Editor:
The current 2019 novel coronavirus disease (COVID-19) pandemic has had an obvious global impact; this includes a major disruption in medical training. Across most medical specialties, including radiology, there have been significant reductions in case volumes (1). Fellows and residents have been reallocated to services outside their specialty to assist with COVID-19 patient care, and in-person educational conferences have been canceled, possibly compounding the loss of experience.
In disciplines such as interventional radiology (IR), where the majority of clinical and technical training currently occurs in a single fellowship year, there are concerns regarding disruptions in training leading to deficiencies in competency. COVID-19 began affecting US hospitals starting in the latter half of this academic year, a time when fellows are typically starting to perform cases autonomously as the primary operator—an important stage of training when they develop independence, aptitude, and confidence in preparation for independent practice. Fellows have attested that reductions in volume in practices across the United States has negatively impacted their employment; some have been unable to find work, while others are furloughed or receiving reduced compensation. Lower case volumes may also affect Early Specialization in Interventional Radiology, as trainees may not meet necessary rotation and case requirements, especially in the context of possible Core Exam cancelations (2). As surges in COVID-19 infections may reoccur on an annual basis, information relating to deficiencies in training and employment is invaluable in helping to prepare for future years.
To characterize losses in training, effects on employment, and the overall perception of how the IR fellowship in the United States has been disrupted by COVID-19, fellow- and program director (PD)–specific surveys were administered. This study was exempt from institutional review board approval. Voluntary electronic surveys were open to all IR PDs and current 2019–2020 IR fellows. Surveys were posted on the Association of Program Directors in Interventional Radiology Forum on May 20, 2020, and shared until closure on June 12, 2020. In total, 46 fellows (22% of 212 nationally) and 25 PDs (33% of 75 nationally) responded to the survey (3).
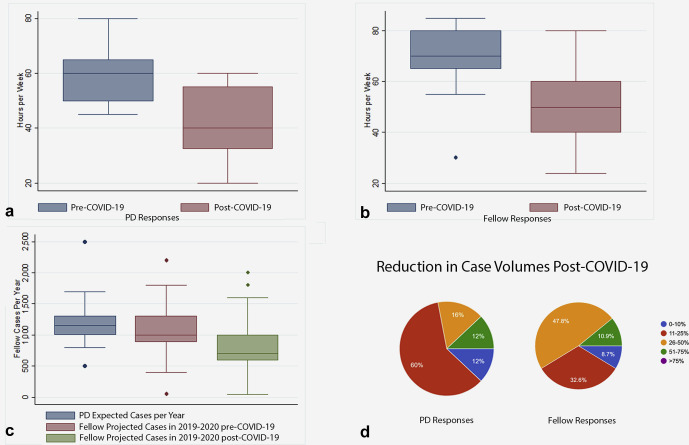
Survey data indicated that there were significant disruptions in training and markedly reduced case volumes compared with previous years (Fig 1a, b ). Most (87%) hospitals began taking precautions against COVID-19 in March 2020, with nearly all (97.8%) programs postponing or canceling elective cases. In addition, 15.6% of IR fellows were asked to participate or assist in care of patients with COVID-19 not related to radiology (interventional or diagnostic). On average, fellow weekly work hours decreased from 69 to 51 (Fig 2a, b ). PDs reported that fellows complete 1,211 cases on average per year; however, responding fellows noted that they were projected to complete only 843 this year owing to COVID-19 (Fig 2c). IR department total case volumes were decreased compared with previous years, and only a minority of responders reported minimal (0–10%) losses in volume (Fig 2d). In terms of education, more than half of respondents noted less in-house service, didactics, and conferences and that all in-person educational events were switched to an online platform.
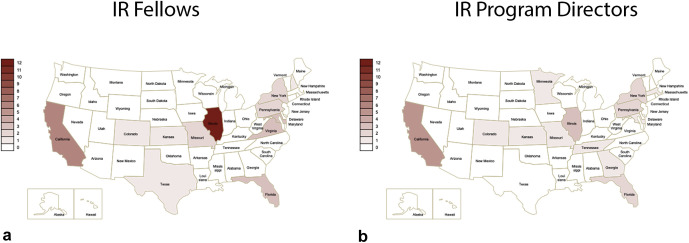
Figure 1.
(a, b) Geographic survey heat map for survey responses.
Figure 2.
Reductions in fellow training by hours worked and case volumes due to COVID-19. (a) Reported number of hours per week by PDs. (b) Reported number of hours per week by fellows. (c) PDs reported the number of cases they expected fellows to complete in 2019–2020 based on prior years (blue). Fellows self-reported how many cases they expected to complete at the end of the year before COVID-19 (red) and after COVID-19 (green). (d) Reduction in IR department overall case volume as reported by PDs and fellows.
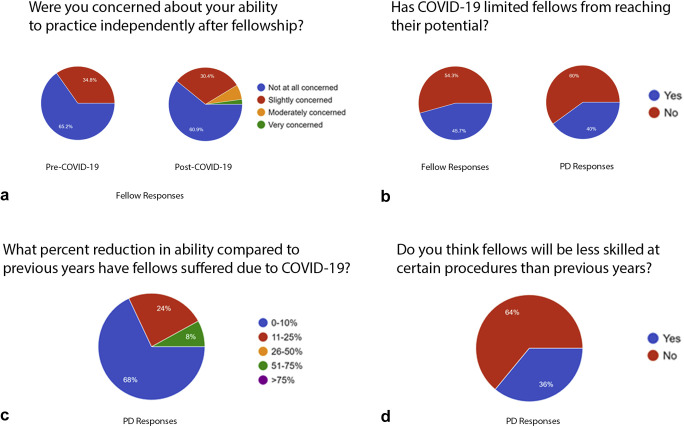
More concerning was that 2 (9%) PDs noted that their fellows would not be able to complete their fellowship on time, and an additional 2 (9%) responded that it is still unclear whether or not fellows will complete training at the conclusion of the academic year. PDs responded that before COVID-19, they had no concerns regarding their fellows’ ability to practice independently; however, after the recent disruptions in training, 4% responded that they were “slightly” concerned, and an additional 4% were “moderately” concerned. When asked to self-assess their readiness to practice independently next year, fellows reported higher rates of concern compared with before COVID-19 (Fig 3a ). Forty percent of PDs and 46% of fellows responded that recent disruptions in training have impeded trainees from “reaching their potential” (Fig 3b). Several PDs also responded that current fellows may have suffered reductions in skill compared with prior fellows due to COVID-19–related disruptions (Fig 3c). Thirteen percent of PDs responded that the current fellows will not graduate with the same skill set, or breadth of cases that could be performed independently, compared with typical graduates from previous years. An even greater percentage of PDs (70%) noted that fellows would be less skilled at performing certain procedures, specifically citing elective and complex cases such as transjugular intrahepatic portosystemic shunt, interventional oncology, complex venous and hepatobiliary procedures, and uterine fibroid embolization/prostatic artery embolization (Fig 3d). As IR departments add new junior faculty, these procedures may be key target areas where more senior staff can offer additional mentorship and guidance to their junior colleagues. Despite this, all surveyed PDs and fellows were confident that graduates would be competent IRs at the completion of fellowship.
Figure 3.
(a–d) Assessment of fellow competency.
In addition to educational losses, almost 30% of fellows responded that their employment for the upcoming year was negatively impacted by the pandemic. Deferred job start dates were reported by 19.6% of fellows, and reductions in compensation were reported by 20%. Approximately 10% of fellows did not have a job offer at the time of the survey, and an additional 10% did not have a signed job contract. Job hunting amidst the reductions in demand is increasingly challenging, and these data may provide important insight to incoming fellows starting their employment search.
The main limitation to these data is the survey nature of the study. Response biases may skew results toward individuals who were most affected by the COVID-19 pandemic, while social desirability bias may result in underreporting of disruptions in training or exaggeration of expected case volumes.
In summary, this survey indicates that the COVID-19 pandemic has had a major negative impact on IR training and employment. As hospitals across the United States begin to adapt to the world after COVID-19, methods to optimize training in Early Specialization in Interventional Radiology and integrated IR/diagnostic radiology training pathways need to be determined to maintain the development of excellent IR physicians and in turn ensure a bright future for our specialty.
Footnotes
R.J.L.’s E-mail: r-lewandowski@northwestern.edu; Twitter handle: @nicholas_s_xiao
None of the authors have identified a conflict of interest.
References
- 1.Cavallo J.J., Forman H.P. The economic impact of the COVID-19 pandemic on radiology practices. Radiology April 15, 2020. https://pubs.rsna.org published online. [DOI] [PMC free article] [PubMed]
- 2.Society of Interventional Radiology IR Training Pathways. https://www.sirweb.org/learning-center/ir-residency/ir-training-pathways-table/ Available at:
- 3.National Resident Matching Program, Results and Data: Specialties Matching Service 2020 Appointment Year National Resident Matching Program, Washington, DC. 2020. https://mk0nrmp3oyqui6wqfm.kinstacdn.com/wp-content/uploads/2020/02/Results-and-Data-SMS-2020.pdf Available at: