Abstract
Background
Patients with psychiatric illnesses are particularly vulnerable to highly contagious, droplet-spread organisms such as SARS-CoV-2. Patients with mental illnesses may not be able to consistently follow up behavioral prescriptions to avoid contagion, and they are frequently found in settings with close contact and inadequate infection control, such as group homes, homeless shelters, residential rehabilitation centers, and correctional facilities. Furthermore, inpatient psychiatry settings are generally designed as communal spaces, with heavy emphasis on group and milieu therapies. As such, inpatient psychiatry services are vulnerable to rampant spread of contagion.
Objective
With this in mind, the authors outline the decision process and ultimate design and implementation of a regional inpatient psychiatry unit for patients infected with asymptomatic SARS-CoV-2 and share key points for consideration in implementing future units elsewhere.
Conclusion
A major takeaway point of the analysis is the particular expertise of trained experts in psychosomatic medicine for treating patients infected with SARS-CoV-2.
Key words: infectious disease, respiratory disorder, mental health, consultation-liaison psychiatry, infection control
Background
Modern inpatient psychiatry is different from medical and surgical inpatient services in several ways. Psychiatric units are designed to be therapeutic communities that provide “milieu therapy” providing a normalizing, structured day. They have communal spaces for group therapies, social and recreational activity, and meals. Patients are encouraged to be up and out of their rooms throughout the day, participating in the milieu. Many units begin and end each day with a community meeting when patients and staff share their goals and progress. When safe, patients are encouraged to wear their own clothing rather than hospital attire, as long as it is not disruptive to the community (e.g., not provocative, sexually or socially inappropriate). In contrast, patients in general hospital rooms wear hospital gowns, mostly stay in bed, and eat in their rooms. Medications are brought to them in bed. They are taken around the hospitals for tests, therapies, and procedures, at least at first. This promotes rest and focus on physical recovery. Psychiatry recovery focuses on resumption of autonomous direction of activities, through participation in a normal day of work (therapy) with relaxing engagement in social activity.
Furthermore, many psychiatrists today specialize in the care of patients with comorbid psychiatric and medical disorders. The branch of psychosomatic medicine encompasses not only experts in consultation-liaison (C-L) psychiatry but includes subspecialists in psycho-oncology, HIV psychiatry, hepatitis psychiatry, perinatal psychiatry, and functional gastroenterologic disorders, to name a few. These C-L and subspecialty psychiatrists often undergo extra fellowship training and board certification and are well suited to care for complex patients with medical and psychiatric comorbidities. In addition, some hospitals have developed special medical psychiatric units to manage acute patients with comorbid disorders. The models vary somewhat but typically involve some form of comanagement process with psychiatric and somatic providers, as well as specialized nurse training to manage patient comorbidities. In this era of integrated care and services, such units, and the specialists who staff them, provide key resources to the health care system.
Challenges in the Care of Psychiatric Inpatients Infected With SARS-CoV-2
With this background in mind, it is easy to see how a highly contagious, droplet- and contact-spread virus, such as SARS-CoV-2, could run rampant through a standard psychiatric unit.1 , 2 Personal isolation is antitherapeutic to many psychiatric illnesses such as depression and schizophrenia. Patients with severe psychotic and manic disorders are vulnerable to inappropriate behaviors, such as intrusiveness and disregard for behavioral rules such as wearing a mask or hand washing. Removal of therapy from the environment in psychiatry would eliminate a significant aspect of recovery, relying only on medications to treat illnesses. Although medications are often necessary for recovery, without the practice of new thoughts and skills, recovery is incomplete. As such, when confronted with the care of psychiatric inpatients infected with SARS-CoV-2 but asymptomatic of its illness, the idea of closing or significantly changing inpatient psychiatry services, or treating such inpatients in medical units, was not accepted at our institution. Instead, we sought to preserve our established methods of treating patients, while finding a way to reduce or eliminate the threat of contagion.
As soon as tests were available, all hospital patients in our system with coronavirus disease-2019 (COVID-19) symptoms were being tested, either in emergency departments or on inpatient medical units. Everyone who tested positive for viral RNA was admitted to an inpatient medical unit. At first, our psychiatry inpatient focus was monitoring for symptoms and preventing the spread of infection, transferring symptomatic patients to medicine units to be ruled out or treated. We attempted to create distances between psychiatric inpatients by implementing single occupancy rooms where possible, moving from family style to tray meals, and moving furniture in our day areas so that they were placed 6 feet apart. We adopted novel practices, such as shared online rounding, with the doctor and patient in one room and staff in their individual offices connected by synchronous video. We began requiring all staff and patients to wear face masks, to avoid droplet spread. These were improvements, but as patients and clinical staff share many spaces at different points in time, we still risked exposure, especially between cleanings of common areas and items. To prevent COVID-19 outbreaks in our units, we next decided to require universal nasal swab testing for SARS-CoV-2 for all medically asymptomatic patients being admitted to psychiatric units.3
With universal testing, 2 challenges remained. First, false negative tests do occur, usually because of inadequate sample collection. We thought that the rate of this was low enough that with frequent symptom screening, distancing, masking, and systematic cleaning, we would likely have safe environments. Second, we realized that we needed to decide where to care for patients with mental illnesses and positive for asymptomatic SARS-CoV-2 who required hospitalization – those without symptoms of COVID-19. One option was to admit such patients to medical units in negative pressure rooms and provide medications and virtual therapies via our consultation services.4 Although attractive, this idea had a few problems. Our patients would be taking up negative pressure rooms best assigned to patients with COVID-19 who required medical care. Furthermore, medical unit COVID-19 rooms are not “psychiatrically safe” as most have many ligature points that would require 1:1 oversight with all patients to mitigate the risk of self-injury. We also faced a legal challenge: our legal team informed us that in Maryland, it is unlawful to involuntarily commit a patient to a “medical bed.” Although we could not find a specific statute prohibiting involuntary psychiatric commitment to a medical facility, we found other language saying that practices involving committed patients do not pertain to facilities without specific psychiatric treatment units.5 Thus, inpatient medical admission can only be an option for voluntary patients. If they chose to leave against medical advice, we would not have a good legal way to detain them for psychiatric care. Some of us argued that it could be declared that the patient lacked capacity to decide to leave and we could detain them. Besides being legally questionable, this argument fell flat because we have a strong commitment to patients’ autonomy and use involuntary certification as a last resort. As such, we had strong opinion against anything that would expand involuntary treatment without due process to protect patient rights and autonomy.
Creation of a Psychiatric Inpatient Unit for Patients Infected With SARS-CoV-2 and Without COVID-19
In light of the above, we concluded it would best serve our patients if we developed an inpatient psychiatric unit capable of accepting patients infected with SARS-CoV-2 and without COVID-19 symptoms or with mild enough symptoms that they would not require medical hospitalization (see Table 1 ). The next question was where in our system to do this and what resources would be required. As the unit would have to be able to accept involuntary patients, only 2 of our hospitals, Johns Hopkins Hospital and Howard County General Hospital, were eligible sites – Johns Hopkins Bayview Medical Center, Suburban Hospital, and Sibley Memorial Hospital are voluntary only for psychiatric admissions and do not have the ability to hold administrative law hearings on site.
Table 1.
Design and Implementation Decision Points for Developing a COVID Psychiatry Unit
|
COVID-19 = coronavirus disease-2019; PPE = personal protective equipment.
As we developed our thoughts as to how to design and implement this unit, we contacted colleagues around the country to see if anyone else was taking this approach. In late March, we only found 1 source in Israel. We sought guidance from Dr. Mark Weiser, head of the psychiatric division of Sheba Medical Center Tel HaShomer in Tel Aviv, Israel. Dr. Weiser had opened a psychiatric unit at his hospital to receive patients infected with SARS-CoV-2 and patients without COVID-19 from all other hospitals in Israel,6 just as we sought to do for Maryland. That unit was designed rapidly, with safety in mind, and an emphasis on minimizing staff presence on the unit to decrease exposures. He detailed for us the installation of cameras in all rooms to monitor patients for decompensation, and a remote ability to lock a patient's room door, allowing staff time to don personal protective equipment (PPE) and to be able to enter and intervene for an acutely agitated patient. We also discussed use of medications for these patients, and our mutual idea was to try to get to full doses of medications as quickly as safely possible, to avoid outbursts, especially in patients with psychotic and manic disorders.
Fortuitously, Howard County General Hospital had just opened a new psychiatric unit, with major safety and cosmetic upgrades. In so doing, the old 20-bed unit had been decommissioned and had not yet been remodeled into something else but had undergone renovations in the year before mitigating ligature risk. It has 10 semiprivate rooms and was a medical unit before a psychiatry unit, thus having available oxygen and suction in all rooms. It has a large day room for groups and activities, and there is a sally port (air-lock type) entrance with 2 sets of double doors providing security for visitors and space to prepare before entry into the unit.
After discussion, we decided that the old unit at Howard County would become the site for the Johns Hopkins inpatient psychiatry unit for patients infected with SARS-CoV-2 and without COVID-19. We would have 1 bed per room to begin, expanding as necessary to meet need, with a maximum of 20 patients.
Unit Design
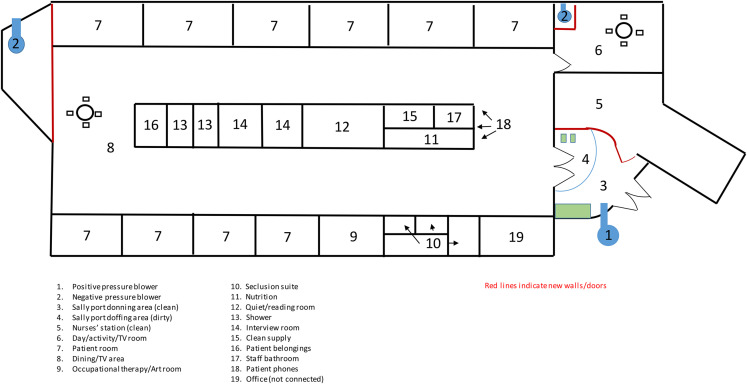
For most medical units treating droplet-borne contagious illnesses, negative pressure rooms are the norm. To ensure droplet precautions, providers don PPE, that is, mask, face shield, gown, and gloves, in the hallway, enter the room, provide service, doff gown and gloves, exit the room, and have assistance with wiping hard surface equipment, that is, face shields, from a safety officer in the hallway. For our psychiatry unit, we wished to normalize behaviors. To this end, we decided to make the entire unit a negative pressure space and use the sally port entrance as the donning/doffing area for staff (see Figures 1 and 2 ). This was accomplished by our engineering department in a matter of days. Three large blowers were installed. The first blows air into the sally port area, making it a positive pressure clean space. Any droplets on the new unit would be kept from entering by positive pressure behind the doors. This area was divided into a “clean” and “dirty” side, so that donning PPE happens on the clean side before entry, whereas doffing takes place on the dirty side after exit. A safety officer is stationed in the space to assist with donning, doffing, and cleaning.
Figure 1.
Unit schematic (not to scale).
Figure 2.
Sally port area. Donning area to the right of blue line, doffing area to left of blue line.
The second and third blowers were installed at the ends of the unit, each blowing air outside through windows that were converted to vents. These blowers are secured behind vented walls. In this way, airflow from the unit itself is vented outside to dissipate to a very low transmission density, and the entire unit becomes a negative pressure space, including the rooms, hallways, showers, and the day room/activity space.
It is important to note here that with this design decision, the unit would accept only patients infected with SARS-CoV-2 and not patients awaiting SARS-CoV-2 test results, so called patients under investigation. Placing a patient under investigation in the space might expose them to SARS-CoV-2, so we have to have a positive nasal swab result before the patient arrives.
The nursing station, being attached to the sally port, was maintained as a positive pressure, clean space. This allows staff to wear only standard precautions in the clean space, which is a surgical mask, without face shield or other eye protection. In the nursing station, medications are kept in the dispenser machine; there are several workstations for documentation, and there is a break room for rehydration and snacks. In the negative pressure space on the unit, there is a single workstation on wheels, for documentation by the nurse on the unit.
Unit Staffing
As wearing PPE for long periods of time is uncomfortable and adds stress to staff, it was decided to staff the unit with enough nurses that they could swap out after every 2 hours of being on the unit – 2 hours in and 2 hours out. Our standard nurse-to-patient ration is 1:6, so we staffed for 6 beds to start – even though we have 10 rooms – with 2 nurses, 1 patient care technician, and 1 security guard. Security typically sits in the nursing station, while the nurses and technician take turns entering the unit with the patients. Security is trained in donning PPE quickly to respond to urgent issues.
As we have only 4 psychiatrists and 1 psychiatric nurse practitioner at Howard County General Hospital and we still have to staff our other inpatient unit, our consult service, our outpatient clinic, and provide support to the Emergency Department, we chose to staff the COVID unit with a single dedicated psychiatrist with a plan for backup with psychiatrists from our other hospitals if needed. To best support the staff through this effort, the Howard County General Hospital department chair (A.A.) decided to personally attend to patients on the unit, following the idea that leaders go first in difficult tasks. Furthermore, so as not to overburden other weekend call providers and to provide continuity, we chose to have the same psychiatrist cover COVID unit rounds on the weekend.
We had a discussion about the best ways to see patients in “hot zone” areas. Other systems had elected to remove the psychiatrist from the in-person experiences, opting to use telehealth solutions exclusively. Although we have adopted use of telepsychiatry for seeing some patients on the consultation service who have COVID-19, the method is problematic at times. Some patients cannot keep the camera on themselves, there are frequent volume issues with microphones and speakers and less frequently, connectivity problems disrupt the flow of conversation. One advantage to telepsychiatry is that the provider can be in an area where s/he can remove the mask, allowing the patient to see a human face with all its expressions.
A second point, however, relates to the division of labor and risk among members of the treatment team. Having providers exclusively use telepsychiatry while nurses and technicians have to wear PPE to enter the infectious area created a discussion for us about fairness. Ultimately, we decided for our inpatient COVID unit, providers would use PPE and round inperson on the patients daily, as on our other inpatient psychiatry units.
Thinking about the patients' needs, we realized that a high degree of medical sophistication would be necessary for daily assessments. Our department is fortunate to have expert trained and certified psychosomatic medicine psychiatrists, with experience in managing patients with serious mental and physical comorbidities. As we wished to describe the staffing needs for this article, we thought about how best to convey this to other systems needing to develop such a unit. We recommend that the psychiatrists and nurses staffing the unit be well versed in the assessment and treatment of COVID-19 disease and have a high comfort level with physical examination and provision of medical treatments, such as oxygen, fluids, and coagulation prophylaxis, to best serve patients with mild disease in situ on the psychiatry unit. Furthermore, it is highly beneficial for continuity of care if the patient requires transfer to a medical COVID-19 unit that the psychiatrist be able to follow up them there and maintain the psychiatric treatments as indicated. Thus, the COVID psychiatry inpatient unit should be the equivalent of a medical psychiatry unit, with the ability to manage mild COVID-19 disease, and the gold standard for psychiatrist staffing is a trained psychosomatic medicine or C-L psychiatrist who has knowledge of COVID-19 disease. Our initial staffing plan with the chair at Howard County General demonstrated this, as he is a specialist in HIV and hepatitis psychiatry and C-L psychiatry, and thus, he is able to provide the medical expertise needed to effectively manage these patients.
Patient assessment for transfer to the COVID inpatient psychiatry unit also involves a degree of expertise about COVID-19 disease. In our system, 1 expert C-L psychiatrist assesses all requested transfers to determine the level of care required on the unit. Some medically hospitalized patients with COVID-19 may be physically recovering from the respiratory illness and require psychiatric intervention for a separate mental illness. While there is some information that such patients may no longer be infectious, we suggest either viral load testing if it is available or the recent practice of 2 negative nasopharyngeal swab tests 24 hours apart if they are to be transferred to a regular psychiatry unit.7 It is our practice that if the patient has a positive nasopharyngeal swab test, they be admitted to the COVID psychiatry inpatient unit to prevent any chance of spreading virus to noninfected patients and staff. Furthermore, some patients develop a protracted delirium after serious COVID-19 illness, especially if a long intubation and intensive care unit stay was involved, and a trained C-L psychiatrist would best be suited to assisting in the treatment of these patients on the medical unit, rather than transferring them to inpatient psychiatry.
Personal Protective Equipment
The infection control experts recommend several options for PPE. In areas with many SARS-CoV-2–infected persons, we can choose between N95 or Drager masks, with a face shield, or a Powered Air Purifying Respirator (PAPR) hood. We were test-fitted for N95 and Drager masks and trained on PAPR use. All persons wear a gown and 2 pairs of gloves, 1 under the gown sleeves and 1 over.
There is a process for donning and doffing. The first decision is mask + face shield or PAPR. The PAPR can be worn without a mask, allowing the patient to see the provider's face, which we think is comforting to psychiatric patients, so we most often use PAPRs on the unit. However, there was concern that if a patient becomes violent, during the response to the violence, a clinician might have the PAPR torn off, exposing the face openly if no mask is worn underneath. Thus, some staff members in some situations wear a PAPR with a mask and glasses underneath. This approach is also used on Dr. Weiser's unit in Israel.
On the subject of violence with PPE, we have several different options for gowning. Most common and cost efficient are yellow paper gowns, often worn by providers making quicker visits to the unit to see patients, such as the rounding psychiatrist. Nurses and technicians, who spend more time on the unit, often wear surgical gowns that provide more coverage around the body and are more tear-resistant should a physical hold be necessary. Finally, we have tear-resistant jumpsuits, most worn by security who have the most hands-on in a violence situation.
A final word about PPE. It is very difficult and far higher risk for an individual to don and doff PPE without help, especially for the wiping down after exiting the unit or room. This requires extra staff to be present. Furthermore, as mentioned previously, we staff 2 nurses per 6 patients, rather than 1, so as to be able to give relief to the nurse wearing the PPE – this was performed in 2-hour shifts as PPE is very uncomfortable to wear for periods longer than 2 hours. It is also important to remind staff to maintain hydration once they are out of PPE, as they do not have the ability to take fluids while on the unit in PPE.
Communication, Medications, and Supplies
We have ASCOM phones for nursing staff. One phone is handed off from nurse to nurse inside the unit. For quick communications, we have a small white board and dry-erase marker to share messages through the window to the nurses' station. Most longer communications are from the ASCOM phone to the landline in the nursing station.
Medications, meals, snacks, and supplies are passed through the entrance to the unit by the safety officer. There is no donning, but the safety officer wears a mask and shield at all times and uses gloves to pass objects through the entrance. We use disposable items – meal trays, utensils, and scrubs – as much as possible for patients. Linens are handled in the normal way. We allow patients to wear some regular clothes, provided they are safe and the patient is clinically OK to do so. There is a washer and dryer on the unit for patients' personal laundry. We have iPads on the unit, encased in strong protective cases, for patients to have video visits with providers and family members and to watch videos or play games. These are swapped out when they need to be charged and wiped down by the safety officer in the sally port before and after charging. The unit has television, and a video game system can be attached for recreation.
Activities and Groups
The most challenging aspect of care is the provision of anything other than 1:1 therapy. We do not have occupational therapy providers on the unit, and we have only 1 nurse at a time, so there is no one available to lead groups. Patients with alcohol and drug problems attend online meetings using iPads. For 1 patient who was struggling with coming out as gay to his family, we were able to find online support groups through an Lesbian Gay Bisexual Trans Queer support organization's website. We are investigating using video connections to the groups already happening on our other inpatient unit, but as of this writing, the logistics are not fully worked out. We have had several art/craft sessions led by our patient care technicians.
Activities are easier to accomplish. We have games and puzzles for patients, and staff members assist in playing them. We allow patients to watch online content on iPads, provided it is appropriate, and there is a room. There is a phone bank so patients may call family. We do not allow inperson visitors at this time.
Involuntary Patients Process
As mentioned previously, we have a unit that accepts both voluntary and involuntary patients. According to Maryland law, involuntary patients must have a hearing with the Administrative Law Judge to determine commitment to treatment within 10 days of admission. For both our regular psychiatric units and our COVID unit, these hearings are currently conducted via secure video conference. The public defender meets with the patient via video conference before the hearing to prepare a position, and the hearing is conducted via group video conference.
Medical Monitoring
We monitor vital signs every 6 hours, including pulse oximetry. Nurses screen thrice daily for cough, shortness of breath, chest pain, nausea, and vomiting. Every patient has a physical examination by an internist, laboratory testing for coagulopathy and inflammation, and follow-up daily by the internist. Our observation thus far has taught us that serious COVID-19 symptoms usually arrive in the first week of infection, and our only transfer out of the unit to medicine happened 4 days after his positive test. Most patients have been completely asymptomatic on the unit, whereas a few have developed mild complaints of cough or subjective shortness of breath. We manage mild complaints symptomatically and have the ability to provide oxygen on the unit. Our medical colleagues are invaluable in determining which patients are sick enough to require transfer to a medical bed – usually this takes the form of an oxygen requirement beyond 2 L by nasal cannula. All other medical care is as usual, with a general rule of thumb being that we manage any chronic medical illness that would be managed as an outpatient, for example, controlled hypertension, controlled diabetes, and so on.
One area that is a bit tricky is the monitoring of patients requiring detoxification from alcohol or opioids on the unit. We provide active withdrawal protocols, using benzodiazepines for alcohol withdrawal and buprenorphine for opioid withdrawal, and in general, monitor vital signs and symptoms closely, concentrating on respiratory symptoms and pulse oximetry to guide intervention for COVID-19.
Discharges
There are 3 ways someone can be discharged from the unit. First and most undesirable, a patient is transferred to a medicine unit if she/he decompensates medically and requires acute medical attention beyond what is available on the unit. While we can provide oxygen, if the person requires >2 L of oxygen by nasal cannula, it is unsafe for him/her to stay on the unit where there is no medical provider nearby 24/7. We did have 1 patient so far leave this way, but he did well with medical treatment and returned to our unit after a few days on medicine.
Second, patients can be discharged if they get better psychiatrically and no longer require inpatient care. This proves challenging if they are still positive for SARS-CoV-2. Many placements, for example, group homes, assisted living facilities, residential rehabilitation facilities, shelters, and so on, require patients to be tested negative before they can enter. Some patients have homes to go to and are discharged home with instructions on maintaining quarantine until it is safe for them to stop – according to Centers for Disease Control (CDC) guidelines.8 Although this discharge-to-quarantine process has a different feel for the social worker arranging aftercare, there is actually not much difference in follow-up care. Many providers are using telepsychiatry visits, so we can get appointments while patients are still in quarantine. Intensive outpatient and partial hospitalization programs in Maryland are currently closed or providing only telepsychiatry options, so this does not differ for patients tested positive for SARS-CoV-2 from noninfected patients. Our only real concern was acquiring medications after discharge, as quarantined patients picking up prescriptions from a pharmacy proved a challenge. We address this by having a 2-week supply of medicines filled before discharge by our pharmacy and delivered to our unit so patients can leave with medications in hand. Transport home as well proves an issue. To decrease exposure of family members owing to close proximity on the ride home, we use a medical transport van that allows for distance from the driver and have the patient wear a mask at home. To sign discharge paperwork, we bring the patient into the sally port wearing a mask, ask them to put on gloves, have them sign the paperwork, and give them a copy. The hospital copy is kept in the nurses' station for 1 day in a secure area before being taken to Health Information Technology (medical records) to be scanned into the record, to decrease possible contamination.
Third, patients may be discharged is if they are on the unit long enough to clear SARS-CoV-2 virus and can be transferred to a regular psychiatric unit, a residential program, or group home or to their own home. We have had only one experience of a patient requiring continued psychiatric care after clearing the virus, and we have had a couple on the unit long enough to merit testing at time of discharge, who were discharged to group homes or programs after testing SARS-CoV-2 negative. We closely follow CDC guidelines as they are updated with new information, so as to best decide on timing of testing and how to handle patients with prolonged positive polymerase chain reaction results.
Staff Support
We are fortunate to have a very dedicated, highly experienced staff of physicians, nurses, patient care technicians, and security. All staff members work on the unit voluntarily. As mentioned previously, the chair of the department personally staffs the unit daily, which also was advised by Dr. Weiser in Israel, as it boosts morale to see leaders working alongside everyone.
We frequently check in with unit staff and the hospital as a whole, to be alert for signs of fatigue, stress, anxiety, and depression. On the whole, our psychiatry staff members are open about their feelings and well-being, as we have created an environment in which expressing such is safe from repercussion or retaliation. We focus efforts on recognizing everyone's vital contribution to the team and our interdependence on one another, creating trust in our culture that everyone is valued and will be supported in our efforts.
Our department has teamed with other support systems within the Johns Hopkins system, including our R.I.S.E program (Resilience In Stressful Events), which provides confidential, trained-peer support 24/7. In addition, our faculty and staff assistance programs provide professional counseling and psychotherapy treatments for our employees. Finally, the department of psychiatry added urgent appointments for psychiatric evaluation by faculty members for employees with more serious issues, including requirement for medications. In addition to this spectrum of care, 1 of our faculty implemented daily virtual mindfulness video conferences, available to all Johns Hopkins employees to participate. We have held video meetings with hospital managers from every department, presenting warning signs of burnout, and a tiered approach to referrals of employees for help.
Community support is widespread and tremendous. From meals and snacks to personal care products such as lotion for chapped hands, many individuals and organizations have contributed to staff support throughout the hospital. Staff members from nonisolation units and administrative areas have been very kind to deliver things to the isolation units for staff who cannot easily and safely get away to collect them from drop-off points.
Conclusion
We present this account of our efforts to inform those faced with a similar problem. When we opened the unit on April 21, 2020, we did not know of any similar units in the United States. We are now aware of several and have learned that their processes are very similar to ours. Most recently, an account of principles that guided the planning of a COVID + unit in California were published online.9 As the practices at our institution and those we have found are compared and discussed, best practices will be defined in this area and support the development and implementation of units everywhere they are required. We recommend that such a unit would be best implemented in a medical psychiatry unit, but if none is available, the unit would be best placed inside a general hospital that has ability to care for patients ill with COVID-19 should they become too acute to be managed safely on the inpatient psychiatry unit. Furthermore, we feel the gold standard of psychiatrist staffing for such a unit be a trained psychosomatic medicine psychiatrist with knowledge of COVID-19 illness, for reviewing appropriateness of patients referred for admission to the unit and for daily monitoring of psychiatric and medical signs and symptoms and management of mild COVID-19 illness.
Acknowledgments
The authors would like to thank Drs. Mark Weiser, Patrick Triplett, Karin Neufeld, Erica Richards, Cynthia Lewis and Ashley Bone, as well as Ryan Brown, Jennifer Baldwin, Angela McKay, Kelly Caslin, Laurie Burdock, Zahra Parva and Susan Webb for their contributions to this process.
References
- 1.Li L. Challenges and priorities in responding to COVID-19 in inpatient psychiatry. Psychiatr Serv Adv. 2020 doi: 10.1176/appi.ps.202000166. [DOI] [PubMed] [Google Scholar]
- 2.Kim M.J. 'It was a medical disaster': the psychiatric ward that saw 100 patients with new coronavirus. Independent. 2020 Available from: https://www.independent.co.uk/news/world/asia/coronavirus-south-korea-outbreak-hospital-patients-lockdown-a9367486.html. Accessed May 15, 2020. [Google Scholar]
- 3.Benson N.M., Öngür D., Hsu J. COVID-19 testing and patients in mental health facilities. Lancet Psychiatry. 2020 doi: 10.1016/52215-0366(20)30198-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fagiolini A., Cuomo A., Frank E. COVID-19 diary from a psychiatry department in Italy. J Clin Psychiatry. 2020;81:20com13357. doi: 10.4088/JCP.20com13357. [DOI] [PubMed] [Google Scholar]
- 5.Annotated code of Maryland. 2020. §10-701 (3) [Google Scholar]
- 6.Cautionary tale spurs 'world's first' COVID-19 psychiatric ward. Medscape. 2020 Available from: https://www.medscape.com/viewarticle/928880. Accessed May 25, 2020. [Google Scholar]
- 7.Wölfel R., Corman V.M., Guggemos W. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Discontinuation of transmission – based precautions and disposition of patients with COVID-19 in healthcare settings (interim guidance) Decis Memo. 2020 Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html. Accessed May 25, 2020. [Google Scholar]
- 9.Planning for a psychiatric COVID-19-positive unit. Medscape. 2020 Available from: https://www.medscape.com/viewarticle/930659. Accessed May 26, 2020. [Google Scholar]