: Surgical technique and literature review. J Stomatol Oral Maxillofac Surg. Elsevier Masson SAS. 2017;118(6):353–358. doi: 10.1016/j.jormas.2017.06.017. [DOI] [PubMed] [Google Scholar]