Abstract
This study uses data from the National Center for Health Statistics to estimate excess deaths (ie, the difference between observed and expected deaths) in the US and the District of Columbia in the early weeks of the COVID-19 pandemic.
The number of publicly reported deaths from coronavirus disease 2019 (COVID-19) may underestimate the pandemic’s death toll. Such estimates rely on provisional data that are often incomplete and may omit undocumented deaths from COVID-19. Moreover, restrictions imposed by the pandemic (eg, stay-at-home orders) could claim lives indirectly through delayed care for acute emergencies, exacerbations of chronic diseases, and psychological distress (eg, drug overdoses). This study estimated excess deaths in the early weeks of the pandemic and the relative contribution of COVID-19 and other causes.
Methods
Weekly death data for the 50 US states and the District of Columbia were obtained from the National Center for Health Statistics for January through April 2020 and the preceding 6 years (2014-2019).1,2 US totals excluded Connecticut and North Carolina because of missing data. The analysis included total deaths and deaths from COVID-19, influenza/pneumonia, heart disease, diabetes, and 10 other grouped causes (Supplement). Mortality rates for causes other than COVID-19 were available only for underlying causes. Death data with any mention of COVID-19 on the death certificate (as an underlying or contributing cause) were used to capture all deaths attributed to the virus. Population counts for calculating mortality rates were obtained from the US Census Bureau.3,4
Observed deaths for the 8 weeks between March 1, 2020, and April 25, 2020, were taken from provisional data released on June 10, 2020.2 Expected deaths (and 95% CIs) for these same weeks were estimated by fitting a hierarchical Poisson regression model to the weekly death counts for the period of December 29, 2013, through February 29, 2020 (assembled from final data for 2014-20181 and provisional data for January 1, 2019, through February 29, 20202). The model with the optimal fit (Supplement) used a combination of harmonic functions to capture seasonality and adjusted for annual trends with a categorical year effect. The model allowed season and time trends to vary by state.
Excess deaths equaled the difference between observed and expected deaths and were summed across the 8 weeks to estimate total excess deaths. To explore increases in cause-specific mortality in jurisdictions overwhelmed by COVID-19, mortality trends for 14 grouped causes (4 reported here) were examined in the 5 states with the most COVID-19 deaths from March through April 2020 (Massachusetts, Michigan, New Jersey, New York, and Pennsylvania). Deaths in these states peaked in the week ending on April 11, 2020, and the proportional increase above baseline (weighted mean of weekly deaths over 9 weeks in January to February 2020) was measured. All calculations were performed using SAS, version 9.4 (SAS Institute Inc).
Results
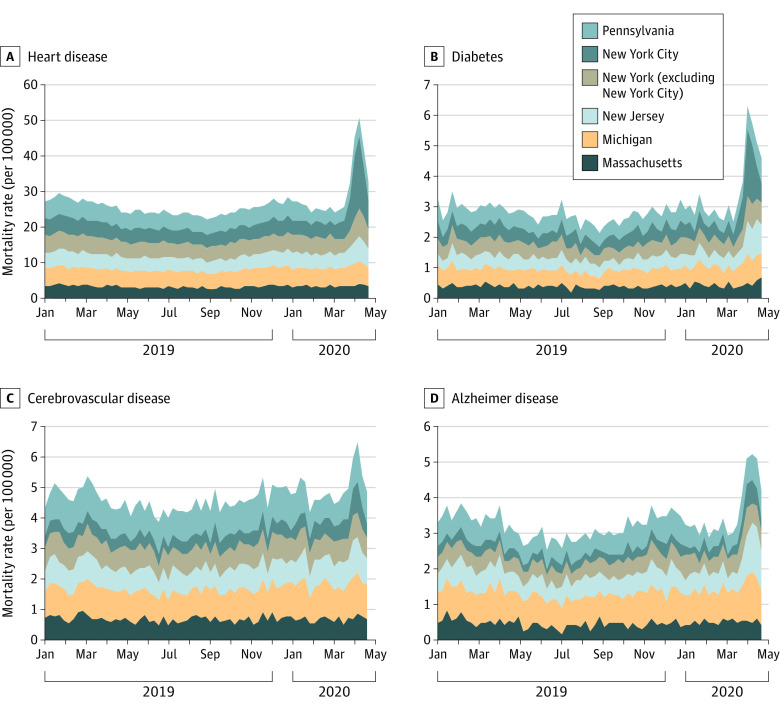
Between March 1, 2020, and April 25, 2020, a total of 505 059 deaths were reported in the US; 87 001 (95% CI, 86 578-87 423) were excess deaths, of which 56 246 (65%) were attributed to COVID-19. In 14 states, more than 50% of excess deaths were attributed to underlying causes other than COVID-19; these included California (55% of excess deaths) and Texas (64% of excess deaths) (Table). The 5 states with the most COVID-19 deaths experienced large proportional increases in deaths due to nonrespiratory underlying causes, including diabetes (96%), heart diseases (89%), Alzheimer disease (64%), and cerebrovascular diseases (35%) (Figure). New York City experienced the largest increases in nonrespiratory deaths, notably those due to heart disease (398%) and diabetes (356%).
Table. Excess Deaths From March 1, 2020, to April 25, 2020, Attributed and Not Attributed to Coronavirus Disease 2019 (COVID-19)a.
| Jurisdiction | Expected deaths, No. (95% CI)b | Observed deaths, No. | Excess deaths, No. (95% CI) | COVID-19 deathsc | Deaths not attributed to COVID-19c | ||
|---|---|---|---|---|---|---|---|
| Reported deaths, No. | Excess deaths, % | Excess deaths, No. (95% CI) | Excess deaths, % | ||||
| United Statesd | 419 058 (418 636 to 419 481) | 505 059 | 87 001 (86 578 to 87 423) | 56 246 | 65 | 30 755 (30 332 to 31 177) | 35 |
| Jurisdictions with highest COVID-19 death countsc | |||||||
| New York City | 8369 (8310 to 8427) | 29 703 | 21 334 (21 276 to 21 393) | 14 952 | 70 | 6382 (6324 to 6441) | 30 |
| New Jersey | 11 458 (11 388 to 11 528) | 23 174 | 11 716 (11 646 to 11 786) | 8037 | 69 | 3679 (3609 to 3749) | 31 |
| New York (excluding New York City) | 15 603 (15 519 to 15 686) | 24 611 | 9008 (8925 to 9092) | 6569 | 73 | 2439 (2356 to 2523) | 27 |
| Michigan | 15 217 (15 134 to 15 300) | 20 232 | 5015 (4932 to 5098) | 3372 | 67 | 1643 (1560 to 1726) | 33 |
| Massachusetts | 9316 (9253 to 9378) | 13 412 | 4096 (4034 to 4159) | 3122 | 76 | 974 (912 to 1037) | 24 |
| Pennsylvania | 17 178 (17 089 to 17 268) | 22 304 | 5126 (5036 to 5215) | 2752 | 54 | 2374 (2284 to 2463) | 46 |
| Other jurisdictions | |||||||
| Illinois | 16 559 (16 473 to 16 646) | 20 310 | 3751 (3664 to 3837) | 2051 | 55 | 1700 (1613 to 1786) | 45 |
| California | 42 263 (42 121 to 42 405) | 46 289 | 4026 (3884 to 4168) | 1801 | 45 | 2225 (2083 to 2367) | 55 |
| Louisiana | 7097 (7044 to 7150) | 9082 | 1985 (1932 to 2038) | 1594 | 80 | 391 (338 to 444) | 20 |
| Florida | 33 550 (33 421 to 33 678) | 35 766 | 2216 (2088 to 2345) | 1250 | 56 | 966 (838 to 1095) | 44 |
| Indiana | 10 459 (10 392 to 10 525) | 11 672 | 1213 (1147 to 1280) | 997 | 82 | 216 (150 to 283) | 18 |
| Maryland | 7664 (7608 to 7719) | 9561 | 1897 (1842 to 1953) | 979 | 52 | 918 (863 to 974) | 48 |
| Georgia | 13 205 (13 128 to 13 281) | 14 576 | 1371 (1295 to 1448) | 973 | 71 | 398 (322 to 475) | 29 |
| Colorado | 6374 (6323 to 6424) | 7573 | 1199 (1149 to 1250) | 822 | 69 | 377 (327 to 428) | 31 |
| Texas | 31 398 (31 277 to 31 520) | 33 672 | 2274 (2152 to 2395) | 809 | 36 | 1465 (1343 to 1586) | 64 |
| Ohio | 18 752 (18 660 to 18 844) | 19 387 | 635 (543 to 727) | 794 | 125 | −159 (−251 to −67) | −25 |
| Washington | 8849 (8789 to 8910) | 9882 | 1033 (972 to 1093) | 719 | 70 | 314 (253 to 374) | 30 |
| Virginia | 10 679 (10 612 to 10 747) | 12 045 | 1366 (1298 to 1433) | 526 | 39 | 840 (772 to 907) | 61 |
| Arizona | 9777 (9713 to 9842) | 10 734 | 957 (892 to 1021) | 365 | 38 | 592 (527 to 656) | 62 |
| Missouri | 9985 (9920 to 10 050) | 10 504 | 519 (454 to 584) | 335 | 65 | 184 (119 to 249) | 35 |
| Alabama | 8079 (8022 to 8136) | 8631 | 552 (495 to 609) | 317 | 57 | 235 (178 to 292) | 43 |
| Wisconsin | 8448 (8388 to 8508) | 9013 | 565 (505 to 625) | 288 | 51 | 277 (217 to 337) | 49 |
| Minnesota | 7088 (7035 to 7142) | 7384 | 296 (242 to 349) | 287 | 97 | 9 (−45 to 62) | 3 |
| Mississippi | 4832 (4790 to 4873) | 5403 | 571 (530 to 613) | 252 | 44 | 319 (278 to 361) | 56 |
| Rhode Island | 1641 (1621 to 1661) | 1870 | 229 (209 to 249) | 250 | 109 | −21 (−41 to −1) | −9 |
| Kentucky | 7451 (7396 to 7505) | 7621 | 170 (116 to 225) | 215 | 126 | −45 (−99 to 10) | −26 |
| South Carolina | 7786 (7729 to 7842) | 8561 | 775 (719 to 832) | 213 | 27 | 562 (506 to 619) | 73 |
| Nevada | 4090 (4052 to 4127) | 4328 | 238 (201 to 276) | 213 | 89 | 25 (−12 to 63) | 11 |
| Oklahoma | 5824 (5777 to 5871) | 6285 | 461 (414 to 508) | 193 | 42 | 268 (221 to 315) | 58 |
| District of Columbia | 947 (934 to 960) | 1223 | 276 (263 to 289) | 185 | 67 | 91 (78 to 104) | 33 |
| Tennessee | 11 604 (11 534 to 11 675) | 12 224 | 620 (549 to 690) | 172 | 28 | 448 (377 to 518) | 72 |
| Iowa | 4741 (4699 to 4782) | 4815 | 74 (33 to 116) | 122 | 164 | −48 (−89 to −6) | −64 |
| Oregon | 5684 (5638 to 5731) | 6101 | 417 (370 to 463) | 114 | 27 | 303 (256 to 349) | 73 |
| Delaware | 1409 (1391 to 1427) | 1623 | 214 (196 to 232) | 113 | 53 | 101 (83 to 119) | 47 |
| Kansas | 4133 (4095 to 4170) | 4254 | 121 (84 to 159) | 104 | 86 | 17 (−20 to 55) | 14 |
| New Mexico | 2896 (2866 to 2926) | 2969 | 73 (43 to 103) | 89 | 121 | −16 (−46 to 14) | −21 |
| New Hampshire | 1894 (1872 to 1916) | 2044 | 150 (128 to 172) | 61 | 41 | 89 (67 to 111) | 59 |
| Nebraska | 2615 (2587 to 2643) | 2715 | 100 (72 to 128) | 51 | 51 | 49 (21 to 77) | 49 |
| Idaho | 2202 (2177 to 2227) | 2321 | 119 (94 to 144) | 46 | 39 | 73 (48 to 98) | 61 |
| Maine | 2347 (2321 to 2373) | 2368 | 21 (−5 to 47) | 41 | 195 | −20 (−46 to 6) | −95 |
| Arkansas | 4973 (4930 to 5015) | 5051 | 78 (36 to 121) | 37 | 47 | 41 (−1 to 84) | 53 |
| West Virginia | 3535 (3500 to 3569) | 3538 | 3 (−31 to 38) | 27 | 777 | −24 (−58 to 11) | −677 |
| Utah | 2952 (2921 to 2982) | 3182 | 230 (200 to 261) | 26 | 11 | 204 (174 to 235) | 89 |
| Vermont | 903 (890 to 916) | 1018 | 115 (102 to 128) | 11 | 10 | 104 (91 to 117) | 90 |
| Wyoming | 718 (708 to 729) | 782 | 64 (53 to 74) | 0 | 0 | 64 (53 to 74) | 100 |
| South Dakota | 1268 (1251 to 1284) | 1306 | 38 (22 to 55) | 0 | 0 | 38 (22 to 55) | 100 |
| Montana | 1614 (1594 to 1634) | 1637 | 23 (3 to 43) | 0 | 0 | 23 (3 to 43) | 100 |
Data were not applicable (and not shown) for states with “negative” excess deaths (COVID-19 deaths exceeding projected deaths), including Alaska (−45 deaths), Hawaii (−45 deaths), and North Dakota (−244 deaths).
Seasonal average predicted by regression model.
COVID-19 deaths include deaths in which COVID-19 was identified as the underlying cause of death or a contributing cause.
The US total was calculated as the sum of results for 48 states and the District of Columbia. Data for Connecticut and North Carolina were omitted because of delays in reporting.
Figure. Weekly Death Rates From January 2019 Through April 2020.
Data refer only to underlying causes of death; COVID-19 may have been a contributing cause in an unknown number of deaths. New Jersey and New York City experienced the largest relative increases.
Discussion
These estimates suggest that the number of COVID-19 deaths reported in the first weeks of the pandemic captured only two-thirds of excess deaths in the US. Potential explanations include delayed reporting of COVID-19 deaths and misattribution of COVID-19 deaths to other respiratory illnesses (eg, pneumonia) or to nonrespiratory causes reflecting complications of COVID-19 (eg, coagulopathy, myocarditis). Few excess deaths involved pneumonia or influenza as underlying causes.
This study has limitations, including the reliance on provisional data, potentially inaccurate death certificates, and modeling assumptions. For example, modeling epidemiologic years instead of calendar years would reduce the excess deaths estimate to 73 524.
Large increases in mortality from heart disease, diabetes, and other diseases were observed. Further investigation is required to determine the extent to which these trends represent nonrespiratory manifestations of COVID-19 or secondary pandemic mortality caused by disruptions in society that diminished or delayed access to health care and the social determinants of health (eg, jobs, income, food security).
Section Editor: Jody W. Zylke, MD, Deputy Editor.
eResults
References
- 1.Weekly counts of deaths by state and select causes, 2014-2018. National Center for Health Statistics website. Updated June 5, 2020. Accessed June 10, 2020. https://data.cdc.gov/NCHS/Weekly-Counts-of-Deaths-by-State-and-Select-Causes/3yf8-kanr
- 2.Weekly counts of deaths by state and select causes, 2019-2020. National Center for Health Statistics website. Updated June 10, 2020. Accessed June 10, 2020. https://data.cdc.gov/NCHS/Weekly-Counts-of-Deaths-by-State-and-Select-Causes/muzy-jte6
- 3.2018 American Community Survey 1-year estimates: table B01003. US Census Bureau website. Accessed May 15, 2020. https://data.census.gov/cedsci/table?hidePreview=false&tid=ACSDT1Y2018.B01003&t=Total%20population&vintage=2018
- 4.QuickFacts: New York City, New York. US Census Bureau website. Accessed May 15, 2020. https://www.census.gov/quickfacts/newyorkcitynewyork
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eResults