Abstract
By March 31, 2020, COVID-19 had spread to more than 200 countries. Over 750,000 confirmed cases were reported, leading to more than 36,000 deaths. In this study, we analysed the efficiency of various intervention strategies to prevent infection by the virus, SARS-CoV-2, using an agent-based SEIIR model, in the fully urbanised city of Shenzhen, Guangdong Province, China. Shortening the duration from symptom onset to hospital admission, quarantining recent arrivals from Hubei Province, and letting symptomatic individuals stay at home were found to be the three most important interventions to reduce the risk of infection in Shenzhen. The ideal time window for a mandatory quarantine of arrivals from Hubei Province was between 10 January and January 17, 2020, while the ideal time window for local intervention strategies was between 15 and 22 January. The risk of infection could have been reduced by 50% if all symptomatic individuals had immediately gone to hospital for isolation, and by 35% if a 14-day quarantine for arrivals from Hubei Province had been introduced one week earlier. Intervention strategies implemented in Shenzhen were effective, and the spread of infection would be controlled even if the initial basic reproduction number had doubled. Our results may be useful for other cities when choosing their intervention strategies to prevent outbreaks of COVID-19.
Keywords: COVID-19, Infection spread, Close contact, Agent-based model, SEIR model
Highlights
-
•
Shortening the delay to hospital is the most effective intervention in Shenzhen.
-
•
10 to 17 January is the best time for a mandatory quarantine of Hubei's arrivals.
-
•
15 to 22 January is the best time for local intervention strategy in Shenzhen.
-
•
Work/school closure and mask wearing are effective interventions in other countries.
-
•
Airport screening is not very effective.
Practical implications
Our analysis shows that the best time point to implement travel restriction and local intervention strategies in Shenzhen is between 10 and 17 January and 15 and 22 January, respectively. For Shenzhen, the most critical intervention strategies are shortening the duration from symptom onset to hospital admission and quarantining arrivals from Hubei province. However, for other countries, quarantining arrivals from high-risk countries, stopping working and schooling and mask wearing stand out. We also found out that screening for imported individuals and implementing strategies too early are ineffective for infection risk reduction.
1. Introduction
The first case of COVID-19 was identified and reported in the city of Wuhan, the capital of Hubei Province, China, in early December 2019 [1]. By March 31, 2020 the disease had spread into more than 200 countries, with more than 750,000 confirmed cases and more than 36,000 deaths [2]. More than 82,000 confirmed cases were reported in China alone, with nearly 15,000 cases in provinces other than Hubei [3]. Guangdong Province, where the city of Shenzhen is located, had 1438 confirmed cases reported, making it the most affected province in China other than Hubei [3]. Within Guangdong, Shenzhen was the most affected city with 450 confirmed cases by 31 March [4].
Many studies have used mathematical models (e.g. the SEIR model, a stochastic branching process model) to predict the spread of SARS-CoV-2 infection, analyse the efficiency of intervention strategies such as contact tracing, and determine the delay from symptom onset to hospital admission [[5], [6], [7], [8]]. However, it is difficult for the existing mathematical models to consider micro-patterns such as personal decisions and preferences, spatial relationships of a population including distributions of buildings [9], and the dynamic links between social and environmental processes [10]. Agent-based models were developed based on cellular automata and artificial life. The defining feature of agent-based models is that elements of the system are represented primarily as discrete agents with several unique attributes [11]. Integrating mathematical models into an agent-based approach is promising [12,13].
Shenzhen became the first fully urbanised city (100% of urbanisation rate) in China in 2016 [14]. An analysis of the spread of SARS-CoV-2 infections in Shenzhen may be useful as a reference for other urbanised cities. In this study, we simulated the spread of SARS-CoV-2 infections in the city between 1 January and February 16, 2020 using an agent-based SEIIR model (defined below in Section 2.3). We analysed the daily effective reproduction number of the virus , the infection type (e.g. imported infection, family secondary infection, etc.), and the spread of SARS-CoV-2 infection under different spatiotemporal settings with different basic reproduction numbers () and seven different intervention strategies including mask wearing, mandatory quarantine for recent arrivals from Hubei, screening at transport stations, work stoppage and school closure, temperature detection in public places, delay from symptom onset to hospital admission, and the probability of self-quarantine at home after symptom onset.
2. Methods
2.1. Data sources
An agent-based SEIIR model was used to simulate the spread of infections in Shenzhen from 1 January to February 16, 2020. All demographic data were obtained from the Statistics Bureau of Shenzhen Municipality [15]. The data for COVID-19 cases were from case reports by Shenzhen Municipal Health Commission [4]. All locations were simplified and divided into seven groups, including residences (D, residential communities including homes), workplaces (W, companies including offices), schools (S, schools including classes), restaurants (R), markets (K), shopping malls (M), and hospitals (H) [9]. Detailed settings for all seven locations can be found in Appendix A. Data for hospitals and schools were from the Shenzhen Municipal Government [16,17], and data for shopping malls were from the Yingshang big data report [18]. We also considered population inflow and outflow in Shenzhen, and all migration data between 1 January and 16 February were obtained from our collaborator, Baidu Map Insight. In the simulation, many time-variant parameters were set based on the governmental policies of Shenzhen, and all of these policies were obtained from the Shenzhen Education Bureau [19,20], Shenzhen Municipal Health Commission [4], Shenzhen CDC [21], Commercial Bureau of Shenzhen Municipality [22], Shenzhen Housing and Construction Bureau [23], Sohu News [24], Shenzhen Special Zone Newspaper [25], and Pengpai News [26].
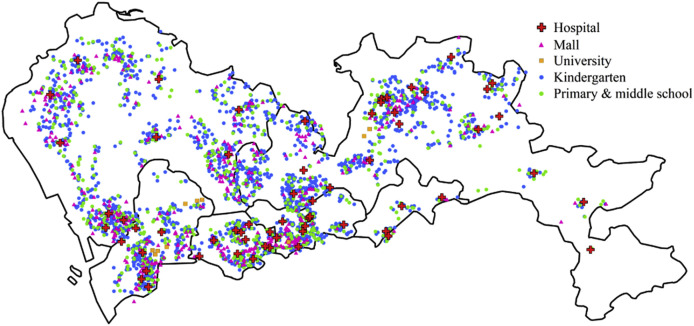
2.2. The city
Shenzhen occupies a total area of 1997 km2 and has a population of more than 13.02 million [15]. The population density is more than 6500 people/km2. Shenzhen has 64 hospitals, 2455 schools [16,17], and 440 shopping malls [18] (Fig. 1 ).
Fig. 1.
Geographic distributions of hospitals, kindergartens, primary and middle schools, universities, and shopping malls in Shenzhen.
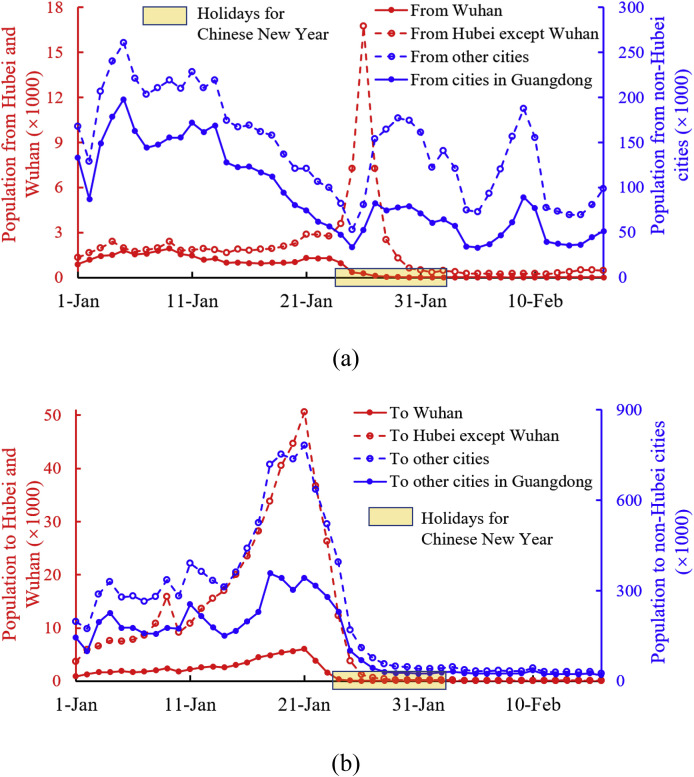
Shenzhen has many migrant workers. The inflow and outflow populations of Shenzhen between 1 January and February 16, 2020 are shown in Fig. 2 . Before the first day of the Chinese New Year holidays (24 January), the net outflow population (the outflow population after subtracting the inflow population) was 6,198,461. Because of the COVID-19 outbreak, only 1,596,987 of the net outflow population returned to Shenzhen from 24 January to 16 February, which means approximately 4.6 million residents were still outside of Shenzhen by 16 February. Of the entire inflow population, 0.5% were from Wuhan, 1.3% were from Hubei Province excluding Wuhan, and 36.9% were from other provinces excluding Hubei and Guangdong Provinces. We only simulated the spread of SARS-CoV-2 infection between 1 January and 16 February.
Fig. 2.
Population moved into and out of Shenzhen between 1 January and February 16, 2020. (a) Inflow and (b) outflow populations.
2.3. Agent-based SEIIR model
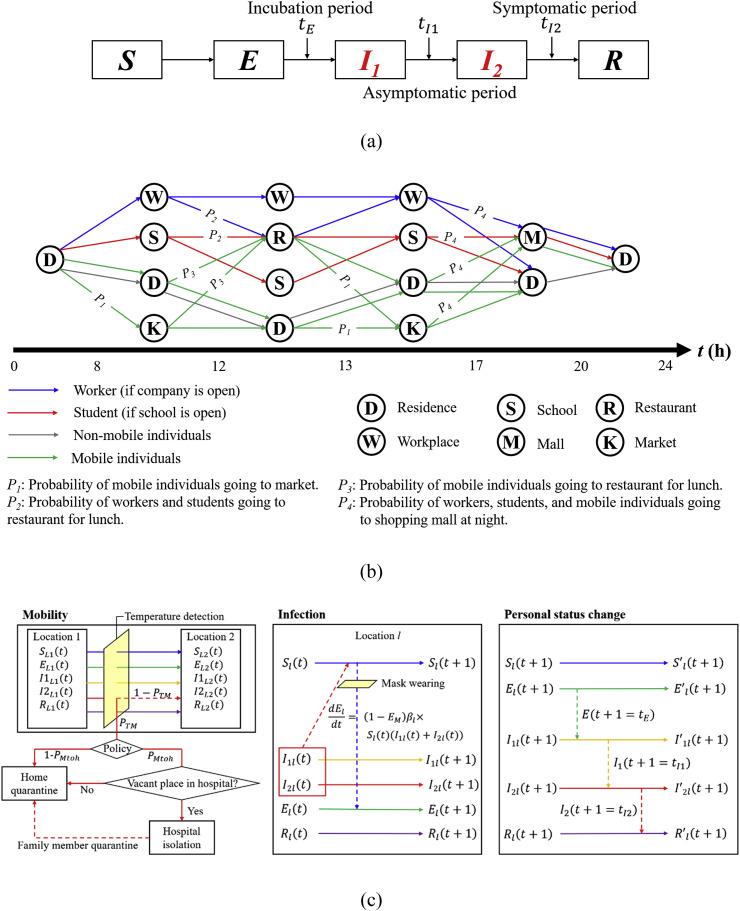
SEIR model is widely used in the simulation of infection spread [27], especially in COVID-19 transmission [28,29]. We used an SEIIR model (Fig. 3 a) and integrated it into an agent-based approach. All individuals were categorised into 5 groups: the susceptible (S), the exposed without symptoms who are also non-infectious (E), the infected without symptoms but who are infectious (), the infected with symptoms but who are not hospitalised (), and the removed, namely the infected who are either hospitalised, recovered, or dead (R). The incubation period was set to 120 h (5 days) [1,30]. The generation time was set to 7 days [1,31], so that the mild symptomatic period was 48 h (2 days). The symptomatic infectious period changes with time and will be introduced later.
Fig. 3.
Model introduction. (a) SEIIR model; (b) daily commutes in an agent-based model (the ratio of workers/students going to companies/schools, and of to , are time-variant parameters); (c) three steps in the simulation (: probability of temperature detection when entering public areas; : probability of hospitalisation if a person is detected to be infected; : mask efficiency for infection risk reduction; means that the personal timer reaches the total time of status ).
In the agent-based model, all individuals were divided into 4 groups: students (), workers (), people without mobility (, simplified as ‘non-mobile individuals’), and people with mobility who do not need to go to work or school (, simplified as ‘mobile individuals’). In this model we considered that students included all people aged between 4 and 18 years, and all university students; workers included everyone aged between 19 and 60 years, except for the unemployed and university students; non-mobile individuals included those aged under 3 and over 80 years; and mobile individuals included those aged between 19 and 79 years who are not workers. The unemployment rate in Shenzhen in 2019 was 2.3% [15]. Therefore, according to the age distribution there were in total 10,421,180 workers (80.0%), 1,650,100 students (12.7%), 358,614 non-mobile individuals (2.8%), and 596,706 mobile individuals (4.6%) in the city as of January 1, 2020.
The time step was set to 1 h in the simulation. The assumptions of individuals’ daily routes are shown in Fig. 3b. Non-mobile individuals were assumed to stay at home the entire day. We considered two commuting patterns, weekday and weekend.
We considered three steps in the simulation: mobility, infection, and personal status change (Fig. 3c). In mobility, all residents move between buildings (lines between locations in Fig. 3b). If there is a temperature detection at all public places, a symptomatic patient would be moved to hospitals and placed under mandatory home quarantine based on detailed policy. Some policies also force family members of the infected to stay at home for 14 days for self-quarantine. In infection, all susceptible individuals have a probability to be infected if there are infectious patients ( and ) in the same indoor environment. The infection probability also considered the risk reduction brought by mask wearing. All people have a timer in the simulation. In personal status change, the timer of each person pluses 1 h every step. And personal status (, , , and ) would change to the next status when the personal timer reaches the threshold of each period.
The SARS-CoV-2 virus is mainly transmitted via the close contact route [[32], [33], [34]]. In offices, people spend 10% of their time in close contact [35,36]. In a primary school, students spend nearly one third of their time in close contact [37]. Here, we assumed that students in schools on average spent 20% of their time in close contact with others. In restaurants, having a meal face-to-face with others is more likely, and we also hypothesised that people spent 20% of their time in close contact. According to Ferguson et al. [38], the ratio of close contact rates in homes, offices, schools, and shopping malls is 1:1:2:1/6. In these simulations, we hypothesised that the close contact rate of people in a residential community (out of their own home), in a company (out of their own office), and in a school (out of their own class) was 10% of the close contact rate in a home, office, or class, respectively. Each person was considered to be randomly having close contacts with others while indoors.
The simulation considered all data between 1 January and February 16, 2020. From the case reports of the Shenzhen Municipal Health Commission [4], for each patient the date of entering Shenzhen, date of symptom onset, date of hospital admission, and city of origin were known. These data were used for the initial settings of the simulation. Individual status () when entering Shenzhen was deduced based on the case report and the length of the different periods. We assumed that individuals entered Shenzhen at random times throughout the day. In the simulation, we set the initial number for viral reproduction, , to 2.5, and we used the effective reproduction number per day, , defined as the number of secondary infections generated by an infected index case in the presence of control interventions, to show the severity of the spread of infection. The details of these data are listed in Appendix B. All fixed parameter settings for the simulation are listed in Table C1.
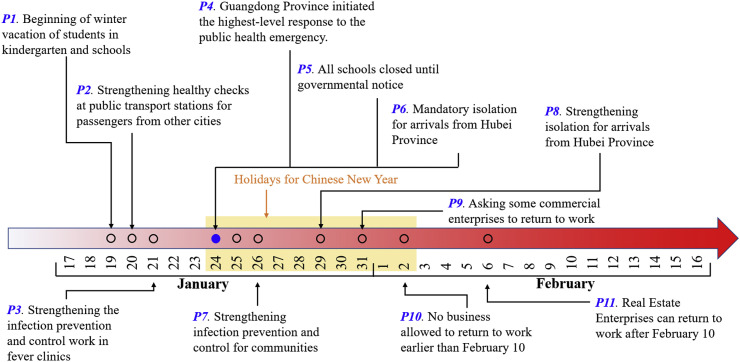
Fig. 4 lists 11 relevant policies for infection prevention and control enacted by the Shenzhen and Guangdong governments. We also set all time-variant parameters in the simulation based on these policies (referenced in Appendix C).
Fig. 4.
Policies for infection prevention and control by the Shenzhen and Guangdong governments.
3. Results
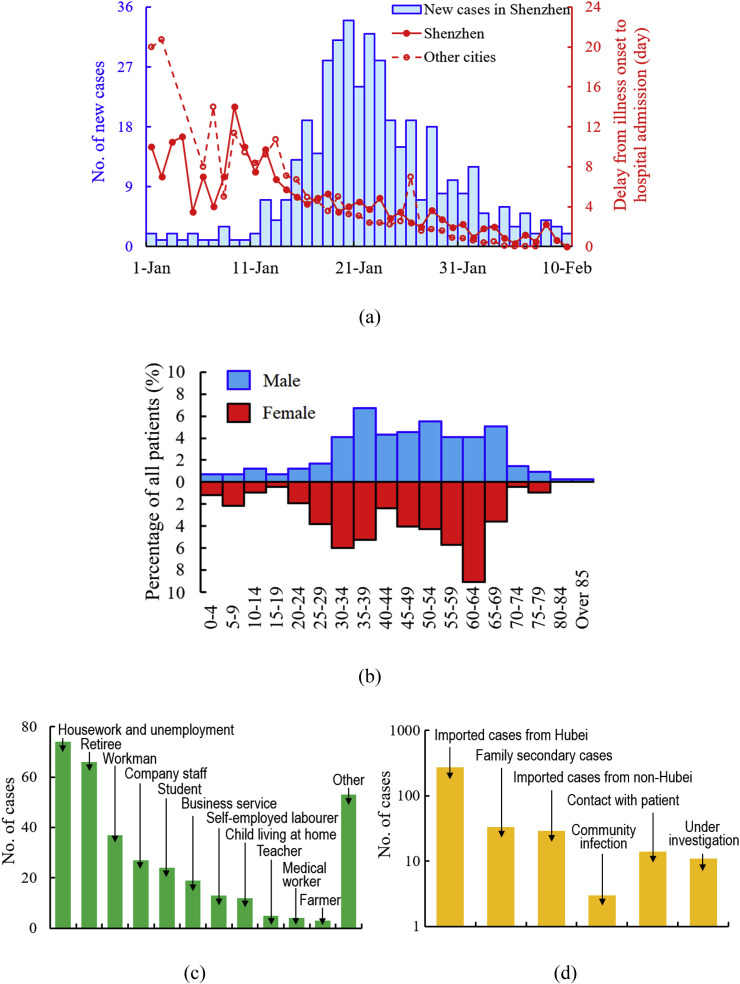
Up until February 16, 2020, Shenzhen had 418 confirmed cases of COVID-19 [4]. From the real statistics, the average delay from symptom onset to hospital admission in Shenzhen was 3.9 days, slightly longer than that of other cities (2.70 days) (Fig. 5 a). Among all infected patients, 47.5% were male, and the average age of infected patients was 45 (Fig. 5b). Except for cases ‘under investigation’, 85.8% of confirmed cases were imported, of which 77.6% were from Hubei Province and 8.2% were from non-Hubei provinces. Among local cases, 66% were home secondary cases (Fig. 5c). House workers, the unemployed, and the retired had the highest infection risks, and accounted for more than 52% of confirmed cases (Fig. 5d).
Fig. 5.
Case analysis of COVID-19. (a) Daily new cases in Shenzhen, and the delay from symptom onset to hospital admission in both Shenzhen and other cities. (b) Confirmed case distribution by age and gender. (c) Occupational distribution of confirmed cases (information from 337 valid cases). (d) Causes of infection (information from 364 valid cases).
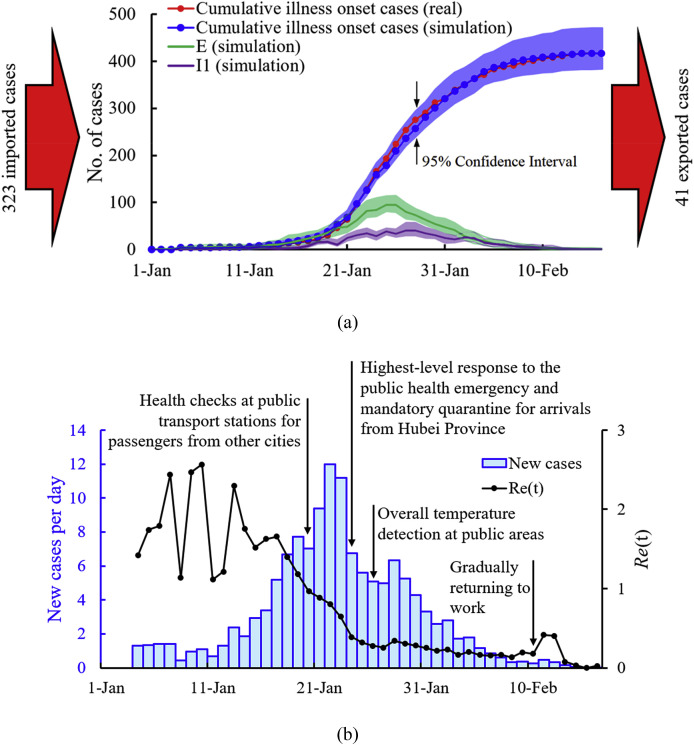
Using these detailed parameters, our simulation of the spread of infections from 1 January to 16 February is shown in Fig. 6 a. The peak values of (92 cases) and (38 cases) appear around 26 January and 28 January, respectively. Because governments appealed to residents not to leave their homes, many residents stayed at home during the outbreak. According to the simulation results, approximately 40 cases who were in the incubation period or the asymptomatic period left Shenzhen. Nearly two-thirds of local patients were infected in their homes. This value is consistent with the observed value of ‘family secondary cases’ in Fig. 5c. For non-family infected cases, 52%, 18%, 16%, and 9% were infected in a workplace, restaurant, shopping mall, or school, respectively (Fig. D1). The daily effective reproduction number fluctuated between 1.1 and 2.6 at the beginning of January and decreased to 1.0 on 20 January (Fig. 6b). After the highest-emergency response on 24 January, decreased to 0.4, and was no higher than 0.1 after 13 February, even though some workers had returned to their workplaces. The simulation results for the spread of infection in Shenzhen under uncontrolled conditions are also shown in Fig. E1.
Fig. 6.
Simulation results. (a) Spread of infections with time (cumulative symptom onset cases are equal to the total numbers of and combined); (b) daily effective reproduction number .
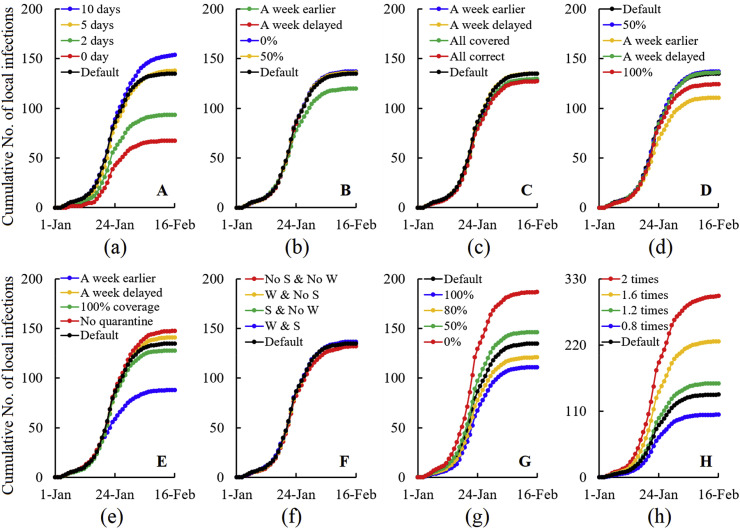
The simulated spread of infections under different intervention methods is shown in Fig. 7 a–g. For all results in Fig. 7, only one parameter was changed at a time in each case, while all other parameters were kept at the default values (shown in Tables C1 and C2). From the simulation results, the three most effective intervention strategies for reducing the risk of infection in Shenzhen were shortening the delay from symptom onset to hospital admission, early implementation of mandatory quarantine for arrivals from Hubei Province, and increasing the probability of staying at home after symptom onset. If all patients had been able to go to hospital immediately after symptom onset, the number of local infections could have been reduced by 50% (Fig. 7a). If temperature detection in public places had been advanced by one week (from 26 January to 19 January), 11% of the local infections could have been avoided (Fig. 7b). Health screening made little contribution in Shenzhen, with only 6% of local infections being avoided even if all symptomatic individuals had been correctly found (Fig. 7c). If all residents in Shenzhen had started wearing masks in all public places one week earlier, local infections could have been reduced by 20% (Fig. 7d). Mandatory quarantine for arrivals from Hubei Province was one of the most critical intervention methods. If the Shenzhen government had advanced the mandatory quarantine for arrivals from Hubei Province by one week (from 24 January to 17 January), 35% of local infections could have been avoided (Fig. 7e). The impact of work stoppage and school closure was not significant because there were few infectious cases after 2 February (the last day of the Chinese New Year holiday, which started on 24 January) (Fig. 7f). Self-quarantine after symptom onset was also important in reducing the risk of infection, and the total number of local infections would have been increased by 39% if there had been no self-quarantine (Fig. 7g). Fig. 7h shows the spread of infection with different . The sensitivity analyses for other parameters are shown in Appendix F.
Fig. 7.
Spread of SARS-CoV-2 infection under different intervention strategies. (a) Delay from symptom onset to hospital admission; (b) temperature detection in public places (0% indicating no temperature detection, 50% indicating half of public places had temperature detection after 24 January. The reference date is 24 Jan); (c) screening for incoming individuals (‘all covered’ means all incoming individuals are screened and ‘all correct’ means the correct rate of detection is 100%); (d) mask wearing; (e) mandatory quarantine for arrivals from Hubei Province (The reference date is 24 Jan); (f) school closure and work stoppage (‘S’, ‘No S’, ‘W’, and ‘No W’ represent schools open, school closure, workplaces open, and work stoppage, respectively); (g) probability of symptomatic patients staying at home; (H) initial . ‘A week earlier’ and ‘A week delayed’ mean that the strategy is conducted a week earlier or a week later than the current implementation date.
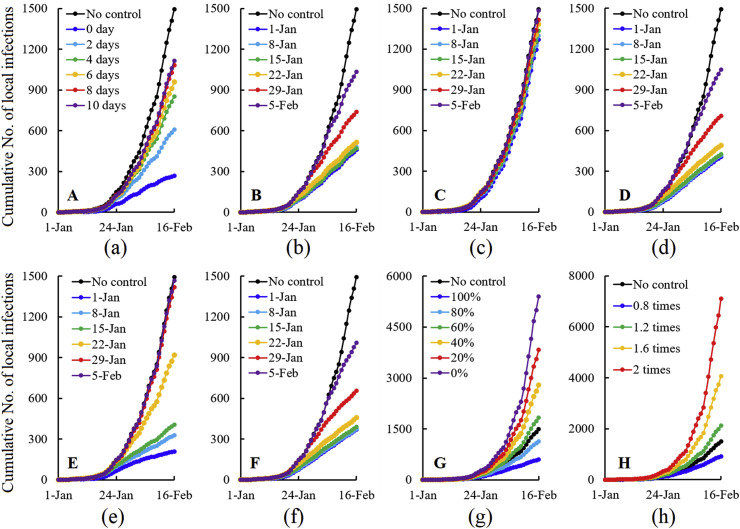
The spread of infection under various conditions with only one control method is shown in Fig. 8 a–g. In this simulation, Chinese New Year holiday is not considered. If all symptomatic patients could have gone to hospital within 2 days, the total infection risk would have been reduced by 60% (Fig. 8a). Temperature detection in public places can filter out many symptomatic patients, and 65% of infections could have been avoided if this control measure had been conducted since 15 January (Fig. 8b). If there had been no intervention strategy against the local spread of infections, screening for all incoming individuals would have been ineffective (Fig. 8c). In addition, 100% mask usage in all public places from 15 January could have prevented 67% of infections (Fig. 8d). Up until 16 February, the total number of infections would have been reduced by 86% if a 14-day mandatory quarantine for arrivals from Hubei Province had been conducted since 1 January (Fig. 8e). However, the risk of infection would have been reduced by only 39% if the quarantine had started on 22 January. If workers and students had stopped working and going to school after 22 January, nearly 70% of infections would have been avoided (Fig. 8f). If 100% of patients had stayed at home after symptom onset, the risk of infection would have been reduced by 60% compared with a situation where only 70% of patients stayed at home (Fig. 8g). Fig. 8h shows the uncontrolled spread of infection under different .
Fig. 8.
SARS-CoV-2 infection under only one intervention strategy. (a) Delay from symptom onset to hospital admission; (b) temperature detection in public places; (c) screening for incoming individuals; (d) mask wearing; (e) mandatory quarantine for arrivals from Hubei province; (f) school closure/work stoppage; (g) probability of symptomatic patients staying at home; (h) initial .
4. Discussion
Almost immediately after the recognition of the human-to-human transmission of the SARS-CoV-2 virus on January 20, 2020, Wuhan implemented its travel ban on 23 January. Unfortunately, approximately 5 million individuals had already left Wuhan as the traditional Chunyun period (Chinese New Year holiday travel season) started at least one week prior to the Chinese New Year celebration on 25 January [39,40]. Following the lockdown of Hubei Province, 30 other Chinese provinces or province-level regions initiated the highest-level emergency response before 26 January. After one month of efforts, the daily new cases reported in mainland China were reduced to fewer than 500 [3]. Currently, COVID-19 has gained a foothold throughout the world. COVID-19 differs from other infectious diseases (e.g. SARS) in terms of infectious period, transmissibility, clinical severity, and the extent of community spread [41]. Therefore, intervention strategies that are useful for control of other infectious diseases may not be effective for the SARS-CoV-2 virus and the COVID-19 disease that it causes.
Based on the current intervention strategies in Shenzhen, by 16 February local infections would have increased by 120% if the had doubled. However, this implies that the outbreak could still have been controlled under Shenzhen's intervention strategies even if the had doubled. We analysed the efficiency of seven intervention strategies on COVID-19 cases in Shenzhen based on both realistic and uncontrolled conditions. Shortening the duration from symptom onset to hospital admission, quarantining recent arrivals from Hubei Province, and letting symptomatic individuals stay at home were found to be the three most important interventions to reduce the risk of infection in Shenzhen.
The simulation was conducted based on a deterministic model, and the uncertainty is relatively small comparing to a stochastic model. The uncertainty of the simulation is relatively higher when the total number of the infected is small. We also did a sensitivity analysis for each parameter to show how uncertainty is influenced by changes of parameters.
In the study, all results were obtained based on the hypothesis that all data are real and complete. Inaccurate and incomplete testing might have biased the findings. We did not consider asymptomatic patients in the simulation, and it would also bring some errors.
4.1. intervention strategies on the early stage
More strategies will lead to greater potential economic impacts [42] and affect the daily life of the population. Intervention strategies implemented at the right time bring not only the highest intervention efficiency, but also the lowest negative impact on society. In this epidemic, many intervention strategies are available to reduce the risk of infection. The efficiency of intervention strategies depends on the phase of the local epidemic. Travel restrictions (including prohibiting all transport from high-risk areas), screening at transport stations (e.g. airport screenings), and a 14-day mandatory quarantine for incoming individuals are efficient in reducing infection risk in the early phases of an outbreak. In Shenzhen, 90% of imported cases were from Hubei Province. If the government had advanced the 14-day mandatory quarantine for arrivals from Hubei Province by one week, 35% of local infections could have been avoided. However, only an additional 4% of local residents would have been infected if the mandatory quarantine had been delayed by one week.
Screening for incoming individuals could on average have shortened the delay from symptom onset to hospitalisation by approximately 3 days compared with local cases [43]. Many countries including the USA, Russia, Australia, and Italy started to suspend or limit flights to mainland China and strengthened airport screening in early February [44,45]. Based on our analysis, the time period from 10 January to 17 January would have been the best to implement mandatory quarantine for people from Hubei Province and health checks for all incoming individuals. However, because of the incubation period, sensitivity of exit and entry screenings, and the proportion of asymptomatic cases, it is estimated that 46% of infected travellers were not detected [46]. The infected would also permeate into a city despite the 14-day quarantine because 1% of cases will develop symptoms after the mandatory quarantine period [47].
4.2. Intervention strategies on the middle and late stages
These methods, which are effective in the early phase of a COVID-19 epidemic, are ineffective in completely eliminating the disease [48]. When local transmissions start (the second phase), other intervention strategies become more effective. For Shenzhen, shortening the delay from symptom onset to hospital admission, staying at home after symptom onset, and wearing a mask were the most effective intervention strategies during this epidemic phase. If 100% of patients could have stayed at home after symptom onset, the local infection risk would have been reduced by 60% compared with a condition of free movement of all symptomatic patients. If all patients could have gone to hospital for isolation as soon as their symptoms began, the local risk of infection would have been reduced by 56% compared with the average conditions of a 10-day delay between symptom onset and hospital admission. In Shenzhen, the average delay from symptom onset to hospital admission was 3.89 days, but there is great room for improvement.
Work stoppages and school closures can reduce the largest source of cross infection outside of homes. Because the COVID-19 outbreak in Shenzhen was around the Chinese New Year holiday (from 24 January to 2 February), work stoppages and school closures only influenced the spread of infection after 2 February. The impact of work stoppages and school closures was therefore not significant because there were few local infected cases after 2 February. If there had been no Chinese New Year holiday, school closures and work stoppages would have been very useful to reduce the risk of infection. Starting school closures and work stoppages too early is ineffective. If they had been implemented after 22 January, 69% of infections could have been avoided compared with using no intervention strategy.
In our simulation of Shenzhen, if we randomly removed temperature detection at 50% of public places, the infection risk only increased by 2%. Active people who frequently move during the day are highly likely to be recorded by temperature detection programmes, with a probability in which n is the number of public places where an individual has been. A susceptible person experiences the highest exposure risk of respiratory infection when he or she is in close proximity with an infected person. Wearing facial masks is necessary to beat COVID-19 [49]. If there had been no other intervention strategy, 67% of infections could have been avoided if 100% of people had worn a mask outside the home after 22 January. However, the Shenzhen government had appealed to all residents to stay at home after 24 January. Most companies and all schools were closed because of the Chinese New Year and governmental policies. The efficiency gain in infection reduction by mask wearing was therefore smaller than it would have been under the uncontrolled condition, and could only reduce the risk of infection by 18%.
All intervention strategies in the second phase are intended to decrease the number of contacted individuals, reduce close contact risks, and shorten the effective infectious period of infected patients. Many national governments have implemented these intervention strategies, such as cancelling or postponing large public events, encouraging people to stay at home, and teaching and learning online [40,50]. In Shenzhen, the best time to implement these intervention strategies was found to be between 15 January and 22 January. Regardless of impacts from other intervention strategies, if only one of various strategies had been implemented by 22 January (or 15 January), 67% (72%) of infections could have been avoided by mask wearing, 65% (68%) by temperature detection in all public places, and 69% (74%) by school closures/work stoppages. There would have been almost no additional risk reduction if all of these intervention strategies had been implemented before 15 January.
4.3. Limitations
There are some limitations in this study. We assumed that the infection is only transmitted by close contact route, which means that long-range airborne and distant fomite routes do not take effect [51]. The time-variant parameters (listed in Table C2) were assumed based on the local policies, and it would bring errors because the human behavior may not conform to assumptions. However, we analysed the sensitivity of all parameters to show their impacts on infection spread (Appendix F). In addition, not all geographic data were extracted from the real distribution. Moreover, we have ignored exposure in public transports since previous literature showed that the infection risk on local public transports is very small [9]. In the simulation, we only considered the mentioned interventions, other interventions such as contact tracing and nucleic acid testing were not considered. All limitations mentioned above will bring little errors to the simulation result. Similar models could be built to examine contact-borne, food/water-borne, and vector-borne diseases. In addition, the limitations in this study should be addressed in future research to improve the accuracy and reliability of the simulation.
5. Conclusions
In this study, we analysed the efficiency of seven intervention strategies (delay from symptom onset to hospital admission, temperature detection in public places, screening for incoming individuals, coverage ratio of mask wearing, mandatory quarantine for arrivals from Hubei province, school closure and work stoppage, and probability of symptom patients staying at home) by simulation based on agent-based SEIIR model. Most population and building data were real (from census and governmental report), and simulation parameters were set based on local governmental policies. We found that shortening the duration from symptom onset to hospital admission and quarantining arrivals from Hubei province are most critical interventions to Shenzhen, while quarantining arrivals from high-risk countries as early as possible, stop working and schooling, and mask wearing are the most effective intervention strategies to other countries. The ideal time window for a mandatory quarantine of arrivals from Hubei Province was between 10 January and January 17, 2020, while the ideal time window for local intervention strategies was between 15 and 22 January. Our results may be useful for other cities when choosing their intervention strategies to prevent outbreaks of COVID-19.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
We are grateful to Professor Ying Long of Tsinghua University for recommending Baidu Map Insight ® to the team. We are also grateful to Baidu Map Insight ® for making their data on inter-city migration available to us. This work was supported by a Collaborative Research Fund (grant number C7025-16G) provided by the Research Grants Council of Hong Kong and an HKU ZIRI seed fund (grant number 04004).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.buildenv.2020.107106.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Li Q., Guan X.H., Wu P., Wang X.Y., Zhou L., Tong Y.Q. Early transmission dynamics in Wuhan, China, of novel noronavirus infected pneumonia. N. Engl. J. Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO, World Health Organization Coronavirus disease 2019 (COVID-19) situation report-71. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200331-sitrep-71-covid-19.pdf?sfvrsn=4360e92b_8 Available from:
- 3.China C.D.C., Chinese Center for Disease Control and Prevention Distribution of COVID-19 pneumonia. 2020. http://2019ncov.chinacdc.cn/2019-nCoV/ Available from: [DOI] [PMC free article] [PubMed]
- 4.Shenzhen Municipal Health Commission Detailed list of case report of confirmed cases of COVID-19 in Shenzhen. 2020. http://m.bendibao.com/mip/827675.html Available from:
- 5.Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob. Health. 2020;8:e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peng L.G., Yang W.Y., Zhang D.Y., Zhuge C.J., Hong L. Epidemic analysis of COVID-19 in China by dynamical modeling. https://arxiv.org/abs/2002.06563 arXiv preprint arXiv:2002.06563 [Preprint]. 2020 [cited 2020 March 1]. Available from:
- 7.Hu Z.X., Ge Q.Y., Li S.D., Jin L., Xiong M.M. Artificial intelligence forecasting of Covid-19 in China. https://arxiv.org/abs/2002.07112 arXiv:2002.07112 [Preprint]. 2020 [cited 2020 March 1]. Available from:
- 8.Zhu X.L., Zhang A.Y., Xu S., Jia P.F., Tan X.Y., Tian J.Q. Spatially explicit modeling of 2019-nCoV epidemic trend based on mobile phone data in mainland China. https://www.medrxiv.org/content/10.1101/2020.02.09.20021360v2 medRxiv [Preprint]. 2020 [cited 2020 February 26]. Available from:
- 9.Zhang N., Huang H., Su B., Ma X., Li Y. A human behavior integrated hierarchical model of airborne disease transmission in a large city. Build. Environ. 2018;127:211–220. doi: 10.1016/j.buildenv.2017.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loomis J., Bond C., Harpman D. The potential of agent-based modelling for performing economic analysis of adaptive natural resource management. J. Nat. Resour. Pol. Res. 2008;1:35–48. [Google Scholar]
- 11.Segovia-Juarez J.L., Ganguli S., Kirschner D. Identifying control mechanisms of granuloma formation during M. tuberculosis infection using an agent-based model. J. Theor. Biol. 2004;231:357–376. doi: 10.1016/j.jtbi.2004.06.031. [DOI] [PubMed] [Google Scholar]
- 12.Zhang N., Huang H., Duarte M., Zhang J.F. Dynamic population flow based risk analysis of infectious disease propagation in a metropolis. Environ. Int. 2016;94:369–379. doi: 10.1016/j.envint.2016.03.038. [DOI] [PubMed] [Google Scholar]
- 13.Zhang N., Zhao P., Li Y.G. Increased infection severity in downstream cities in infectious disease transmission and tourists surveillance analysis. J. Theor. Biol. 2019;470:20–29. doi: 10.1016/j.jtbi.2019.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong W.Y., Jiang R.R., Yang C.Y., Zhang F.F., Su M., Liao Q. Establishing an ecological vulnerability assessment indicator system for spatial recognition and management of ecologically vulnerable areas in highly urbanized regions: a case study of Shenzhen, China. Ecol. Indicat. 2016;69:540–547. [Google Scholar]
- 15.Statistics Bureau of Shenzhen Municipality . Chinese Statistics Press; 2019. Survey Office of the National Bureau of Statistics in Shenzhen, Shenzhen Statistical Yearbook of 2019. ([Beijing]) [Google Scholar]
- 16.Shenzhen Municipal Government School information catalogue. http://www.sz.gov.cn/school/ssxx/ Available from:
- 17.Shenzhen Municipal Government Hospital information catalogue. http://www.sz.gov.cn/hospital/ Available from:
- 18.Yingshang big data center. http://www.winshang.com/winshangdata/index.aspx Available from:
- 19.Shenzhen Education Bureau Notice on winter vacation for primary school, middle school, and kindergarten in 2020. http://szeb.sz.gov.cn/jyfw/fwxsjz/ywjy/tzgg/201912/t20191223_18945630.htm Available from:
- 20.Shenzhen Education Bureau . 2020. Notice of Shenzhen Education Bureau on Printing “Work Plan on COVID-19 Infection Prevention and Control of Shenzhen Education System”.http://szeb.sz.gov.cn/xxgk/flzy/wjtz/202001/t20200122_18991422.htm Available from: [Google Scholar]
- 21.Shenzhen, Shenzhen Center for Disease Control and Prevention Need to strengthen infection prevention and control in communities. 2020. http://www.sznews.com/news/content/2020-01/26/content_22805531.htm Available from:
- 22.Commercial Bureau of Shenzhen Municipality “Five measures” of Commercial Bureau of Shenzhen Municipality for strengthening COVID-19 infection prevention and control and ensuring stable supply. 2020. http://www.sz.gov.cn/stztgs/sztztgs/xxgk/qt/gzdt_1/202001/t20200131_18994178.htm Available from:
- 23.Housing Shenzhen, Construction Bureau Housing enterprises cannot start returning work without authorization. 2020. http://finance.china.com.cn/news/20200206/5187190.shtml Available from:
- 24.Wang T. Shenzhen has allocated 25.3 million Chinese Yuan for COVID-19 infection prevention and control. 2020. https://m.sohu.com/a/369418180_161795/ Available from:
- 25.Yu H.R. People from epidemic area need to be quarantined for 14 days. 2020. http://sztqb.sznews.com/PC/content/202002/03/content_815082.html Available from:
- 26.Pengpai News Shenzhen government deployed works on COVID-19 infection prevention and control. 2020. https://www.thepaper.cn/newsDetail_forward_5591398 Available from:
- 27.Stehlé J., Voirin N., Barrat A., Cattuto C., Colizza V., Isella L. Simulation of an SEIR infectious disease model on the dynamic contact network of conference attendees. BMC Med. 2011;9(1):87. doi: 10.1186/1741-7015-9-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang Z., Zeng Z., Wang K., Wong S.S., Liang W., Zanin M. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. J. Thorac. Dis. 2020;12(3):165–174. doi: 10.21037/jtd.2020.02.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hou C., Chen J., Zhou Y., Hua L., Yuan J., He S. The effectiveness of quarantine of Wuhan city against the Corona Virus Disease 2019 (COVID‐19): a well‐mixed SEIR model analysis. J. Med. Virol. 2020 doi: 10.1002/jmv.25827. [DOI] [PubMed] [Google Scholar]
- 30.Liu T., Hu J.X., Kang M., Lin L.F., Zhong H.J., Xiao J.P. Transmission dynamics of 2019 novel coronavirus (2019-nCoV), Preprints with the Lancet. 2019. [Preprint]. 2020 [cited 2020 March 1]. Available from: [DOI]
- 31.Tindale L., Coombe M., Stockdale J.E., Garlock E., Lau W.Y.V., Saraswat M. Transmission interval estimates suggest pre-symptomatic spread of COVID-19. https://www.medrxiv.org/content/10.1101/2020.03.03.20029983v1 medRxiv [Preprint]. 2020 [cited March 15]. Available from:
- 32.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020;1009:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. J. Am. Med. Assoc. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 34.Chen W., Zhang N., Wei J., Yen H.L., Li Y. Short-range airborne route dominates exposure of respiratory infection during close contact. Build. Environ. 2020;176:106859. [Google Scholar]
- 35.Zhang N., Su B., Chan P.T., Miao T., Wang P.H., Li Y.G. Infection spread and high-resolution detection of close contact behaviors. Int. J. Environ. Res. Publ. Health. 2020;17:1445. doi: 10.3390/ijerph17041445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang N., Tang J.W., Li Y.G. Human behavior during close contact in a graduate student office. Indoor Air. 2019;29:577–590. doi: 10.1111/ina.12554. [DOI] [PubMed] [Google Scholar]
- 37.Stehlé J., Voirin N., Barrat A., Cattuto C., Isella L., Pinton J.F. High-resolution measurements of face-to-face contact patterns in a primary school. PloS One. 2011;6 doi: 10.1371/journal.pone.0023176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferguson N.M., Cummings D.A.T., Cauchemez S., Fraser C., Riley S., Meeyai A. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature (Lond.) 2005;437:209–214. doi: 10.1038/nature04017. [DOI] [PubMed] [Google Scholar]
- 39.Phelan A.L., Katz R., Gostin L.O. The novel coronavirus originating in Wuhan, China: challenges for global health governance. J. Am. Med. Assoc. 2020;323:709–710. doi: 10.1001/jama.2020.1097. [DOI] [PubMed] [Google Scholar]
- 40.Chen S.M., Yang J.T., Yang W.Z., Wang C., Bärnighausen T. COVID-19 control in China during mass population movements at New Year. Lancet. 2020;395:764–766. doi: 10.1016/S0140-6736(20)30421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilder-Smith A., Chiew C.J., Lee V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spiteri G., Fielding J., Diercke M., Campese C., Enouf V., Gaymard A. First cases of coronavirus disease 2019 (COVID-19) in the WHO European region, 24 january to 21 february 2020. Euro Surveill. 2020;25:2000178. doi: 10.2807/1560-7917.ES.2020.25.9.2000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chinazzi M., Davis J.T., Ajelli M., Gioannini C., Litvinova M., Merler S. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368:395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.US CDC, Centers for Disease Control and Prevention Update: public health response to the coronavirus disease 2019 outbreak—United States. 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6908e1.htm?s_cid%3Dmm6908e1_e%26deliveryName%3DUSCDC_921-DM20815 Available from:
- 46.Quilty B.J., Clifford S., CMMID nCoV working group2. Flasche S., Eggo R.M. Effectiveness of airport screening at detecting travellers infected with novel coronavirus (2019-nCoV) Euro Surveill. 2020;25(5) doi: 10.2807/1560-7917.ES.2020.25.5.2000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020 doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aleta A., Hu Q.T., Ye J.C., Ji P., Moreno Y. A data-driven assessment of early travel restrictions related to the spreading of the novel COVID-19 within mainland China. https://www.medrxiv.org/content/10.1101/2020.03.05.20031740v2 medRxiv [Preprint]. 2020 [cited 2020 March 15]. Available from: [DOI] [PMC free article] [PubMed]
- 49.Zhai J. Facial mask: a necessity to beat COVID-19. Build. Environ. 2020;175:106827. doi: 10.1016/j.buildenv.2020.106827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fauci A.S., Lane H.C., Redfield R.R. Covid-19—navigating the uncharted. N. Engl. J. Med. 2020;382:1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang N., Chen W., Chan P.T., Yen H., Tang J.W., Li Y. Close contact behaviour in indoor environment and transmission of respiratory infection. Indoor Air. 2020 doi: 10.1111/ina.12673. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.