Highlights
-
•
The true incidence of SARS-COV-2 is much higher than the reported number of cases.
-
•
Large sample size studies have shown 1.2–12.9% incidence of SARS-COV-2 among asymptomatic people.
-
•
Studies with a small sample size showed up to 87.9% incidence among asymptomatic people.
-
•
Asymptomatic individuals could be a potential source of infection to the community.
Keywords: COVID-19, SARS-CoV-2, Asymptomatic carrier, Viruses, Incidence
Abstract
Background
The recent outbreak of the coronavirus disease 2019 (COVID-19) has quickly spread globally since its discovery in Wuhan, China, in December 2019. A comprehensive strategy – including surveillance, diagnostics, research, and clinical treatment – is urgently needed to win the battle against COVID-19. Recently, numerous studies have reported the incidence of SARS-CoV-2 in asymptomatic patients. Yet, the incidence and viral transmission from the asymptomatic cases are not yet apparent.
Aim
To estimate the incidence of COVID-19 among asymptomatic cases and describe its epidemiological and clinical significance this review systematically examined the published literature on SARS-CoV-2 in asymptomatic patients.
Methods
The literature was searched through four scientific databases: PubMed, Web of Science, Scopus, and Science Direct.
Results
Sixty-three studies satisfied the inclusion criteria. The majority of the reported studies were from China. However, there was a lack of SARS-CoV-2 epidemiological studies, from several countries worldwide, tracing the actual incidence of COVID-19, especially in asymptomatic patients. Studies with a large sample size (>1000) estimated that the percentage of people contracting SARS-CoV-2 and likely to be asymptomatic ranged from 1.2–12.9%. However, other studies with a smaller sample size reported a much higher incidence and indicated that up to 87.9% of COVID-19 infected individuals could be asymptomatic. Most of these studies indicated that asymptopatics are a potential source of infection to the community.
Conclusion
This review highlighted the need for more robust and well-designed studies to better estimate COVID-19 incidence among asymptomatic patients worldwide. Early identification of asymptomatic cases, as well as monitoring and tracing close contacts, could help in mitigating the spread of COVID-19.
Introduction
Infectious diseases impose a major global health threat, leading to 15 million deaths annually (Fauci et al., 2005). Although the percentage of mortality due to infectious diseases has declined, numerous new infectious diseases have recently been identified and reported. The novel coronavirus disease (COVID-19), caused by the SARS-CoV-2 virus, was firstly identified in Wuhan, China, in late December 2019 as an outbreak of unusual viral pneumonia (Mousavizadeh and Ghasemi, 2020). Later, the World Health Organisation (WHO) declared a global public health emergency. The total number of infected cases reached 4.4 million by May 2020 (WHO, 2020). Consequently, educational institutions, business centres, public transport, and other social interactions were locked down to prevent the spread of COVID-19 and ease the burden on health facilities. SARS-CoV-2 is an enveloped positive-sense single-stranded RNA virus with six open reading frames that codes for structural proteins, including surface (S), envelope (E), membrane (M), and nucleocapsid N proteins (Khailany et al., 2020). Based on the genomic structures and phylogenetic analysis of SARS-CoV-2, the virus belongs to genera Betacoronavirus, which includes SARS-CoV and MERS-CoV. Yet, SARS-CoV-2 has differences in its genomic makeup that can influence its pathogenesis.
The most effective approach in preventing and mitigating the adverse consequences of this viral pandemic requires the development of effective surveillance programmes, incorporated with laboratory preparedness. Diagnostic laboratory tests play a significant role in the rapid and accurate detection of new viruses (Song et al., 2019, Parreira, 2018). Currently, real-time reverse-transcription polymerase chain reaction (RT-PCR) testing is the main technique used for the diagnosis of COVID-19. However, false-negative RT-PCR results occur in up to 30% of COVID-19 patients (Wikramaratna et al., 2020, Breslin et al., 2020, Qin et al., 2020). This could be due to the collection of inappropriate or insufficient sample, inaccurate conditions of sample transportation and storage, as well as collecting the sample too late in the disease process.
On the other hand, serology testing could cover this gap, since detecting SARS-CoV-2 IgG antibodies could indicate recovery or immunity from COVID-19 infection. Besides, IgM could be detected in the acute phase of infections. Although manual enzyme-linked immunoassay (ELISA) kits could be subjected to non-specific binding and cross-reactivity with other coronaviruses such as MERS-CoV and SARS-CoV-1, the most commercially available antibodies use lateral flow assays (Al Kahlout et al., 2019). However, ELISA and automated-based assays were also recently introduced. The diagnostic performance, including sensitivity and specificity, of these assays was better than lateral flow assays (Amanat et al., 2020). It worth mentioning that there is a high percentage of COVID-19 asymptomatic patients who could transmit the infection to all communities. For instance, the asymptomatic ratio of COVID-19 was estimated to be 41.6% of Japanese individuals who were evacuated from China (He et al., 2020). Similarly, 72% of people infected with COVID-19 on board the Diamond Princess cruise ship were asymptomatic (LSHTM, 2020). However, the extent of viral transmission from the asymptomatic cases is not yet clear. Positive RT-PCR results only imply potential infectivity. A prospective study was published on 28 March 2020, in which the viral load and clinical manifestations of 2147 close contacts of symptomatic and asymptomatic COVID-19 cases were followed up (Chen et al., 2020). The study concluded that the virus infection rate of close contacts with asymptomatic patients was 4.11%.
Since the transmission ability of asymptomatic individuals should not be ignored, it was interesting to conduct this systemic review to paint a picture of the current status and incidence of SARS-CoV-2 in asymptomatic patients. Therefore, this review provided significant insights into COVID-19 infection and could help health authorities to determine the need for social distancing close contact restrictions in specific areas or populations.
Methods
Search strategy
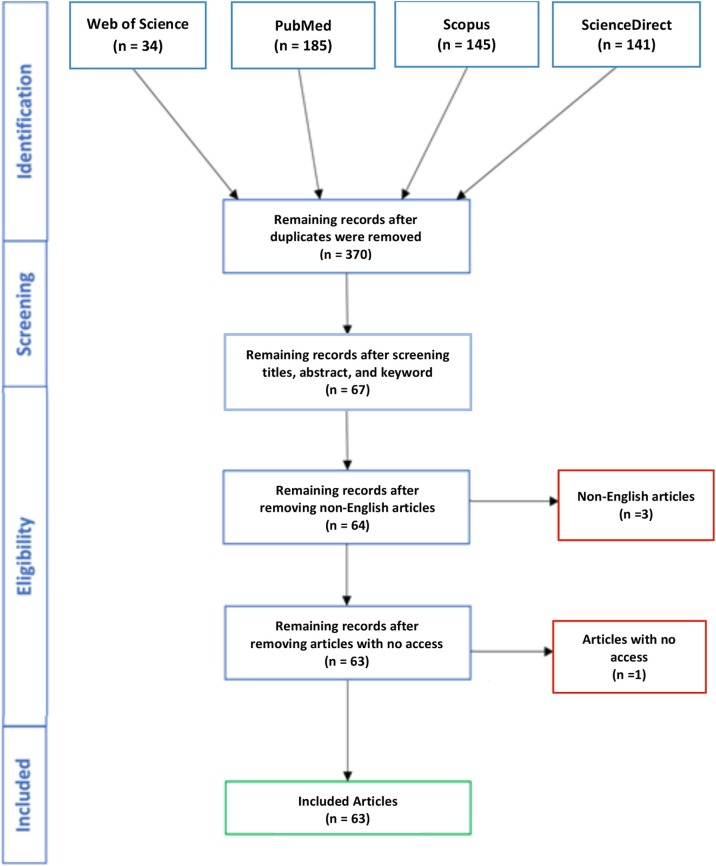
A systematic review of all literature published on COVID-19 in asymptomatic patients was performed using four databases: PubMed, Web of Science, Scopus, and ScienceDirect. The search covered all literature within the databases up to April 2020. The four databases were searched without filters with the keywords: “COVID-19”, “SARS-CoV-2”, “seroprevalence”, and “asymptomatic” to ensure complete coverage of all literature. Therefore, results that were letters and commentaries were also included. All retrieved citations were imported into Clarivate Analytics, Philadelphia, Pennsylvania, United States, and duplicates were removed using the Clarivate Analytics, Philadelphia, Pennsylvania, United States built-in ‘Find Duplicates’ feature. Finally, the titles and abstracts of the remaining citations were screened to remove any irrelevant articles.
Study selection
The following inclusion criteria were used in study selection: (i) published in a peer-reviewed journal, letters, case reports, and commentaries; (ii) articles studying the COVID-19 infection in asymptomatic patients; and (iii) articles published in English or at least with an abstract in English. A schematic of the search strategy and study selection process is shown in Figure 1. Studies that reported the coinfection of COVID-19 with other viruses as well as comorbidities, such as cancer and cystic fibrosis, were also included in this study. No exclusion criteria were followed unless the studies did not report the incidence of SARS-CoV-2 in asymptomatic patients, were published in a non-English language, or did not have full-text access.
Figure 1.
Flow diagram of the search strategy and article selection.
Data extraction and analysis
The studies included in this systematic review were analysed twice by the same individual to ensure accurate capture of the information. The analysed data included the incidence of SARS-Cov-2 in asymptomatic COVID-19 patients, incidence of COVID-19 infection, routes of transmission, laboratory diagnostic tests, laboratory results, as well as CT scan findings.
Results
Search findings
The search yielded 505 studies, of which 370 citations remained after removing duplicates (Figure 1). After screening the titles, abstracts and keywords, 312 citations were excluded. The removed citations included irrelevant studies. The remaining 67 citations were screened against the eligibility criteria. Of these, one study was removed due to the unavailability of full-text access. Furthermore, three studies were removed: two for being published in languages other than English with no English abstract. The remaining 63 studies were included in this study for further analysis, and they consisted of letters to the editor, commentaries, case reports, and research studies.
Epidemiological findings
The reviewed studies covered SARS-CoV-2 incidence worldwide. Country-wise, the majority of the studies were from China (n = 44) and included different provinces such as Wuhan, Shenzhen, Guangzhou, Beijing, Shanghai, Hunan, Nanjing, Guangdong, Anhui, Hubei, Zhejiang, Jinan, and Hefei (Table 1 ). The remaining studies were published in Japan (n = 2), Italy (n = 3), Germany (n = 1), Iran (n = 2), and USA (n = 6), which included studies from Texas, Washington and New York. However, there was a lack of SARS-CoV-2 epidemiological studies tracing the actual incidence of COVID-19, especially in asymptomatic patients from several countries worldwide.
Table 1.
Characteristics and summary data of the included studies.
| Country | Type of study | Total case number | Number of asymptomatic patients | Age/mean age | Gender | Clinical features | Chest CT findings | Reference |
|---|---|---|---|---|---|---|---|---|
| China (Guangzhou) | Correspondence | 295 | 45 (15.2%) | – | – | RT-PCR positive for SARS-CoV-2. Thirty patients started to show a few clinical symptoms after 3–14 days | Persistent negative CT findings. Fifteen were CT scan positive (after 3–6 days) for COVID-19 pneumonia | Ling et al. (2020) |
| China (Guangzhou) | Correspondence | 5 | 2 (40%) | 3-year-old male 33-year-old female |
1 male 1 female |
Normal lymphocyte counts. Positive qRT-PCR results |
Normal chest CT images | Pan et al. (2020a) |
| China (Guangzhou) | Research letter | – | 7 | Age range: 21–56 years | 4 males 3 females |
Positive for SARS-CoV-2 by RT-PCR | A 56-year-old showed multiple ground-glass-like high-density shadows on both lungs | Li et al. (2020) |
| China (Guangdong) | Research article (familial cluster) | 5 | 1 (20%) | 10-year-old | Male | RT-PCR positive for SARS-CoV-2. Lymphopenia, thrombocytopenia, and increased C-reactive protein and lactate dehydrogenase levels | Ground-glass lung opacities | Chan et al. (2020) |
| China (Wuhan) | Research article | – | 58 | The average age of patients was 42.60 ± 16.56 years old | 26 males and 32 females | After a short-term follow-up, 16 patients (27.6%) presented symptoms with lower lymphocyte count and higher CRP, mainly including fever, cough and fatigue | Ground-glass opacity in 55 (94.8%) with peripheral in 44 (75.9%). Distribution unilateral in 34 (58.6%) and mostly involving one or two lobes in 38 (65.5%) | Meng et al. (2020) |
| China (Wuhan) | Research letter (familial cluster) | – | 5 | 37-year-old wife 7-year-old fraternal twins 62-year-old grandfather 64-year-old grandmother |
2 females 1 male Twins gender not determined |
Throat swab specimens tested for SARS-CoV-2 were positive by PCR, except for one patient who tested negative on four consecutive throat swab specimen tests for SARS-CoV-2 but whose stool specimen was positive for SARS-CoV-2 | Abnormal chest CT scans showing features consistent with SARS-CoV-2 infection in one of the twins | Luo et al. (2020a) |
| China (Wuhan) | Case report | – | 1 (diagnosed as advanced lung adenocarcinoma) | 56-years | Male | RT-PCR of SARS-CoV-2 and IgM were negative, while his serological IgG antibody to SARS-CoV-2 was positive | CT scan was negative | Ouyang et al. (2020) |
| China (Wuhan) | Case report | – | 1 | 8-year-old | Female | No clinical symptoms or decreased lymphocyte count. Positive for SARS-CoV-2 IgG | Normal chest CT image | Jiang et al. (2020a) |
| China (Wuhan) | Research article | 1012 | 30 (3%) | The median age was 50 years (range: 6–89) | – | Positive RT-PCR for SARS-CoV-2. During follow-up from admission to the end, fever occurred in 6, with cough in 8, myalgia in 3, dyspnoea in 2, nasal congestion in 1, and abdominal pain in 1. Fourteen of 1012 patients (1.4%) remained asymptomatic during the whole follow-up | Small patchy opacities (38.7%) and ground-glass opacities (55.4%) | Wang et al. (2020a) |
| China (Wuhan) | Research article | 155 | 51 (33%) | – | – | Positive RT-PCR for SARS-CoV-2 | CT showed no signs of viral pneumonia | Wang et al. (2020b) |
| China (Hubei) | Letter to the Editor | – | 25 | Average age 42.2 years (range: 28–73) | 17 males 8 females |
16 of the patients recovered without any symptoms. Nine developed a mild cough and/or other symptoms | Two-thirds of the patients had involvement of a single lobe, and two-thirds had a ground-glass density shadow. The least common CT finding was interlobular septal thickening | An et al. (2020) |
| China (Hubei) | Case report | – | 1 | 3 months | Male | No nasal congestion, cough, shortness of breath, cyanosis, nausea, vomiting, and diarrhoea. Good mental response and crying sound. All blood, liver and kidney tests were normal. RT-PCR positive for SARS-CoV-2 | Chest X-ray showed a slightly thicker texture of the right lung | Zhang et al. (2020) |
| China (Shanghai) | Letter to the Editor | 328 | 13 (3.9%) | Mean age was 51.8 years (range: 25–80) | 6 males 7 females |
Leucocytes were below the normal range in two patients (15.4%). Ten patients (76.9%) had differing degrees of elevation of the ESR. Liver, renal and coagulation function were within the normal range. No fever. Positive RT-PCR for SARS-CoV-2 | A patient developed signs such as pneumonia on chest CT | Zhou et al. (2020a) |
| China (Nanjing) | Research article | – | 24 screened due to close contact with COVID-19 patients | Cases with symptoms after diagnosis (n = 5) 53.0 (range: 23.0–65.0) Cases without symptoms after diagnosis (n = 19) 32.0 (15.0–57.0) |
8 males and 16 females | Five cases (20.8%) developed symptoms (fever, cough, fatigue, etc.) during hospitalisation. Five (20.8%) presented stripe shadowing in the lungs. The remaining seven had no symptoms during hospitalisation.Four had C-reactive protein levels ≥10 mg/L |
Twelve (50.0%) cases showed typical CT images of the ground-glass chest | Hu et al. (2020) |
| China (Hunan) | Research article | 78 | 2 (2.5%) | 36-year-old 19-year-old |
Males | Positive RT-PCR for SARS-CoV-2. Patient 1: laboratory evaluation showed an elevated myoglobin, ALT, and uric acid level. Patient 2: laboratory tests including blood routine test, erythrocyte sedimentation rate, C-reactive protein and three items of myocardial enzyme spectrum were all negative | Chest CT scan was negative for both | Mao et al. (2020) |
| China (Guangdong) | Short communication | – | 3 | – | Patient 1: not determined Patient 2: female Patient 3: male |
No fever, cough and expectoration during hospitalisation | Patient 1: multiple patchy and ground-glass shadows with uneven density and fuzzy edges in the outer zone of both lungs | Lu et al. (2020a) |
| China (Anhui) | Short communication | – | 1 | 22-year-old pregnant woman | Female | No cough, dyspnoea or diarrhoea was noted | CT re-examination showed a small amount of pleural effusion on both sides | Lu et al. (2020b) |
| China (Zhejiang) | Research article (observational cohort study) | 36 | 10 (28%) | Age range: 0–16 years; mean 8·3 years | – | Decreased lymphocytes, high levels of procalcitonin, D-dimer, and creatine kinase MB | – | Qiu et al. (2020) |
| China (Hefei) | Prospective contact-tracing study | – | 1 | 22-year-old | Male | – | Lung infiltrates | Huang et al. (2020) |
| China (Jinan) | Research article | 47 | 11 (23.4%) | Median age: 23 years (range: 1–60) | 6 males 7 females |
Pharyngeal swab COVID-19 nucleic acid was positive. The blood cell test results showed that 27.3% (3/11) had decreased white blood cell and 36.4% (4/11). The patients had increased lymphocyte count as well as high D-dimmer levels, C-reactive protein and ESR were also reported | 4 (36.4%) showed bilateral involvement and 3 (27.3%) showed unilateral involvement | Ma et al. (2020) |
| China | Research article | 2143 | 94 (12.9%) | Median age 7 years (range: 2–13) | – | No clinical symptoms and signs, while the 2019-nCoV nucleic acid test was positive | The chest imaging was normal | Dong et al. (2020) |
| China | Clinical observations | 83 | 1 (1.2%) | 50-year old | Female | Persistent positivity of the virus nucleic acid in her throat swabs and anal swabs for at least 17 days, suggesting that she was very likely a healthy carrier | – | Luo et al. (2020b) |
| China | Research article (familial cluster) | 5 | 2 (40%) | 28-year-old 23-year-old |
Males | Patients were afebrile without any clinical signs. On days 3–5 of hospitalisation, the 23-year-old man developed fever and cough symptoms. Other laboratory examinations showed increasing C-reactive protein | Chest CT images showed no abnormalities On days 3–5 of hospitalisation, the 23-year-old man's chest CT scans showed ground-glass opacities in the lungs |
Ye et al. (2020) |
| China | News journal article | 166 | 130 (78%) | – | – | – | – | Day (2020a) |
| China | Research article | 21 | 5 (20.8%) | 25 (10–61) years | 3 males 3 females |
RT-PCR positive for SARS-CoV-2. One case generated SARS-CoV-2 specific antibody responses | – | Yongchen et al. (2020) |
| China | Research article | 72,314 | 889 (1.2%) | Most were aged 30–79 years | – | Positive viral nucleic acid test results but without any COVID19 symptoms | – | Surveillances (2020) |
| China | Research article (hospitalised patients) | – | 26 | median age: 29.5 years | 16 males 10 females |
RT-PCR positive for SARS-CoV-2. C-reactive protein and lymphocytes count were normal in all patients. Three patients had reduced albumin and two patients with slightly elevated creatinine levels | Nine patients with normal CT scans, 10 patients with typical manifestations (patch-like, ground-glass opacities distributed in the extrapulmonary zone), seven patients with changes in a unilateral lung, and three patients with changes in bilateral lungs | Pan et al. (2020b) |
| China | Familial cluster study | 8 | 3 (37.5%) | 35-year-old 53-year-old 3-month-old infant |
Female | RT-PCR positive for SARS-CoV-2. No clinical symptoms | Ground-glass opacities except in the infant | Jiang et al. (2020b) |
| China | Research letter | 6 | 1 (16.6%) | 20-year-old | Female | RT-PCR positive for SARS-CoV-2. No elevated temperature measured or self-reported fever and no gastrointestinal or respiratory symptoms, including cough and sore throat, reported or observed by the physicians | Normal chest CT image | Bai et al. (2020) |
| Japan (Cruise Ship) | Rapid communication | 634 | 328 (51.7%) | Female age range: 0–59 years. Males: not determined | 313 female 321 male |
SARS-CoV-2 positive by PCR | – | Mizumoto et al. (2020) |
| Japan | Research article | 112 | 38 (33.9%) | Age range: 61.5–73.75 years | 22 females 16 males |
RT-PCR positive for SARS-CoV-2. IgM was detected in 27.8% of the collected specimens and IgG was detected in 3.3% | Chest CT showed abnormal lung findings consistent with the radiographic features of COVID-19 in 22 (57.9%) | Imai et al. (2020) |
| USA (Texas) | Case report | – | 1 | 63-year-old | Female | SARS-Cov2 nasopharyngeal swab RT-PCR positive. No respiratory symptoms, normal body temperature, no recent travel | CT-simulation scan revealed interval development of new multifocal ground-glass opacities of the lungs | McGinnis et al. (2020) |
| USA (Washington) | Research article | 48 | 27 (56%) | Mean age: 75.9 years | 14 females 13 males |
Real-time RT-PCR to test all samples. 15 reported no symptoms and 12 reported stable chronic symptoms. Fifteen (56%) residents who were asymptomatic at the time of testing had documented cognitive impairment | – | Arons et al. (2020) |
| USA (Washington) | Synopsis | 23 | 13 (57%) | Mean age: 80.7 years | – | The RT-PCR testing cycle threshold (Ct) values indicated large quantities of viral RNA | – | Kimball et al. (2020) |
| USA (Washington) | Editorial | 48 | 27 (56%) | – | – | RT-PCR positive for SARS-CoV-2 | – | Gandhi et al. (2020) |
| USA (New York) | News journal article | 33 | 29 (87.9%) | – | Pregnant females | RT-PCR positive for SARS-CoV-2 | – | Mayor (2020) |
| USA (New York) | Case series | 43 | 14 (32.6%) | Maternal age ranged 20–39 years with a mean age of 26.9 years | Pregnant females | PCR-confirmed SARS-CoV-2. Eight patients developed fever ranging from 37.9–39.2 °C during hospital admission | Breslin et al. (2020) | |
| Italy (Brescia) | Report (Incidental Findings) | Patients with different types of cancer | 7 | Median age 64.6 years old (Range: 55–79) years | 2 males 5 females |
RT-PCR positive for SARS-CoV-2 | Patient 3: chest CT showed a suspicious retrosternal lymph node but no lung pathology. Patient 5: Thoracic CT displayed several ground-glass opacities in the right lung. Patient 7: CT showed diffuse interstitial pneumonia with peripheral ground-glass opacities |
Albano et al. (2020) |
| Italy | Case report | – | 1 | 1 month | Male | Real-time PCR confirmed infection The infant is a cystic fibrosis patient. He never developed a fever or any signs of infection. |
– | Poli et al. (2020) |
| Italy | News journal article | 3300 | 90 (2.7%) | – | – | RT-PCR positive for SARS-CoV-2 | – | Day (2020b) |
| Germany | Correspondence | – | 4 | Patient 1: 33-year-old | Patient 1: male | RT-PCR positive for SARS-CoV-2 | – | Rothe et al. (2020) |
| Iran (Tehran) | Case report | – | 1 | 44-year-old | Male | RT-PCR positive for SARS-CoV-2 | Patchy ground-glass opacity in the upper lobe of the right lung | Asadollahi-Amin et al. (2020) |
| Iran | Case report | multiple trauma patients admitted to hospital | 8 | 49.71 ± 13.13 (range: 34–67) years | 62.5% male | None of the patients had COVID-19 symptoms at the time of admission to the hospital. RT-PCR positive for SARS-CoV-2. Laboratory results showed 4 (50%) patients with slight increase in C-reactive protein |
Pneumonia in chest CT scan | Samsami et al. (2020) |
Abbreviations: RT-PCR, reverse transcription–polymerase chain reaction; CT, computed tomography.
Looking at all the included studies with a large sample size (>1000 cases), these studies (Table 1, highlighted with bold text) estimated that the percentage of people who contracted SARS-CoV-2 and likely to be asymptomatic ranged from 1.2–12.9%. However, the other studies with a smaller sample size (<1000) reported a much higher incidence and indicated that up to 87.9% of COVID-19 infected individuals could be asymptomatic (Table 1). Most of these estimates were based on RT-PCR results. On the other hand, the estimated seroprevalence of antibodies to SARS-CoV-2 was reported to be higher. For instance, a study that was performed on 2857 blood donors from Rio de Janeiro showed 23.7% IgM positive cases, 11.4% IgG positive cases, while both IgM and IgG were detected in 64.9% (Amorim Filho et al., 2020). This is could be due to the limitation of nasal swabs, since a PCR diagnosis could be negative even though antibody detection is positive. In fact, this finding was reported in a study where four of 317 asymptomatic participants had a negative PCR diagnosis, while antibody testing was positive (Korth et al., 2020). Therefore, solely relying on molecular testing could significantly underestimate the seroprevalence of SARS-CoV-2, especially in asymptomatic individuals.
Discussion
The spread of COVID-19 is an emerging condition with pandemic potential that threatens all countries. More than three million cases of COVID-19 have been confirmed worldwide over the last 4 months. Numerous epidemiologic investigations have identified an association with respiratory droplet transmission. Yet, understanding of the transmission risk is incomplete. It is worth mentioning that COVID-19 asymptomatic individuals may pose a significant public health threat. The majority of these patients might be unaware of their disease and therefore not isolate themselves or seek treatment, consequently unknowingly transmit the virus to others. It is believed that this is the first systematic review study that has investigated the incidence of SARS-CoV-2 in asymptomatic patients.
A total of 63 of 505 screened studies reporting COVID-19 asymptomatic patients were included in this review. Epidemiological data, clinical laboratory results, CT image findings, and medical and contact history of the patients are critical knowledge that should be carefully studied when a new infectious disease emerges (Rodriguez-Morales et al., 2020). Although asymptomatic patients with SARS-CoV-2 were uncommon, studies have shown that the prevalence of SARS-CoV-2 in asymptomatic patients is underestimated and might increase. For instance, a review paper showed that the rate of asymptomatic individuals with Middle East Respiratory Syndrome coronavirus (MERS-CoV) ranged from 0–28.6% (Al-Tawfiq and Gautret, 2019). It was also reported that 75% of COVID-19 infected individuals could be asymptomatic (Day, 2020b).
COVID-19 infection ranges from asymptomatic to severe respiratory distress. Clinically it shows a milder infection in children, and many studies have reported children with asymptomatic COVID-19 infection. For instance, a study in China (Guangzhou) reported an asymptomatic 3-year-old male who tested positive for SARS-CoV-2, yet had normal lymphocyte counts and chest CT images (Pan et al., 2020a). Similarly, a study reported in China (Wuhan) showed a 3-year-old male asymptomatic patient with positive RT-PCR for SARS-CoV-2 and normal lymphocyte counts and chest CT images (Li et al., 2020). The reason for having a benign clinical course and low incidence of COVID-19 in children compared with adults is still unknown. A proposed hypothesis suggested that it might be due to the low expression of ACE2 receptors, high plasticity of their immune system, or to the exposure of other coronaviruses, which are generally more common in children (Cruz and Zeichner, 2020, Jia et al., 2005). Children may play a major role in community-based viral transmission. For instance, it was reported that viral shedding in a stool sample could persist for several weeks after diagnosis (Cai et al., 2020, Xiao et al., 2020). This poses a threat of viral transmission through the faecal-oral route, particularly for infants and children who are not toilet trained. Most of the reported COVID-19 cases in children were due to close contact with family members with SARS-CoV-2 infection (Table 1). Many experts believe that undetermined asymptomatic cases of COVID-19 infection could be an important source of contagion (Day, 2020a). Therefore, early identification of asymptomatic cases, as well as monitoring and tracing close contacts, could help in mitigating the spread of COVID-19 infection.
Another factor that increases the asymptomatic rate of COVID-19 is the inaccuracy of diagnostic testing. A recent article highlighted key important steps to be considered when designing seroprevalence studies, as well as experts’ opinion on the recent studies. A major concern raised about the recently published results was the type of antibody test used, since most of them were inaccurate in supporting the conclusions (Offord, 2020). It was reported that the manual ELISA kits are subject to cross-reaction with other coronaviruses such as SARS-CoV-1 and MERS-CoV (Al Kahlout et al., 2019). This depends on the type of antibody or antigen used to coat the plates. For instance, a recent study used a previously developed ELISA method based on bat SARS-CoV Rp3N protein, since it does not cross-react with other human coronaviruses except SARS-CoV (Zhou et al., 2020b). This method successfully detected IgM and IgG antibodies against SARS-CoV-2 in early cases of COVID-19. Yet, various studies, such as the studies included in this review, used Chinese-manufactured test kits that are not approved by Chinese authorities or the US Food and Drug Administration (FDA). A seroprevalence population-based study was carried in Santa Clara County, USA, and suggested that >30% of positive cases are missed by the PCR test and result in an underestimation of the incidence (Bendavid et al., 2020). The most significant implication of their findings is that the true infection rate is much higher than the reported number of cases. For instance, the study showed that the infection was 50–85-fold higher than confirmed positive cases by PCR (Bendavid et al., 2020). Although most of the included articles in this study used RT-PCR to confirm asymptomatic cases, no serological or other tests were performed to accurately estimate the incidence of SARS-CoV-2 in asymptomatic patients. In other words: PCR is considered the gold standard for diagnosis; however, if the sample was collected ≥14 weeks after infection, the viral genome/antigen might not be detected. Therefore, it could underestimate the prevalence of the infection.
Some of the included studies reported that the patients were positive for SARS-CoV-2 IgG, which suggests that the patients were asymptomatic SARS-CoV-2 carriers. The differential use of serology for confirming acute infection is not appropriate without additional collaboration of results. Therefore, combining both molecular and serological testing would be the best approach to accurately estimate the prevalence of COVID-19 infection, especially if the patient is at later stages of the infection and does not show symptoms (Younes et al., 2020).
Although governments in many countries are planning to conduct large-scale seroprevalence surveys, many laboratories try to rely on well-established and validated tests rather than rapid tests. The latter is based on blood collected from finger pricks to detect SARS-CoV-2 antibodies; however, the test performance and efficacy are not up to the required level, and many false results have been detected. Both specificity and sensitivity are essential in detecting SARS-CoV-2 to prevent false positive and negative results. It is unreliable to examine the test performance and efficacy of rapid tests based on finger-prick blood compared with the ELISA test, which uses venous blood. Consequently, this prevents underestimation of the asymptomatic COVID-19 infection rate.
Such positive cases may contribute to the silent spread of the virus. One of the significant limitations of many studies reporting asymptomatic cases is the difficulty in differentiating between asymptomatic or pre-symptomatic people, who are asymptomatic at the time of testing and develop symptoms later on. Citing data from China, WHO officials said on 01 April, “some cases of asymptomatic carriers have been confirmed by finding and testing people who were in close contact with COVID-19 patients. For those who tested positive without symptoms, follow-up exams confirmed that about 25% continued to show no signs”. For instance, a clinical study with a small sample size from China, performed in March 2020, followed up 24 asymptomatic positive PCR patients; 60% of them were pre-symptomatic and showed COVID-19 symptoms after 1–3 weeks (Hu et al., 2020). More follow-up studies should be performed to determine whether these cases continue to be asymptomatic or eventually develop symptoms. The question remains to be answered with further follow-up studies: can these asymptomatic or pre-symptomatic individuals spread the infection?
Conclusion
COVID-19 is a new infectious disease that has infected more than three million people in many countries all over the world. The severity and clinical manifestation of COVID-19 varies, and some individuals have been reported as asymptomatic. Based on the results of this study, many of the COVID-19 infected cases show no symptoms, and the infection could be transmitted during the incubation period. Consequently, asymptomatic patients are considered carriers and a potential source of infection to the community. Therefore, additional research studies on the epidemiological significance of COVID-19 asymptomatic cases are required.
Conflicts of interest
The authors declare no conflict of interest.
Contributions
Conceptualization, GKN; data curation, DWA and GKN; writing – original draft preparation, DWA; writing – review and editing, DWA and GKN; supervision, GKN; project administration, GKN; funding acquisition, GKN. All authors have read and agreed to the published version of the manuscript.
Funding
This work was made possible by grant No. RRC-2-032 from the Qatar National Research Fund (a member of Qatar Foundation) given to GKN. The statements made herein are solely the responsibility of the authors. Authors would like also to acknowledge funds from the Qatar University’s internal grant QUERG-CMED-2020-2.
Ethical approval
The work presented in this manuscript does not involve work with animals or with human subjects, and therefore does not require ethics clearance.
Acknowledgment
We would like to thank Nadin Younes for reviewing this article.
References
- Al Kahlout R.A., Nasrallah G.K., Farag E.A., Wang L., Lattwein E., Müller M.A. Comparative serological study for the prevalence of anti-MERS coronavirus antibodies in high-and low-risk groups in Qatar. J Immunol Res. 2019 doi: 10.1155/2019/1386740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albano D., Bertagna F., Bertoli M., Bosio G., Lucchini S., Motta F. Incidental findings suggestive of covid-19 in asymptomatic patients undergoing nuclear medicine procedures in a high prevalence region. J Nucl Med. 2020 doi: 10.2967/jnumed.120.246256. [DOI] [PubMed] [Google Scholar]
- Al-Tawfiq J.A., Gautret P. Asymptomatic Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection: extent and implications for infection control: a systematic review. Travel Med Infect Dis. 2019;27:27–32. doi: 10.1016/j.tmaid.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amanat F. A serological assay to detect SARS-CoV-2 seroconversion in humans. Nature Med. 2020:1–4. doi: 10.1038/s41591-020-0913-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amorim Filho L., Szwarcwald C.L., Mateos S.D.O.G., de Leon A.C.M.P., de Andrade Medronho R., Veloso V.G. SciELO; 2020. Seroprevalence of IgG and IgM anti-SARS-CoV-2 among voluntary blood donors in Rio de Janeiro, Brazil. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An P., Song P., Wang Y., Liu B. Asymptomatic patients with novel Coronavirus Disease (COVID-19) Balkan Med J. 2020 doi: 10.4274/balkanmedj.galenos.2020.2020.4.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arons M.M., Hatfield K.M., Reddy S.C., Kimball A., James A., Jacobs J.R. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020 doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asadollahi-Amin A., Hasibi M., Ghadimi F., Rezaei H., SeyedAlinaghi S. Lung involvement found on chest CT scan in a pre-symptomatic person with SARS-CoV-2 infection: a case report. Trop Med Infect Dis. 2020;5(2) doi: 10.3390/tropicalmed5020056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai Y., Yao L., Wei T., Tian F., Jin D.Y., Chen L. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendavid E., Mulaney B., Sood N., Shah S., Ling E., Bromley-Dulfano R. COVID-19 antibody seroprevalence in Santa Clara County, California. medRxiv. 2020 doi: 10.1093/ije/dyab010. 2020.04.14.20062463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslin N., Baptiste C., Gyamfi-Bannerman C., Miller R., Martinez R., Bernstein K. COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. 2020:100118. doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai J., Xu J., Lin D., Xu L., Qu Z., Zhang Y. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.F.-W., Yuan S., Kok K.-H., To K.K.-W., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Wang A., Yi B., Ding K., Wang H., Wang J. The epidemiological characteristics of infection in close contacts of COVID-19 in Ningbo city. Chin J Epidemiol. 2020;41 doi: 10.3760/cma.j.cn112338-20200304-00251. [DOI] [PubMed] [Google Scholar]
- Cruz A.T., Zeichner S.L. COVID-19 in children: initial characterization of the pediatric disease. Pediatrics. 2020 doi: 10.1542/peds.2020-0834. [DOI] [PubMed] [Google Scholar]
- Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ (Clin Res Ed) 2020;369:m1375. doi: 10.1136/bmj.m1375. [DOI] [PubMed] [Google Scholar]
- Day M. Covid-19: identifying and isolating asymptomatic people helped eliminate virus in Italian village. BMJ (Clin Res Ed.) 2020;368:m1165. doi: 10.1136/bmj.m1165. [DOI] [PubMed] [Google Scholar]
- Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020 [Google Scholar]
- Fauci A.S., Touchette N.A., Folkers G.K. Emerging infectious diseases: a 10-year perspective from the National Institute of Allergy and Infectious Diseases. Emerg Infect Dis. 2005;11(4):519–525. doi: 10.3201/eid1104.041167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandhi M., Yokoe D.S., Havlir D.V. Asymptomatic transmission, the Achilles’ heel of current strategies to control Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMe2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He D., Zhao S., Lin Q., Zhuang Z., Cao P., Wang M.H. The relative transmissibility of asymptomatic COVID-19 infections among close contacts. Int J Infect Dis. 2020;94:145–147. doi: 10.1016/j.ijid.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Z., Song C., Xu C., Jin G., Chen Y., Xu X. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci China Life Sci. 2020 doi: 10.1007/s11427-020-1661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L., Zhang X., Zhang X., Wei Z., Zhang L., Xu J. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16–23 years outside Wuhan and characteristics of young patients with COVID-19: a prospective contact-tracing study. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai K., Tabata S., Ikeda M., Noguchi S., Kitagawa Y., Matuoka M. Clinical evaluation of an immunochromatographic IgM/IgG antibody assay and chest computed tomography for the diagnosis of COVID-19. J Clin Virol. 2020:104393. doi: 10.1016/j.jcv.2020.104393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia H.P., Look D.C., Shi L., Hickey M., Pewe L., Netland J. ACE2 receptor expression and severe acute respiratory syndrome coronavirus infection depend on differentiation of human airway epithelia. J Virol. 2005;79(23):14614–14621. doi: 10.1128/JVI.79.23.14614-14621.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang X.L., Zhang X.L., Zhao X.N., Li C.B., Lei J., Kou Z.Q. Transmission potential of asymptomatic and paucisymptomatic SARS-CoV-2 infections: a three-family cluster study in China. J Infect Dis. 2020 doi: 10.1093/infdis/jiaa206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang X., Luo M., Zou Z., Wang X., Chen C., Qiu J. Asymptomatic SARS-CoV-2 infected case with viral detection positive in stool but negative in nasopharyngeal samples lasts for 42 days. J Med Virol. 2020 doi: 10.1002/jmv.25941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khailany R.A., Safdar M., Ozaslan M. Genomic characterization of a novel SARS-CoV-2. Gene Rep. 2020;(1006):82. doi: 10.1016/j.genrep.2020.100682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimball A., Hatfield K.M., Arons M., James A., Taylor J., Spicer K. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility – King County, Washington, March 2020. Morb Mortal Wkly Rep. 2020;69(13):377–381. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korth J., Wilde B., Dolff S., Anastasiou O.E., Krawczyk A., Jahn M. SARS-CoV-2-specific antibody detection in healthcare workers in Germany with direct contact to COVID-19 patients. J Clin Virol. 2020;128:104437. doi: 10.1016/j.jcv.2020.104437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., Ji F., Wang L., Wang L., Hao J., Dai M. Asymptomatic and human-to-human transmission of SARS-CoV-2 in a 2-family cluster, Xuzhou, China. Emerg Infect Dis. 2020;26(7) doi: 10.3201/eid2607.200718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling Z., Xu X., Gan Q., Zhang L., Luo L., Tang X. Asymptomatic SARS-CoV-2 infected patients with persistent negative CT findings. Eur J Radiol. 2020:126. doi: 10.1016/j.ejrad.2020.108956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P., Yang X.-L., Wang X.-G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X., Li Y., Li T., Zhang W. Follow-up of asymptomatic patients with SARS-CoV-2 infection. Clin Microbiol Infect. 2020 doi: 10.1016/j.cmi.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- London School of Hygiene and Tropical Medicine. Almost 75% of people on board Diamond Princess with COVID-19 may have been asymptomatic. Available from: https://www.lshtm.ac.uk/newsevents/news/2020/almost-75-people-board-diamond-princess-covid-19-may-have-been-asymptomatic [accessed 16.06.20].
- Lu D., Sang L., Du S., Li T., Chang Y., Yang X.A. Asymptomatic COVID-19 infection in late pregnancy indicated no vertical transmission. J Med Virol. 2020 doi: 10.1002/jmv.25927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu S., Lin J., Zhang Z., Xiao L., Jiang Z., Chen J. Alert for non-respiratory symptoms of Coronavirus Disease 2019 (COVID-19) patients in epidemic period: a case report of familial cluster with three asymptomatic COVID-19 patients. J Med Virol. 2020 doi: 10.1002/jmv.25776. [DOI] [PubMed] [Google Scholar]
- Luo S.H., Liu W., Liu Z.J., Zheng X.Y., Hong C.X., Liu Z.R. A confirmed asymptomatic carrier of 2019 novel coronavirus (SARS-CoV-2) Chin Med J. 2020 doi: 10.1097/CM9.0000000000000798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., Trevathan E., Qian Z., Li Y., Li J., Xiao W. Asymptomatic SARS-CoV-2 Infection in Household Contacts of a Healthcare Provider, Wuhan, China. Emerg Infect Dis. 2020;26(8) doi: 10.3201/eid2608.201016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Xu Q.-n., Wang F.-l., Ma X.-m., Wang X.-y., Zhang X.-g. Characteristics of asymptomatic patients with SARS-CoV-2 infection in Jinan, China. Microbes Infect. 2020 doi: 10.1016/j.micinf.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao Z.Q., Wan R., He L.Y., Hu Y.C., Chen W. The enlightenment from two cases of asymptomatic infection with SARS-CoV-2: is it safe after 14 days of isolation? Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayor S. Covid-19: Nine in 10 pregnant women with infection when admitted for delivery are asymptomatic, small study finds. BMJ (Clin Res Ed) 2020;369:m1485. doi: 10.1136/bmj.m1485. [DOI] [PubMed] [Google Scholar]
- McGinnis G.J., Ning M.S., Nitsch P.L., O’Reilly M., McAleer M.F., Koong A.C. Rapid detection of asymptomatic COVID-19 by CT image-guidance for stereotactic ablative radiotherapy. J Thorac Oncol. 2020 doi: 10.1016/j.jtho.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng H., Xiong R., He R., Lin W., Hao B., Zhang L. CT imaging and clinical course of asymptomatic cases with COVID-19 pneumonia at admission in Wuhan, China. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizumoto K., Kagaya K., Zarebski A., Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Eurosurveillance. 2020;25(10) doi: 10.2807/1560-7917.ES.2020.25.10.2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mousavizadeh L., Ghasemi S. Genotype and phenotype of COVID-19: their roles in pathogenesis. J Microbiol Immunol Infect. 2020 doi: 10.1016/j.jmii.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Offord C. 2020. How (not) to do an antibody survey for SARS-CoV-2. Available from: https://www.the-scientist.com/news-opinion/how-not-to-do-an-antibody-survey-for-sars-cov-2-67488?utm_campaign=TS_OTC_2020&utm_source=hs_email&utm_medium=email&utm_content=87227297&_hsenc=p2ANqtz--OX79Py05lz3KB_wqDMHJfcVa3bRgNFKwz-ImL1fxCEQ_fZwMR1zxNctcNqGZAYwBFm8PrGdjQib1gWD3oZ0NWpLCEaw&_hsmi=87227297 [accessed 01.05.20] [Google Scholar]
- Ouyang W., Yu J., Zhang J., Xie C. Alert to potential contagiousness: a case of lung cancer with asymptomatic SARS-CoV-2 infection. J Thorac Oncol. 2020 doi: 10.1016/j.jtho.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan X., Chen D., Xia Y., Wu X., Li T., Ou X. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect Dis. 2020;20(4):410–411. doi: 10.1016/S1473-3099(20)30114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan Y., Yu X., Du X., Li Q., Li X., Qin T. Epidemiological and clinical characteristics of 26 asymptomatic SARS-CoV-2 carriers. J Infect Dis. 2020 doi: 10.1093/infdis/jiaa205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parreira R. Laboratory methods in molecular epidemiology: viral infections. Microbiol Spectr. 2018;6(6) doi: 10.1128/microbiolspec.ame-0003-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poli P., Timpano S., Goffredo M., Padoan R., Badolato R. Asymptomatic case of Covid-19 in an infant with cystic fibrosis. J Cystic Fibrosis. 2020 doi: 10.1016/j.jcf.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin C., Liu F., Yen T.-C., Lan X. 18 F-FDG PET/CT findings of COVID-19: a series of four highly suspected cases. Eur J Nucl Med Molec Imaging. 2020:1–6. doi: 10.1007/s00259-020-04734-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu H., Wu J., Hong L., Luo Y., Song Q., Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Morales A.J., Cardona-Ospina J.A., Gutiérrez-Ocampo E., Villamizar-Peña R., Holguin-Rivera Y., Escalera-Antezana J.P. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020:101623. doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. New Eng J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samsami M., Zebarjadi Bagherpour J., Nematihonar B., Tahmasbi H. COVID-19 pneumonia in asymptomatic trauma patients; report of 8 cases. Arch Acad Emerg Med. 2020;8(1):e46. [PMC free article] [PubMed] [Google Scholar]
- Song Z., Xu Y., Bao L., Zhang L., Yu P., Qu Y. From SARS to MERS, thrusting coronaviruses into the spotlight. Viruses. 2019;11(1) doi: 10.3390/v11010059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surveillances V. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Wkly. 2020;2(8):113–122. [PMC free article] [PubMed] [Google Scholar]
- Wang X., Fang J., Zhu Y., Chen L., Ding F., Zhou R. Clinical characteristics of non-critically ill patients with novel coronavirus infection (COVID-19) in a Fangcang Hospital. Clin Microbiol Infect. 2020 doi: 10.1016/j.cmi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Ma W., Zheng X., Wu G., Zhang R. Household transmission of SARS-CoV-2. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2020. Coronavirus disease (COVID-19) pandemic. [Google Scholar]
- Wikramaratna P., Paton R.S., Ghafari M., Lourenco J. Estimating false-negative detection rate of SARS-CoV-2 by RT-PCR. medRxiv. 2020 doi: 10.2807/1560-7917.ES.2020.25.50.2000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao F., Tang M., Zheng X., Liu Y., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6) doi: 10.1053/j.gastro.2020.02.055. 1831–33.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye F., Xu S., Rong Z., Xu R., Liu X., Deng P. Delivery of infection from asymptomatic carriers of COVID-19 in a familial cluster. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yongchen Z., Shen H., Wang X., Shi X., Li Y., Yan J. Different longitudinal patterns of nucleic acid and serology testing results based on disease severity of COVID-19 patients. Emerg Microbes Infect. 2020:1–14. doi: 10.1080/22221751.2020.1756699. (just-accepted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younes N., Al-Sadeq D.W., Al-Jighefee H., Younes S., Al-Jamal O., Daas H.I. Challenges in laboratory diagnosis of the novel coronavirus SARS-CoV-2. Viruses. 2020;12(6):582. doi: 10.3390/v12060582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y.H., Lin D.J., Xiao M.F., Wang J.C., Wei Y., Lei Z.X. 2019 novel coronavirus infection in a three-month-old baby. Zhonghua Er Ke Za Zhi. 2020;58(3):182–184. doi: 10.3760/cma.j.issn.0578-1310.2020.03.004. [DOI] [PubMed] [Google Scholar]