Abstract
As the number of Coronavirus Disease (2019) (COVID-19) cases increase globally, countries are taking more aggressive preventive measures against this pandemic. Transmission routes of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) include droplet and contact transmissions. There are also evidence of transmission through aerosol generating procedures (AGP) in specific circumstances and settings. Institutionalized populations without mobility and living in close proximity with unavoidable contact are especially vulnerable to higher risks of COVID-19 infection, such as the elderly in nursing homes, children in orphanages, and inmates in prisons. In these places, higher prevention and control measures are needed. In this study, we proposed prevention and control strategies for these facilities and provided practical guidance for general measures, health management, personal protection measures, and prevention measures in nursing homes, orphanages, and prisons, respectively.
Keywords: COVID-19, Nursing home, Orphanage, Prison, Prevention, Control
1. Introduction
Coronavirus Disease (COVID-19) was first reported in Wuhan, China (Wuhan Municipal Health Commission, 2019). As of June 30, 2020, the number of confirmed cases exceeded 10.1 million with over 0.5 million mortalities; in particular, in the United States, the number of confirmed cases has all exceeded 2 million, accounting for approximately 25% of total confirmed cases in the globe. The proportions of confirmed cases in Chile (14.8‰), Peru (9.2‰), United States (7.7‰), Brazil (6.4‰), and Spain (5.3‰) have all exceeded 5‰. With the increasing number of COVID-19 cases globally, countries have utilized precautionary measures against this pandemic. Main transmission routes of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) include droplet and contact transmissions. Airborne transmission may be possible in specific circumstances and settings in which aerosol generating procedures (AGP) are performed (World Health Organization, 2020b). The aerosol deposition on the surface and subsequent resuspension could also be a potential transmission route. Additionally, SARS-CoV-2 could remain viable in aerosols for 3 hours and has shown to be viable on various surfaces for a period of time: plastic (72 h), stainless steel (48 h), copper (4 h), and cardboard (24 h) surfaces (van Doremalen et al., 2020).
SARS-CoV-2 can spread quickly in relatively confined spaces, such as nursing homes, orphanages, and prisons. For examples, over 200 infections were reported in a women’s prison in Wuhan, China, the epicenter of the outbreak, 100 m from a local hospital for pulmonary diseases (Yang, 2020). As of April 12, 2020, a total of 306 inmates and 218 staffs in a prison were tested positive for the COVID-19 in Cook County, the United States (Cook County Sheriff’s Office, 2020). In Arkansas, 51 of 280 confirmed COVID-19 cases were found in nursing homes (THV11 Digital, 2020). In Louisiana, at least 61 nursing homes have confirmed COVID-19 cases, totally 261 nursing home residents have tested positive for the virus with 60 deaths (WBRZ, 2020). These are reinforcing evidence that people over the age of 65 are at a higher risk of developing life-threatening complications due to COVID-19. Looking at the transmission characteristics of SARS-CoV-2, the most efficient protection measures are mask use and hand hygiene, according to previous studies on influenza virus and coronavirus (Aiello et al., 2010; Jefferson et al., 2011; Leung et al., 2020). In the globe, it is estimated that 8 million children (Browne, 2017) and 10.74 million inmates (Walmsley, 2018) live in orphanages and prisons, respectively. It was estimated that there are approximately 703 million persons aged 65 years or over in the globe and 2% of them are living in the nursing home (Lloyd-Sherlock et al., 2020; United Nations, 2019). Elderly people, children, and inmates in these facilities are people either with limited mobility or deprived of liberty. They live in close proximity with others thus close contact is unavoidable. Although entrance to these facilities is strictly limited, which could protect them from outside infectious agents, inadequate prevention and control measures taken inside may still exacerbate COVID-19 transmissions from within. The purpose of this study is to illustrate the rationale of prevention and control measures in nursing homes, orphanages, and prisons and provide suggestions for general measures, health management, personal protection measures, and prevention measures in specific facilities.
2. Rationale
2.1. Nursing home
The elderly in nursing homes are vulnerable populations who are at a higher risk of infection and adverse outcome because they usually live in close proximity to others (World Health Organization, 2020a). COVID-19 has an increased mortality in older people and in those with chronic diseases or immunosuppression. In Italy, the mean age of patients dying for COVID-2019 infection was 78.5, which was 15 years higher as compared with the national sample diagnosed with COVID-2019 infection (COVID-19 Surveillance Group, 2020). The lack of knowledge and proper care may make them more vulnerable. Therefore, to protect residents, employees, and visitors, prevention and control measures should be taken in nursing homes to prevent SARS-CoV-2 from entering the facility and spreading inside and outside the facility.
2.2. Orphanage
The COVID-19 outbreak has led to a level of heightened vigilance in the community which involves the extra responsibility of caring for children in need of protection and those who cannot be cared for by their biological parents as an orphanage. Although the confirmed COVID-19 cases in children account for a relatively small proportion at this point, there is evidence that children are also susceptible to COVID-19 infection (Kelvin and Halperin, 2020). Pneumonia is a leading cause of mortality in children, and distinct immunological responses to viral infections might exist in children which can cause severe damage to vital organs (Campbell and Nair, 2015). Recent study suggests that children with COVID-19 are at risk for a Multisystem Inflammatory Syndrome in Children (MIS-C) with cardiovascular manifestations (Beroukhim and Friedman, 2020). In addition, children in orphanages live in congregated and relatively confined environment with limited health protection awareness. Thus, the importance to promote the welfare, protection, and care for children and staffs within the orphanage facility could never be overemphasized.
2.3. Prison
Inmates in prisons and other custodial settings live in close proximity with each other under poor ventilation conditions, thus the risk level of person-to-person transmission through droplet and aerosol transmissions are higher (Kamarulzaman et al., 2016). In addition, inmates generally have a higher number of co-morbid conditions and are in worse health conditions. This is made worse by general poorer hygiene and weaker immune defense due to stress and poorer nutrition (WHO Regional Office for Europe, 2020). Infections can be transmitted between prisoners, staffs, and visitors, between prisons through transfers and staff cross-deployment, to and from the community. Many scholars have appealed for revision of prison guidelines on infection control because most prisoners will eventually be released back into their communities and may further spread infectious diseases (Moazen et al., 2019). Moreover, during COVID-19 pandemic, the COVID-19 clusters in this setting have the potential to overwhelm prison health-care services (Kinner et al., 2020).
3. Prevention and control measures
In order to timely respond to COVID-19 pandemic for nursing homes, orphanages, and prisons, it is recommended to enhance risk control, strengthen daily prevention and control measures such as personnel protection, environmental cleaning, and disinfection.
3.1. Health management measures
The nursing homes, orphanages, and prisons should establish the prevention and control system and develop emergency plans during COVID-19 pandemic. The establishment of health monitoring is helpful in early detection of COVID-19 cases, especially those with mild symptoms (Heymann and Shindo, 2020). Close management should be adopted during the COVID-19 pandemic, and personnel in and out, especially visits, should be reduced. Since as high as 60% of all infections were converted from cases with mild symptom or asymptotic cases, admission health screening should be carried out to mitigate asymptomatic transmission (Qiu, 2020). It is also suggested to set isolation observation area in each facility for people who develop symptoms. In particular, people who are new to nursing homes, orphanages, and prisons should be isolated for at least 14 days. Similarly, children or the elderly who leave or relocate from facilities, as well as people who are released from prisons should be isolated for 14 days. For facilities providing shuttles for workers, measurement of body temperature should be carried out before getting on. People with suspected symptoms of fever, cough, sneezing should not be allowed to enter these facilities. Since the control of COVID-19 needs at least a couple of months, the preparation of sufficient protection products (masks, disinfectants, gloves, etc.) is highly recommended. Meanwhile, distribution priority of medical supplies should be given to healthcare workers providing care services (e.g. front-line healthcare workers, nursing staff in institutions, and healthcare personnel in private clinics); personnel who provide essential services and who are required to have contact with the public at work (e.g. those providing public transport, emergency services and immigration services); and marginalized and vulnerable groups in the society (e.g. unaccompanied children, elderly people without family support, and disabled persons). Health education should also be carried out to increase the protection awareness via training, posters, videos, etc. During the COVID-19 pandemic, nursing homes, orphanages, and prisons should provide psychological consulting services to the elderly, children, inmates, and workers to mitigate probable negative emotions such as anxiety and panic under the stress.
3.2. General measures
3.2.1. Basic hygiene measures
Ventilation is one of the most effective measures to significantly reduce the exposure to infectious diseases (Zhai, 2020). Therefore, the ventilation during COVID-19 should be strengthened. Under the prerequisite of thermal comfort, natural ventilation is preferred. It is recommended to open the window 2 or more times a day with duration of 0.5 h. For facilities using air conditioners for ventilation and indoor temperature adjustment, it is suggested to regularly clean and disinfect the air inlet and outlet of the air conditioner using chlorine containing disinfectant with available chlorine content of 500mg/L and strengthen the cleaning and disinfection of the condensate pan and cooling water of the fan coil unit. The operation of hand washing facilities should be maintained regularly. Also, the wastes should be classified before disposal and the disinfection frequency of waste containers could be increased. Spraying or wiping disinfections using chlorine containing disinfectant with available chlorine content of 500 mg/L are recommended. In addition, since SARS-CoV-2 may spread through contaminated waste surfaces and aerosols from wastewater systems, it is necessary to assess disease prevalence and spread by monitoring the viral RNA in wastewater for early warning of COVID-19 outbreaks (Nghiem et al., 2020).
3.2.2. Object surface cleaning and disinfection
Indoor and outdoor environment of facilities should be kept clean and hygienic, daily cleaning and disinfection measures should be recorded. The floor could be kept clean using chlorine containing disinfectant with available chlorine content of 250–500 mg/L. Vomitus could be covered and disinfected using disposal water absorbing materials and adequate disinfectant or effective disinfection towel. After removal of vomitus, the object surface should be disinfected using quaternary ammonium salt disinfectant or chlorine containing disinfectant.
3.2.3. Prevention measures in functional places
The restroom should be kept clean and dry, in addition, ideal ventilation and disinfection frequency should be adjusted according to actual situation. The sink, shower, and other drainage pipes should be frequently checked to ensure the effect of water seal of U-shaped pipe and sewer. The surface of public table, sink, door handle, and other objects should be disinfected using chlorine containing disinfectant with available chlorine content of 500 mg/L. After then, wipe the surface with clean water 30 minutes after spraying or wiping disinfection. Gatherings (leisure activity, having meal, workout, etc.) should be reduced and the personnel density should be well controlled (Bedford et al., 2020). The dining room in use as well as used kitchen utensils should be disinfected after each meal. Food debris must be removed before the disinfection of tableware because the presence of organic matters would weaken the disinfection performance. It is recommended to disinfect the kitchen utensils via boiling or steam for 15 min, disinfection cabinet, or soaking in chlorine containing disinfectant with available chlorine content of 250 mg/L, and wash completely after disinfect.
3.3. Personal protection measures
In congregated places, people are encouraged to correctly wear the mask and enhance hand hygiene simultaneously. To stop the spread of SARS-CoV-2, it is recommended to avoid large gatherings, direct contact with public facilities or public objects, and maintain a distance of at least 3 feet from other people (Fiorino et al., 2020). Avoid touching face with hands or gloves to minimize spread of SARS-CoV-2 and other pathogens. When cough or sneezing, people are suggested to cover their mouth and nose using the napkin or elbow, and wash hands completely using soap or liquid soap after throwing the used napkin into the dustbin. When communicating with others, direct contact without mask should be avoided. Under the condition of sufficient protection products supply, people could consider to use hand sanitizer and keep hands clean all the time. In orphanages, specific masks or face shield should be prepared for children because the use of adult masks might lead to air leak and expose them to infection. The care givers should also rationally guide children to wear the mask or face shield in certain scenarios, such as before eating, before and after playing, after sneezing, etc. The protection of infants is indirect because they are not required to wear the mask, thus the personal protection of care givers must be strengthened.
3.4. Specific measures
3.4.1. Nursing home
Once COVID-19 case is found in a nursing home, the confirmed case and suspected case (if any) should be immediately isolated from others. Before entering the isolation area, cases should change their clothes throughout. The healthcare workers should adopt proper personal protection measures. Unnecessary personnel in and out should be forbidden in isolation area. Strict disinfection should be carried out for isolation area and contaminated objects as shown in Table 1 .
Table 1.
Disinfection strategy for nursing homes when a COVID-19 case is found.
| Category | Disinfection technology | Disinfectant concentration | Disinfection time | |
|---|---|---|---|---|
| Clothes and bedclothes | Heat and humidity resistant | Boil | – | 15 min |
| Steam | – | 30 min under 121 °C | ||
| Pressure steam | – | 30 min under 121 °C | ||
| Wash after soaking in chlorine containing disinfectant | 1000–2000 mg/L | 2 h | ||
| Heat and humidity sensitive | ethylene oxide disinfection cabinet | – | – | |
| Contaminated objects | Heat and humidity resistant | Boil | – | 15 min |
| Steam | – | 30 min under 121 °C | ||
| Pressure steam | – | 30 min under 121 °C | ||
| Wash after soaking in chlorine containing disinfectant | 1000–2000 mg/L | 2 h | ||
| Heat and humidity sensitive | ethylene oxide disinfection cabinet | – | – | |
| Humidity resistant | Soak in chlorine containing disinfectant or wipe the surface | 1000–2000 mg/L | 30 min | |
| Soak in peracetic acid or wipe the surface | 2000 mg/L | 30 min | ||
| Precision instrument and electrical appliances | Wipe using alcohol or quaternary ammonium salt disinfectant | |||
| Kitchen utensils | Boil | 30 min | ||
| Steam | 30 min | |||
| Wash after soaking in chlorine containing disinfectant | 500 mg/L | |||
| Indoor environment | Surface | Spray disinfection (300 mL/m2) | 1000–2000 mg/L (chlorine containing disinfectant); 2000–5000 mg/L (peracetic acid) |
|
| Air | Fumigation (1 g/m2) | 5000–10,000 mg/L (peracetic acid) | 2 h under relative humidity of 60%–80% | |
3.4.2. Orphanage
Personnel with abnormal body temperature, cough, fatigue, diarrhea, sore throat, or with potential exposure to SARS-CoV-2 should be isolated in temporary isolation area. Confirmed and suspected COVID-19 cases should be sent to designated hospitals for further treatment. The orphanage facility must report the situation to relevant government departments and local CDCs in time. In addition, orphanages should also conduct investigations on close contacts under the guidance of local health departments, a 14-day isolation should also be required for close contacts. Children and staffs who get back from hospital should be isolated for at least 14 days. At the same time, the orphanages need to be thoroughly disinfected, and the personal belongings should be handled properly. All clothes, bedding, sheets, and other textiles should be kept clean and washed regularly. If disinfection treatment is required, steam or boiling for 30 minutes are recommended. It is also feasible to soak with chlorine-containing disinfectants with available chlorine content of 500 mg/L for 30 minutes, followed by routine cleaning (World Health Organization, 2020c). Restrooms, bathrooms, and laundries in orphanages should be disinfected on a daily basis with chlorine-containing disinfectants with available chlorine content of 500 mg/L, then rinsed under running water.
3.4.3. Prison
If a COVID-19 case was found in a prison, it is suggested to immediately organize screening for all inmates and staffs. People with abnormal symptoms (fever, cough, diarrhea etc.) should be recorded and examined via Computed Tomography (CT). Close contacts could be evacuated to other custodial facilities without cases in order to block the transmission routes and reduce the risk of cross infection. Isolation requirements should be strictly implemented and health monitoring should be enhanced to these close contacts. The prison should be divided into case area, isolation area, isolation observation area, and general area. It is also recommended to distribute disposable masks to inmates and staffs, and guide the use and disposal of the mask. The ventilation, regular disinfection, and personal protection measures should be strengthened, and unnecessary personnel in and out should be avoided. It is recommended to provide sufficient soap or liquid soap in order to strengthen hand hygiene. Moreover, if the hand hygiene product supply is limited, 75% Alcohol Hand Sanitizer could also be utilized to clean hands. Terminal disinfection must be provided for the places where COVID-19 cases lived or stayed for relatively long time.
If a COVID-19 cluster was found in a prison, in addition to prevention measures mentioned above, partition management is also recommended. Cases with severe and moderate symptoms should be arranged in case area. Cases with mild symptoms, those who with positive results of pharyngeal swab viral nucleic acid detection but do not have obvious clinical symptoms (such as fever, fatigue, pneumonia, etc.), should be arranged in isolation area. Suspected cases, close contacts, and other people with symptoms of fever, cough, diarrhea, etc. should be arranged in isolation observation area. The rest could stay in general area. From the perspective of security, the partition management for prison staffs and inmates should be separated. Healthcare area of other diseases should be strictly separated with case area, isolation area, isolation observation area, and general area to avoid cross infection. If the prison has limited isolation and medical conditions, it is recommended to transfer confirmed cases and suspected cases to COVID-19 designated hospitals and strengthen the custody during the treatment.
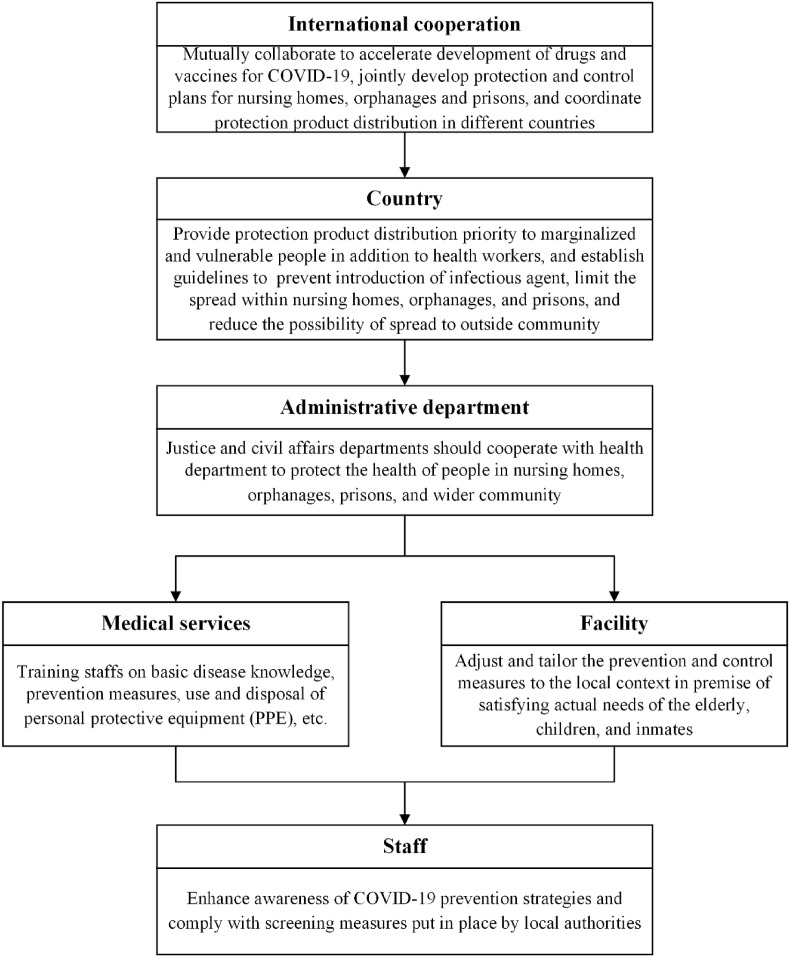
4. Perspectives
The elderly in nursing homes, children in orphanages, and inmates in prisons are marginalized and vulnerable groups in the society. However, they live in congregated and relatively confined environment due to specific management, which significantly increase their risks exposed to COVID-19. Therefore, it is crucial to strictly implement routine cleaning and disinfection measures and publicize health protection knowledge to improve the awareness. The best way to prevent illness is to avoid being exposed to the pathogens which requires all to work together and comply with the rules (Fig. 1 ). Inter-/intra-national cooperation should be encouraged. Each country should establish nationwide prevention and control strategies, and health departments should provide technical support to nursing homes, orphanages, and prisons. Facilities should have sufficient management oversight of practice previously proposed on a daily basis and arrangements in place to ensure proper scrutiny of the well-being of the elderly, children, and inmates. Apart from these, everyone should stay informed and vigilant, and update information from health departments or other official channels in a timely way. On the other hand, social activities and interactions are reduced dramatically during the COVID-19 pandemic, and people in these facilities become much more socially isolated which might cause more psychological harm. Therefore, close attention must be paid to their mental health, especially those who are isolated. Moreover, the health monitoring of people in these facilities should be further improved at national scale. It is recommended to establish an access for nursing homes, orphanages, and prisons in order to directly report outbreak information to the health department.
Fig. 1.
Strategic framework for prevention and control of COVID-19 pandemic.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This work was supported by the National Natural Science Foundation of China [grant number 81903377]. The authors would like to acknowledge all health-care workers involved in the diagnosis and treatment of patients and staffs involved nursing homes, orphanages, and prisons during the pandemic in the globe. We thank Ms. Dan Ye, Ms. Yan Liao, Mr. Xu Yan, Mr. Yujing Zhang and many other staff members at the China CDC for their contributions. The present perspective has not been subjected to the peer and policy review from China CDC, and therefore does not necessarily reflect the views of the China CDC and no official endorsement should be inferred.
References
- Aiello A.E., Murray G.F., Perez V., Coulborn R.M., Davis B.M., Uddin M., Shay D.K., Waterman S.H., Monto A.S. Mask use, hand hygiene, and seasonal influenza-like illness among young adults: a randomized intervention trial. JID (J. Infect. Dis.) 2010;201:491–498. doi: 10.1086/650396. [DOI] [PubMed] [Google Scholar]
- Bedford J., Enria D., Giesecke J., Heymann D.L., Ihekweazu C., Kobinger G., Lane H.C., Memish Z., Oh M.-d., Schuchat A. COVID-19: towards controlling of a pandemic. Lancet. 2020;395:1015–1018. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beroukhim R.S., Friedman K. JACC: Case Reports; 2020. Children at Risk: Multisystem Inflammatory Syndrome and COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne E. nstitute of Development Studies; the United Kingdom: 2017. Children in Care Institutions, K4D Helpdesk Report. [Google Scholar]
- Campbell H., Nair H. Child pneumonia at a time of epidemiological transition. Lancet Glob. Health. 2015;3:e65–e66. doi: 10.1016/S2214-109X(14)70308-0. [DOI] [PubMed] [Google Scholar]
- Cook County Sheriff’s Office . 2020. COVID-19 Cases at CCDOC. [Google Scholar]
- COVID-19 Surveillance Group . Istituto Superiore di Sanità; 2020. Characteristics of COVID-19 Patients Dying in Italy. [Google Scholar]
- THV11 Digital . 2020. 47 Positive COVID-19 Cases at Little Rock Nursing Home, Officials Say. [Google Scholar]
- Fiorino G., Allocca M., Furfaro F., Gilardi D., Zilli A., Radice S., Spinelli A., Danese S. Inflammatory bowel disease care in the COVID-19 pandemic era: the humanitas, milan, experience. J. Crohn’s Colitis. 2020;(jjaa058):1–4. doi: 10.1093/ecco-jcc/jjaa058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann D.L., Shindo N. COVID-19: what is next for public health? Lancet. 2020;395:542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson T., Del Mar C.B., Dooley L., Ferroni E., Al-Ansary L.A., Bawazeer G.A., van Driel M.L., Nair S., Jones M.A., Thorning S., Conly J.M. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst. Rev. 2011 doi: 10.1002/14651858.CD006207.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamarulzaman A., Reid S.E., Schwitters A., Wiessing L., El-Bassel N., Dolan K., Moazen B., Wirtz A.L., Verster A., Altice F.L. Prevention of transmission of HIV, hepatitis B virus, hepatitis C virus, and tuberculosis in prisoners. Lancet. 2016;388:1115–1126. doi: 10.1016/S0140-6736(16)30769-3. [DOI] [PubMed] [Google Scholar]
- Kelvin A.A., Halperin S. 2020. COVID-19 in Children: the Link in the Transmission Chain. The Lancet Infectious Diseases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinner S.A., Young J.T., Snow K., Southalan L., Lopez-Acuña D., Ferreira-Borges C., O’Moore É. Prisons and custodial settings are part of a comprehensive response to COVID-19. Lancet Public Health. 2020;5:e188–e189. doi: 10.1016/S2468-2667(20)30058-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung N.H.L., Chu D.K.W., Shiu E.Y.C., Chan K.-H., McDevitt J.J., Hau B.J.P., Yen H.-L., Li Y., Ip D.K.M., Peiris J.S.M., Seto W.-H., Leung G.M., Milton D.K., Cowling B.J. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020 doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Sherlock P.G., Kalache A., McKee M., Derbyshire J., Geffen L., Casas F.G. WHO must prioritise the needs of older people in its response to the covid-19 pandemic. Br. Med. J. 2020;368 doi: 10.1136/bmj.m1164. [DOI] [PubMed] [Google Scholar]
- Moazen B., Assari S., Neuhann F., Stöver H. The guidelines on infection control in prisons need revising. Lancet. 2019;394:301–302. doi: 10.1016/S0140-6736(19)30279-X. [DOI] [PubMed] [Google Scholar]
- Nghiem L.D., Morgan B., Donner E., Short M.D. The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case Stud. Chem. Environ. Eng. 2020;1 doi: 10.1016/j.cscee.2020.100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J. Covert coronavirus infections could be seeding new outbreaks. Nature. 2020 doi: 10.1038/d41586-020-00822-x. [DOI] [PubMed] [Google Scholar]
- United Nations . Department of Economic and Social Affairs, Population Division; New York: 2019. World Population Ageing 2019: Highlights. [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walmsley R. twelfth ed. Institute for Criminal Policy Research; 2018. World Prison Population List. [Google Scholar]
- WBRZ . 2020. More than 60 La. Nursing Homes Have Coronavirus Cases, Several Local Facilities with Clusters. [Google Scholar]
- WHO Regional Office for Europe . 2020. Preparedness, Prevention and Control of COVID-19 in Prisons and Other Places of Detention (2020) (Denmar) [Google Scholar]
- World Health Organization . 2020. Q&A on Infection Prevention and Control for Health Care Workers Caring for Patients with Suspected or Confirmed 2019-nCoV. [Google Scholar]
- World Health Organization . 2020. Infection Prevention and Control Guidance for Long-Term Care Facilities in the Context of COVID -19. [Google Scholar]
- World Health Organization . 2020. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. [Google Scholar]
- Wuhan Municipal Health Commission . 2019. Report of Clustering Pneumonia of Unknown Etiology in Wuhan City. [Google Scholar]
- Yang Z. 2020. Hundreds of Infections Reported in Five Prisons. [Google Scholar]
- Zhai J. Facial mask: a necessity to beat COVID-19. Build. Environ. 2020;175:1–2. doi: 10.1016/j.buildenv.2020.106827. [DOI] [PMC free article] [PubMed] [Google Scholar]