Abstract
Introduction:
Each year millions of patients undergo procedures that require moderate sedation. These patients are at risk of complications from oversedation that can progress to respiratory depression or even death. This article describes the creation of a simulation-based medical education course for nonanesthesiologists who use sedation in their specialty practice and preliminary data from our precourse and postcourse assessments.
Methods:
Our course combined online and lecture-based didactics with simulation education to teach moderate sedation and basic emergency airway management to nonanesthesiologists. After online precourse materials were reviewed, participants attended an 8-hour simulation-based training course focused on the recognition of different levels of sedation, medication titration, sedation reversal, and airway support and rescue. To evaluate the course, precourse, and postcourse educational impacts, cognitive and simulation tests were administered. Participants completed a postcourse survey.
Results:
To date, 45 physicians have participated in the course. We have cognitive performance data on 19 participants and survey data for 45 participants. Postcourse simulation tests results were improved compared with precourse tests. Our course was rated “better” or “much better” in comparison to courses using lecture-only format by 100% of the participants.
Conclusions:
A course using a combination of didactic and simulation education to teach moderate sedation is described. Our initial data demonstrated a significant increase in knowledge, skills, and clinical judgment. Future research efforts should focus on examining the validity and reliability of scenario scoring and the impact of training on clinical practice.
Keywords: Moderate sedation, Simulation-based medical education, Moderate sedation complications, ASA sedation guidelines
Millions of patients annually undergo diagnostic and therapeutic procedures under moderate sedation. According to the American Society of Anesthesiologists (ASA) guidelines, drug-induced sedation is graded at 3 levels (Table 1). Minimal sedation occurs when patients respond appropriately to verbal commands. Moderate sedation occurs when patients respond purposefully to verbal commands alone or accompanied by light tactile stimulation. Deep sedation occurs when patients are difficult to arouse but should respond purposefully after repeated or painful stimulation. General anesthesia is defined as a state in which the patient is unarousable even with painful stimuli.1 Medications are administered by the licensed physician performing the procedure or, as in most settings, by a registered nurse under physician supervision. Fourteen million colonoscopies, 1 million cardiac catheterizations, and 5 million wisdom teeth extractions are performed annually in the United States, with most of these procedures being performed under moderate sedation.2-5 A significant number of these patients are at risk of complications from oversedation that can progress from respiratory depression with hypoxemia to apnea and potentially to cardiac arrest.6
TABLE 1.
Definitions of Level of Sedation and Anesthesia9
| Minimal Sedation | Moderate Sedation/Analgesia | Deep Sedation/Analgesia | General Anesthesia | |
|---|---|---|---|---|
| Responsiveness | Normal response to verbal stimulation | Purposeful response to verbal or tactile stimulation | Purposeful response after repeated or painful stimulation | Unarousable even with painful stimulation |
| Airway patency | Unaffected | No intervention required normally* | Intervention may need to be required | Intervention often required |
| Spontaneous ventilation | Unaffected | Adequate* | May be inadequate | Frequently inadequate |
| Cardiovascular function | Unaffected | Usually maintained | Usually maintained* | May be impaired |
This table outlines the levels of sedation and anesthesia as defined by the ASA. Table entries in italics indicate where airway or cardiovascular intervention is required in the average adult patient.
Indicates how the level of intervention may be needed earlier in patients who are susceptible to airway obstruction (eg, patient with obstructive sleep apnea) or cardiovascular instability (eg, patients on multiple antihypertensive agents or with a dysrhythmia).
In a prospective study involving 594 adult interventional radiology patients, 4.7% had respiratory complications, 4.2% had oversedation complications, and 2% had severe hypotension or cardiopulmonary arrest.6 Alarmingly, 1 study, although from the 1980s, found a death rate caused directly by oversedation to be 1/5000 during colonoscopies.7 As noted previously, complications specific to sedation are usually a result of incorrect titration of the medication causing respiratory depression, which can ultimately lead to cardiac arrest. Frequently, there is a failure to recognize respiratory depression in a timely manner and failure to manage it with basic emergency airway management.8
The Joint Commission (TJC) has recognized both the increasing number of procedures being performed under moderate sedation and ensuing increase in complications.9 Together with the ASA, the TJC developed statements regarding granting of privileges for the administration of moderate sedation by nonanesthesia providers, as shown in Appendix 2.9 According to these guidelines, the nonanesthesiologist sedation practitioner who is to supervise or personally administer medications for moderate sedation should have satisfactorily completed a formal training program in (1) the safe administration of sedative and analgesic drugs used to establish a level of moderate sedation and (2) the rescue of patients who exhibit adverse physiologic consequences of a deeper-than-intended level of sedation. Although the TJC recommendations for moderate sedation training are extensive, it is up to each individual hospital or institution to determine their own set of credentialing criteria for granting moderate sedation administration privileges.10
The sedation goal for common procedures, such as colonoscopies or heart catheterizations, is either minimal or moderate, but patients can mistakenly be placed under deep sedation or general anesthesia. This can occur due to the practitioner not understanding common dosing ranges or a patient being particularly susceptible to medications that are used.8 Thus, training is needed, which is centered on the 3-fold goals as follows:
a proper understanding of the pharmacokinetics and pharmacodynamics of medications used for sedation;
an understanding of the levels of sedation and medication titration based on patient-specific responses to stimulation; and
appropriate rescue and management of the patient who becomes oversedated.
Simulation-based medical education (SBME) allows participants to learn and practice techniques without placing patients at risk. This is an ideal environment for a physician to learn administration, titration, and rescue of oversedated patients. Recently, a 3-level approach has been used to evaluate the impact of simulation training as translation science, T1 to T3.11 Numerous studies have shown that simulation can achieve the T1 level, which is where simulation training shows improvement in participant performance in the simulation setting. Fewer studies have shown that simulation training can achieve the T2 level, where results transfer to improved downstream patient care practices in the clinical setting. Only a few trials have actually translated improved performance in the simulation laboratory into improved patient outcomes in the clinical setting, the T3 level.11-13 For instance, simulation training has been found to improve patient outcomes in central venous catheter insertion, reduced mechanical ventilation infectious complications in intensive care units, and in obstetric and perinatal outcomes with respect to patient morbidity.14-20 However, improvement in patient outcomes through simulation training has not been demonstrated in the arena of moderate sedation. Thus, research that can demonstrate results at the T3 level for moderate sedation training programs will be of great importance.
In light of this need, we created a simulation-based moderate sedation course that includes basic emergency airway management (BEAM) to train nonanesthesiologist physicians who give or direct the administration of moderate sedation. We believe that the improper sedation of patients represents a serious patient safety issue that can be addressed by using SBME and that our pedagogic approach can be generalizable to any setting that has simulation technology. It is our future goal to demonstrate that this novel educational program may show improved patient safety by teaching physicians to avoid oversedation and to avert complications of oversedation and inadequate rescue. In the remainder of this article, we described the design and content of an SBME course for learning safe and effective practice for moderate sedation and baseline results of initial participant performance.
METHODS
Course Design
After review of the institutional review board, our course was designated an educational program evaluation and not in the purview of the institutional review board. The moderate sedation course consisted of 3 components. First, participants completed extensive online didactics (Table 2). Second, the BEAM component taught easy bag mask ventilation, difficult bag mask ventilation, and laryngeal mask airway (LMA) placement. Third, in the moderate sedation simulation component, multiple scenarios were created, scripted, and programmed for the purposes of training and evaluating participant performance in administering moderate sedation and reversal of oversedation. The scenarios use programmed simulator responses that varied based on the administration of different opioids and benzodiazepines (fentanyl, morphine, meperidine, hydromorphone, midazolam, and diazepam) and reversal drugs (naloxone and flumazenil). We chose the sedative options used in the course because they were commonly used by other specialties at our institution. Four different patient response types (normal, resistant, sensitive, and very sensitive) were also created. A list of all precourse and postcourse assessment components is described later and can be found in Table 3.
TABLE 2.
Online Precourse Modules
| I. | Goals of moderate sedation |
| II. | Educational requirements for personnel providing sedation |
| III. | Cardiopulmonary considerations |
| IV. | Pharmacologic review |
| V. | Patient monitoring |
| VI. | Facilities and equipment |
| VII. | Preprocedural preparation |
| VIII. | Development of a sedation plan |
| IX. | Postprocedural transport and recovery |
| X. | Diagnosis and management of risks associated with moderate sedation |
| XI. | Special considerations “(eg, cardiac and respiratory complications, nothing by mouth guidelines)” |
| XII. | TJC requirements and quality improvement |
TABLE 3.
Precourse and Postcourse Assessment Components
| Cognitive test | 50-MCQ test |
| Airway test | Easy bag mask ventilation test for 2 min* Difficult bag mask ventilation test for 2 min* Successful LMA placement within 2 min |
| Sedation test | Sedate a normal simulated patient to a level of moderate sedation Sedate a sensitive simulated patient to a level of moderate sedation Reverse a simulated patient from deep sedation Reverse a simulated patient from general anesthesia/apnea and support airway |
Passing this portion of the pretest and posttest required 2 minutes of adequate, sustained bag mask ventilation
Before attending the simulation course, participants completed 12 online training modules developed by 3 experienced anesthesiologists, which covered key concepts in line with TJC and ASA guidelines (Table 2). At the end of each module, there was a self-assessment quiz to help the participant ascertain if competency was achieved for that knowledge domain. After completion of the modules, participants were asked to complete a 50-question multiple-choice question (MCQ) pretest. The questions were selected from the total of all of the quiz questions used in the training modules. The modules and pretests were developed by 3 experienced anesthesiologists and were validated using medical students. A score of greater than 70% correct was considered passing. Questions and online course were designed to take approximately 6 hours to complete.
On the day of the course, all participants underwent baseline testing for airway management. The instructors did not determine passing grades. The BEAM simulation testing had specific guidelines for passing and failing grades, and the simulation programs generated these. To pass the BEAM component simulation pretest, one had to successfully perform easy mask ventilation (correct rate and tidal volume for 70% of 2 minutes), difficult mask ventilation (maintain oxygen saturation >90% for 2 minutes), and LMA placement (correct placement within 2 minutes).
Participants then attended brief lectures on BEAM, which were given by 1 of 2 experienced anesthesiologists who alternated in teaching the courses. The lectures included techniques on easy and difficult mask ventilation and proper LMA placement. The facilitators demonstrated easy mask ventilation skills on both Laerdal Resusci Anne. The skills that were demonstrated included appropriate hand positioning for holding the face mask, appropriate tidal volume and respiratory rate, and maneuvers to improve ventilation. Difficult airway skills were then demonstrated using the Advanced Life Support manikin (Laerdal Medical Corp, Stavanger, Norway), which is a high-fidelity simulator and has been modified in standardized manner and validated running these scenarios for 2 minutes with automated grading.21 This station included instruction on placement of oral and nasal pharyngeal airways, recognizing when to call for assistance and 2-person mask ventilation. Participants then practiced these airway management skills using practice simulator scenarios under the guidance of the course instructor. The facilitators were available to correct techniques and give immediate feedback. Time was allowed for questions and corrections of technique, if needed. The number of times the participants practiced varied based on their self-assessment and the instructor’s approval. Skills were repeated with deliberate practice until the instructor and participant were satisfied with the participant’s skill level. Participants were always offered the opportunity to continue to practice if they felt they needed more experience. Subsequently, all participants underwent a simulated BEAM posttest identical to the pretest. Any participants who failed any or all portions underwent immediate remediation and retesting until they passed. For this portion of our course, we used the Laerdal Resusci Anne, Advanced Life Support manikin (Laerdal Medical Corp). However, any platform could be used, which is able to provide the same level of monitoring and feedback concerning airway and ventilation management.
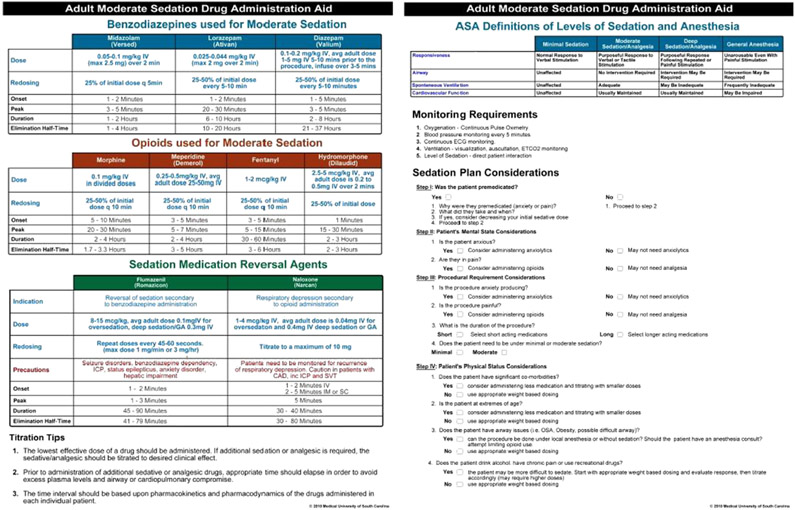
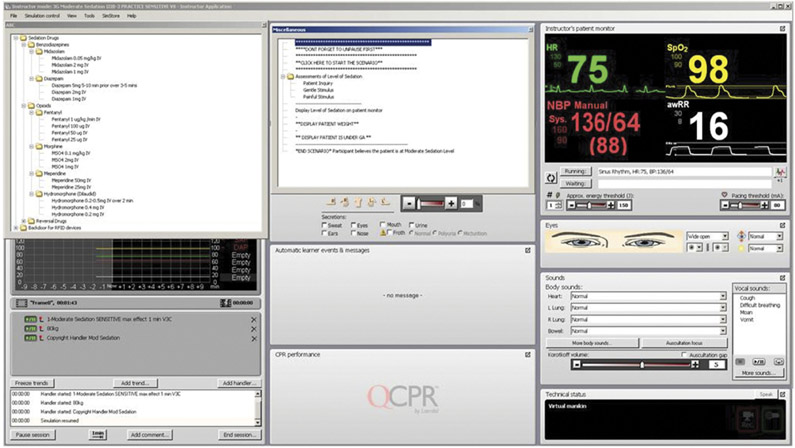
Following the airway portion, baseline testing for moderate sedation administration and reversal of oversedation was completed. After this skills-based portion of the training, lectures were then given on topics pertinent to moderate sedation. These included (1) patient screening, (2) nothing by mouth/fasting guidelines, (3) sedative and reversal pharmacokinetics and pharmacodynamics, (4) sedation planning, and (5) the titration of medications to a goal of moderate sedation. Participants individually completed several practice simulation scenarios. The other participants were able to watch and participate in the debriefing after each exercise by giving feedback regarding their patient evaluation, medication selection, and overall performance. Simulated scenarios required participants to titrate medications to reach a level of moderate sedation, to return patients to moderate sedation after a procedural stimulus, and to reverse a patient from the level of general anesthesia. The scenarios provided exposure to a variety of clinical settings and patient sensitivity. The participants were given cognitive aids (Fig. 1) that could be used during the course and in clinical practice. The simulation setup is seen in Figure 2, and a screenshot of the facilitator screen is shown in Figure 3. For the moderate sedation component of the course, we used the SimMan 3G (Laerdal Medical Corp). Again, any platform with comparable functionality should be able to be substituted.
FIGURE 1.
Moderate sedation cognitive aid. The aid includes the ASA levels of sedation, medication information (dosages, onsets, peaks, duration, precautions, and elimination half times), and requirements for patient monitoring and considerations when making a sedation plan, and information about titration strategies.
FIGURE 2.
The physical setup used during the moderate sedation component of the course. The facilitator stands to the right of the patient simulator, which is on a hospital bed. The participant is on the right side of the manikin with the monitor on their left so that they can easily visualize the vital signs, which appear on the screen as the scenario begins and will change with sedation administration. The participant has access to a peripheral intravenous line and medications in labeled syringes for administration.
FIGURE 3.
A screenshot from the facilitator program. Dropdown screens display the medication selection and dosages and scenario controls. Changes in sedation levels with medication administration are automatically generated and displayed for the facilitator in the bottom left dropdown screen.
After completion of practice scenarios, all participants were required to sedate 2 simulated patients to a level of moderate sedation and to reverse 2 patients from oversedation. Failure of these scenarios led to immediate remediation with the course instructor and retesting. Once the scenarios were successfully completed, a Web-based MCQ cognitive posttest was administered. The MCQ posttest was composed of questions from the same question bank as the pretest. A score of 70% or higher on the 50-question posttest was required to pass the course and receive a continuing medical education credit of 14 hours in moderate sedation training. Participants then completed a confidential online survey of the course, instructor, and experience at the simulation center (Appendix 1).
The Department of Anesthesia and Perioperative Medicine funded the development and validation of the course. The trainees tuition and instructor time was funded by the hospital to meet TJC standards that those administering moderate sedation must be qualified to do so as seen in Appendix 2.
Statistical Analysis
Participants’ mean pretest and posttest cognitive scores and the difference between pretest and posttest scores were calculated for the cognitive test. A paired t test was used to determine if the mean difference between pretest and posttest cognitive scores was greater than 0. The analysis was conducted in SAS version 9.2 (SAS Institute, Cary, NC).
Programming
The simulator included a state-based model with an associated flexible scenario editor that was programmed in the SimMan 2G and SimMan 3G simulators (Laerdal Medical Corp) Pharmacodynamic responses (patient response/level of sedation, respiratory rate, heart rate, blood pressure, oxygen saturation, and end-tidal CO2) to the sedation drugs were programmed through association of the individual drug dosage with a pharmacodynamic trend, which then would be applied to a base state for each dose in an additive fashion. This allowed for the use of multiple drugs to be administered with additive effects. Separately, a sedation scale was programmed with associated patient responses and eye opening (Tables 4 and 5) within the scenario program. These responses were designed to emulate the ASA guidelines for levels of sedation. Before course delivery, the simulator and scenarios were tested for construct and face validity by 5 anesthesiologists. Inputs for trainee interaction with the simulator including “patient inquiry (vocal questions),” “gentle stimulus,” and “painful stimulus” were programmed along with eye signs and respiratory sounds (ie, snoring), such that for a specific trainee interaction with the simulator (ie, checks level of sedation), a standardized response would occur for a given level of sedation (Tables 4 and 5). For example, under moderate sedation, the simulator has closed eyes, is lightly snoring, and does not respond to voice alone. With a gentle stimulus, he talks in a sleepy voice with half open eyes to say “I am gonna take a nap now.” With painful stimulus, the simulator opens his eyes wide to say, “Hey, what did you do that for?” Finally, for each drug dosage programmed, an impact on the overall sedation scale was linked, such that for each dose, it would increase the sedation score for sedatives and decrease it for reversal agents. Therefore, multiple doses or varying drug potencies would sedate the patient in a standardized manner. To create variant patient population responses (very sensitive, sensitive, normal, or resistant), the relative impact of drugs was individually increased or decreased within different scenarios. At any point during the simulation or at the end of a trainee implementing a sedation plan, one could click a menu item, and the level of sedation at that time would be displayed on the patient monitor to give immediate feedback to the participant.
TABLE 4.
Simulated Patient Vocal Responses for Depth of Sedation
| Sedation Level | None | Minimal Light | Minimal Deep | Moderate Light | Moderate Deep | Deep | General |
|---|---|---|---|---|---|---|---|
| Patient inquiry | It does not feel like you have given me anything. | I can tell you have given me something. | I am less anxious now | None | None | None | None |
| Gentle stimulus | I am still here | I am still here | I am still here | I am pretty sleepy now | I am going to take a nap. | None | None |
| Painful stimulus | Ouch | Ouch | Hey | Hey | Hey | Stop that (groggy) | None |
| Respiratory sounds | Normal | Normal | Normal | Light snoring | Light snoring | Loud snoring | None |
TABLE 5.
Simulated Patient Eye Status for Depth of Sedation
| Sedation Level | None | Minimal | Moderate | Deep | General |
|---|---|---|---|---|---|
| Baseline | Open | 1/2 Open | Closed | Closed | Closed |
| Patient inquiry | Open | 1/2 Open | Closed | Closed | Closed |
| Gentle stimulus | Open | Open Wide | 1/2 Open | Closed | Closed |
| Painful stimulus | Open | Open Wide | Open Wide | 1/2 Open | Closed |
To date, 45 practicing physicians have completed the moderate sedation educational simulation course. Our trainees were all from within our institution but represented different subspecialties including emergency medicine, critical care, trauma and transplant surgery, gastroenterology, radiology, oral surgery, pediatric cardiology, and pulmonology medicine.
The instructors were 2 faculty anesthesiologists (C.D.T., C.A.C.). On average, there was 1 instructor and 4 participants in each session (range, 1:2 to 1:4).
RESULTS
We have complete precourse and postcourse data from all assessment components for 19 participants and postcourse survey data from all 45 participants who have taken the course thus far. To attend our simulation day, we required the participants to complete the online modules and 50-MCQ pretest, and all the participants were compliant. Fifty-seven percent of the participants failed the pretest cognitive examination by answering less than 70% of the questions correctly. The mean (SD) pretest and posttest cognitive examination scores were 70.4 (8.4) and 88.0 (6.8), respectively. All subjects demonstrated an increase in their cognitive examination performance after simulation training. The mean (SD) difference between pretest and posttest cognitive examination scores was 17.6 (9.3) (P<0.001). For the BEAM component of the course, 100% of the participants failed the simulation pretest. Only 13% (6/45) were able to successfully perform easy mask ventilation. Twenty percent (9/45) were able to successfully perform difficult mask ventilation. Successful LMA placement was only accomplished by 55% (25/45). See Figure 4 for details.
FIGURE 4.
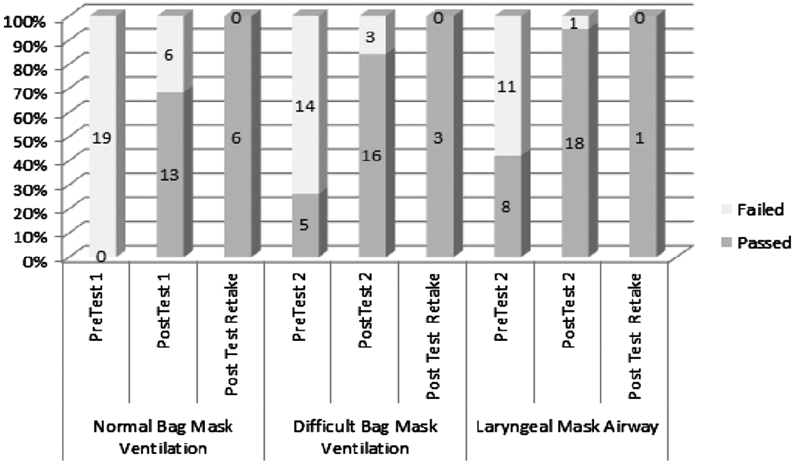
The difference in performance on the BEAM before and after the moderate sedation course. (n = 19 for all data fields; precourse and postcourse normal bag mask ventilation, precourse and postcourse difficult mask ventilation, and precourse and postcourse LMA placement.)
Seventy-nine percent of the participants failed the simulation pretest for moderate sedation. Specifically, the pass rate for the first simulated patient sedation was 50% (10/20). For the second simulated patient sedation, the pass rate was 80% (16/20). For the first simulated reversal, the pass rate was 60% (12/20), and for the second simulated reversal, the pass rate was 70% (14/20). One participant failed the posttest and had immediate remediation and retesting with the instructor, resulting in a passing grade. All other participants passed the posttest on the simulated patients to a level of moderate sedation (Fig. 5). Of participants, 100% passed the MCQ cognitive examination. Overall results for the course can be seen in Figure 6.
FIGURE 5.
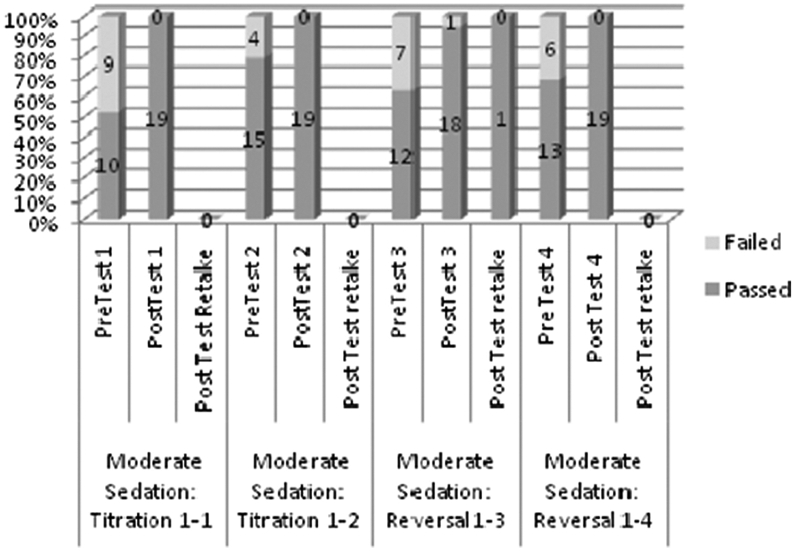
The difference in performance on the moderate sedation simulation scenarios before and after the moderate sedation course. (n = 19 for all data fields; presedation and postsedation titration 1 and 2 and prereversal and postreversal 1 and 2.)
FIGURE 6.
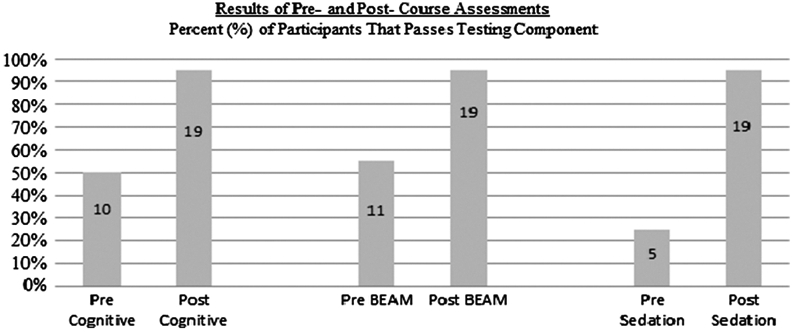
The difference in performance on 3 measures of assessment before and after the moderate sedation course. (n = 19 for all data fields; Precognitive/Postcognitive, precourse and postcourse cognitive test; Pre-BEAM/Post-BEAM, precourse and postcourse basic emergency airway management test; Presedation/Postsedation, precourse and postcourse moderate sedation simulation test).
On the anonymous postcourse survey, participants reported that they believed the simulation course improved their technical skills, clinical knowledge and judgment, and confidence in managing moderate sedation. In addition, the simulation course was rated as “better” (28.9%) or “much better” (71.1%) than a lecture-based course. Almost all (97.8%), either “strongly agreed” or “agreed” that they planned to apply what they learned in knowledge and skills in the simulation-based course/module into their practice. The overall rating for the course by participants was “good” (28.9%) or “exceptional” (68.9%). A full report of survey data is available as Appendix 1.
DISCUSSION
We developed a novel moderate sedation simulation training course that allowed participants to practice delivering moderate sedation to simulated patients that were sensitive, resistant, and normal to the effects of opioid and benzodiazepine sedation. To date nationally, most courses are lecture based or Web-based courses, providing little to no hands-on experience with administering, titrating, or reversing sedative medications. In our course, participants were able to learn how a patient would respond to different medication dosages and combinations of medications in a controlled simulated environment. Within a limited range of choices, the participant chose the medications they would use in their clinical practice or selected new medications in which they may have had limited clinical experience. For example, a gastroenterologist selected meperidine, which he or she used for colonoscopy sedation, whereas a radiologist wanted to simulate the use of midazolam for a magnetic resonance imaging. There was the added advantage of managing sensitive, resistant, and normal patient responses so that participants can develop a frame of reference and further develop their sedation planning and administration skills. This is not possible with didactics alone. In addition, the course allowed for standardization such that it maybe transportable to other institutions.
Completing the online modules, quizzes, and cognitive pretest provided the learners with insight into their baseline knowledge. The online modules not only allowed for easier access to didactic materials and participants completed them at their leisure but also are easily reproducible if the course were to extend outside our institution. We realize 14 hours is a time-consuming course, and we developed such a comprehensive course because we felt it was important for participants to understand all components of moderate sedation, including BEAM. After teaching the course for more than a year, we now have the experience to edit the course and possibly reduce the time without reducing the experience and education. Although nonanesthesiologist physicians have been the participants to date, the simulation and didactic components could easily be used to educate other medical care team members who participate in sedation administration.
Despite the fact that most physicians had experience in moderate sedation, most were unable to pass all components of the pretest. Unfortunately, we did not collect detailed data regarding the participants’ years of training, previous experiences with procedural sedation including complications. This information may be insightful into participant performance during the course; however, we were currently unable to extrapolate poor performance on the pretest to poor clinical performance. We will consider adding this information to our course survey. Regardless, we believe the high failure rates on the pretests shows the need for improved education. After participating in our course, all participants were able to master the knowledge and skill set necessary to obtain a passing score. Survey results demonstrated a high participant satisfaction rating. However, 22% rated the overall simulation course as “poor” Our course was mandatory not only for newly hired physicians but also experienced physicians who use moderate sedation in their practice. It is possible that some of the physicians were frustrated with being required to take a course that they believed they did not need; however, we have taken this review quite seriously and frequently revisit the course for potential improvements. As an indirect measure of clinical effectiveness of this course, our institutional quality assurance program will be prospectively evaluating whether we are experiencing a decrease in the incidence and absolute numbers of adverse moderate sedation events at an institutional level.
A weakness of our report is our lack of a complete data set for all 45 participants. We initially had difficulty with saving the online MCQ pretest and lost that data. In addition, the simulation pretest for moderate sedation titration and reversal was not a component of the course. We realized this was needed to access baseline knowledge of the participants and for future course validation, so the moderate sedation pretest was added after the course was already ongoing. After addition, only 21% managed to pass the pretest sedation simulation. Another possible limitation is that our course was programmed within the SimMan structure. The description of the course, along with the online materials, should allow for the use of this course with other simulators at other institutions. We report only on the construction of the course and overall course assessment data for the participants. We need to further investigate and validate our checklists used for scenario scoring. Lastly, we programmed the simulators to respond to commonly used sedatives and analgesics, but several of the participants had limited experience with these medications, which could have hindered their performance. In the future, we plan to expand the number of medications available for the participants to use during moderate sedation simulation practice and testing. In addition, we programmed the simulator to treat drug administrations in an additive manner. Of note, current simulator programming did not allow for complete nonlinear mixed effects modeling of benzodiazepines and opioids, as has been described in the anesthesiology literature previously.22 This would require varying effects of the medications based on an innumerable number of combinations. However, we believe that our additive scoring of drug administration with specified changes in pharmacodynamics response for each added dose is a significant advance in moderate sedation training as the level of sedation score could be reached through any combination of benzodiazepine and opioid dosings but always in an additive fashion.
CONCLUSIONS
A course using a combination of didactic and SBME to teach moderate sedation to nonanesthesiologist physicians was developed. Through the use of simulation, the participants practiced pertinent airway management skills and se-dation administration on a variety of different patient drug sensitivity scenarios. Signs and symptoms of oversedation with opioids and benzodiazepines were tested and treated in a controlled environment. We believe our course led to an increase in both knowledge and skill. In the future, our long-term goals will include evaluating whether our moderate sedation course can produce T3 level results, as measured by reduced clinical incidence of need for sedation reversal, severe hypoxemia, airway intervention, and cardiopulmonary collapse.
ACKNOWLEDGMENTS
The authors would like to thank John Walker, Jason Flamm, and Erika Jenkins for their assistance in data collection. The authors would also like to thank all of the staff at the MUSC Clinical Effectiveness and Patient Safety Center for their assistance during this project.
Funding Sources: None.
Appendix
APPENDIX 1:
“Participants” Survey Summary
| Simulative Experience | |||||
|---|---|---|---|---|---|
| Question | Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree |
| The objectives of the simulation-based course/module were clearly stated. | 73.3% | 26.7% | |||
| The simulation-based course/module was appropriate for my level of learning. | 57.8% | 37.8% | 2.2% | 2.2% | |
| I plan to apply what I learned (knowledge, skills) in this simulation-based course/module to my practice. | 62.2% | 35.6% | 2.2% | ||
| The Web-based precourse curriculum was helpful. | 44.4% | 42.1% | 8.9% | 4.4% | |
| The Web-based precourse curriculum was easy to use. | 37.8% | 51% | 6.7% | 4.4% | |
| The discussion of my performance during debriefing contributed to my learning. | 53.3% | 44.4% | 2.2% | ||
| Question | Once to enough | 3 mo | 6 mo | 12 mo | 18 mo |
| I would recommend that this simulation-based course/module be offered every | 54.1% | 2.2% | 11.1% | 35.6% | |
| Question | Much better | Better | Worse | ||
| How would you take this simulation-based course/module compared with a lecture on this topic? | 71.1% | 28.9% | |||
| Question | Exceptional | Good | Poor | ||
| Overall simulation-based course/module rating | 66.9% | 28.9% | 22.2% | ||
| Question | Technical skills | Clinical knowledge | Judgment | Confidence | |
| The simulation experience has improved my Facilitator | 36.4% | 40.9% | 2.3% | 20.5% | |
| Question | Strongly agree | Agree | Neutral | Disagree | Strongly disagree |
| The debriefing was completed in a professional and nonpersonal manner. | 55.6% | 24.4% | |||
| The facilitator explained difficult concepts slowly. | 73.3% | 26.7% | |||
| The facilitator demonstrated respect for course participants. | 91.1% | 8.9% | |||
| The facilitator was effective in teaching this simulation-based course/module. | 93.3% | 6.7% | |||
| Facility | |||||
| Question | Strongly agree | Agree | Neutral | Disagree | Strongly disagree |
| My orientation to the simulation environment was adequate. | 60% | 40% | |||
| Question | Strongly agree | Agree | Neutral | Disagree | Strongly disagree |
| The MUSC Healthcare Simulation Staff was supportive. | 77.8% | 22.2% | |||
| Question | Exceptional | Good | Poor | ||
| Overall facility rating | 86.7% | 11.1% | 2.2% | ||
| Question | Yes | No | |||
| The course was free from commercial bias. | 100% | ||||
APPENDIX 2:
| TJC Standards | Elements of Performance |
|---|---|
| PC 13.20 | Sufficient numbers of qualified staff (in addition to the individual performing the procedure) are present to evaluate the patient, help with the procedure, provide the sedation and/or anesthesia, and monitor and recover the patient. Individuals administering moderate or deep sedation and anesthesia are qualified and have the appropriate credentials to manage patients at whatever level of sedation or anesthesia achieved, either intentionally or unintentionally. A registered nurse supervises perioperative nursing care. Appropriate equipment to monitor the patient’s physiological status is available. Appropriate equipment to administer intravenous fluids and drugs, including blood and blood components, is available as needed. Resuscitation capabilities are available. The following must occur before the operative and other procedures or the administration of moderate or deep sedation or anesthesia: °The anticipated needs of the patient are assessed to plan for the appropriate level of postprocedure care. °Preprocedural education, treatments, and services are provided according to the plan for care, treatment, and services. °Conduct a “time out” immediately before starting the procedure as described in the Universal Protocol. °A presedation or preanesthesia assessment is conducted. °A licensed independent practitioner with appropriate clinical privileges plans or concurs with the planned anesthesia. °The patient is reevaluated immediately before moderate or deep sedation and before anesthesia induction. |
| PC 13.30 | Appropriate methods are used to continuously monitor oxygenation, ventilation, and circulation during procedures that may affect the patient’s physiological status The procedure and/or the administration of moderate or deep sedation or anesthesia for each patient is documented in the medical record. |
| PC 13.40 | The patient’s status is assessed immediately after the procedure and/or administration of moderate or deep sedation or anesthesia Each patient’s physiological status, mental status, and pain level are monitored. Monitoring is at a level consistent with the potential effect of the procedure and/or sedation or anesthesia. Patients are discharged from the recovery area and the hospital by a qualified licensed independent practitioner or according to rigorously applied criteria approved by the clinical leaders. Patients who have received sedation or anesthesia in the outpatient setting are discharged in the companyofa responsible, designated adult. |
Footnotes
Conflict of Interest/Financial Disclosure information: Dr. McEvoy is the recipient of a Foundation for Anesthesia Education and Research grant, but it is not associated with this project. Dr. Schaefer has Patent royalties from Laerdal Medical Corp. (SimMan/Baby/3G) and a non-majority ownership of SimTunes (an outlet copyrightable simulation material).
Contributor Information
Catherine D. Tobin, Department of Anesthesia and Perioperative Medicine, Medical University of South Carolina, 167 Ashley Ave, Suite 301, MSC 912, Charleston, SC 29425-9120.
Carlee A. Clark, Departments of Anesthesia and Perioperative Medicine; Department of Medicine, Ashley River Tower Operating Room; Medical University of South Carolina, Charleston, SC..
Matthew D. McEvoy, Departments of Anesthesia and Perioperative Medicine; Patient Safety and Simulation; College of Medicine, and Healthcare Simulation Center, Charleston, SC..
John J. Schaefer, Departments of Anesthesia and Perioperative Medicine; College of Medicine, and Healthcare Simulation Center, Charleston, SC..
Bethany J. Wolf, Division of Biostatistics and Epidemiology, Charleston, SC..
Scott T. Reeves, Departments of Anesthesia and Perioperative Medicine, Charleston, SC..
REFERENCES
- 1.American Society of Anesthesiologists Consensus Guidelines: Quality Management and Departmental Administration. Continuum of Depth of Sedation: Definition of General Anesthesia and Levels of Sedation/Analgesia. ASA House of Delegates October 21, 2009. Available at: http://www.asahq.org/For-Members/Standards-Guidelines-and-Statements.aspx. Accessed May 28, 2012. [Google Scholar]
- 2.Cohen LB, Wecsler JS, Gaetano JN, et al. Endoscopic sedation in the United States: results from a nationwide survey. Am J Gastroenterol 2006;101:967–974. [DOI] [PubMed] [Google Scholar]
- 3.Seeff LC, Richards TB, Shapiro JA, et al. How many endoscopies are performed for colorectal cancer screening? Results from CDC’s survey of endoscopic capacity. Gastroenterology 2004;127:1670–1677. [DOI] [PubMed] [Google Scholar]
- 4.Roger VL, Go AS, Lloyd-Jones DM, et al. Executive Summary: heart disease and stroke statistics—2012 update; a report from the American Heart Association. Circulation 2012;125:e20–e220. [DOI] [PubMed] [Google Scholar]
- 5.Friedman JW. The prophylactic extraction of third molars: a public health hazard. Am J Public Health 2007;97:1554–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arepally A, Oechsle D, Kirkwood S, Savader SJ. Safety of conscious sedation in interventional radiology. Cardiovasc Intervent Radiol 2001;24:185–190. [DOI] [PubMed] [Google Scholar]
- 7.Macrae FA, Tan KG, Williams CB. Towards safer colonoscopy: a report on complications of 5000 diagnostic or therapeutic colonoscopies. Gut 1983;24:376–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cote CJ, Daniel AN, Karl HW, Weinberg JA, McCloskey C. Adverse sedation events in pediatrics: a critical incident analysis of contributing factors. Pediatrics 2000;105;805–814. [DOI] [PubMed] [Google Scholar]
- 9.American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology 2002;96:1004–1017. [DOI] [PubMed] [Google Scholar]
- 10.The Joint Commission. Standards FAQ Website: Permission to Administer Moderate Sedation. Available at: http://www.jointcommission.org/standards_information/jc6faqdetails.aspx?StandardsFAQId=230&StandardsFAQChapterId=78. Accessed May 26, 2012.
- 11.McGaghie WC, Draycott TJ, Dunn WF, Lopez CM, Stefanidis D. Evaluating the impact of simulation on translational patient outcomes. Simul Healthc 2011;6(Suppl 7):S42–S47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park CS. Simulation and quality improvement in anesthesiology. Anesthesiol Clin 2011;29:13–28. [DOI] [PubMed] [Google Scholar]
- 13.Barsuk JH, Ahya SN, Cohen ER, McGaghie WC, Wayne DB. Mastery learning of temporary hemodialysis catheter insertion by nephrology fellows using simulation technology and deliberate practice. Am J Kidney Dis 2009;54:70–76. [DOI] [PubMed] [Google Scholar]
- 14.Evans LV, Dodge KL, Shah TD, et al. Simulation training in central venous catheter insertion: improved performance in clinical practice. Acad Med 2010;85:1462–1469. [DOI] [PubMed] [Google Scholar]
- 15.Khouli H, Jahnes K, Shapiro J, et al. Performance of medical residents in sterile techniques during central vein catheterizations. randomized trial of efficacy of simulation-based training. Chest 2011;139:80–87. [DOI] [PubMed] [Google Scholar]
- 16.Ma IW, Brindle ME, Ronksley PE, Lorenzetti DL, Sauve RS, Ghali WA. Use of simulation-based education improve outcomes of central venous catheterization: a systematic review and meta-analysis. Acad Med 2011;86:1137–1147. [DOI] [PubMed] [Google Scholar]
- 17.Barsuk JH, Cohen ER, Feinglass J, McGaghie WC, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med 2009;169:1420–1423. [DOI] [PubMed] [Google Scholar]
- 18.Wagner B, Meirowitz N, Shah J, et al. Comprehensive perinatal safety initiative to reduce adverse obstetric events. J Healthc Qual 2011;34:6–15. [DOI] [PubMed] [Google Scholar]
- 19.Riley W, Davis S, Miller K, Hansen H, Sainfort F, Sweet R. Didactic and simulation nontechnical skills team training to improve perinatal patient outcomes in a community hospital. Jt Comm J Qual Patient Saf 2011;37:357–364. [DOI] [PubMed] [Google Scholar]
- 20.Phipps MG, Lindquist DG, McConaughey E, O’Brien JA, Raker CA, Paglia MJ. Outcomes from a labor and delivery team training program with simulation component. Am J Obstet Gynecol 2012;206:3–9. [DOI] [PubMed] [Google Scholar]
- 21.Pastis NJ, Doelken P, Vanderbilt AA, Walker J, Schaefer JJ III. Validation of simulated difficult bag-mask ventilation as a training and evaluation method for the first-year internal medicine house staff. Simul Healthc 2012; Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 22.Barr J, Zomorodi K, Bertaccini EJ, Shafer SL, Geller E. A double-blind, randomized comparison of i.v. lorazepam versus midazolam for sedation of ICU patients via a pharmacologic model. Anesthesiology 2001;95:286–298. [DOI] [PubMed] [Google Scholar]