Abstract
Background:
Turkey has one of the highest death rates in the world due to COVID-19 pandemic. The pandemic caused anxiety and depression in individuals. However, there is insufficient information on the effects of COVID-19 on individuals and their coping methods. Therefore, mental problems associated with the pandemic need to be evaluated rapidly.
Aims:
This study was carried out to determine depression levels and related factors in a society affected by COVID-19.
Method:
The study was planned using a descriptive cross-sectional design. The study started 2 weeks after the first diagnosis of COVID-19 in Turkey and was carried out between March 23 and April 3, 2020. The study included 1115 adult participants who were between 18 and 65 years of age and were citizens of the Turkish Republic. The study was carried out using online questionnaires, and data were collected with the Personal Information Form and the Beck Depression Inventory. The data were evaluated using IBM SPSS Statistics, version 20 software program.
Results:
The depression scores of female participants who were between 18 and 29 years of age, single, students, and had less income than their expenses were found to be higher than others. People who experienced fear of being infected and infecting others, had a cleaning obsession, anxiety about the future, sadness, and anxiousness experienced depression at lower levels when compared to other participants. Participants who had to change their place of residence during the quarantine, experienced loneliness, fear of death, hopelessness, sleep problems, felt useless and worthless, started to smoke and drink alcohol, and experienced depression at moderate levels. Depression scores of those who spent time with their family, made time for themselves, were busy with home education or work were lower compared to others.
Conclusion:
The COVID-19 pandemic caused mild-level depression in the Turkish society.
Keywords: COVID-19, coronavirus, pandemic, quarantine, depression
Introduction
The coronavirus causes upper respiratory infection which presents with symptoms such as high fever and difficulty in breathing (Gralinski & Menachery, 2020). The new coronavirus (COVID-19) was first detected in November 2019 in Wuhan in the Hubei state of China (World Health Organization (WHO), 2020b). It spread rapidly within China and to other countries (Shigemura et al., 2020).
Since January 23, 2020, strict quarantine measures have been taken in Wuhan and other regions of China to prevent the COVID-19 pandemic (J. B. Li et al., 2020). The reopening of the schools after spring break was postponed, citizens were encouraged to work from their homes, to stay at home if possible, to use personal protective equipment such as face masks, and all meetings were canceled (Kickbusch & Leung, 2020). On January 30, 2020, the WHO (2020b) declared the COVID-19 outbreak to be a Public Health Emergency of International Concern, a pandemic, on March 11, 2020. As of writing this article, the number of positive COVID-19 cases is 7,255,960 and the number of deaths due to this fatal virus have reached 412,583 (WHO, 2020b). The highest number of cases were observed in the United States of America, Brazil, Russian Federation, the United Kingdom, and India, in that order (WHO, 2020a).
The first COVID-19 case in Turkey was detected on March 10, 2020, and the first death due the virus was reported on March 17, 2020 (Ministry of Health, 2020). In Turkey, teams have been created to conduct studies on the COVID-19, and preventive measures have been taken that are required for the pandemic plan. As of March 16, 2020, flexible working hours and a home office working system have been adopted throughout Turkey. On the same date, schools and universities started distance education. A lockdown was imposed on individuals above 65 years of age as of March 21, 2020. As of April 4, 2020, a lockdown was also applied on individuals under 20 years of age, and entrance/exit restrictions to 30 metropolises and the city Zonguldak. As of writing this article, the number of cases in Turkey was declared to be 173,036 and the number of deaths, 4,746 (Ministry of Health, 2020). Turkey has one of the highest death rates in the world, being the 11th country in order of death rates (WHO, 2020a).
Administration of the quarantine measures taken to combat the pandemic affects many aspects of life at the individual and societal levels (Qiu et al., 2020). The COVID-19 pandemic not only threatens human safety and physical health but also causes mental problems in societies affected by this situation by causing thousands of deaths worldwide (W. Li et al., 2020; Liu et al., 2020; Zhou, 2020). A series of undesirable emotional and behavioral problems developed in individuals during this period: an increase in negative emotions such as despair, anxiety, guilt, stigma, insomnia, anger, fear of being infected, an increase in alcohol consumption and smoking, and social isolation (Dong & Bouey, 2020; Ho et al., 2020; J. B. Li et al., 2020; W. Li et al., 2020; Shigemura et al., 2020; Wang et al., 2020; Zhou, 2020).
The pandemic caused anxiety disorders such as somatization, post-traumatic stress disorder, and panic disorder and depression in individuals (Ho et al., 2020; J. B. Li et al., 2020; Qiu et al., 2020; Shigemura et al., 2020). However, there is insufficient information on the effects of COVID-19 on individuals and their coping methods (Ho et al., 2020; W. Li et al., 2020). Therefore, mental problems associated with the pandemic need to be evaluated rapidly (Gao et al., 2020).
This study in Turkey applies to adult individuals between 18 and 65 years of age: it is structured to be a lead study for future studies and for assessing depression in individuals who overcome this period after the effect of the pandemic in Turkey ends. Moreover, considering this pandemic as a social crisis, this study is important in terms of realizing the seriousness of the conditions and demonstrating its effects on the society. This study will also approach subjects such as implementing strengthening programs and developing coping skills by determining the groups most affected by the pandemic.
This study was carried out to determine depression levels and related factors in a society affected by COVID-19.
Method
Study design
This study was planned using the descriptive cross-sectional design, a quantitative research method.
Time and place of the study
The study was carried out between March 23 and April 3, 2020. It started 2 weeks after the first confirmed diagnosis of COVID-19 in Turkey and was completed within 12 days in seven regions.
Population and sample
The random opportunistic online sample was determined for this study representing the Turkish society. All individuals who met the inclusion criteria and answered the questions completely were included in the study sample. Inclusion criteria were as follows:
Being a citizen of Turkish Republic.
Being an adult between 18 and 65 years of age.
Exclusion criteria were as follows:
Receiving treatment at the hospital during the time that the study was in progress.
Having been diagnosed with COVID-19.
Having been diagnosed with psychiatric illness.
The study was completed with 1115 participants; 44 of the 1159 original participants were excluded from the study for reason of having a psychiatric illness diagnosis.
Data collection tools
The study data were collected using a Personal Information Form that was developed by the researcher and the Beck Depression Inventory (BDI).
Personal Information Form: the Personal Information Form includes closed-ended questions that include participants’ sociodemographic characteristics, their personal, family-related, social, educational, or word-related problems, mental disorders that they experienced due to the COVID-19 pandemic, and how they handled the “quarantine/lockdown” process initiated to prevent the pandemic from spreading further.
BDI: the Turkish validity and reliability study of the inventory developed by Beck (1961) was carried out by Hisli (1989). The BDI is a 21-item self-evaluation scale that measures depression symptoms. Every item is scored from 0 to 3; possible scores range from 0 to 63. It was suggested that those who obtain 17 and more points are in the group with a risk for depression (Hisli, 1989). Depression levels were defined as follows: 0–9, minimal; 10–16, mild; 17–29, medium; 30–63, severe (Kilinc & Torun, 2011). The Cronbach’s alpha value of Hisli’s validity and reliability study was .74, that of this study was .90.
Study process
Data collection forms were opened for access through Google Forms over the internet as online questionnaires using social media channels. Announcements open for sharing were made via Instagram, Facebook, WhatsApp, LinkedIn, and Twitter accounts, and messages were sent for further spread of the announcements. The participants filled out the forms in approximately 10 minutes.
The first COVID-19 case in Turkey was diagnosed on March 11, 2020. Administration of the questionnaire continued for 12 days between the 13th and 24th days of the pandemic and was completed when the number of valid questionnaires reached 1115. The duration of the study was planned according to the quarantine measures of the Ministry of Health. During the 12-day period during which the administration of the questionnaire continued, a lockdown was imposed on individuals over 65 years of age in addition to precautions such as closing workplaces, schools, and universities, making an effort to obey the lockdown, and minimizing human contact. Entry/exit restrictions to 30 metropolitan areas and the Zonguldak municipality and a face mask obligation in markets and bazaars were implemented; a lockdown was imposed on individuals under the age of 20 in April 4, 2020, in addition to the precautions already in place.
Because the most recent residence- and age-related measures would have affected the sample group, the study was concluded on April 3, 2020. The response rate of the questionnaires, and the speed of questionnaires reaching the potential audience, decreased, which led to the discontinuing of administration of the questionnaire.
Ethical considerations
The Ministry of Health (consent code: T17_25_46) and the Amasya University Clinical Research Ethics Committee (consent number: 15,386,878-044) granted permission for the study. Participants were provided with an obligatory informed consent form before they accessed the questionnaire forms.
Data analysis
The data were evaluated using the IBM SPSS Statistics, version 20 software program. Descriptive statistics were calculated for the classification of study data and explanation of their characteristics. Because the variables were not normally distributed, Mann–Whitney U-test was used for the comparison of two groups, and the Kruskal–Wallis H test was used for the comparison of three or more groups. For the evaluation of the results, the significance level was accepted as 0.05: p < .05 indicated a significant difference, and p > .05 indicated no significant difference. When there was a significant difference between more than two groups, multiple comparison was carried out using the Mann–Whitney U-test to determine the source of the significance. The significance level 0.05 was determined to be the comparison threshold.
Results
The mean age of the 1115 participant was 27.98 ± 8.79 years (min. = 18, max. = 65), 71.7% of the participants were female, 62.9% were single, 69.9% had graduated from university, 42.7% were students, and 26.9% were public employees (Table 1). Participants’ mean depression score was 12.07 ± 9.60 (min. = 0.00, max. = 63); therefore, the overall depression was at the mild level. Among the participants, 47% showed minimal-level depression symptoms (0–9 points); 25.7%, mild-level depression symptoms (10–16 points); 22.3%, moderate-level depression symptoms (17–29 points); and 5%, severe depression symptoms (30–63 points) (Figure 1).
Table 1.
Comparison of participants’ sociodemographic characteristics and depression.
| Variables |
n
|
% |
BDI |
Significance |
||
|---|---|---|---|---|---|---|
| 1115 | 100 | Mean ± SD | Mean rank | Test | p | |
| Age groups | ||||||
| 18–29 years of age | 693 | 62.2 | 13.13 ± 10.07 | 592.07 |
χ2 = 22.366 Multiple comparisons (1–2) (1–3) (1–4) |
p = .000 |
| 30–39 years of age | 291 | 26.1 | 10.54 ± 8.69 | 509.34 | ||
| 40–49 years of age | 103 | 9.2 | 10.24 ± 8.04 | 502.88 | ||
| 50–65 years of age | 28 | 2.5 | 8.25 ± 7.80 | 423.20 | ||
| Gender | ||||||
| Female | 799 | 71.7 | 12.98 ± 9.81 | 590.75 | Z = −5.404 | p = .000 |
| Male | 316 | 28.3 | 9.75 ± 8.62 | 475.20 | ||
| Education level | ||||||
| Primary school and secondary school | 50 | 4.5 | 11.98 ± 9.54 | 556.72 |
χ2 = 11.544 Multiple comparisons (2–4) (3–4) |
p = .009 |
| High school | 131 | 11.7 | 12.48 ± 9.49 | 577.85 | ||
| University | 779 | 69.9 | 12.45 ± 9.74 | 570.84 | ||
| Postgraduate | 155 | 13.9 | 9.79 ± 8.70 | 477.08 | ||
| Profession | ||||||
| Student | 476 | 42.7 | 13.68 ± 10.34 | 608.30 |
χ2 = 23.939 Multiple comparisons (1–2) |
p = .000 |
| Public employee | 300 | 26.9 | 10.11 ± 8.32 | 495.50 | ||
| Private sector employee | 150 | 13.5 | 11.65 ± 9.97 | 535.94 | ||
| Own business | 45 | 4.0 | 11.37 ± 8.97 | 539.46 | ||
| Unemployed | 110 | 9.9 | 11.55 ± 8.38 | 554.30 | ||
| Other | 34 | 3.0 | 11.23 ± 8.84 | 539.10 | ||
| Income status | ||||||
| Income lower than expenses | 270 | 24.2 | 15.37 ± 10.84 | 661.89 |
χ2 = 38.018 Multiple comparisons (1–2) (1–3) |
p = .000 |
| Equal income and expenses | 590 | 52.9 | 11.14 ± 8.80 | 531.61 | ||
| Income higher than expenses | 255 | 22.9 | 10.72 ± 9.18 | 509.05 | ||
| Region of residence | ||||||
| Mediterranean region | 66 | 5.9 | 12.34 ± 9.06 | 581.87 |
χ2 = 14.150 Multiple comparisons (2–4) (4–6) (4–7) |
p = .028 |
| East Anatolia | 46 | 4.1 | 10.28 ± 9.89 | 476.77 | ||
| Aegean region | 67 | 6.0 | 12.14 ± 8.81 | 572.12 | ||
| Southeastern Anatolia | 55 | 4.9 | 16.30 ± 11.50 | 692.50 | ||
| Central Anatolia | 175 | 15.7 | 12.65 ± 10.49 | 566.99 | ||
| Black Sea region | 508 | 45.6 | 11.66 ± 9.04 | 550.00 | ||
| Marmara region | 198 | 17.8 | 11.70 ± 9.73 | 539.37 | ||
| Place of residence | ||||||
| City center | 653 | 58.6 | 11.77 ± 9.26 | 550.78 | χ2 = 0.905 | p = .636 |
| County town | 357 | 32.0 | 12.48 ± 10.26 | 565.48 | ||
| Village | 105 | 9.4 | 12.51 ± 9.33 | 577.44 | ||
| Marital status | ||||||
| Single | 701 | 62.9 | 12.88 ± 10.09 | 581.83 | Z = −3.218 | p = .001 |
| Married | 414 | 37.1 | 10.68 ± 8.52 | 517.65 | ||
| Individuals participants are living with | ||||||
| Alone | 75 | 6.7 | 9.60 ± 8.59 | 469.85 | χ2 = 6.431 | p = .092 |
| Nuclear family (single partner/partner and children) | 772 | 69.2 | 11.97 ± 9.20 | 560.90 | ||
| Extended family (partner, children, and family elders) | 149 | 13.4 | 13.30 ± 11.29 | 578.21 | ||
| Other | 119 | 10.7 | 12.68 ± 10.20 | 569.46 | ||
| Individuals over 65 years of age for whom the participants should provide care or with whom they live together | ||||||
| Yes | 181 | 16.2 | 12.40 ± 9.62 | 570.81 | Z = −0.585 | p = .558 |
| No | 934 | 83.8 | 12.00 ± 9.59 | 555.52 | ||
BDI: Beck Depression Inventory.
Bold values denote statistical significance at the p < 0.05 level.
Figure 1.
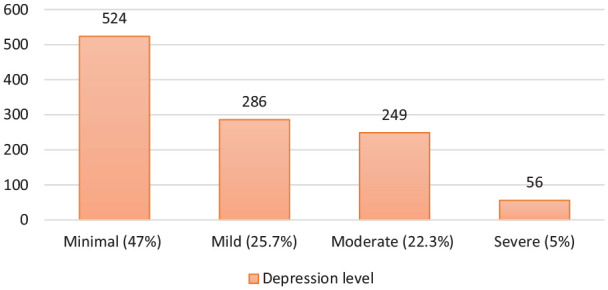
Distribution of participants regarding their depression levels.
Table 1 shows the comparison of participants’ sociodemographic characteristics and depression scores. In an analysis of participants’ gender and marital status, those who were female and single had significantly higher depression levels than other participants (p < .05). There was a significant difference between participants’ depression scores in terms of their age groups, education status, occupation, income levels, and place of residence (p < .05). The depression levels were higher in the 18–29 year age group than in other groups, in students than in public employees, in individuals who had income lower than their expenses than among other participants. Participants who had completed an undergraduate education had significantly lower levels of depression than those who had graduated from high school or university. No significant difference was found between depression levels in terms of participants’ place of residence, people they were living with, and participants’ family members over 65 years of age who needed care (p > .05).
Table 2 shows the comparison of participants’ COVID-19–related characteristics and depression scores. No significant difference was found between depression scores in terms the following characteristics: having a chronic illness determined by the Ministry of Health to be within the risk group; taking a COVID-19 test; whether a family member took a COVID-19 test or having been diagnosed with the disease; to what extent respondents said they pay attention to and follow the warnings of the Ministry of Health; the information sources; and the person with whom the participants go through this process (p > .05). Participants who said that they need psychological support during the quarantine had significantly higher depression levels than others (p < .05). It was found that the participants who took the COVID-19 test and reported that they need psychological support during the quarantine showed moderate-level depression symptoms and were in the risk group for depression.
Table 2.
Comparison of participants’ COVID-19 characteristics and depression scores.
| Variables |
N
|
% |
BDI |
Significance |
|||
|---|---|---|---|---|---|---|---|
| 1115 | 100 | Mean ± SD | Mean rank | Test | p | ||
| Do you have a chronic illness that the Ministry of Health determined for the risk groups? | |||||||
| Yes | 101 | 9.1 | 12.55 ± 8.94 | 588.37 | Z = −0.995 | p = .320 | |
| No | 1014 | 90.9 | 12.02 ± 9.66 | 554.97 | |||
| Did you take a test after you had a suspicion of COVID-19? | |||||||
| Yes | 3 | 0.3 | 23.66 ± 26.10 | 693.50 | Z = −0.730 | p = .465 | |
| No | 1112 | 99.7 | 12.03 ± 9.52 | 557.63 | |||
| Did a family member of yours take a test after they had a suspicion of COVID-19? | |||||||
| Yes | 34 | 3.0 | 13.82 ± 8.27 | 646.07 | Z = −1.621 | p = .105 | |
| No | 1081 | 97.0 | 12.01 ± 9.63 | 555.23 | |||
| Was a family member of your diagnosed with COVID-19? | |||||||
| Yes | 12 | 1.1 | 12.83 ± 8.00 | 610.92 | Z = −0.573 | p = .567 | |
| No | 1103 | 98.9 | 12.06 ± 9.61 | 557.42 | |||
| To what extent do you pay attention to and apply COVID-19 pandemic warnings? | |||||||
| I do not pay attention to them at all | 3 | 0.3 | 15.66 ± 5.85 | 753.33 | χ2 = 5.375 | p = .146 | |
| I partly pay attention to them | 42 | 3.8 | 15.66 ± 13.88 | 612.40 | |||
| I pay attention to them | 452 | 40.5 | 11.34 ± 9.15 | 535.41 | |||
| I pay attention to them too much | 618 | 55.4 | 12.33 ± 9.53 | 569.87 | |||
| With whom do you frequently spend the quarantine period? | |||||||
| Alone | 84 | 7.5 | 11.02 ± 8.87 | 528.63 | χ2 = 2.073 | p = .557 | |
| Family | 962 | 86.3 | 12.12 ± 9.50 | 561.99 | |||
| Friend | 24 | 2.2 | 11.45 ± 12.01 | 486.10 | |||
| Colleague | 45 | 4.0 | 13.13 ± 11.59 | 565.77 | |||
| Do think you need psychological support during this period? | |||||||
| Yes | 278 | 24.9 | 19.30 ± 10.81 | 786.13 | Z = −13.645 | p = .000 | |
| No | 837 | 75.1 | 9.66 ± 7.80 | 482.23 | |||
| Which resources do you use to obtain information about COVID-19 a | |||||||
| I do not follow the agenda | Yes | 151 | 13.5 | 11.74 ± 10.74 | 529.22 | Z = −1.182 | p = .237 |
| No | 964 | 86.5 | 12.12 ± 9.41 | 562.51 | |||
| Television and internet news | Yes | 774 | 69.4 | 12.27 ± 9.68 | 564.92 | Z = −1.082 | p = .279 |
| No | 341 | 30.6 | 11.60 ± 9.39 | 542.29 | |||
| Social media | Yes | 544 | 48.8 | 12.64 ± 10.25 | 570.67 | Z = −1.284 | p = .199 |
| No | 571 | 51.2 | 11.52 ± 8.90 | 545.93 | |||
| Ministries and government agencies | Yes | 770 | 69.1 | 11.88 ± 9.54 | 551.00 | Z = −1.085 | p = .278 |
| No | 345 | 30.9 | 12.48 ± 9.72 | 573.62 | |||
| Healthcare professionals | Yes | 261 | 23.4 | 12.50 ± 10.63 | 559.61 | Z = −0.092 | p = .926 |
| No | 854 | 76.6 | 11.93 ± 9.26 | 557.51 | |||
| Scientific researches | Yes | 239 | 21.4 | 11.10 ± 9.22 | 522.08 | Z = −1.947 | p = .052 |
| No | 876 | 78.6 | 12.33 ± 9.68 | 567.80 | |||
| Friends and relatives | Yes | 197 | 17.7 | 12.48 ± 10.13 | 567.95 | Z = −0.478 | p = .632 |
| No | 918 | 82.3 | 11.98 ± 9.48 | 555.86 | |||
BDI: Beck Depression Inventory.
Bold values denote statistical significance at the p < 0.05 level.
Multiple options were marked and the percentages were calculated over the sample size.
Of the participants, 86.3% went through this period accompanied by their families; 55.4% claimed to pay too much attention to the COVID-19 pandemic warnings; 69.4% used television and internet news; and 69.1% used the resources of the ministries and government agencies for obtaining information about the COVID-19 pandemic (Table 2).
Table 3 shows the problems that participants frequently encountered as a result of the pandemic and their mean depression scores. In analyzing the personal problems of participants, those who reported that their daily routine and cleaning habits changed, and that they were exposed to social media more than previously had significantly higher depression scores than others (p < .05).
Table 3.
Comparison of participants’ problems during the quarantine and their depression scores.
| Variables |
n
|
% |
BDI |
Significance |
|||
|---|---|---|---|---|---|---|---|
| 1115 | 100 | Mean ± SD | Mean rank | Test | p | ||
| Situation that personally affected you the most a | |||||||
| I was not affected at all | Yes | 93 | 8.3 | 6.79 ± 8.21 | 343.40 | Z = −6.718 | p = .000 |
| No | 1022 | 91.7 | 12.55 ± 9.57 | 577.53 | |||
| My daily routines (such as meals, sleep, shopping) have changed | Yes | 521 | 46.7 | 14.05 ± 10.36 | 622.00 | Z = −6.220 | p = .000 |
| No | 594 | 53.3 | 10.32 ± 8.50 | 501.87 | |||
| My cleaning habits (such as washing hands, cleaning the house) have changed | Yes | 647 | 58.0 | 12.76 ± 9.69 | 584.96 | Z = −3.290 | p = .001 |
| No | 468 | 42.0 | 11.11 ± 9.38 | 520.73 | |||
| I was exposed to social media more than before | Yes | 538 | 48.3 | 13.37 ± 9.75 | 607.74 | Z = −4.985 | p = .000 |
| No | 577 | 51.7 | 10.85 ± 9.30 | 511.62 | |||
| Situation in the family and social life that affected you the most a | |||||||
| I was not affected at all | Yes | 93 | 8.3 | 6.50 ± 7.46 | 339.78 | Z = −6.831 | p = .000 |
| No | 1022 | 91.7 | 12.57 ± 9.61 | 577.86 | |||
| I have had to stay away from my family | Yes | 147 | 13.2 | 14.55 ± 10.87 | 629.65 | Z = −2.898 | p = .004 |
| No | 968 | 86.8 | 11.69 ± 9.34 | 547.12 | |||
| Meetings with my friends, relatives, and neighbors have become rare | Yes | 574 | 51.5 | 12.41 ± 9.53 | 573.41 | Z =−1.647 | p = .100 |
| No | 541 | 48.5 | 11.70 ± 9.66 | 541.65 | |||
| I drift apart from by entertainment and social life | Yes | 734 | 65.8 | 12.78 ± 10.03 | 579.35 | Z = −3.075 | p = .002 |
| No | 381 | 34.2 | 10.69 ± 8.53 | 516.87 | |||
| I have had to change my place of residence | Yes | 150 | 13.5 | 17.06 ± 11.48 | 705.18 | Z = −6.022 | p = .000 |
| No | 965 | 86.5 | 11.29 ± 9.03 | 535.12 | |||
| I got lonely | Yes | 60 | 5.4 | 17.33 ± 11.16 | 713.22 | Z = −3.842 | p = .000 |
| No | 1055 | 94.6 | 11.77 ± 9.42 | 549.17 | |||
| Situation in your work/education life that affected you the most a | |||||||
| I was not affected at all | Yes | 161 | 14.4 | 9.54 ± 8.98 | 460.11 | Z = −4.173 | p = .000 |
| No | 954 | 85.6 | 12.49 ± 9.64 | 574.52 | |||
| I drifted apart from my school/work place | Yes | 642 | 57.6 | 12.44 ± 9.85 | 569.11 | Z = −1.343 | p = .179 |
| No | 473 | 42.4 | 11.56 ± 9.23 | 542.93 | |||
| My financial income has been negatively affected | Yes | 159 | 14.3 | 15.39 ± 9.62 | 680.76 | Z = −5.196 | p = .000 |
| No | 956 | 85.7 | 11.51 ± 9.48 | 537.58 | |||
| I had to go to work | Yes | 193 | 17.3 | 12.16 ± 9.08 | 570.18 | Z = −0.579 | p = .563 |
| No | 922 | 82.7 | 12.05 ± 9.70 | 555.45 | |||
| I had to close down my business | Yes | 27 | 2.4 | 15.14 ± 8.47 | 694.02 | Z = −2.224 | p = .026 |
| No | 1088 | 97.6 | 11.99 ± 9.61 | 554.62 | |||
| I had to work from home | Yes | 159 | 14.3 | 10.50 ± 8.69 | 507.03 | Z = −2.157 | p = .031 |
| No | 956 | 85.7 | 12.33 ± 9.72 | 566.48 | |||
| Situation that affected your mental health the most a | |||||||
| I was not affected at all | Yes | 100 | 9.0 | 5.28 ± 6.94 | 284.37 | Z = −8.914 | p = .000 |
| No | 1015 | 91.0 | 12.73 ± 9.56 | 584.96 | |||
| I was afraid to be infected by the virus | Yes | 611 | 54.8 | 13.36 ± 9.79 | 606.72 | Z = −5.567 | p = .000 |
| No | 504 | 45.2 | 10.49 ± 9.12 | 498.94 | |||
| I was afraid to infect others with the virus | Yes | 508 | 45.6 | 13.41 ± 9.87 | 607.32 | Z = −4.682 | p = .000 |
| No | 607 | 54.4 | 10.94 ± 9.21 | 516.72 | |||
| I experienced fear of death | Yes | 203 | 18.2 | 18.78 ± 10.94 | 770.16 | Z = −10.388 | p = .000 |
| No | 912 | 81.8 | 10.57 ± 8.59 | 510.78 | |||
| I have started to experience cleaning obsession | Yes | 360 | 32.3 | 14.88 ± 10.36 | 653.93 | Z = −6.875 | p = .000 |
| No | 755 | 67.7 | 10.72 ± 8.91 | 512.26 | |||
| I felt useless and worthless | Yes | 48 | 4.3 | 24.39 ± 11.61 | 894.59 | Z = −7.409 | p = .000 |
| No | 1067 | 95.7 | 11.51 ± 9.12 | 542.86 | |||
| I was worried about my future | Yes | 486 | 43.6 | 15.29 ± 10.09 | 671.85 | Z = −10.386 | p = .000 |
| No | 629 | 56.4 | 9.58 ± 8.39 | 470.03 | |||
| I was unhappy | Yes | 498 | 44.7 | 14.13 ± 10.22 | 627.35 | Z = −6.466 | p = .000 |
| No | 617 | 55.3 | 10.40 ± 8.72 | 502.03 | |||
| I experienced anxiety | Yes | 500 | 44.8 | 15.45 ± 9.99 | 678.62 | Z = −11.287 | p = .000 |
| No | 615 | 55.2 | 9.31 ± 8.31 | 459.93 | |||
| I experienced hopelessness | Yes | 352 | 31.6 | 17.70 ± 10.07 | 749.54 | Z = −13.502 | p = .000 |
| No | 763 | 68.4 | 9.47 ± 8.16 | 469.63 | |||
| I experienced sleep problems | Yes | 216 | 19.4 | 19.68 ± 9.91 | 810.22 | Z = −12.831 | p = .000 |
| No | 899 | 80.6 | 10.24 ± 8.57 | 497.40 | |||
| I started to smoke and use alcohol | Yes | 24 | 2.2 | 26.20 ± 10.85 | 937.60 | Z = −5.843 | p = .000 |
| No | 1091 | 97.8 | 11.75 ± 9.33 | 549.65 | |||
BDI: Beck Depression Inventory.
Bold values denote statistical significance at the p < 0.05 level.
Multiple options were marked and the percentages were calculated over the sample size.
In analyzing the situations affecting participants’ family relationships and social life, participants who had to be away from their family, place of residence, entertainment, and social life, and those who reported that they felt lonely during this process, had significantly higher depression scores than others (p < .05). Participants who had to change their place of residence and were lonely were in the risk group and had moderate-level depression (Table 3).
In the analysis of situations affecting participants’ work and educational life, those who had to close their business and reported that their financial income was affected negatively had significantly higher depression scores than others (p < .05). Participants who could not go to school or had to work from home had significantly lower depression scores (p < .05). In comparing the depression scores of those who had to be away from their school or work and had to go to work with others, no significant difference was found (p > .05; Table 3).
There was a significant difference between the participants’ depression scores and their psychological problems experienced during this period (p < .05). The participants who were afraid of being infected by the virus or infecting others, were obsessed with cleaning, had anxiety about the future, were unhappy and anxious, and were found to have mild-level depression scores. The depression levels of participants who experienced fear of death, feeling useless and worthless, hopelessness, sleep problems, and started to smoke and consume alcohol were found to be at a moderate level (Table 3).
In analyzing the situations participants are frequently affected during the quarantine, 58% of them reported that their cleaning habits changed, 65.8% that they were feeling deprived of their entertainment and social life, and 57.6% said that they were deprived of their school and workplace. Moreover, 54.8% of the participants reported that they experienced fear of being infected by the virus, and 45.6% that they experienced fear of infecting others with the virus (Table 3).
Table 4 shows the comparison of participants’ coping strategies (behaviors that helped them to feel better during the quarantine) and their depression scores. The most helpful methods for the participants were spending time with their families (56.5%) and making more time for themselves (51.6%). Participants who spent time with their families, made time for themselves, and were busy with home education or work were found to have significantly lower depression scores than others (p < .05). Participants who used social media, communicated with their friends through phone calls or video calls, and cleaned their houses more often had significantly higher depression scores than others (p < .05). It was found that behaviors such as going on a walk, exercising, sleeping regularly, eating a balanced diet, and praying created no significant difference in depression scores (p > .05); however, participants who applied those behaviors had lower depression levels than others.
Table 4.
Comparison of participants’ coping methods during the quarantine and their depression scores.
| Variables |
n
|
% |
BDI |
Significance |
|||
|---|---|---|---|---|---|---|---|
| 1115 | 100 | Mean ± SD | Mean rank | Test | p | ||
| Coping strategies during the quarantine period a | |||||||
| Sparing time for myself (reading book, watching movies, etc.) | Yes | 575 | 51.6 | 11.26 ± 9.13 | 531.08 | Z = −2.883 | p = .004 |
| No | 540 | 48.4 | 12.93 ± 10.00 | 586.67 | |||
| Spending time with my family | Yes | 630 | 56.5 | 10.92 ± 8.46 | 527.34 | Z = −3.626 | p = .000 |
| No | 485 | 43.5 | 13.56 ± 10.72 | 597.82 | |||
| Spending time on social media | Yes | 317 | 28.4 | 13.98 ± 9.68 | 630.15 | Z = −4.719 | p = .000 |
| No | 798 | 71.6 | 11.31 ± 9.46 | 529.34 | |||
| Talking to my friends through phone call or video call | Yes | 276 | 24.8 | 14.09 ± 11.39 | 606.68 | Z = −2.898 | p = .004 |
| No | 839 | 75.2 | 11.40 ± 8.83 | 541.99 | |||
| Working (doing my job/studying) | Yes | 279 | 25.0 | 10.58 ± 8.82 | 508.90 | Z = −2.944 | p = .003 |
| No | 836 | 75.0 | 12.56 ± 9.79 | 574.39 | |||
| Cleaning the house | Yes | 336 | 30.1 | 13.46 ± 10.32 | 602.30 | Z = −3.020 | p = .003 |
| No | 779 | 69.9 | 11.47 ± 9.21 | 538.89 | |||
| Going on a walk in open areas | Yes | 58 | 5.2 | 11.44 ± 10.29 | 519.22 | Z = −0.943 | p = .346 |
| No | 1057 | 94.8 | 12.10 ± 9.56 | 560.13 | |||
| Exercising | Yes | 112 | 10.0 | 10.43 ± 7.78 | 517.24 | Z = −1.413 | p = .158 |
| No | 1003 | 90.0 | 12.25 ± 9.76 | 562.55 | |||
| Sleeping regularly | Yes | 187 | 16.8 | 11.28 ± 10.28 | 519.06 | Z = −1.814 | p = .070 |
| No | 928 | 83.2 | 12.22 ± 9.45 | 565.85 | |||
| Eating regularly | Yes | 201 | 18.0 | 11.63 ± 9.72 | 540.59 | Z = −0.847 | p = .397 |
| No | 914 | 82.0 | 12.16 ± 9.57 | 561.83 | |||
| Praying | Yes | 332 | 29.8 | 11.86 ± 9.12 | 556.76 | Z = −0.084 | p = .933 |
| No | 783 | 70.2 | 12.15 ± 9.79 | 558.53 | |||
BDI: Beck Depression Inventory.
Bold values denote statistical significance at the p < 0.05 level.
Multiple options were marked and the percentages were calculated over the sample size.
Discussion
The COVID-19 pandemic caused psychological problems in China and other societies that were similarly affected (J. B. Li et al., 2020; Xiao, 2020). One of the first studies that determined the psychological problems of China’s general population was carried out by Qiu et al. (2020). It collected 52,730 valid questionnaires from 36 provinces, self-governing territories, and municipalities, Hong Kong, Macau, and Taiwan. Of the individuals participating in the questionnaire, 35% experienced psychological problems. In the study of Wang et al. (2020), 53.8% of the general population of China regarded the psychological effect of the pandemic to be moderate or severe.
Administration of strict quarantine measures never previously experienced caused people to gradually drift apart from one another and caused isolation in the society (Qiu et al., 2020; Xiao, 2020). Lack of interpersonal communication can also cause or worsen depression (Xiao, 2020). In studies evaluating a society’s overall mental health in terms of COVID-19 through online questionnaires in 31 provinces and self-governing territories of China, individuals above 18 years of age experienced depression (Gao et al., 2020; Liu et al., 2020). In the study by Gao et al. (2020), carried out with 4,872 participants, 48.3% showed depression symptoms. In the study of Liu et al. (2020) of the 14,592 participants, 53.5% showed depression symptoms.
In the study carried out with 1210 participants in 194 cities in China using online questionnaires, 69.7% of the participants were found to be normal, 13.8% had mild-level depression, 12.2% had moderate-level depression, and 4.3% had severe- or extreme-level depression (Wang et al., 2020). In this study, with participants from all regions of Turkey, participants’ mean depression scores were at a mild level: 47% of the participants showed minimal-level depression symptoms, 25.7% mild-level depression symptoms, 22.3% moderate-level depression symptoms, and 5% severe-level depression symptoms.
In different studies carried out during the pandemic, certain sociodemographic characteristics affected depression levels. Similarly to the current study, these studies also determined that being female, a student (Wang et al., 2020), and young and single (Liu et al., 2020) are risk factors for depression. Females were more inclined to depression, which may have inclined them to be more affected by the pandemic. Although being away from school might seem to be an advantage for students, it can be concluded that in an education system that is unfamiliar and the uncertainty of the process in that system may have caused depression symptoms. Because younger and single individuals use social media more than others, they often obtain excessive and inaccurate information that may have triggered depression.
Trusting in the measures taken by the government and trying to adapt better encourage the society to work together support the struggle against the pandemic (Ho et al., 2020). In Italy, 3,452 young adults above 18 years of age reported being cautious about health measures recommended for countering the COVID-19 pandemic. Approximately 100% of the participants approved four public health measures: 95.2% avoided hand shaking, 94.7% avoided social communities, 93.1% followed lockdown for nonobligatory activities, and 89% approved closing non-mandatory shops (Barari et al., 2020). In this study, 95.9% of the participants reported that they pay attention to and apply the measures recommended by the Ministry of Health. Participants who followed the recommendations had lower depression points than the ones who did not.
Insufficient information and tabloid news about COVID-19 caused the anxiety and fear against the situation to increase (Jiloha, 2020; J. B. Li et al., 2020; Shigemura et al., 2020). The WHO emphasized that people should minimize their habit of following news about COVID-19, and that they should obtain information only once or twice daily during certain hours and only from reliable sources. In addition, following the WHO (2020c) website and local health authority platforms is also recommended to distinguish accurate from inaccurate information. Of the participants, 69.1% obtained information from the Ministry and government agencies. However, people who obtained information from social media constituted 48.8% of the study; this group had the highest depression score as compared to other groups.
It is important for individuals to maintain their daily routines, regular life activities, and join entertaining activities for coping with their personal problems during the quarantine (Jiloha, 2020; Park & Park, 2020). Depression scores of the participants who stated that their daily routine and cleaning habits changed and were exposed to social media more were higher compared to those of others. In a study conducted in the China, more than 80% of the participants stated that they were exposed to social media more than before and that was positively correlated with their anxiety level (Gao et al., 2020).
Minimizing the contact among people to prevent spreading the virus requires a conscious effort. In contagious diseases, including COVID-19, social distancing should be minded even in groups that show no symptoms and are not at risk. People should avoid public places and stay at home. They should leave 1 m distance from other people when they are outdoors (Jiloha, 2020). Despite social distance warnings, staying in touch with family, friends, and colleagues is recommended as coping methods (Park & Park, 2020). This study determined that those who were alone during the quarantine were in the risk group for depression and had moderate-level depression symptoms. However, those who communicated with their friends through voice or video calls were found to be more depressive. This situation may have arisen because people experiencing psychological problems want to get in touch with others more frequently.
Because closing public services and the collapse of the industries negatively affected the economy, many people experienced financial losses and were exposed to a risk of unemployment. This situation intensified the negative emotions individuals experienced (Ho et al., 2020). People who stated that they had to close their businesses and their financial income was negatively affected had higher depression scores, but depression scores of the people who did not go to work and had to work from home were found to be lower. Because staying at home decreased infection risk, provided a safer environment than the workplace, and provided the opportunity to spend more time with their families, working from home can be seen as an advantage.
Different studies evaluating mental effects of the COVID-19 pandemic on society found that people often experienced anxiety, despair, fear of being infected, worry, hopelessness, and sleep deprivation (Dong & Bouey, 2020; Gao et al., 2020; Ho et al., 2020; W. Li et al., 2020; Liu et al., 2020; Park & Park, 2020; Shigemura et al., 2020; Wang et al., 2020). In this study, people who experienced fear of being infected and infecting others, had a cleaning obsession, anxiety about the future, sadness, and anxiousness were found to have mild-level depression symptoms. Depression levels of participants who experienced fear of death, feeling useless and worthless, hopelessness, sleep problems, and started to smoke and consume alcohol were found to be at moderate level.
Limitations
This cross-sectional study had some limitations. Because the sample size was large, the questionnaires were carried out on the internet to make rapid evaluation possible. Therefore, access to elderly population (50–65 year of age) was limited (2.5% of the sample) and for the same reason, participation of younger individuals was higher (62.2% of the sample). Because the study was conducted in the Black Sea region of Turkey, participation from this region was higher (45.6% of the sample). Moreover, the sample was limited only to those who used social media; therefore, homogeneity of regions could not be achieved.
In this study, numerous parameters such as depression could have been evaluated with nonmeasurable variables. However, only a single variable was evaluated considering that the questionnaires were administrated online; the number of questions was planned so that the participants would not have difficulties in terms of time; and the access to internet could be limited. The study was carried out during the early periods of the quarantine process. Therefore, because there was no control group, it was uncertain whether the variables were affected by the quarantine process or by previously diagnosed depression.
Conclusion and recommendations
In Turkey, the COVID-19 pandemic caused mild-level depression in the society. The depression scores of female participants who were between 18 and 29 years of age, single, students, and had less income than their expenses were found to be higher than others. People who experienced fear of being infected and infecting others, had a cleaning obsession, anxiety about the future, sadness, and anxiousness experienced depression at lower levels when compared to other participants. Participants who had to change their place of residence during the quarantine, experienced loneliness, fear of death, hopelessness, sleep problems, felt useless and worthless, and started to smoke and drink alcohol experienced depression at moderate levels. Depression scores of those who spent time with their family, made time for themselves, were busy with home education or work were lower compared to others.
Early intervention programs and studies that will strengthen the society’s mental health should be carried out in groups at risk for depression. Studies analyzing effects of this period on mental health in different groups, defining the needs and problems of quarantined people should be carried out. Studies reevaluating the depression in individuals who overcame this period should be carried out after the pandemic ends.
Footnotes
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by author.
ORCID iD: Gonca Ustun  https://orcid.org/0000-0003-3548-4351
https://orcid.org/0000-0003-3548-4351
References
- Barari S., Caria S., Davola A., Falco P., Fetzer T., Fiorin S., Slepoi F. R. (2020). Evaluating COVID-19 public health messaging in Italy: Self-reported compliance and growing mental health concerns. IEEE Transactions on Visualization and Computer Graphics, 27, 46–68. 10.1101/2020.03.27.20042820 [DOI] [Google Scholar]
- Beck A. T., Ward C., Mendelson M., Mock J., Erbaugh J. (1961). Beck Depression Inventory (BDI). Archives of General Psychiatry, 4(6), 561–571. [DOI] [PubMed] [Google Scholar]
- Dong L., Bouey J. (2020). Public mental health crisis during COVID-19 pandemic, China. Emerging Infectious Diseases, 26(7), 1616–1618. 10.3201/eid2607.200407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Dai J., Zheng P., Chen H., Mao Y., Chen S., . . . Jia Y. (2020). Mental health problems and social media exposure during COVID-19 outbreak. PLOS ONE, 15(4), Article e0231924. 10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gralinski L. E., Menachery V. D. (2020). Return of the coronavirus: 2019-nCoV. Viruses, 12(2), 135. 10.3390/v12020135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hisli N. (1989). Validity and reliability of Beck Depression Inventory for university students. Journal of Psychology, 7(23), 3–13. [Google Scholar]
- Ho C. S., Chee C. Y., Ho R. C. (2020). Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Annals of the Academy of Medicine Singapore, 49(1), 1–6. https://www.ncbi.nlm.nih.gov/pubmed/32200399 [PubMed] [Google Scholar]
- Jiloha R. C. (2020). COVID-19 and mental health. Epidemiology International, 5(1), 7–9. 10.24321/2455.7048.202002 [DOI] [Google Scholar]
- Kickbusch I., Leung G. (2020). Response to the emerging novel coronavirus outbreak. BMJ, 368, Article m406. 10.1136/bmj.m406 [DOI] [PubMed] [Google Scholar]
- Kilinc S., Torun F. (2011). Depression rating scales used in clinical practice in Turkey. Dirim Medical Newspaper, 86, 39–47. [Google Scholar]
- Li J. B., Yang A., Dou K., Cheung R. Y. (2020). Self-control moderates the association between perceived severity of the coronavirus disease 2019 (COVID-19) and mental health problems among the Chinese public. 10.31234/osf.io/2xadq [DOI] [PMC free article] [PubMed]
- Li W., Yang Y., Liu Z. H., Zhao Y. J., Zhang Q., Zhang L., . . . Xiang Y. T. (2020). Progression of mental health services during the COVID-19 outbreak in China. International Journal of Biological Sciences, 16(10), 1732–1738. https://www.ijbs.com/v16p1732.htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Ren Y., Yan F., Li Y., Xu X., Yu X., . . . Tan S. (2020). Psychological impact and predisposing factors of the coronavirus disease 2019 (COVID-19) pandemic on general public in China. The Lancet Psychiatry. Advance online publication. 10.2139/ssrn.3551415 [DOI]
- Ministry of Health. (2020). Coronavirus table daily in Turkey. https://covid19.saglik.gov.tr/
- Park S. C., Park Y. C. (2020). Mental health care measures in response to the 2019 novel coronavirus outbreak in Korea. Psychiatry Investigation, 17(2), 85–86. 10.30773/pi.2020.0058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33(2), 1–2. 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigemura J., Ursano R. J., Morganstein J. C., Kurosawa M., Benedek D. M. (2020). Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry and Clinical Neurosciences, 74, 281–282. 10.1111/pcn.12988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C. S., Ho R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), Article 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020. a). Coronavirus (COVID-19). https://covid19.who.int/
- World Health Organization. (2020. b). Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- World Health Organization. (2020. c). Mental health and psychosocial considerations during the COVID-19 outbreak. https://www.who.int/publications-detail/WHO-2019-nCoV-MentalHealth-2020.1
- Xiao C. (2020). A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: Structured letter therapy. Psychiatry Investigation, 17(2), 175–176. 10.30773/pi.2020.0047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X. (2020). Psychological crisis interventions in Sichuan Province during the 2019 novel coronavirus outbreak. Psychiatry Research, 286, Author 112895. 10.1016/j.psychres.2020.112895 [DOI] [PMC free article] [PubMed] [Google Scholar]


