Abstract
Background and aims
COVID-19 disease has been associated with disproportionate mortality amongst world population. We try to elucidate various reasons for lower mortality rate in the Indian subcontinent due to COVID-19 pandemic.
Method
We carried out a comprehensive review of the literature using suitable keywords such as ‘COVID-19’, ‘Pandemics’, ‘disease outbreaks’ and ‘India’ on the search engines of PubMed, SCOPUS, Google Scholar and Research Gate in the month of May 2020 during the current COVID-19 pandemic and assessed mortality data.
Results
The mortality observed in Indian and south Asian subcontinent is lower than in the west.
Multifactorial reasons indicated for this differential mortality due to COVID-19 have been described in the current literature.
Conclusions
The effects of COVID-19 on the health of racial and ethnic minority groups are still emerging with disproportionate burden of illness and death amongst some black and ethnic minority groups. Overall the current COVID-19 related mortality appears to be lower in the health and resource challenged populous Indian subcontinent. Further scientific studies would be helpful to understand this disparity in mortality due to COVID-19 in the world population.
Keywords: COVID-19, Coronavirus, Pandemics, Public health, Disease outbreaks, India
1. Background
Pneumonia from a new novel Coronavirus SARS-CoV-2 virus was detected in Wuhan, China in December 2019 and spread worldwide. The outbreak was declared a Public Health Emergency of International Concern by World Health Organization (WHO) on January 30, 2020 and announced a name for the new coronavirus disease: COVID-19. Since the reporting of the first case, COVID-19 has so far affected 232 countries and has infected over 6 million people globally [1]. In India, COVID-19 has currently more than 456251 total cases out of which 183384 are active cases and has claimed 14483 lives so far. This figure keeps changing every day. Though the number of cases of COVID 19 is increasing day by day due to relief in lockdown measures and migration of people, it is intriguing to note that so far the mortality has remained at a lower level in the Indian subcontinent than in other countries with similar numbers of COVID-19 infections (Table 1 ) (Fig. 1, Fig. 2, Fig. 3 ). Even with poor infrastructure and health facilities found in India, compared to other countries with more robust health facilities such as in Italy, Spain, United Kingdom and United States of America; the mortality data in India is a fraction to that seen in Western countries. India’s recovery rate from COVID-19 is higher than those of many nations at the same level of infection and can be due to high suspicion of diagnosis, timely detection, and treatment. The possible reasons behind lower mortality figures in India is ambiguous, with many theories described for this. We try to elucidate various reasons for lower mortality rate in the Indian subcontinent due to COVID-19.
Table 1.
Infection and Death rates in the worst-hit ten countries by COVID-19 (Source: Worldometer) https://www.worldometers.info/(Accessed June 24, 2020) [32].
| Rank | Country | Population | No. of reported cases | COVID-19 Infection rate (in percent) | No. of deaths | Death rate, according to infected population (in percent) | Death rate, according to overall population (per million) | P-Value |
|---|---|---|---|---|---|---|---|---|
| 1 | USA | 330,965,224 | 2,424,418 | 0.7 | 123,477 | 5.09 | 373.08 | <0.001 |
| 2 | Brazil | 212,529,324 | 1151479 | 0.5 | 52,771 | 4.58 | 248.29 | |
| 3 | Russia | 145,933,426 | 599,705 | 0.4 | 8359 | 1.39 | 57.28 | |
| 4 | India∗ | 1,379,715,223 | 456251 | 0.03 | 14,483 | 3.17 | 10.50 | |
| 5 | UK | 67,879,245 | 306,210 | 0.45 | 42,927 | 14.01 | 632.40 | |
| 6 | Spain | 46,754,479 | 293,832 | 0.62 | 28,325 | 9.6 | 605.82 | |
| 7 | Peru | 32,961,088 | 260,810 | 0.79 | 8404 | 3.2 | 254.96 | |
| 8 | Chile | 19,112,809 | 250,767 | 1.31 | 4505 | 1.79 | 235.70 | |
| 9 | Italy | 60,463,214 | 238,833 | 0.39 | 34,675 | 14.51 | 573.48 | |
| 10 | Iran | 83,968,383 | 209,970 | 0.25 | 9863 | 4.6 | 117.46 |
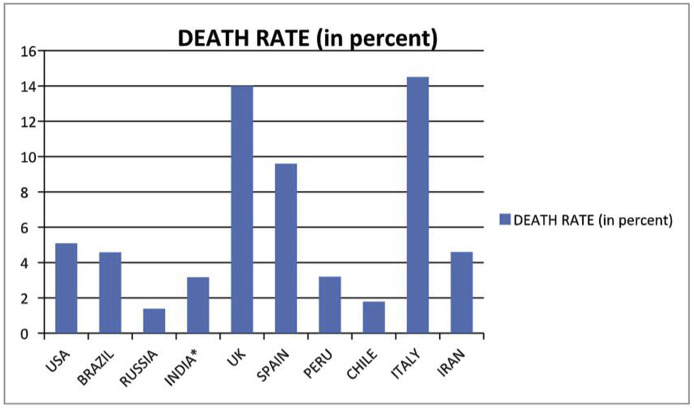
Fig. 1.
Death rate Chart in percentage population due to COVID-19.
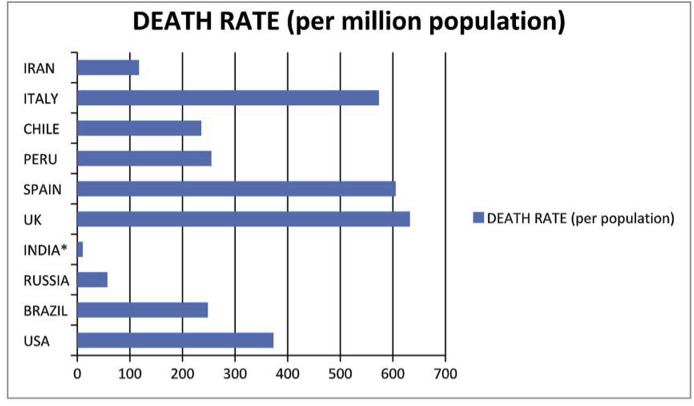
Fig. 2.
Death chart rate per million due to COVID-19.
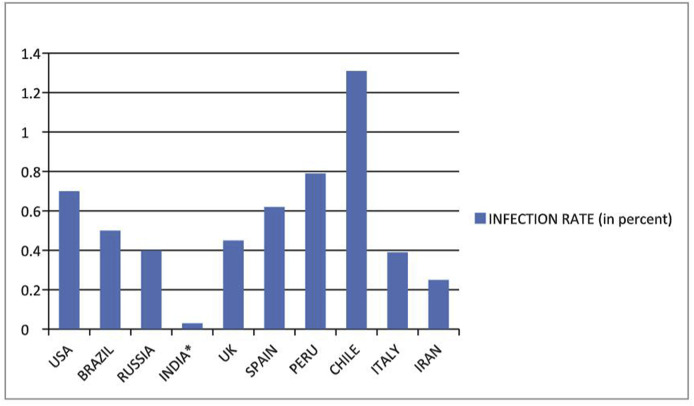
Fig. 3.
Infection rate chart in percentage due to COVID-19.
2. Rationales for low mortality in India
We have investigated and identified the possible reasons and hypotheses for this disparity in mortality on several parameters as below and shall discuss them in some details.
2.1. Age
It is acknowledged that the elderly population makes up a high proportion of the COVID-19 mortality across all countries [2,3]. The Western natives are significantly older than their Asian and African counterparts. India is a young nation. According to a report by the Ministry of Statistics and Programme implementation the share of its youth is expected to be 34.33% of the total population of India by 2020 [4]. Availability of universal health care and the social culture of family ties and protection of the elderly in India support high self-rated health amongst elders [5].
2.2. Genetics
Certain immune variations such as genetic or acquired differences might separate people who fall severely ill and develop pneumonia with COVID-19 from those who contract the infection but hardly develop any discernible symptom [6]. Such differences in fatality rates could be linked to genetic variations in SARS-CoV-2, but the current literature pertaining to this is lacking. Individual genetic variation may help to explain different immune responses to a virus across a population. In particular, understanding how variation in HLA may affect the course of COVID-19 could help identify individuals at higher risk from the disease [7].
Studies have found that higher mortality rate in Western countries is due to genetics. The Cell entry of coronaviruses depends on binding of the viral spike (S) proteins to cellular receptors (SARS-CoV-2 receptor ACE2)and on S protein priming by host cell proteases (serine protease TMPRSS2). The mechanisms of SARS-CoV-2 infection have been explained by a recent study that the angiotensin-converting enzyme 2 (ACE2) responsible for the cleavage of Angiotensin I and Angiotensin II as the host cell surface receptor allowing for the viral infection COVID-19. SARS-CoV-2 infection causes decrease of ACE2 expression leading to severity of the lung damage [8]. The presence of D allele of ACE1 genes is associated with a reduced expression of ACE2 genes, which results in fewer ACE2 receptors thus lower chance of infection but increasing the severity of lung damage. This D/I polymorphism shows an important geographical variation. Low D allele frequencies have been reported in Asians as compared to the European population and could be the cause of more severe pulmonary infection due to COVID-19 and deaths [9].
The HLA gene variant has been tied to high rates of severe symptoms of Severe Adult Respiratory Syndrome (SARS), a coronavirus related to COVID-19. The occurrence and development of SARS-CoV-2 depend on the interaction between the virus and the individual’s immune system [10]. The genes responsible for proteins that prevent the immune system from attacking the body itself come in several variants. It has been shown that people with some variants are more susceptible to the corona virus than those with the others and that these variants may be specific by region [11].
An Indo-US team of researchers has found that Indians, compared to other world populations, carry more natural killer cells that can detect and terminate infections at an early stage [12].
2.3. Mutation of the SARS-CoV-2
Mutations are a part of the natural life cycle of any virus. The Indian Council of Medical Research (ICMR), the apex health research body of India, is planning to study the genetic diversity of the virus to study the evolution of SARS-CoV-2 and to evaluate, if the present strain has evolved or is the same as the initial strain. It has been believed that higher mortalities seen in some of Indian regions may be due to a mutant, more virulent strain of the SARS-CoV-2 virus [13]. Many mutations observed in the SARS-CoV-2 sequences are therefore expected. The current estimates for the mutation rate of SARS-CoV-2 are about one mutation in two weeks. Currently there are at least 11 different strains of SARS-CoV-2 (the causative agent of COVID-19) in the world.
Researchers at Cambridge University found that the virus may have mutated as it spreads from Asia to Europe becoming more resilient to conditions in Europe and thus, deadlier however, not enough data is available on different strains [14]. The study identifies three strains of virus A, B and C; Type A is prevalent in US and Australia, Type B Wuhan’s major virus type, ‘B’, is prevalent in patients from across East Asia, C′ variant, is the major European type, found in early patients from France, Italy, Sweden and England [14].
Recently, scientists identified several hundreds of point mutations in SARS-CoV-2 across the genome. They elucidate the link between the constant change and variable virulence with an increase in mortality and morbidity. They noted 47 key point mutations located along the entire genome that might have impacted in the virulence and response to different antivirals against SARS-CoV-2 [15].
Furthermore, Eaaswarkhanth et al. have reported that S-D614 G strains may be virulent and lead to increasing its severity in the infected individuals especially in Europe, where this mutation is prominent. It is also plausible that the SARS-CoV-2 mutations giving rise to different phylogenetic clades are responsible for the obvious death disparities around the world [16].
2.4. Climate
There are some suggestions that temperature variation and humidity may also be important factors affecting the COVID-19 mortality [17,18]. Coronavirus spread is slow in hot and humid weather and spreads easily in dry and cold conditions [19]. Warmer Asian countries saw the infection spread more slowly than Europe and the US. With the start of summer in India and with temperatures more than 35–40° centigrade, the infection rate has not been coming down, indicating that this may not be such a relevant factor.
2.5. Lockdown effect
High infection and death rate due to COVID 19 can also be due to stringency of lockdown. USA, Sweden, Iran, and Turkey did not implement strict curbs and have high rates of mortality. India’s 21 days of complete national wide lockdown was one of the most stringent in the world for keeping the number of cases down [20]. The current low levels of mortality are surely a pointer of what happened before the lockdown began. It is also possible that COVID-19 has had a substantial mortality impact, but that the total deaths have not risen because the complete lockdown reduced non-COVID deaths. Recent unlocking of restrictions in India has seen a rise in the numbers of reported infections and mortality [21].
2.6. BCG vaccination is a potential new tool in the fight against COVID-19
Lack of BCG vaccination has been claimed to be a possible explanation for the high heterogeneity of infection/mortality rates across involved countries. The widespread use of BCG vaccination for prevention of tuberculosis (TB) in India may be the reason for lower rates of COVID-19. The BCG vaccine is an Approved Vaccine Product by the FDA for people who have not been previously infected with Mycobacterium Tuberculosis and who are at a high risk of being infected with this bacillus. It appears that in countries with routine BCG vaccination, the pandemic appears to be less severe as this vaccine is a general immune-system enhancer. The BCG vaccination has been given to Indian children since 1948. Countries without universal policies of BCG vaccination (Italy, Netherland,USA) have been more severely affected compared to countries with universal and long-standing BCG policies. Countries that have a late start of universal BCG policy (Iran, 1984) have had high mortality in elderly population. Hence this explanation demands more in-depth research and explanation [22]. BCG vaccine is currently being trialed to reduce the frequency and severity of COVID-19 [23]. It is hoped that the vaccine will increase the trained immunity, so that the immune system is boosted against coronavirus SARS-COV-2.
2.7. Inherent immunity
Indians suffer repeated attacks of respiratory viruses that keep their immune system primed; destroying pathogens, attempting to attack, could be one important factor (this has probably also provided prevention from SARS and MERS-CoV). Nutritional factors, tough life, unhygienic conditions, poor community hygiene etc. may also be responsible for repeated respiratory infections [24].
2.8. Obesity
Obesity rates are higher in the US and the western world than in India. The prevalence of obesity in the USA around 40%, versus a prevalence of 6·2% in China, 20% in Italy, and 24% in Spain [25] A recent study has demonstrated that hospitalized patients younger than 50 with morbid obesity (BMI ≥40 kg/m2) are more likely to die from COVID-19 [26]. Patients with obesity are associated with impaired immune response, endothelial dysfunction, decreased functional residual capacity in the lungs and hypoxemia and expression of ACE2 in adipose tissue which has high affinity to the SARCOV2 virus [27,28].
2.9. Race and ethnicity
The effects of COVID-19 on the health of racial and ethnic minority groups are still emerging; however, current data suggest a disproportionate burden of illness and death in this cohort [29]. Factors that influence racial and ethnic minority group health, include economic and social conditions. These groups also find it difficult to access resources during outbreaks such as COVID-19. Racial residential segregation and living in densely populated areas does not allow principles of social distancing and underlying health conditions [30]. As such, scientific studies that result in improved understanding of COVID-19 may lead to more targeted and effective community and health care system–based interventions in the future. Hence, analyzing the disproportionate affliction of the black and ethnic minority group will be essential [31].
2.10. Late presentation of COVID-19 in India
The COVID-19 pandemic struck India in early March i.e. later than in other countries and hence there is a substantial delay in the reported infections and fatality in India. The spread to all countries from China was almost simultaneous. India’s response was initiated on 8th January, much before WHO declared COVID-19 as a public health emergency. The screening of travelers from abroad at airports and at ports was started exceedingly early in Jan 2020. All incoming travellers, including Indian nationals, arriving from, or having visited China, Italy, Iran, Republic of Korea, France, Spain, and Germany after February 15, 2020 were quarantined for a minimum period of 14 days [33]. However, in many other countries (the USA, UK, and EU countries) did not resort to any such measures.
2.11. Use of hydroxychloroquine
Anti-malarial drug hydroxychloroquine was suggested to reduce the COVID-19 risk in health workers with potential for retinal and cardiac toxicity. This drug has diverse modes of action, including inhibition of cytokine storms in the host cell which work against the viral infections and help prevent deaths [34]. The recent study found that COVID-19 infections are higher in countries where malaria islessendemic and lower in countries where malaria is highly endemic. Large numbers of mortality in health care professionals across the globe have been observed during pandemic [35]. In India; Indian Council of Medical Research (ICMR) recommended the use of hydroxychloroquine in asymptomatic health professionals who cared for suspected or confirmed COVID-19 cases early in the rise of the pandemic; this may have prevented more fatalities in the western countries [36,37]. However, there is no hard evidence that hydroxychloroquine reduces the risk of COVID-19 so far. A recent article in the Lancet journal about hydroxychloroquine role and use has been retracted [38].
3. Conclusion
The COVID-19 pandemic has devastated the global population by hitting the health individuals. It is a highly contagious disease and has caused a high rate of mortality particularly in high risk individuals. The pattern of infection and mortality rates has varied significantly amongst the countries. Surprisingly, more affluent countries with greater healthcare resources have been more affected by it and have seen higher mortality rates, compared to less affluent countries like India and other Southeast Asian nations. We have analyzed and discussed several factors that may be responsible for such discrepancy.
Funding
No funding received.
Declaration of competing interest
None.
References
- 1.World Health Organisation COVID-19 Situation report. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200531-covid-19-sitrep-132.pdf
- 2.Li H., Wang S., Zhong F. Age-dependent risks of incidence and mortality of COVID-19 in hubei province and other parts of China. Front Med. 2020;7:190. doi: 10.3389/fmed.2020.00190. Published 2020 Apr 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Docherty A.B., Harrison E.M., Green C.A. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. Published 2020 May 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ministry of Statistics and Programme Implementation 2017. http://mospi.nic.in/sites/default/files/publication_reports/Youth_in_India-2017.pdf
- 5.Sudha S., Suchindran C., Mutran E.J., Rajan S.I., Sarma P.S. Marital status, family ties, and self-rated health among elders in South India. J Cross Cult Gerontol. 2006;21(3–4):103–120. doi: 10.1007/s10823-006-9027-x. [DOI] [PubMed] [Google Scholar]
- 6.Lanese N. Could genetics explain why some COVID-19 patients worse than others. https://www.livescience.com/genetics-could-explain-extreme-covid19-coronavirus-infections.html
- 7.Nguyen A., David J.K., Maden S.K. Human leukocyte antigen susceptibility map for SARS-CoV-2 [published online ahead of print, 2020 Apr 17] J Virol. 2020 doi: 10.1128/JVI.00510-20. JVI.00510-20. [DOI] [Google Scholar]
- 8.Hoffmann M., Kleine-Weber H., Schroeder S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181(2) doi: 10.1016/j.cell.2020.02.052. 271-280.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delanghe J.R., Speeckaert M.M., De Buyzere M.L. The host’s angiotensin-converting enzyme polymorphism may explain epidemiological findings in COVID-19 infections. Clin Chim Acta. 2020;505:192–193. doi: 10.1016/j.cca.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li X., Geng M., Peng Y., Meng L., Lu S. Molecular immune pathogenesis, and diagnosis of COVID-19. J Pharm Anal. 2020;10(2):102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohanty Kenneth, Das Anjishnu. Why some Western countries have a higher death rate compared. http://timesofindia.indiatimes.com/articleshow/76115513.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst_prime
- 12.Du Z., Sharma S.K., Spellman S., Reed E.F., Rajalingam R. KIR2DL5 alleles mark certain combination of activating KIR genes. Gene Immun. 2008;9(5):470–480. doi: 10.1038/gene.2008.39. [DOI] [PubMed] [Google Scholar]
- 13.Chandna H., Chakrabarti A. Has COVID-19 strain evolved since it was first reported in India? ICMR study to find answer. https://theprint.in/health/has-covid-19-strain-evolved-since-it-was-first-reported-in-india-icmr-study-to-find-answer/412445/ Online 01May 2020.
- 14.Forster P., Forster L., Renfrew C., Forster M. Phylogenetic network analysis of SARS-CoV-2 genomes. Proc Natl Acad Sci U S A. 2020;117(17):9241–9243. doi: 10.1073/pnas.2004999117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vankadari N. Overwhelming mutations or SNPs of SARS-CoV-2: a point of caution [published online ahead of print, 2020 May 20] Gene. 2020;752:144792. doi: 10.1016/j.gene.2020.144792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eaaswarkhanth M., Madhoun A.A., Al-Mulla F. Could the D614 G substitution in the SARS-CoV-2 spike (S) protein be associated with higher COVID-19 mortality? [Published online ahead of print, 2020 May 25] Int J Infect Dis. 2020;S1201–9712(20) doi: 10.1016/j.ijid.2020.05.071. 30378-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma Y., Zhao Y., Liu J. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oliveiros Barbara, Caramelo Liliana, Ferreira Nuno C., Caramelo Francisco. Role of temperature and humidity in the modulation of the doubling time of COVID-19 cases. https://www.medrxiv.org/content/medrxiv/early/2020/03/08/2020.03.05.20031872.full.pdf
- 19.Madaan N. 85% correlation between temperature rise & cut in virus spread. https://timesofindia.indiatimes.com/india/85-correlation-between-temperature-rise-cut-in-virus-spread-study/articleshow/75439996.cms
- 20.Chandrashekhar V. 1.3 billion people. A 21-day lockdown. Can India curb the coronavirus? https://www.sciencemag.org/news/2020/03/13-billion-people-21-day-lockdown-can-india-curb-coronavirus Online 31 March 2020.
- 21.https://www.hindustantimes.com/india-news/as-unlock-1-0-begins-here-s-a-look-at-top-states-battling-the-coronavirus-menace-covid-19-tally/story-y3xUuFjYSsPOxokw47177M.html.As unlock 1.0 begins, here’s a look at top states battling the coronavirus menace: Covid-19 tally (Accessed 03June 2020)
- 22.Dayal D., Gupta S. Connecting BCG vaccination and COVID-19: additional data medRxiv 2020.04.07.20053272. 2020. [DOI]
- 23.Clinical Trials Arena Australian researchers to trial BCG vaccine for Covid-19. https://www.clinicaltrialsarena.com/news/australia-bcg-vaccine-trial-covid-19/
- 24.Varshney Vibha. Do Indians have higher immunity to novel coronavirus? https://www.downtoearth.org.in/news/health/covid-19-do-indians-have-higher-immunity-to-novel-coronavirus-70322.COVID-19
- 25.World Health Organization Global Health Observatory (GHO) data: overweight and obesity. 2017. https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adults/en
- 26.Klang E., Kassim G., Soffer S., Freeman R., Levin M.A., Reich D.L. 2020. Morbid obesity as an independent risk factor for COVID-19 mortality in hospitalized patients younger than 50. [published online ahead of print, 2020 May 23]. Obesity (Silver Spring) 10.1002/oby.22913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tibiriçá E., De Lorenzo A. Obesity (Silver Spring); 2020. Increased severity of COVID-19 in people with obesity: are we overlooking plausible biological mechanisms? [Published online ahead of print, 2020 May 13] 10.1002/oby.22887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parameswaran K., Todd D.C., Soth M. Altered respiratory physiology in obesity. Can Respir J J Can Thorac Soc. 2006;13:203–210. doi: 10.1155/2006/834786. Kassir R. Risk of COVID-19 for patients with obesity. Obesity Reviews 2020.Ryan PM, Caplice NM. Is Adipose Tissue a Reservoir for Viral Spread, Immune Activation andCytokine Amplification in COVID-19?Obesity 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kirby T. Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities Lancet. Respir Med. 2020 doi: 10.1016/S2213-2600(20)30228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention (CDC) COVID-19 in racial and ethnic minority groups. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
- 31.Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. 2020. COVID-19 and racial/ethnic disparities. JAMA. Published online May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Worldometer- real time world statistics Coronavirus cases. https://www.worldometers.info/
- 33.Ministry of Family and Welfare https://pib.gov.in/PressReleasePage.aspx?PRID=1606079 Government of India. Public Information Bureau.
- 34.Tripathy S., Dassarma B., Roy S., Chabalala H., Matsabisa M.G. A review on possible modes of actions of Chloroquine/Hydroxychloroquine: repurposing against SAR-COV-2 (COVID 19) pandemic [published online ahead of print, 2020 May 22] Int J Antimicrob Agents. 2020:106028. doi: 10.1016/j.ijantimicag.2020.106028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meo S.A., Klonoff D.C., Akram J. Efficacy of chloroquine and hydroxychloroquine in the treatment of COVID-19. Eur Rev Med Pharmacol Sci. 2020;24(8):4539–4547. doi: 10.26355/eurrev_202004_21038. [DOI] [PubMed] [Google Scholar]
- 36.Lapolla P., Mingoli A., Lee R. Deaths from COVID-19 in healthcare workers in Italy-What can we learn? [published online ahead of print, 2020 May 15] Infect Control Hosp Epidemiol. 2020;1-2 doi: 10.1017/ice.2020.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.https://www.icmr.gov.in/pdf/covid/techdoc/V5_Revised_advisory_on_the_use_of_HCQ_SARS_CoV2_infection.pdf
- 38.Mehra M.R., Desai S.S., Ruschitzka F., Patel A.N. RETRACTED: hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet. 2020;S0140–6736(20):31180–31186. doi: 10.1016/S0140-6736(20)31180-6. [published online ahead of print, 2020 May 22] [retracted in: Lancet. 2020 Jun 5; null] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]