Abstract
Atlantoaxial rotatory subluxation (AARS) is the loss of normal alignment and stability of the first (atlas) and second (axis) cervical vertebrae with respect to each other. We describe the clinical challenges of managing a 10-year-old boy who presented with repetitive episodes of torticollis. Open-mouth odontoid radiograph and computed tomographic (CT) scan gave a diagnosis in ARRS, based on its characteristic imaging findings. The child was admitted multiple times for continuous halter traction in the first 6 months after symptom onset. He also experienced a temporary complication from an overcorrection with correcting neck bracing. Seven months after symptom onset, this case was discussed by a multidisciplinary spine team and referred to chiropractic clinic. Despite persistent radiographic evidence of atlantoaxial instability, after 5 months of chiropractic treatment, the child was asymptomatic with nearly full range of neck movement. He also weaned off acetaminophen he had been taking over the past year. Incidentally, bilateral gynecomastia was discovered at the surveillance after treatment. The incidental finding of innocent gynecomastia, even if common in preteen boys, brings up the topic of acetaminophen’s effects on the regulation of sex hormones that was previously overlooked.
Keywords: Acetaminophen, atlantoaxial subluxation, chiropractic, estrogenic effects, gynecomastia
Introduction
Atlantoaxial (C1C2) subluxation is extremely rare in individuals with no predisposing factors.1 Following a minor trauma, the development of cervical instability is more likely in children because of increased ligamentous laxity related to estrogen function.2 Infectious and some inflammatory processes are also considered as underlying, precipitating causes.3 There are several ways in which a subluxation can present, including anteroposterior, rotatory, vertical, and lateral subluxations. Rotatory subluxation is often missed in the emergency medical setting in patients presenting with neck pain and torticollis. Because the transverse ligament of the atlas remains intact an open-mouth radiograph typically shows deviation of the odontoid process with slippage of the C1 on the C2. Treatment involved neck traction, collar immobilization and anti-inflammatory medications.4 In cases of AARS with a delayed diagnosis, the subluxation can become fixation of the joint. Persistent torticollis, neurological compromise and even life-threatening results may be seen as a result of AARS.5 The most important factor for success of conservative treatment is early diagnosis and the timing of treatment.3
Case Report
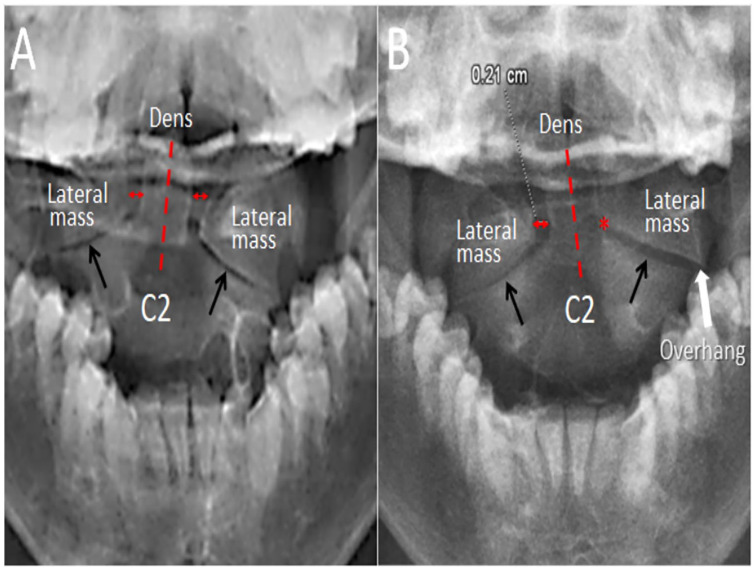
A 10-year-old boy woke up with painfully torticollis locking his head in right rotation. There were no prior traumatic or infectious events. His family doctor, at first, gave him a tentative diagnosis of acute torticollis and prescribed some nonopioid analgesics (acetaminophen). After 2 weeks of unsuccessful treatment, the child was referred to local hospital for an orthopedic assessment. Open-mouth odontoid radiograph (Figure 1A) revealed unequal spacing of lateral atlantodental intervals and the C1 lateral masses, consistent with atlantoaxial rotatory subluxation. Halter neck traction with 5 lbs weight on an inclined bed following procedural sedation with Ketamine was promptly utilized to restore correct atlantoaxial alignment. Reposition of the subluxated joint was achieved after 3 weeks of continuous halter traction, and the patient was discharged without symptoms or locked positioning of the neck. Philadelphia collar and oral analgesics were prescribed after discharge.
Figure 1.
Initial (A) and 12-month (B) open-mouth radiographs in a boy with a lateral and rotatory atlantoaxial subluxation. There was narrowing of the atlantoaxial joints (black arrows), lateral displacement of the C2 with respect to the overhang of C1 lateral mass (white arrow), and asymmetry of the lateral atlantodental intervals, indicating rotatory displacement of the atlantoaxial joint.
Two weeks after discharge, the painful torticollis continued. Cervical range of motion (ROM) was limited to 40° left rotation and 20° right rotation. Follow-up dynamic computed tomographic (CT) scan showed recurrence of the C1/C2 subluxation in left rotation. Halter traction and analgesics were repeated. Four weeks later, a follow-up radiograph showed significant improvement. Halo gravity traction and full-time use of a Philadelphia collar to prevent the head and neck movement were utilized after discharge from hospital.
The child was transferred to children’s hospital following a third recurrence of painful torticollis with confirmed C1/C2 subluxation 2½ months after initial onset of symptoms. Cervical ROM was 70° and 60°, left and right rotation, respectively. C1/C2 reduction was achieved after 2 weeks of continuous halter traction. He was discharged home with a neck collar, but shortly afterward his torticollis recurred in a left-ward position. The patient was then prescribed halo gravity traction combined with a correcting neck brace, rotating the neck 30° to the right, in an effort to correct the locked positioning and bring neck alignment to a neutral position. However, his neck was overcorrected and locked after 6 weeks of the regimen. The patient was readmitted to the hospital. At admittance, cervical rotation was limited 20° and 50°, left and right, respectively. Correcting bracing was discontinued and the joint was realigned within 4 days of halter neck traction with 7 lbs, although the head still rotated slightly to the right. The patient maintained use of a rigid cervical collar for stabilization after discharge.
The child was brought in by a family member for a consultation with our multidisciplinary spine team 1 month following discharge from his fourth hospital stay and referred for chiropractic care. At the time of initial consultation, the patient had severe neck pain, and the neck was stuck in right rotation without any neurological complaints. Computed tomography of the neck (Figure 2) displayed eccentric positioning of the dens at C1 level, and evidences of incomplete ossification of the synchondroses. Given the repetitive nature of this patient’s atlantoaxial subluxations and successful reductions, unstable AARS was considered. Multimodal chiropractic treatment comprised intermittent motorized traction (Spine Decompression Device, MID 4M Series, WIZ Medical, Korea) focused on C1/C2, thermal ultrasound therapy, spinal adjustment, stretching exercise, and pain medications, applied 3 times a week for 4 weeks. After 4 weeks of treatment, patient’s pain was significantly relieved. Cervical mobility restored by 70% and the collar was discontinued. Subsequently, treatment sessions were scheduled twice weekly for the following 4 months. His pain medication (acetaminophen) was gradually reduced and tapered off near the end of treatment. He had no neurological sequelae before or after the treatments. At posttreatment surveillance, the patient was asymptomatic with nearly full cervical ROM, despite persistent radiographic evidence of C1C2 instability (Figure 1B). Bilateral gynecomastia was incidentally discovered, with no pain or complaints (Figure 3).
Figure 2.
Seven months after symptom onset of atlantoaxial subluxation. Axial (A) and reconstructed (B) CT images displayed eccentric positioning of the dens at C1 level. Coronal slice (C) showed cartilaginous structures in both the apical and the subdental synchondroses. Small spur formation noted. Sagittal slice (D) demonstrated a gap in the dens in addition to the cartilaginous structures remained in the ossification centers (white arrows). The pediatric patterns of the vertebral structure placed the atlantoaxial joint at a significant risk of instability.
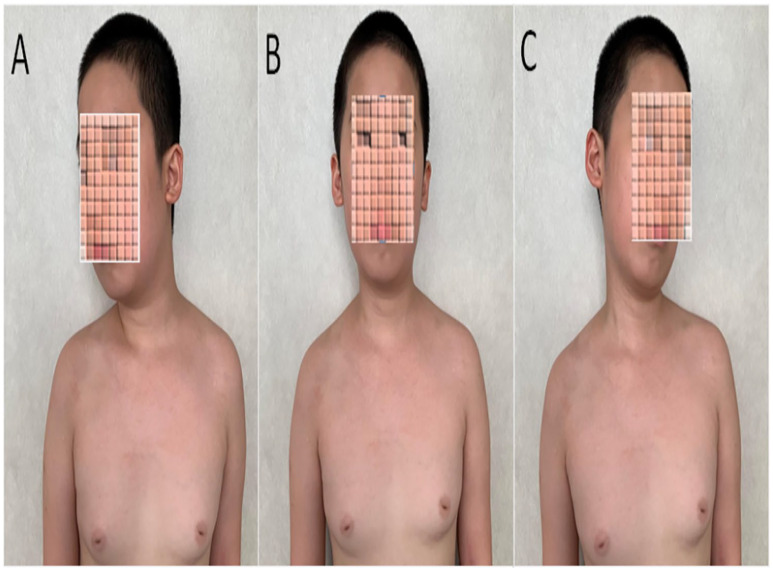
Figure 3.
Head position and neck rotation after treatment were restored in a 10-year-old boy with chronic atlantoaxial subluxation. Temporary gynecomastia is usually physiological in preteen boys and an unrelated finding to atlantoaxial subluxation. However, sulfation is a principal catabolic pathway of sex hormones. Long-term acetaminophen use can increase the bioavailability of estradiol by decreasing estradiol sulfation. Much of these relationships, as in this case, remain unconfirmed.
Discussion
Atlantoaxial subluxation is defined by a loss of stability between the atlas and axis (C1/C2) joint because of ligamentous laxity or osseous abnormalities.3 The C1 and C2 form a unique set of articulation responsible for 60% of total rotation in the craniocervical region. The hallmark structure of the C2 vertebra is its odontoid process (the dens), which is embryologically the body of the C1. The apical dental segment does not become fused to the basal dens till 6 to 9 years of age, and fully formed by age 12.6,7 The dens serves as the principal attachment point for stabilizing the articulation.6 Stabilization of this joint is primarily by the transverse ligament which holds the dens to the anterior arch of the C1. The tip of the dens is also connected to the occipital condyles by the paired alar ligaments to prevent anterior shift as well as excessive rotation. The cervical spine in children is hypermobile compared with that in adults as ligamentous laxity, robust synovia, and malleable (cartilaginous) features of the pediatric vertebrae allow greater joint mobility. As a result, non-traumatic C1 C2 instability occurs almost exclusively during childhood.8 Correlation between chronological age, cervical vertebral morphology, and different stages of bone maturation is important in clinical practice.
Cervical radiographs continue to be an effective method for identifying C1C2 subluxation.9 On an open-mouth view, the asymmetry of the interspaces between the C1 lateral masses and the dens is sufficient to make a diagnosis.5 Alternative techniques for imaging in cases of torticollis, such as CT and magnetic resonance imaging, are sensitive in ruling out traumatic or destructive processes10 and are recommended when neurological signs and symptoms are present.9 In general, the appropriate approach to a child presenting with acute torticollis is to first identify potential red flags, which may require emergency intervention. It is also necessary to rule out trauma, as well as the destructive process of neoplastic or inflammatory in nature. Second is to estimate the demand for cervical traction and prevent pathologic transition to chronic joint fixation in those with true AARS.
Treatment regimen is correlated to the severity and type of the C1C2 instability in addition to the maturational stage of the child. Conservative treatments are encouraged to start right away. If left untreated, some cases may resolve spontaneously, but other cases may cause secondary morbidities ranging from neck restriction, permanent torticollis, facial asymmetry, and even sudden death.3,5 Cervical collar and halter traction are routinely used for patients diagnosed with AARS.10 It is necessary to exclude all contraindications related to upper cervical instability prior to proceeding with manual therapy. Chiropractic approach aims to provide therapy for tight musculature, joint mobilizations for pain relief, and strengthening exercises for stabilization.11 Acetaminophen and anti-inflammatory drugs are often used to relieve pain but there are no pharmacologic interventions for atlantoaxial instability. Patients with risk of mechanical and neurological instability need stabilization by posterior atlantoaxial arthrodesis.
Gynecomastia is common in preteen boys due to temporary hormonal imbalance. It is also imperative to be aware that acetaminophen use can bring on estrogen effects by reducing the catabolism of estrogen. Acetaminophen (brand names Tylenol, Panadol, and Paracetamol) is often prescribed to treat fever, arthritis, and musculoskeletal pain. Recent researches show that the use of acetaminophen has overlooked effects on the regulation of sex hormones.12,13 Sulfation (sulfate conjugation), catalyzed by sulfotransferase enzymes (SULTs), is an important pathway of metabolism for sex hormones. As both acetaminophen and estrogens are metabolized by SULT, acetaminophen acts as competitive inhibitors for sulfation of estrogens.14 Thus, the catabolism of estrogen is modified and the bioavailability of estradiol (the most potent circulating estrogen) increases. In a mice model, prenatal exposure of acetaminophen altered the masculinization of male brain and behavior.11 The incidental finding of innocent gynecomastia in our case may shed light on estrogenic effects of acetaminophen that have received little attention in clinical practice. Much of these relationships, as in this referral case, remain unconfirmed. The present study is limited by the retrospective nature of the data available. Moreover, the small sample size affects the power and significance of the findings. Further studies are warranted before conclusions can be drawn.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ Contribution: Dr. Chu contributed the case information and drafted the manuscript. Dr. Lo edited the article. The article took form under Dr. Bhaumik’s guidance. All the authors have read and approved the final manuscript.
Informed Consent: The patient’s guardian provided written informed consent for publication of this case report and any accompanying images.
ORCID iD: Eric Chun Pu Chu  https://orcid.org/0000-0002-0893-556X
https://orcid.org/0000-0002-0893-556X
References
- 1. Lacy J, Gillis CC. Atlantoaxial Instability. Treasure Island, FL: StatPearls Publishing; 2019. https://www.ncbi.nlm.nih.gov/books/NBK519563/. [PubMed] [Google Scholar]
- 2. Karski J, Matuszewski Ł, Jakubowski P, Karska K, Kandzierski G. Clavicle fracture associated with atlantoaxial rotatory displacement, type II in an 8-year-old girl. Medicine. 2017;96:e8781. doi: 10.1097/MD.0000000000008781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Neal KM, Mohamed AS. Atlantoaxial rotatory subluxation in children. J Am Acad Orthop Surg. 2015;23:382-392. [DOI] [PubMed] [Google Scholar]
- 4. Kuppermann N. Neck stiffness. In: Fleisher GR, Ludwig S, Silverman BK, eds. Synopsis of Pediatric Emergency Medicine. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002:151. [Google Scholar]
- 5. Çiftdemir M, Copuroğlu C, Ozcan M, Ulusam AO, Yalnız E. Non-operative treatment in children and adolescents with atlantoaxial rotatory subluxation. Balkan Med J. 2012;29:277-280. doi: 10.5152/balkanmedj.2012.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kaiser JT, Lugo-Pico JG. Anatomy, Head and Neck, Cervical Vertebrae. Treasure Island, FL: StatPearls Publishing; 2019. https://www.ncbi.nlm.nih.gov/books/NBK539734/. [PubMed] [Google Scholar]
- 7. O’Brien WT, Shen P, Lee P. The dens: normal development, developmental variants and anomalies, and traumatic injuries. J Clin Imaging Sci. 2015;5:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Powell EC, Leonard JR, Olsen CS, Jaffe DM, Anders J, Leonard JC. Atlantoaxial rotatory subluxation in children. Pediatr Emerg Care. 2017;33:86-91. doi: 10.1097/PEC.0000000000001023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cunningham S. Upper cervical instability associated with rheumatoid arthritis: a case report. J Man Manip Ther. 2016;24:151-157. doi: 10.1179/2042618614Y.0000000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gubin A. General description of pediatric acute wryneck condition. In: Chung KJ, ed. Spine Surgery. London, England: IntechOpen; 2012:121-134. http://www.intechopen.com [Google Scholar]
- 11. Marchand AA, Wong JJ. Conservative management of idiopathic anterior atlantoaxial subluxation without neurological deficits in an 83-year-old female: a case report. J Can Chiropr Assoc. 2014;58:76-84. [PMC free article] [PubMed] [Google Scholar]
- 12. Hay-Schmidt A, Finkielman OTE, Jensen BAH, et al. Prenatal exposure to paracetamol/acetaminophen and precursor aniline impairs masculinisation of male brain and behaviour. Reproduction. 2017;154:145-152. [DOI] [PubMed] [Google Scholar]
- 13. Cohen IV, Cirulli ET, Mitchell MW, et al. Acetaminophen (Paracetamol) use modifies the sulfation of sex hormones. EBioMedicine. 2018;28:316-323. doi: 10.1016/j.ebiom.2018.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shenfield GM. Oral contraceptives. Are drug interactions of clinical significance? Drug Saf. 1993;9:21-37. doi: 10.2165/00002018-199309010-00003. [DOI] [PubMed] [Google Scholar]