Highlights
-
•
The mental health status of individuals with mood disorder during COVID-19 is unclear.
-
•
Our data indicates that psychological distress in these individuals is heightened.
-
•
The distress is linked to adverse lifestyle changes occurring in response to COVID-19.
-
•
Current concerns relate to loved one's health, and access to appropriate medical care.
Keywords: Bipolar disorder, Major depressive disorder, Exercise, sleep, Alcohol use, Coronavirus
Abstract
Background
Physical-distancing strategies during the coronavirus (COVID-19) pandemic may be particularly detrimental to the mental health of individuals with a pre-existing mood disorder. Data on the mental health status of these individuals during the current pandemic is sparse, and their current mental health needs unclear.
Method
We characterised COVID-19 related lifestyle changes, primary concerns and psychological distress in n=1292 respondents self-reporting a mood disorder (either bipolar disorder or depressive disorder) and n=3167 respondents without any reported mental disorder from the COLLATE (COvid-19 and you: mentaL heaLth in AusTralia now survEy) project; an Australian national survey launched on April 1st 2020.
Results
Psychological distress was heightened in the mood disorder group compared to the group with no mental disorder, with stress and depression further elevated in respondents with bipolar disorder compared to those with depressive disorder; and men with bipolar disorder having even higher levels of depression than women with bipolar disorder. Respondents with bipolar disorder were particularly concerned about financial issues associated with COVID-19 compared to those with depressive disorder and those with no mental disorder. Adverse changes to lifestyle behaviours were more prevalent in respondents with a mood disorder and linked to higher levels of distress.
Limitations
Mood disorder was self-reported and was not clinically verified.
Conclusions
Current psychological distress levels are elevated in individuals with mood disorder and are associated with maladaptive situational and lifestyle changes occurring in response to COVID-19.
1. Introduction
As a result of the coronavirus (COVID-19) pandemic, governments around the world have instituted physical distancing measures to contain transmission and limit the potential for healthcare system saturation that could result in unnecessary deaths. From a population health perspective, physical distancing is critically important, although the direct and indirect impact (i.e. through economic downturn) it may have on mental health is of significant concern (Tan et al., In press). COVID-19 containment measures, including the physical-isolation strategies implemented by the Australian Government in late March 2020 (Vic Gov, 2020), may be especially aversive for individuals with pre-existing mood disorders. This is because they disrupt a myriad of factors critical to the management of clinical and cognitive symptoms, including easy access to in-person psychiatric care, and stability in daily routines, social rhythms and sleep patterns (Balanzá–Martínez et al., 2020; Bowen et al., 2013; Harvey et al., 2009; Van Rheenen et al., 2019). In those with a mood disorder, the occurrence of such disruptions in the context of economic volatility and financial insecurity, is likely to perpetuate the natural negative emotional responses (i.e. depression, anxiety and stress) that occur in the face of disaster (North and Pfefferbaum, 2013; Stein et al., 2004).
Further, in mood disorders there is a heightened prevalence of co-occurring medical conditions such as obesity, diabetes and cardiovascular disease (Coello et al., 2019; Dalack and Roose, 1990; Goldstein et al., 2020; Mansur et al., 2019). These have been linked to a more severe coronavirus 2 (SARS-CoV-2) manifestation (Zaman et al., 2020), and may amplify psychological distress by increasing a patient's worries about the heightened personal risk of infection-related mortality or poor long-term health outcomes (Goldstein, 2017; Mansur et al., 2015; Zaman et al., 2020). Compounding this, may be worries about adverse psychiatric and COVID-19 drug treatment interactions should one become infected, or by the potentially negative implications for oneself should one's carer(s) become infected (Sato et al., 2020).
Disaster research indicates that up to 40% of distressed individuals presenting for mental health assistance during or post disaster have pre-existing psychiatric disorders (North and Pfefferbaum, 2013). To date, several studies have characterised the mental health status of the general population in relation to COVID-19 in different countries, but work comparing community-living individuals with a pre-existing mood disorder to those with no mental disorder is lacking. To elucidate the current mental health needs of those with a mood disorder, observational studies that identify specific COVID-19 related concerns and characterise related lifestyle changes and psychological distress in this population are needed. This will inform evidence-based strategies for patient care in the clinic, and help to mitigate long-term symptom exacerbation and adverse psychological outcomes in these individuals.
In this paper, we address this need by reporting outcomes from the COvid-19 and you: mentaL heaLth in AusTralia now survEy (COLLATE), a nationwide study aimed at understanding the impact of the COVID-19 pandemic on the mental health and wellbeing of Australians. Using cross-sectional data from wave 1 of the project, we compared respondents self-reporting a pre-existing mood disorder and those with no reported mental disorder in terms of their; i) primary concerns related to COVID-19, ii) COVID-19 related changes in personal situation, perceptions or behaviours, and iii) current psychological distress levels. In secondary analyses we compared individuals with depressive disorder and bipolar disorder on these factors. We hypothesised that psychological distress levels would be elevated in the mood disorder groups, and that distress levels would be associated with an increased presence of negative behavioural change in areas relevant to maintaining stable mood, including sleep, exercise and alcohol use.
2. Method
This study received ethics approval from the Swinburne University Human Research Ethics Committee (approval number: 20202917-4107) and complied with the Declaration of Helsinki.
2.1. Design
The COLLATE project is a population-based study that includes a series of anonymous online surveys, open for 72 hours at the beginning of each month for 12 months. This is followed by annual surveys until 2024, which will allow for future longitudinal data collection and characterisation (Phillipou et al., 2020; Tan et al., In press). The cross-sectional findings from wave 1 of the COLLATE project are reported here. Members of the general public residing in Australia, aged 18 years or older were invited to complete the survey over a time period extending from April 1’st to April 4’th 2020. This coincided with federal and state mandated restrictions (Stage 3) coming into effect, whereby Australians were expected to self-isolate as much as reasonably possible (COVID-19 National Incident Room Surveillance Team, 2020; Vic Gov, 2020). This self-isolation meant Australians were only allowed to leave their homes for essential activities, such as employment, exercise, medical care, or to buy groceries.
Respondents were recruited through social media and other advertisements, participant registries and non-discriminative snowball sampling. Respondents completed the survey which covered three broad topics: a) current concerns, b) current emotional experiences, and c) socio-demographics/risk factors. Within this, they were asked to respond to one question asking them to self-identify whether they had a mental illness, and if so, which mental illness/es they had. Measures relevant to the aims of this paper are described below.
2.2. Measures
Primary concerns related to COVID-19: Respondents were asked to identify and rank their top 10 concerns relating to the COVID-19 pandemic from 23 options (see Table 1 ).
Table 1.
Items relating to current concerns about the COVID-19 pandemic ranked by frequency of endorsement for each group
| Items | No mental disorder | Mood disorder | Depressive disorder | Bipolar disorder |
| Implications for health and wellbeing of family/loved ones | 1 | 1 | 1 | 2 |
| Loved one dying from COVID-19 | 2 | 2 | 2 | 3 |
| Loved one catching COVID-19 | 3 | 3 | 3 | 4 |
| Implications for health and wellbeing of society | 4 | 4 | 4 | 5 |
| Australian economy | 5 | 10 | 10 | 13 |
| Catching COVID-19 myself | 6 | 8 | 8 | 11 |
| Implications for health and wellbeing of self | 7 | 5 | 5 | 1 |
| Social isolation and social distancing | 8 | 6 | 6 | 8 |
| Availability of food and medicines | 9 | 7 | 7 | 6 |
| Dying of COVID-19 myself | 10 | 12 | 12 | 12 |
| Access to appropriate medical care | 11 | 9 | 9 | 9 |
| World economy | 12 | 14 | 14 | 15 |
| Personal finances | 13 | 11 | 11 | 10 |
| Risk of unemployment or reduced employment | 14 | 13 | 13 | 7 |
| Travel restrictions | 15 | 17 | 17 | 16 |
| The rapidly changing landscape | 16 | 15 | 15 | 14 |
| Balancing work & caring for children/dependents | 17 | 21 | 21 | 18 |
| Government communication of key messages | 18 | 16 | 16 | 20 |
| Media coverage of the pandemic | 19 | 18 | 18 | 17 |
| Adapting to working from home (e.g. IT/connectivity issues) | 20 | 20 | 20 | 19 |
| Domestic violence | 21 | 19 | 19 | 21 |
| Others | 22 | 22 | 22 | 22 |
| Not being able to attend regular place of worship | 23 | 23 | 23 | 23 |
Note: Bolded values represent the top 10 most frequently endorsed items for each respective group. For the group not reporting any mental disorder, values reflect item ordering by frequency of endorsement from most (1) to least (23). In other groups, values also reflect frequency of endorsement from most (1) to least (23), but deviations from sequential ordering reflect deviations in endorsement frequencies from the group not reporting any mental disorder.
COVID-19 related changes in personal situation, perceptions or behaviours were measured through self-reported changes (in the previous week) in employment status, work arrangements and perceived difficulty working from home, as well as non-employment related contact with others outside the home. Lifestyle factors including exercise, sleep and drinking compared to the period before the COVID-19 pandemic began were also measured, as well as ratings of the perceived impact of government restrictions on mental health and expectations about time to return to ‘normal’ (see Supplementary Table 1 for details).
Psychological distress was measured with the 21-item Depression Anxiety Stress Scale (DASS-21; Lovibond and Lovibond, 1995). The DASS-21 yields three subscales, each comprising seven items scored on a four-point scale from never (0) to almost always (3). Higher subscale scores reflect higher levels of depression, anxiety, and stress in the past week, with a higher sum score representing greater general distress. DASS-21 raw scores were doubled for comparability to full-length (42 items) DASS scores.
Confounding variables of interest included age, gender and momentary affect, as measured by the Positive and Negative Affect Schedule (PANAS; Watson et al., 1988). The PANAS is a 20-item measure comprising a 10-item scale measuring indicators of positive affect (PA) and a 10-item scale measuring indicators of negative affect (NA). It is scored on the extent to which one has a particular feeling at that moment, with ratings on a 5-point scale ranging from very slightly or not at all (1) to extremely (5). A high score on the Positive Affect scale reflects an energetic and alert mood state, whereas a high score on the Negative Affect scale indicates greater levels of general distress. Items include “distressed” (NA scale) and “excited” (PA scale).
2.3. Statistical analyses
Respondents who self-identified as having a mood disorder (either a bipolar or depressive disorder)2 were compared to individuals that did not self-identify as having a mental disorder using the Statistical Package for the Social Sciences (SPSS) v24.0.
First (1), chi-square or one-way analysis of variance was used to ascertain the presence of group differences in age, gender and momentary affect. Pearson or Spearman correlations were then conducted to examine associations between these variables and psychological distress. Second (2), the frequency of endorsements for each of the 23 items of concern was obtained for each group. For each respondent, rankings of zero were assigned to options not endorsed, and then mean rankings (scale 1-10) per group were computed for the 10 most commonly selected options for each group. Third (3), chi-square and column proportions tests were used to compare categorical responses within the nominal variables assessing COVID-19 related changes in personal situation, perceptions or behaviours across groups. Fourth (4), DASS total and subscale scores were square root (SQRT) transformed to account for positive skew in the sample, and then entered as dependent variables in a multivariate analysis of covariance. Given significant, albeit mild, correlations (r's =.1-.2, p's<.001) between confounding variables ascertained at the first step, group was entered as a fixed factor alongside gender, while age and both PANAS subscale scores were entered as covariates. The estimated marginal means of the square root transformed DASS scores were back-transformed to determine their place among the four defined DASS severity levels (normal, mild, moderate, severe/extremely severe) and to compare the scores of respondents with no mental disorder to norms from a non-clinical Australian sample3 . Finally (5), to assess whether DASS total scores differed by the levels of the variables assessing COVID-19 related changes in personal situation, perceptions or behaviours, univariate analyses of covariance were conducted, with each given nominal variable and group entered as fixed factors and DASS score as the dependent variable.
Analyses 1-4 were first conducted to compare respondents with a self-reported mood disorder and those not reporting any mental disorder, and then comparing those with depressive disorder to those with bipolar disorder. The univariate analyses (step 5) were not analysed by mood disorder subtype given likely inadequacies in power from stratification analyses of the (relatively) modest number of respondents self-reporting bipolar disorder. A conservative alpha of p<.01 was adopted for all first-level analyses, while post-hoc test results were corrected using Tukey's method where necessary.
3. Results
A total of 8,014 respondents participated in survey 1 of the COLLATE project. There was substantial missing data for n=2545 respondents, and n=1010 of the remaining 5,469 respondents reported a mental disorder other than bipolar or depressive disorder. The final sample included the data of the n=1292 respondents self-reporting a mood disorder (either bipolar disorder or depressive disorder) and the n=3167 without any reported mental disorder.
3.1. Primary concerns
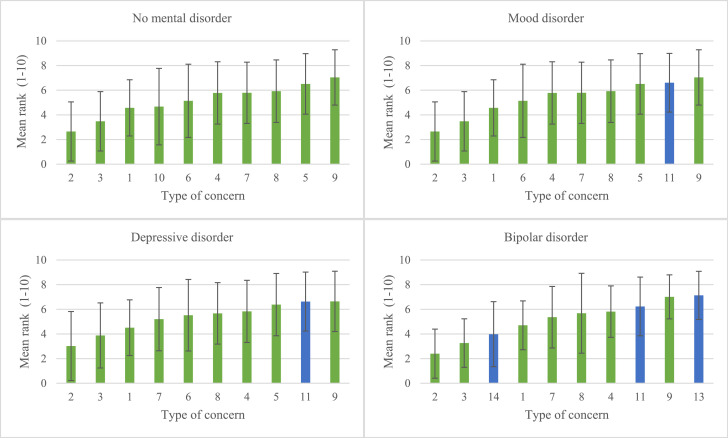
Table 1 shows the items relating to current concerns about the COVID-19 pandemic ranked by the frequency of endorsement in each group. Figure 1 shows the mean rankings of the top 10 most frequently endorsed items for each group ordered by mean ranking from most concerning (1) to least concerning (10). The most frequently endorsed item for those with a mood disorder and those with no mental disorder was “Implications for health and wellbeing of family/loved ones”. Compared to those with no mental disorder, “Dying of COVID-19 myself” did not fall into the top 10 most frequently endorsed items for respondents with a mood disorder. Instead, “Access to appropriate medical care” was included and ranked 9’th in order of importance.
Fig. 1.
Top 10 most frequently endorsed concerns for each group ordered by mean ranking from most concerning (1/left) to least concerning (10/right).
Note: Values reflect item ordering in the leftmost column in Table 1; 1=Implications for health and wellbeing of family/loved ones; 2= Loved one dying from COVID-19; 3=Loved one catching COVID-19; 4= Implications for health and wellbeing of society; 5=Australian economy; 6= Catching COVID-19 myself; 7= Implications for health and wellbeing of self; 8=Social isolation and social distancing; 9=Availability of food and medicines; 10=Dying of COVID-19 myself; 11=Access to appropriate medical care; 12=World economy; 13=Personal finances; 14=Risk of unemployment or reduced employment. Blue bars indicate deviation from top 10 most endorsed items by the group with no mental disorder. Error bars represent standard deviation.
When respondents with a mood disorder were separated by type, “Access to appropriate medical care”, “Risk of unemployment or reduced employment” and “Personal finances” were ranked in the top 10 most endorsed concerns for those with bipolar disorder (ranked 3’rd, 8’th and 10’th by importance). This was in place of “Australian economy” and “Catching COVID -19 myself” for respondents with depressive disorder (ranked 8’th and 4’th by importance); and “Catching COVID 19 myself”, “Dying of COVID -19 myself” and “Australian economy” in respondents with no mental disorder (ranked 5’th, 4’th and 9’th by importance).
3.2. COVID-19 related changes in personal situation, perceptions or behaviours
Within the mood disorder group, there were no differences in the personal situation, perceptions or behaviours of respondents with depressive disorder versus bipolar disorder (see Supplementary Table 4). Table 2 reports the proportions for these factors comparing the group with no mental disorder to the group with a mood disorder irrespective of subtype. Although the pattern of within-group proportion differences on all variables did not differ between those with a mood disorder and those without a mental disorder (see Supplementary Tables 2 and 3), there were significant differences in the distribution of responses between groups for several variables.
Table 2.
Age and PANAS descriptives, and comparisons of the proportions of respondents with no mental disorder versus respondents with mood disorder endorsing each category of the variables assessing COVID-19 related changes in personal situation, perceptions or behaviours.
| NO MENTAL DISORDER | MOOD DISORDER | COMPARISONS | |||||||||
| n per analysis | Proportion (%) | M(SD) | n per analysis | Proportion (%) | M(SD) | Test statistic | df | P value | Effect size | ||
| Age* | 3167 | 42.26(14.11) | 1292 | 37.16 (11.84) | 151.60 | 1,2832.55 | <.001 | 0.39 | |||
| Positive affect* | 3053 | 25.7(8.33) | 1261 | 22.44(7.61) | 154.73 | 1,2556.40 | <.001 | 0.41 | |||
| Negative affect* | 3053 | 17.86(6.98) | 1261 | 21.45 (7.86) | 198.09 | 1,2120.2 | <.001 | 0.48 | |||
| Gender | Male Female |
3167 | 20.7a 79.3a |
1292 | 13.5 86.5 |
31.10 | 1 | <.001 | 0.08 | ||
| Job loss | Yes No, reduced hours No but expected No |
3155 | 9.3a 12.4 7.1 71.2a |
1290 | 13.6 13.4 7.3 65.7 |
23.36 | 3 | <.001 | 0.07 | ||
| Work from home | Yes No |
3165 | 41.2a 58.8a |
1291 | 46.6 53.4 |
11.18 | 1 | .001 | 0.05 | ||
| Work from home difficulty | Very difficult Somewhat difficult No issues |
1857 | 10.2a 51.1 38.7a |
688 | 19.6 51.6 28.8 |
48.46 | 2 | <.001 | 0.14 | ||
| Change in non-employment related contact with others outside the home | No change Less time More time |
3164 | 36.1 44.0a 19.9a |
1292 | 33.6 49.3 17.1 |
11.24 | 2 | .001 | 0.05 | ||
| Change in exercise behaviour | More Less No change or I do not exercise normally+ |
3166 | 36.0a 42.3 21.7 |
1291 | 32.1 45.1 22.8 |
5.97 | 2 | .05 | 0.04 | ||
| Change in sleep duration | More Less No change+ |
3165 | 26.4a 42.3a 31.3a |
1291 | 35.6 46.7 17.7 |
93.38 | 2 | <.001 | 0.15 | ||
| Change in drinking behaviour | More Less No change+ |
3122 | 28.8a 13.8 70.7a |
1267 | 35.4 12.1 52.5 |
18.68 | 2 | <.001 | 0.07 | ||
| Perceived impact of government restrictions on mental health | Positive Negative No impact+ |
3162 | 25.4a 54.8a 19.9a |
1292 | 18.4 70.0 11.5 |
91.46 | 2 | <.001 | 0.14 | ||
| Expectations about return to ‘normal’ | <3 months <6 months <12 months >12 months No idea |
3158 | 4.7a 29.1a 38.2a 17.6 10.4 |
1286 | 3.0 23.6 41.8 19.5 12.1 |
24.14 | 4 | .001 | 0.07 | ||
Note: PANAS = Positive and Negative Affect Schedule; *Welch test statistics; Effect size is given as Cramer's V for nominal variables and Cohen's d for continuous variables. Bolded p values indicate significant differences between groups overall. a indicates significant difference in proportion of response between groups. + Wording of response category has been slightly changed for readability/consistency. Refer to Supplementary Table 1 for wording provided to respondents.
A higher proportion of the group with a mood disorder had lost their jobs as a result of COVID-19 compared to the group with no mental disorder, but the groups did not differ in the proportion of respondents working reduced hours or expecting to lose their job. A higher proportion of the mood disorder group were working from home compared to the group with no mental disorder; with double the proportion finding it ‘very difficult’ due to motivational or technical reasons, and 10% less having ‘no issues’. Compared to the group with no mental disorder, a higher proportion of respondents with mood disorder had less non-employment related contact with others outside the home compared to before the pandemic. Further, more experienced sleep disruptions, with less reporting no change and more reporting sleeping both more and less since the pandemic began. More mood disorder respondents also reported drinking more since the pandemic began, while less reported no change compared to the group with no mental disorder.
A perceived positive impact or no change in mental health as a result of government restrictions was reported by fewer respondents in the mood disorder compared to the group with no mental disorder, while 15% more respondents in the mood disorder group reported a negative impact. Finally, more respondents in the mood disorder group expected it to take longer for life to return to ‘normal’ than the group with no mental disorder i.e., less than 12 months versus less than six.
3.3. Psychological distress
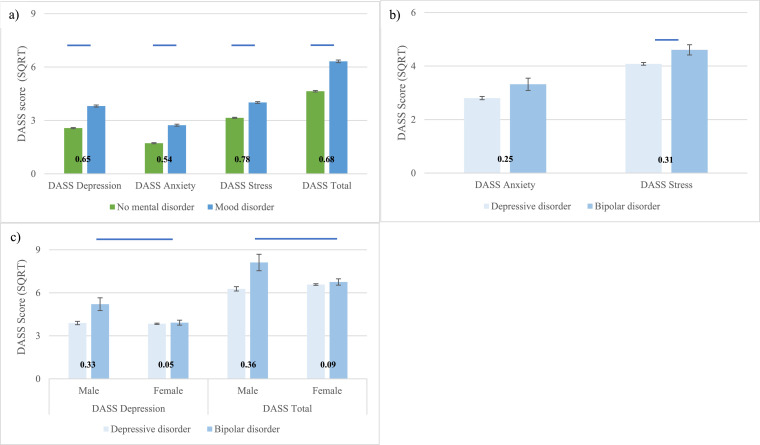
Group differences in DASS scores are shown in Fig. 2 (see Supplementary Table 5 for statistical values and Supplementary Table 6 for severity levels and comparison to non-clinical norms). As expected, psychological distress was elevated in respondents self-reporting a mood disorder compared to those with no mental disorder for all subscales of the DASS and the total score, after adjusting for momentary affect, age and gender. Mean scores remained in the ‘normal’ range across subscales for the group with no mental disorder, albeit with a 25-30% increase relative to published norms for depression and stress. In the mood disorder group, mean scores indicated moderate levels of depression, normal levels of anxiety and mild stress. Large effects were evident between those with no mental disorder and those with a mood disorder. Respondents with depressive disorder had lower stress levels (mild) than those with bipolar disorder (moderate), but anxiety was mild and equivalent in both subgroups. A significant group by gender interaction was evident for depression and total scores, where males and females with depressive disorder did not differ, but males with bipolar disorder had higher scores (borderline of severe and extremely severe) than females (moderate) with bipolar disorder.
Fig. 2.
Square root (SQRT) transformed Depression, Anxiety and Stress Scales (DASS) scores by group. Numbers in figures represent Cohen's d effects. Errors bars represent standard error.
a) DASS scores for respondents with no mental disorder versus a mood disorder. No group*gender interactions evident. Bars represent estimated marginal means adjusting for age, gender and momentary affect. Blue lines represent main effects of group.
b) DASS scores for respondents with depressive disorder versus bipolar disorder. Group*gender interactions were not evident for these variables. Bars represent estimated marginal means adjusting for age, gender and momentary affect. Blue lines represent main effects of group.
c) Gender*group interactions for depressive disorder versus bipolar disorder. Bars represent estimated marginal means adjusting for age and momentary affect. Blue lines represent gender differences in the bipolar disorder group (p≤.05 corrected [Tukey]). Cohens d= 0.02 vs. 0.08 for males vs females with depressive disorder and d=0.44 vs 0.36 for males and females with bipolar disorder.
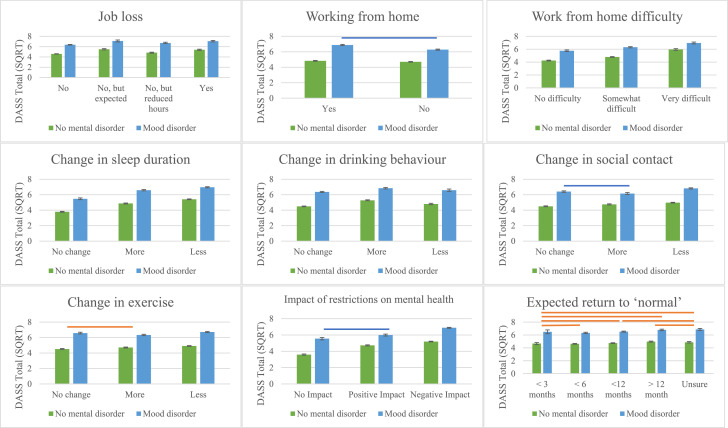
Fig. 3 shows the differences in DASS total scores for each level of the variables assessing COVID-19 related changes in personal situation, behaviours and perceptions between respondents with a mood disorder and those with no mental disorder. Significant main effects were evident for every variable (see also Supplementary Table 7), as were main effects of group; with mood disorder respondents having higher scores than those with no mental disorder irrespective of response to each variable.
Fig. 3.
Square root (SQRT) transformed Depression Anxiety and Stress Scale (DASS) scores as a function of COVID-19 related changes in personal situation, perceptions or behaviours in respondents with no mental disorder versus those with self-reported mood disorder.
Note bars represent estimated marginal means. A conservative alpha of p≤.01 was adopted at the first level. Post-hoc results are significant at p≤.05 corrected (Tukey). All comparisons are significant, except those represented by orange (main effect of group) or blue (interaction: mood disorder only) lines. Errors bars represent standard error.
Interaction effects were also evident for three variables, where in the mood disorder group, higher DASS scores were evident in respondents working from home than those who were not, but did not differ between those reporting ‘more’ or ‘no change’ in social time with others, or those reporting a ‘positive’ or ‘no impact’ of government restrictions on mental health. By contrast, DASS scores in the group with no mental disorder were higher for the former than the latter but did not differ by work location. In both groups, respondents who were spending less time with others outside the home or were perceiving a negative impact of government restrictions on mental health had higher DASS scores compared to those endorsing other categories, although scores were higher for those with a mood disorder.
4. Discussion
In this paper we provide an overview of the key current concerns, situational, perceptual and behavioural changes, and psychological distress levels of Australian's self-reporting a pre-existing mood disorder compared to those with no mental disorder during the COVID-19 pandemic. As expected, depression, anxiety, stress and general distress was heightened in the former compared to the latter, with all but anxiety further elevated in respondents with bipolar disorder compared to those with depressive disorder (albeit with small effects); and men with bipolar disorder having even higher levels of depression and general distress than women with bipolar disorder. This latter finding contradicts that of several prior studies showing the opposite gender effect under non-pandemic conditions (Arnold et al., 2016; Nivoli et al., 2011; Parker et al., 2014), such that males with bipolar disorder appear to be experiencing particularly severe psychological ill-health during the time of COVID-19. In light of evidence that suicidality is more common in males and the severely depressed (Hansson et al., 2018; Leadholm et al., 2014), this subgroup of people may be at an especially high risk of suicide given that their mean current depression severity fell at the borderline of severe and extremely severe.
The top 10 most frequently endorsed concerns related to COVID-19 appeared to be generally similar for individuals with mood disorders and those with no mental disorder; with the top 4 reflecting concerns for the health and wellbeing of loved ones, including loved ones catching or dying from COVID-19, and the health and well-being of society. However, compared to those with no mental disorder, respondents with a mood disorder were more likely to express concern for access to appropriate medical care, and were less likely to be concerned about dying of COVID-19 themselves. Within this, respondents with bipolar disorder were more likely to be concerned about their personal finances and their risk of unemployment or reduced employment than those with depressive disorder, and less likely than them to be concerned with the Australian economy or catching COVID-19 themselves.
While all groups were most concerned about the prospect of a loved one dying of COVID-19 followed by them contracting it, those with no mental disorder or a depressive disorder were next most concerned about implications for the health and well-being of loved ones, while those with bipolar disorder were next most concerned about the risk of unemployment or reduced employment. Notably however, although more respondents with a mood disorder had lost their job as a result of COVID-19 compared to respondents with no mental disorder, job loss rates or expectations about job loss did not differ between respondents with bipolar disorder and those with depressive disorder. The more common endorsement of items relating to financial stress in the former may thus be reflective of the heightened economic burden of bipolar disorder compared to the latter.
Indeed, there is evidence that healthcare utilisation costs are higher for bipolar disorder than depressive disorder, particularly for specialised psychiatric (as opposed to primary care) and pharmaceutical services (Williams et al., 2011). In terms of work productivity, the cost per year to bipolar disorder is double that of depressive disorder, with a greater number of lost work days, and thus income, likely to confer heightened financial disadvantage (Kessler et al., 2006). Reduced financial life-satisfaction has been documented in bipolar disorder previously (Van Rheenen and Rossell, 2014), where impulsive risk-taking behaviours such as reckless spending are central to (hypo)mania and represent a major source of financial difficulty and subsequent stress (Richardson et al., 2018). The convergence of these factors may thus confer a heavier personal financial strain to those with bipolar disorder, for which concern may be currently amplified by the economic precarity of the COVID-19 situation.
As expected, changes to lifestyle behaviours that are known to be important for emotional stability were more prevalent in individuals with a mood disorder; but did not differ between those with depressive disorder or bipolar disorder. That is, compared to those with no mental disorder, a higher proportion of individuals with a mood disorder reported spending less time in non-employment related contact with others, getting more or less sleep, and drinking more since the pandemic began. Further, a higher proportion expected it to take longer for life to return to ‘normal’, or perceived a negative impact of government restrictions on mental health. Psychological distress was highest in individuals reporting adverse situational or behavioural changes/perceptions; with those sleeping or exercising less more distressed than those sleeping or exercising more, and those who had lost their jobs more distressed than those who had not or those working reduced hours, but not those still expecting to. These same patterns were also evident in the individuals with no mental disorder, although general distress was higher in the mood disorder group compared to the no mental disorder group in every case.
Notably, respondents with a mood disorder were also more likely to find it very difficult to work from home due to technical or motivational reasons than those with no mental disorder. Those with a mood disorder were also more distressed if they were working from home than if they were not, particularly if they found it very difficult to do so. It is possible that this distress could be mitigated, in part, through regular employer check-ins or the provision of extra assistance to vulnerable staff who may be known to experience extremes of mood.
From the perspective of mood stability, the high proportion of individuals reporting COVID-19 related changes in situational and lifestyle factors key to its maintenance is concerning. It thus seems evident that the focus of population-based health promotion should be on ways to maintain a healthy lifestyle in the home even in the context of physical distancing restrictions. From a clinical care standpoint, individuals with mood disorders who report acute changes in maladaptive lifestyle behaviours should be monitored even more closely, especially given the association of these behaviours with elevated levels of depression, anxiety, and stress reported here. Psychoeducation in the form of healthy lifestyle-based guidance seems particularly pertinent for these individuals, given that that the impact of maladaptive lifestyle changes may unfortunately extend beyond emotional symptom exacerbation.
Indeed, lifestyle behaviours are key mediators of physical and cognitive health, which is typically compromised in bipolar and depressive disorder already (Evans et al., 2005; McIntyre et al., 2006). There is evidence that cessation of exercise, as well as sleep loss and increased alcohol intake, can amplify cardiometabolic dysfunction by altering biochemical and inflammatory marker profiles, reducing insulin sensitivity and inducing hypertriglyceridemia (Booth et al., 2008; Lippi et al., 2020; Poole et al., 2011). These factors have been widely linked to cognitive impairment as well as metabolic disease, to which those with mood disorders are more susceptible by virtue of genetic diathesis or psychotropic medication use (Killgore, 2010; Klop et al., 2013; Markwald et al., 2013; Mcintyre et al., 2005; Nixon et al., 2017; Rasgon et al., 2010; Shao et al., 2017). Thus, the maladaptive lifestyle changes documented in this group in response to COVID-19 might not only contribute to emotional decline and also cognitive impairment, but may further compound the risk of severe SARS-CoV-2 infection and associated medical complications (Zaman et al., 2020).
There are several factors that should be considered in the interpretation of our findings. First, we have described data from the first wave of the mental-health-focused COLLATE project dataset, in which participation was self-selected and subsequent sample representativeness potentially biased. Second, the data we report is cross-sectional, and any changes in situation, perceptions and behaviours since the pandemic began were retrospectively reported using non-validated questions devised by the authors. Longitudinal data is being collected to address this as part of the ongoing COLLATE project. Third, as the COLLATE project is population-focused, the presence (or absence) of mood disorder was self-reported. Medication use and other important clinical variables such as age of onset, psychosis history, bipolar subtype or predominant polarity was also not measured, nor were symptoms of relevance to mania. Hence, diagnosis of (or absence of) mental disorder could not be clinically verified and the clinical characteristics of the mood disorder group not ascertained. Nonetheless, there is evidence that individuals self-identifying as having bipolar disorder or depressive disorder typically meet criteria for each respective diagnosis (Kupfer et al., 2002; Sanchez-Villegas et al., 2008). Fourth, the number of individuals self-reporting a mood disorder in the sample was modest and the gender distribution within this unbalanced. Thus, caution should be used in interpreting the results of analyses of this subsample stratified by gender.
Finally, given the unexpected nature and fast-paced way in which the COVID-19 pandemic took hold, we do not have pre-COVID-19 baseline measures of mood and lifestyle in our respondents. Thus, we cannot be sure that the high levels of psychological distress in those with mood disorder reported here are a result of the pandemic. It is certainly a reasonable assumption that heightened distress in this group reflects pre-existing symptomatology inherent to the very essence of mood disorder. However, since variations in distress were associated with self-reported changes in personal situation, perceptions and lifestyle behaviours directly tied to COVID-19 in largely the same manner as seen in those without a mental disorder, it is plausible that such symptoms have worsened on account of the social and economic consequences of the virus.
In sum, the data reported here indicates that current psychological distress levels are elevated in individuals with mood disorder and are associated with maladaptive situational and lifestyle changes occurring in response to COVID-19. Concerns related to the pandemic strongly centre around the health and wellbeing of loved ones, oneself and society, as well as access to food, medicines and appropriate medical care. Individuals with bipolar disorder also appear to be more uniquely concerned about personal finances and unemployment than they are about the broader economy. In light of evidence that financial worries may represent a ‘final straw’ that triggers self-harm and suicidality (Barnes et al., 2016; Richardson et al., 2017), especially close attention to the mental health of individuals with bipolar disorder may be warranted. This is pertinent given the very severe levels of depression currently evident in males with the disorder, and the widespread economic hardships that are likely to be encountered as the pandemic continues to unfold.
Declaration of Competing Interests
The authors have no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Acknowledgments
Acknowledgements
The authors would like to thank all the participants who took the time and effort to take part in this study, especially during these challenging and unprecedented times. SLR holds a NHMRC Senior Fellowship (GNT1154651), and EJT (GNT1142424) and TVR (GNT1088785) hold NHMRC Early Career Fellowships. WLT (GNT1161609) and AP (GNT1159953) are supported by National Health and Medical Research Council (NHMRC) New Investigator Project Grants.
Role of the funding source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Contents of this article are the sole responsibility of the authors.
Data sharing
The dataset is available on request by qualified researchers/scientists. Requests require a concept proposal describing the purpose of data access, appropriate ethical approval, and provision for data security. All data analysis scripts and results files are available for review.
Footnotes
Those reporting a past history of hormone-related depression (e.g. postnatal depression or premenstrual dysphoric disorder) were not included in any analysis in this paper.
Compared to Australian norms for 18-90 year old's from Crawford et al. (2011). Note that mean DASS subscale scores in the Crawford et al. study were reported in raw form. To determine severity levels between COLLATE data and normative levels, these scores were subsequently doubled, as per prescribed methodology, to equate them to full scale DASS scores.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.06.037.
Appendix. Supplementary materials
References
- Arnold J.G., Martinez C., Zavala J., Prihoda T.J., Escamilla M., Singh V., Bazan M., Quiñones M., Bowden C.L. Investigating symptom domains of bipolar disorder for Spanish-speakers using the Bipolar Inventory of Symptoms Scale. J. Affect. Disord. 2016;205:239–244. doi: 10.1016/j.jad.2016.07.014. [DOI] [PubMed] [Google Scholar]
- Balanzá–Martínez V., Atienza–Carbonell B., Kapczinski F., De Boni R.B. Lifestyle behaviours during the COVID-19–time to connect. Acta Psychiatr. Scand. 2020 doi: 10.1111/acps.13177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes M., Gunnell D., Davies R., Hawton K., Kapur N., Potokar J., Donovan J. Understanding vulnerability to self-harm in times of economic hardship and austerity: a qualitative study. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-010131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth F.W., Laye M.J., Lees S.J., Rector R.S., Thyfault J.P. Reduced physical activity and risk of chronic disease: the biology behind the consequences. Eur. J. Appl. Physiol. 2008;102:381–390. doi: 10.1007/s00421-007-0606-5. [DOI] [PubMed] [Google Scholar]
- Bowen R., Balbuena L., Baetz M., Schwartz L. Maintaining sleep and physical activity alleviate mood instability. Prev. Med. 2013;57:461–465. doi: 10.1016/j.ypmed.2013.06.025. [DOI] [PubMed] [Google Scholar]
- Coello K., Kjærstad H.L., Stanislaus S., Melbye S., Faurholt-Jepsen M., Miskowiak K.W., McIntyre R.S., Vinberg M., Kessing L.V., Munkholm K. Thirty-year cardiovascular risk score in patients with newly diagnosed bipolar disorder and their unaffected first-degree relatives. Aust. N. Z. J. Psychiatry. 2019;53:651–662. doi: 10.1177/0004867418815987. [DOI] [PubMed] [Google Scholar]
- COVID-19 National Incident Room Surveillance Team COVID-19, Australia: Epidemiology Report 10: Reporting week ending 23:59 AEST 5 April 2020. Commun. Dis. Intell. 2020;44 doi: 10.33321/cdi.2020.44.30. [DOI] [PubMed] [Google Scholar]
- Crawford J., Cayley C., Lovibond P.F., Wilson P.H., Hartley C. Percentile norms and accompanying interval estimates from an Australian general adult population sample for self-report mood scales (BAI, BDI, CRSD, CES-D, DASS, DASS-21, STAI-X, STAI-Y, SRDS, and SRAS) Aust. Psychol. 2011;46:3–14. [Google Scholar]
- Dalack G.W., Roose S.P. Perspectives on the relationship between cardiovascular disease and affective disorder. J. Clin. Psychiatry. 1990 [PubMed] [Google Scholar]
- Evans D.L., Charney D.S., Lewis L., Golden R.N., Gorman J.M., Krishnan K.R.R., Nemeroff C.B., Bremner J.D., Carney R.M., Coyne J.C. Mood disorders in the medically ill: scientific review and recommendations. Biol. Psychiatry. 2005;58:175–189. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Goldstein B.I. Bipolar disorder and the vascular system: mechanisms and new prevention opportunities. Can. J. Cardiol. 2017;33:1565–1576. doi: 10.1016/j.cjca.2017.10.006. [DOI] [PubMed] [Google Scholar]
- Goldstein B.I., Baune B.T., Bond D.J., Chen P.H., Eyler L., Fagiolini A., Gomes F., Hajek T., Hatch J., McElroy S.L. Call to action regarding the vascular-bipolar link: a report from the vascular task force of the international society for bipolar disorders. Bipolar Disord. 2020 doi: 10.1111/bdi.12921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansson C., Joas E., Pålsson E., Hawton K., Runeson B., Landén M. Risk factors for suicide in bipolar disorder: a cohort study of 12 850 patients. Acta Psychiatr. Scand. 2018;138:456–463. doi: 10.1111/acps.12946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey A.G., Talbot L.S., Gershon A. Sleep disturbance in bipolar disorder across the lifespan. Clin. Psychol. (New York) 2009;16:256–277. doi: 10.1111/j.1468-2850.2009.01164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Akiskal H.S., Ames M., Birnbaum H., Greenberg P., Hirschfeld R.M.A., Jin R., Merikangas K.R., Wang P.S. The prevalence and effects of mood disorders on work performance in a nationally representative sample of US workers. A. J. Psychiatry. 2006;163:1561–1568. doi: 10.1176/appi.ajp.163.9.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D. Effects of sleep deprivation on cognition. Prog. Brain Res. Elsevier. 2010:105–129. doi: 10.1016/B978-0-444-53702-7.00007-5. [DOI] [PubMed] [Google Scholar]
- Klop B., do Rego A.T., Cabezas M.C. Alcohol and plasma triglycerides. Curr. Opin. Lipidol. 2013;24:321–326. doi: 10.1097/MOL.0b013e3283606845. [DOI] [PubMed] [Google Scholar]
- Kupfer D.J., Frank E., Grochocinski V.J., Cluss P.A., Houck P.R., Stapf D.A. Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J. Clin. Psychiatry. 2002;63:120–125. doi: 10.4088/jcp.v63n0206. [DOI] [PubMed] [Google Scholar]
- Leadholm A.K.K., Rothschild A.J., Nielsen J., Bech P., Østergaard S.D. Risk factors for suicide among 34,671 patients with psychotic and non-psychotic severe depression. J. Affect. Disord. 2014;156:119–125. doi: 10.1016/j.jad.2013.12.003. [DOI] [PubMed] [Google Scholar]
- Lippi G., Henry B.M., Sanchis-Gomar F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19) Eur. J. Prevent. Cardiol. 2020 doi: 10.1177/2047487320916823. 2047487320916823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the depression anxiety stress scales (Dass) with the beck depression and anxiety inventories. Behav. Res. Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Mansur R.B., Brietzke E., McIntyre R.S. Is there a “metabolic-mood syndrome”? A review of the relationship between obesity and mood disorders. Neurosci. Biobehav. Rev. 2015;52:89–104. doi: 10.1016/j.neubiorev.2014.12.017. [DOI] [PubMed] [Google Scholar]
- Mansur R.B., Lee Y., Subramaniapillai M., Cha D.S., Brietzke E., McIntyre R.S. Parsing metabolic heterogeneity in mood disorders: a hypothesis-driven cluster analysis of glucose and insulin abnormalities. Bipolar Disord. 2019 doi: 10.1111/bdi.12826. [DOI] [PubMed] [Google Scholar]
- Markwald R.R., Melanson E.L., Smith M.R., Higgins J., Perreault L., Eckel R.H., Wright K.P. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc. Natl. Acad. Sci. 2013;110:5695–5700. doi: 10.1073/pnas.1216951110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcintyre R.S., Konarski J.Z., Misener V.L., Kennedy S.H. Bipolar disorder and diabetes mellitus: epidemiology, etiology, and treatment implications. Ann. Clin. Psychiatry. 2005;17:83–93. doi: 10.1080/10401230590932380. [DOI] [PubMed] [Google Scholar]
- McIntyre R.S., Konarski J.Z., Soczynska J.K., Wilkins K., Panjwani G., Bouffard B., Bottas A., Kennedy S.H. Medical comorbidity in bipolar disorder: implications for functional outcomes and health service utilization. Psychiatr. Serv. 2006;57:1140–1144. doi: 10.1176/ps.2006.57.8.1140. [DOI] [PubMed] [Google Scholar]
- Nivoli A.M., Pacchiarotti I., Rosa A.R., Popovic D., Murru A., Valenti M., Bonnin C.M., Grande I., Sanchez-Moreno J., Vieta E. Gender differences in a cohort study of 604 bipolar patients: the role of predominant polarity. J. Affect. Disord. 2011;133:443–449. doi: 10.1016/j.jad.2011.04.055. [DOI] [PubMed] [Google Scholar]
- Nixon A.J., Huỳnh C., Godbout R., Robillard R. Sleep and cardiovascular dysfunctions in bipolar disorder. Curr. Sleep Med. Rep. 2017;3:251–261. [Google Scholar]
- North C.S., Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013;310:507–518. doi: 10.1001/jama.2013.107799. [DOI] [PubMed] [Google Scholar]
- Parker G., Fletcher K., Paterson A., Anderson J., Hong M. Gender differences in depression severity and symptoms across depressive sub-types. J. Affect. Disord. 2014;167:351–357. doi: 10.1016/j.jad.2014.06.018. [DOI] [PubMed] [Google Scholar]
- Phillipou A., Meyer D., Neill E., Tan E.J., Toh W.L., Van Rheenen T.E., Rossell S.L. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Int. J. Eat. Disord. 2020 doi: 10.1002/eat.23317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole L., Hamer M., Wawrzyniak A.J., Steptoe A. The effects of exercise withdrawal on mood and inflammatory cytokine responses in humans. Stress. 2011;14:439–447. doi: 10.3109/10253890.2011.557109. [DOI] [PubMed] [Google Scholar]
- Rasgon N.L., Kenna H.A., Reynolds-May M.F., Stemmle P.G., Vemuri M., Marsh W., Wang P., Ketter T.A. Metabolic dysfunction in women with bipolar disorder: the potential influence of family history of type 2 diabetes mellitus. Bipolar Disord. 2010;12:504–513. doi: 10.1111/j.1399-5618.2010.00839.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson T., Jansen M., Fitch C. Financial difficulties in bipolar disorder part 1: Longitudinal relationships with mental health. J. Mental Health. 2018;27:595–601. doi: 10.1080/09638237.2018.1521920. [DOI] [PubMed] [Google Scholar]
- Richardson T., Jansen M., Turton W., Bell L. The relationship between Bipolar Disorder and financial difficulties: A qualitative exploration of client's views. Clin. Psychol. Forum. 2017 [Google Scholar]
- Sanchez-Villegas A., Schlatter J., Ortuno F., Lahortiga F., Pla J., Benito S., Martinez-Gonzalez M.A. Validity of a self-reported diagnosis of depression among participants in a cohort study using the Structured Clinical Interview for DSM-IV (SCID-I) BMC Psychiatry. 2008;8:43. doi: 10.1186/1471-244X-8-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato K., Mano T., Iwata A., Toda T. Neuropsychiatric adverse events of chloroquine: a real-world pharmacovigilance study using the FDA Adverse Event Reporting System (FAERS) database. BioScience Trends. 2020 doi: 10.5582/bst.2020.03082. [DOI] [PubMed] [Google Scholar]
- Shao T.N., Yin G.Z., Yin X.L., Wu J.Q., Du X.D., Zhu H.L., Liu J.H., Wang X.Q., Xu D.W., Tang W.J. Elevated triglyceride levels are associated with cognitive impairments among patients with major depressive disorder. Compr. Psychiatry. 2017;75:103–109. doi: 10.1016/j.comppsych.2017.03.007. [DOI] [PubMed] [Google Scholar]
- Stein B.D., Elliott M.N., Jaycox L.H., Collins R.L., Berry S.H., Klein D.J., Schuster M.A. A national longitudinal study of the psychological consequences of the September 11, 2001 terrorist attacks: Reactions, impairment, and help-seeking. Psychiatry: Interpersonal Biol. Processes. 2004;67:105–117. doi: 10.1521/psyc.67.2.105.35964. [DOI] [PubMed] [Google Scholar]
- Tan, E.J., Rossell, S.L., Neill, E., Phillipou, A., Tan, E.J., Toh, W.L., Van Rheenen, T.E., Meyer, D., In press. Considerations for assessing the impact of the COVID-19 pandemic on mental health in Australia. Aust. N. Z. J. Psychiatry. [DOI] [PMC free article] [PubMed]
- Van Rheenen T.E., Lewandowski K.E., Bauer I.E., Kapczinski F., Miskowiak K., Burdick K.E., Balanzá‐Martínez V. Current understandings of the trajectory and emerging correlates of cognitive impairment in bipolar disorder: an overview of evidence. Bipolar Disord. 2019 doi: 10.1111/bdi.12821. [DOI] [PubMed] [Google Scholar]
- Van Rheenen T.E., Rossell S.L. Objective and subjective psychosocial functioning in bipolar disorder: an investigation of the relative importance of neurocognition, social cognition and emotion regulation. J. Affect. Disord. 2014;162:134–141. doi: 10.1016/j.jad.2014.03.043. [DOI] [PubMed] [Google Scholar]
- Vic Gov, 2020. Stage 3 restrictions are now in placehttps://www.vic.gov.au/coronavirus-covid-19-restrictions-victoria#stage-3-restrictions-are-now-in-place.
- Watson D., Clark L.A., Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J.Personal. Soc. Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Williams M.D., Shah N.D., Wagie A.E., Wood D.L., Frye M.A. Direct costs of bipolar disorder versus other chronic conditions: an employer-based health plan analysis. Psychiatr. Serv. 2011;62:1073–1078. doi: 10.1176/ps.62.9.pss6209_1073. [DOI] [PubMed] [Google Scholar]
- Zaman S., MacIsaac A.I., Jennings G.L., Schlaich M., Inglis S.C., Arnold R., Chew D.P., Kumar S., Thomas L., Wahi S. Cardiovascular disease and COVID-19: Australian/New Zealand consensus statement. Med. J. Aust. 2020;1 doi: 10.5694/mja2.50714. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.