Abstract
Background
The COVID-19 pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is of a scale not seen since the 1918 influenza pandemic. Although the predominant clinical presentation is with respiratory disease, neurological manifestations are being recognised increasingly. On the basis of knowledge of other coronaviruses, especially those that caused the severe acute respiratory syndrome and Middle East respiratory syndrome epidemics, cases of CNS and peripheral nervous system disease caused by SARS-CoV-2 might be expected to be rare.
Recent developments
A growing number of case reports and series describe a wide array of neurological manifestations in 901 patients, but many have insufficient detail, reflecting the challenge of studying such patients. Encephalopathy has been reported for 93 patients in total, including 16 (7%) of 214 hospitalised patients with COVID-19 in Wuhan, China, and 40 (69%) of 58 patients in intensive care with COVID-19 in France. Encephalitis has been described in eight patients to date, and Guillain-Barré syndrome in 19 patients. SARS-CoV-2 has been detected in the CSF of some patients. Anosmia and ageusia are common, and can occur in the absence of other clinical features. Unexpectedly, acute cerebrovascular disease is also emerging as an important complication, with cohort studies reporting stroke in 2–6% of patients hospitalised with COVID-19. So far, 96 patients with stroke have been described, who frequently had vascular events in the context of a pro-inflammatory hypercoagulable state with elevated C-reactive protein, D-dimer, and ferritin.
Where next?
Careful clinical, diagnostic, and epidemiological studies are needed to help define the manifestations and burden of neurological disease caused by SARS-CoV-2. Precise case definitions must be used to distinguish non-specific complications of severe disease (eg, hypoxic encephalopathy and critical care neuropathy) from those caused directly or indirectly by the virus, including infectious, para-infectious, and post-infectious encephalitis, hypercoagulable states leading to stroke, and acute neuropathies such as Guillain-Barré syndrome. Recognition of neurological disease associated with SARS-CoV-2 in patients whose respiratory infection is mild or asymptomatic might prove challenging, especially if the primary COVID-19 illness occurred weeks earlier. The proportion of infections leading to neurological disease will probably remain small. However, these patients might be left with severe neurological sequelae. With so many people infected, the overall number of neurological patients, and their associated health burden and social and economic costs might be large. Health-care planners and policy makers must prepare for this eventuality, while the many ongoing studies investigating neurological associations increase our knowledge base.
Introduction
As of May 19, 2020, the COVID-19 pandemic, caused by the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in more than 4·8 million confirmed cases worldwide and more than 300 000 deaths.1 It is the largest and most severe pandemic since the 1918 influenza pandemic.2 Although the most common and important presentation is with respiratory disease, reports of neurological features are increasing. These features appear to be a combination of non-specific complications of systemic disease, the effects of direct viral infection, or inflammation of the nervous system and vasculature, which can be para-infectious or post-infectious. In this Rapid Review, we consider which neurological manifestations might be expected for COVID-19, given what is known about related coronaviruses and respiratory viruses more broadly. We summarise the evidence to date for COVID-19, examine putative disease mechanisms, and finally suggest a framework for investigating patients with suspected COVID-19-associated neurological disease to support clinico-epidemiological, disease mechanism, and treatment studies.
Evidence from other viruses
Before identification of SARS-CoV-2, six coronaviruses were known to infect humans. Four of these coronaviruses cause seasonal, predominantly mild respiratory illness, and have a high incidence globally, accounting for 15–30% of upper respiratory tract infections.3 The other two coronaviruses have led to major epidemics with deaths principally from respiratory disease; severe acute respiratory syndrome (SARS) was caused by SARS-CoV in 2002–03, and Middle East respiratory syndrome (MERS) by MERS-CoV in 2012.4, 5 Both the more innocuous coronaviruses and these epidemic strains have been associated with occasional disease of the CNS and peripheral nervous system (PNS).
Both CNS and PNS disease were reported following SARS (appendix pp 2–3). SARS-CoV was detected in CSF by RT-PCR in two of three cases of encephalopathy with seizures,6, 7 and was cultured from brain tissue at autopsy in the third.8 Four patients with severe SARS developed neuromuscular disease, predominantly motor neuropathy, myopathy, or both,9 which might have been SARS-specific or secondary to critical illness.10 CNS involvement was described for five adults with MERS; two had acute disseminated encephalomyelitis, two had cerebrovascular disease, and one had Bickerstaff's brainstem encephalitis.11, 12, 13 Neuropathy was described in three patients.11, 13 Human coronavirus OC43, a seasonal coronavirus, has caused encephalitis in an infant with severe combined immunodeficiency,14 and acute disseminated encephalomyelitis in an older immunocompetent child.15 Headache, neck stiffness, and seizures were described among 22 children (median age 36 months; range 0·8–72 months) with suspected CNS infection and coronavirus IgM antibodies in their serum, CSF, or both.16 Ten of these children had pleiocytosis and eight had brain imaging abnormalities. All 22 made a full recovery.16
Neurological complications have also been described for other respiratory viruses, particularly seasonal and pandemic influenza.3 These complications include acute necrotising encephalopathy (associated with mutations in the RANBP2 gene), acute infantile encephalopathy, and acute haemorrhagic leukoencephalopathy and myelopathy in adults.17, 18 The estimated incidence of neurological disorders during the 2009 influenza A H1N1 pandemic was 1·2 per 100 000, with children affected more than adults.19, 20, 21, 22 The 1918 H1N1 influenza pandemic has been associated with post-infectious encephalitis lethargica, although a causative link has not been proven.23
Projected epidemiology of COVID-19-associated neurological disease
Although neurological complications are rare in SARS, MERS, and COVID-19, the scale of the current pandemic means that even a small proportion could build up to a large number of cases. The minimum prevalence of CNS complications ranged from 0·04% for SARS to 0·20% for MERS, and PNS complications ranged from 0·05% for SARS to 0·16% for MERS, from which we have extrapolated the number of cases with neurological complications of COVID-19 (table 1 ). Given the 4·8 million cases of COVID-19 globally, these prevalences project to a total of 1805–9671 patients with CNS complications and 2407–7737 with PNS complications. These numbers, which do not include the increasingly important syndromes of stroke-associated COVID-19 infection, will rise as the pandemic continues.
Table 1.
Estimated neurological disease case numbers associated with COVID-19, extrapolated from SARS and MERS data
| SARS case count (n=8096) | MERS case count (n=2228) |
COVID-19 worldwide minimum case count (n=4 872 308) |
COVID-19 minimum case count in China (n=84 500) |
COVID-19 minimum case count in USA (n=1 464 232) |
COVID-19 minimum case count in UK (n=246 410) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Extrapolated from SARS (95% CI) | Extrapolated from MERS (95% CI) | Extrapolated from SARS (95% CI) | Extrapolated from MERS (95% CI) | Extrapolated from SARS (95% CI) | Extrapolated from MERS (95% CI) | Extrapolated from SARS (95% CI) | Extrapolated from MERS (95% CI) | |||
| Patients with CNS disease (proportion of total coronavirus cases [95% CI]) | 3 (0·04% [0·01–0·10]) | 5 (0·20% [0·06–0·50]) | 1805 (370–5277) | 9671 (3143–22539) | 31 (6–92) | 168 (55–391) | 543 (111–1586) | 2906 (944–6774) | 91 (19–267) | 489 (159–1140) |
| Patients with PNS disease (proportion of total coronavirus cases [95% CI]) | 4 (0·05% [0·01–0·13]) | 4 (0·16% [0·04–0·41]) | 2407 (658–6163) | 7737 (2110–19786) | 42 (11–107) | 134 (37–343) | 723 (198–1852) | 2325 (634–5946) | 122 (33–312) | 391 (107–1001) |
| Total patients with neurological disease (proportion of total coronavirus cases [95% CI]) | 7 (0·09% [0·03–0·18]) | 9 (0·36% [0·16–0·68]) | 4213 (1028–11440) | 17 408 (5252–42326) | 73 (18–198) | 302 (91–734) | 1266 (309–3438) | 5231 (1578–12720) | 213 (52–579) | 880 (266–2141) |
Calculated using data available up to May 19, 2020. COVID-19 cases based on Johns Hopkins COVID-19 Dashboard. 95% CI calculated with Clopper-Pearson exact method24 for proportions using Ausvet Epitools. SARS=severe acute respiratory syndrome. MERS=Middle East respiratory syndrome. PNS=peripheral nervous system.
Clinical features of COVID-19-associated neurological disease
As the COVID-19 pandemic progresses, reports of neurological manifestations are increasing; to date, 901 patients have been reported. These manifestations can be considered as direct effects of the virus on the nervous system, para-infectious or post-infectious immune-mediated disease, and neurological complications of the systemic effects of COVID-19 (appendix p 4). In one national registry of 125 patients with COVID-19 and neurological or psychiatric disease reported over a 3-week period,25 39 (31%) patients had altered mental status, which included 16 (13%) with encephalopathy (of whom seven [6%] had encephalitis), and 23 (18%) with a neuropsychiatric diagnosis, including ten (8%) with psychosis, six (5%) with neurocognitive (dementia-like) syndrome, and four (3%) with an affective disorder. Notably, 77 (62%) patients had a cerebrovascular event: 57 (46%) ischaemic strokes, nine (7%) intracerebral haemorrhages, one (<1%) CNS vasculitis, and ten (8%) other cerebrovascular events.25 The challenges in managing patients with a highly contagious infection, and the overwhelming number of cases, have meant that many early reports did not have sufficient detail, few included comprehensive description of CSF analysis, imaging, or follow-up, and they often appear on non-peer-reviewed websites. Most are not reported using standard case definitions (panel ; appendix pp 5–12). In what follows, we review the CNS and PNS infectious and inflammatory complications that are well recognised for viral respiratory infections, followed by cerebrovascular disease, which is relatively unusual (table 2 ).
Panel. Provisional case definitions for the association of COVID-19 with neurological disease.
WHO COVID-19 case definitions 26
Confirmed
A person with laboratory confirmation27 of SARS-CoV-2 infection, irrespective of clinical signs and symptoms; confirmatory tests include a nucleic acid amplication test (eg, RT-PCR) or validated antibody test; in an area with established circulation of virus, there should be one positive RT-PCR test or identification of virus on sequencing (one or more negative tests do not rule out infection if there is clinical suspicion); and in an area without established circulation of virus, there should be one positive RT-PCR test for two different viral genome targets or one positive result with partial or whole genome sequencing
Probable
(1) A suspect case for whom testing for the COVID-19 virus is inconclusive; or (2) a suspect case for whom testing could not be done for any reason
Suspected
(1) A patient with acute respiratory illness (fever and at least one sign or symptom of respiratory distress) and history of travel to or residence in a location reporting community transmission of COVID-19 disease during the 14 days before onset; or (2) a patient with acute respiratory illness who has been in contact with a confirmed or probable case in the last 14 days before symptom onset; or (3) a patient with severe acute respiratory illness that requires hospitalisation, and in the absence of an alternative explanation that fully explains the clinical presentation
SARS-CoV-2 meningitis, encephalitis, myelitis, or CNS vasculitis *
Confirmed
(1) SARS-CoV-2 detected in CSF or brain tissue† or evidence of SARS-CoV-2-specific intrathecal antibody; and (2) no other explanatory pathogen or cause found
Probable
(1) SARS-CoV-2 detected in respiratory or other non-CNS sample,‡ or evidence of SARS-CoV-2-specific antibody in serum indicating acute infection;§ and (2) no other explanatory pathogen or cause found
Possible
Patient meets suspected case definition of COVID-19 according to national or WHO guidance on the basis of clinical symptoms and epidemiological risk factors; in the context of known community SARS-CoV-2 transmission, supportive features include the following: the new onset of at least one of cough, fever, muscle aches, loss of smell, or loss of taste; lymphopenia or raised D-dimer level; and radiological evidence of abnormalities consistent with infection or inflammation (eg, ground glass changes)
Acute disseminated encephalomyelitis * associated with SARS-CoV-2 infection, Guillain-Barré syndrome, * and other acute neuropathies associated with SARS-CoV-2 infection
Probable association
(1) Neurological disease onset within 6 weeks of acute infection; and (2) either SARS-CoV-2 RNA detected in any sample or antibody evidence of acute SARS-CoV-2 infection; and (3) no evidence of other commonly associated causes
Possible association
(1) Neurological disease onset within 6 weeks of acute infection; and (2) either SARS-CoV-2 RNA detected in any sample or antibody evidence of acute SARS-CoV-2 infection; and (3) evidence of other commonly associated causes¶
Stroke * associated with SARS-CoV-2 infection
Probable association
(1) Either SARS-CoV-2 detected in CSF or other sample,‡ or evidence of SARS-CoV-2-specific antibody in serum indicating acute infection; and (2) no other known traditional cardiovascular risk factors||
Possible association
(1) Either SARS-CoV-2 detected in CSF or other sample, or evidence of SARS-CoV-2-specific antibody indicating acute infection; and (2) other traditional cardiovascular risk factors||
These case definitions are suggestions based on published information to date; they are likely to need refining as more data emerge. The terms confirmed, probable, and suspected are used in the WHO COVID-19 case definitions; the terms confirmed, probable, possible, probable association, and possible association reflect the terminology used for the different syndromes in the original publications from which this panel derives.28, 29, 30 SARS-CoV-2=severe acute respiratory syndrome coronavirus 2.
Table 2.
Selected reports of neurological manifestations associated with COVID-19
| Clinical presentation | SARS-CoV-2 diagnostics | Other pathogen and antibody investigations | Relevant blood tests and radiology findings | Neurological investigations (CSF findings, neuroimaging, neurophysiology) | Management, progress, and outcome | ||
|---|---|---|---|---|---|---|---|
| CNS disease | |||||||
| Encephalitis | |||||||
| Moriguchi et al;31 one case, Japan | Man aged 24 years, 9 days of fatigue, headache, fever, sore throat; then generalised seizures, reduced consciousness, and meningism | RT-PCR was negative in nasopharyngeal swab; positive in CSF | Serum: anti-HSV-1 and VZV IgM antibodies tests were negative | Increased blood white cell count, neutrophil dominant, relatively decreased lymphocytes, increased CRP; chest CT: small ground glass opacity in right upper zone and bilaterally in lower zones | CSF: clear, colourless, raised opening pressure (320 mm H20) and cell count (12/mm3; ten mononuclear and two polymorphonuclear cells); head CT: no brain oedema; brain MRI: hyperintensity along wall of right lateral ventricle on diffusion-weighted imaging, and hyperintense signal in right medial temporal lobe and hippocampus on T2-weighted images | Treated empirically for bacterial pneumonia and viral encephalitis; on admission, required intubation and mechanical ventilation because of seizures; admitted to ICU; still on intensive care at time of report (day 15) | |
| Sohal et al;32 one case, USA | Man aged 72 years with weakness and light headedness following a hypoglycaemic episode; shortly after admission he had difficulty breathing and altered mental status; on day 2 of admission he started to have seizures | RT-PCR was positive; source not specified | Blood: culture was negative for bacterial growth; influenza PCR was negative | Arterial blood gas test: pH 7·13, PaO2 68 mm Hg, PCO2 78 mm Hg, raised brain natriuretic peptide, troponin, CRP, LDH; lymphopenia, and leucopenia; chest x-ray: normal; chest CT: bibasilar opacities along with right lower lobe consolidation | Head CT: no acute changes, chronic microvascular ischaemic changes; 24-h EEG: six left temporal seizures and left temporal sharp waves that were epileptogenic | Required intubation and ventilation and was admitted to ICU; became hypotensive requiring norepinephrine via central line; hydroxychloroquine and azithromycin were started in addition to vancomycin and piperacillin tazobactam; after onset of seizures, treated with levetiracetam and valproate but they were not controlled; died on day 5 of illness | |
| Wong et al;33 one case, UK | Man aged 40 years with ataxia, diplopia, oscillopsia, and bilateral facial weakness (rhombencephalitis); 13 days before he had fever and progressive shortness of breath on exertion, followed 10 days later by a productive cough and diarrhoea | RT-PCR was positive in nasopharyngeal swab; CSF RT-PCR was not done | Blood: negative for hepatitis A, B, and C, HIV-1 and HIV-2, and syphilis antibody; CSF: bacterial culture was negative; anti-MOG-IgG antibody and anti-aquaporin 4 antibody test results not reported | Normal white cell count but lymphopenia; raised CRP and abnormal raised liver function tests; chest x-ray: right lower zone consolidation; liver ultrasound: inflammatory diffusely hypoechoic liver with raised periportal and pericholecystic echogenicity | Normal cell count and protein (0·42 g/L); brain MRI: increased signal lesion in right inferior cerebellar peduncle extending to involve a small portion of the upper cord (lesion 13 mm in maximum cross-sectional area and 28 mm in longitudinal extent); swelling at the affected tissue and associated micro-haemorrhage | Treated with oral amoxicillin, but no other treatment; gradual improvement in neurological symptoms; discharged home after 11 days on gabapentin; oscillopsia and ataxia persisted | |
| Other encephalopathies | |||||||
| Dugue et al;34 one case, USA | Infant aged 6 weeks with cough, fever, and episodes of bilateral leg stiffening and sustained upward gaze | RT-PCR was positive and high-throughput sequencing detected viral RNA in nasopharyngeal and anal swabs; RT-PCR was negative in plasma and CSF | Nasopharyngeal sample tested for respiratory pathogen; PCR panel positive for rhinovirus–enterovirus; high-throughput sequencing was positive for rhinovirus C; CSF: meningitis–encephalitis pathogen PCR panel was negative; culture negative | Leucopenia (5·07 × 103 white blood cells per μL) with a normal differential, and elevated procalcitonin of 0·21 ng/m; normal urea and electrolytes | CSF: normal; brain MRI: normal; prolonged EEG monitoring: excess of temporal sharp transients and intermittent vertex delta, slowing with normal sleep–wake cycling | No specific treatment; no further episodes and discharged home after 1 day | |
| Helms et al;35 49 cases, France | 40 patients had agitation; 26 of the 40 evaluated had confusion, 39 had corticospinal tract signs, 15 had a dysexecutive syndrome at discharge, and seven had history of neurological disorders, including transient ischaemic attack, partial epilepsy, and mild cognitive impairment | RT-PCR was positive for all patients' nasopharyngeal samples; negative RT-PCR in CSF in seven patients | NR | NR | In seven patients who had CSF analysis, none had pleiocytosis, two had matched oligoclonal bands, and one had raised protein; in 13 patients who had brain MRI, eight had enhancement in leptomeningeal spaces; in 11 patients who had perfusion imaging, all had bilateral frontotemporal hypoperfusion, two patients had acute ischaemic stroke, and one had subacute ischaemic stroke; in eight patients who had EEG, one had diffuse bifrontal slowing | All patients required treatment on ICU for severe COVID-19; 45 had been discharged from ICU at the time of writing | |
| Mao et al;36 16 cases, China | 16 patients were hospitalised with COVID-19 and had impaired consciousness; one had a seizure characterised by a sudden onset of limb twitching and loss of consciousness, lasting 3 min | RT-PCR was positive in all patients' throat swabs | NR | Patients with CNS disease and severe respiratory disease had lower lymphocyte levels and platelet counts and higher blood urea nitrogen levels than those without CNS symptoms | NR | 13 patients had severe respiratory disease and three had non-severe respiratory disease, according to American Thoracic Society guidelines; no further details | |
| Poyiadji et al;37 one case, USA | Female patient with cough, fever, and altered mental status; imaging consistent with acute necrotising encephalopathy | RT-PCR was positive in nasopharyngeal swab; CSF RT-PCR not done | CSF: bacterial culture negative after 3 days and tests for HSV, VZV, and WNV were negative | NR | Non-contrast head CT: symmetric hypoattenuation in bilateral medial thalami; brain MRI: T2 FLAIR hyperintensity in bilateral medial temporal lobes, thalami, and subinsular regions, and evidence of haemorrhage indicated by hypointensity on susceptibility-weighted images and rim enhancement on post-contrast images | Treated with intravenous immunoglobulin; outcome not reported | |
| Paniz-Mondolfi et al;38 one case, USA | Man aged 74 years with history of Parkinson's disease presented following two falls at home with fever, confusion, and agitation | RT-PCR was positive in nasopharyngeal swab; electron microscopy of brain tissue: viral particles in endothelial and neural cells | NR | Increased CRP, ferritin, D-dimer, and thrombocytopenia; initial chest radiology: no changes in lung fields; subsequently developed new changes bilaterally on chest x-ray suggestive of consolidation | Head CT: no acute changes | Given hydroxychloroquine and low-molecular-weight heparin initially, then tocilizumab; persistently febrile and agitated with episodes of hypotension and increasing hypoxia; developed new onset atrial fibrillation; given fluids and amiodarone, reverting to sinus rhythm, then metoprolol; deteriorated and died | |
| Zhou et al;39 one case, China | Patient aged 56 years with COVID-19 pneumonia | SARS-CoV2 detected by sequencing in CSF | NR | NR | NR | NR | |
| Acute disseminated encephalomyelitis | |||||||
| Zanin et al;40 one case, Italy | Woman aged 54 years presented with agitation, decreased consciousness, and seizures following several days of anosmia and ageusia | RT-PCR was positive in respiratory sample | Blood: cultures were negative; urine: cultures were negative | Lymphopenia (0·3 × 109 cells per L) with mild elevation of inflammatory markers (CRP 41·3 mg/L, fibrinogen 520 mg/dL); chest x-ray: interstitial pneumonia | CSF: normal; brain and spine MRI: periventricular confluent white matter lesions and numerous high signal cord lesions from bulbomedullary junction to T6 level; no contrast enhancement | Treated with antiretrovirals and hydroxychloroquine; clinically deteriorated becoming hypoxic, requiring intubation and mechanical ventilation; treated with high dose dexamethasone; tracheostomy done on day 7; weaned off ventilator on day 15; discharged and transferred to rehabilitation without sensorimotor deficit about 1 month after admission | |
| Zhang et al;41 one case, USA | Woman in early 40s with a 9-day history of headache and myalgia presented with dysphagia, dysarthria, expressive dysphasia, and encephalopathy; left sided facial weakness, fever, and dyspnoea on admission | RT-PCR was positive; site not specified (presumed respiratory sample) | Negative influenza swab and negative rapid streptococcus test; CSF: negative; PCR test for HSV-1 and HSV-2, HHV-6, and VZV, and negative Cryptococcus test; bacterial cultures were negative | Mild leukocytosis with lymphopenia; chest x-ray: patchy consolidation in right lower lung | CSF: normal cell count, protein, and glucose; brain MRI: extensive areas of high signal in bilateral frontoparietal white matter, anterior temporal lobes, basal ganglia, external capsules, and thalami; some foci showed diffusion-weighted imaging changes and corresponding apparent diffusion coefficient changes; brain and neck magnetic resonance angiography: normal; EEG: no evidence of seizures | Treated with hydroxychloroquine, ceftriaxone, and intravenous immunoglobulin; some improvement in dysphagia and dysarthria after 5 days | |
| Myelitis | |||||||
| Zhao et al;42 one case, China | Man aged 66 years admitted with fever, dyspnoea, and asthma; 5 days after respiratory symptom onset, developed acute flaccid paralysis of lower limbs, urinary and faecal incontinence, and a sensory level at T10 | RT-PCR was positive in nasopharyngeal swab | Blood: negative for EBV, influenza A, influenza B, adenovirus, coxsackievirus, parainfluenza virus, CMV, and RSV on serum IgM testing; negative for Chlamydia pneumoniae, Mycoplasma pneumoniae, and tuberculosis | Lymphopenia (0·55 × 109 cells per L) and raised CRP (277 mg/L) and procalcitonin (4·33 ng/mL); slightly raised alanine aminotransferase (56 U/L) and aspartate aminotransferase (50 U/L); chest CT: bilateral patchy changes | Brain CT: lacunar infarcts; spinal imaging not done | On admission, deteriorated rapidly and admitted to ICU; treated with moxifloxacin, oseltamivir, lopinavir–ritonavir, ganciclovir, and meropenem, followed by dexamethasone and intravenous immunoglobulin for neurological symptoms; required oxygen; slight improvement in power in upper and lower limbs following treatment, but still unable to walk; discharged and transferred for rehabilitation | |
| Peripheral nervous system disease | |||||||
| Guillain-Barré syndrome | |||||||
| Camdessanche et al;43 one case, France | Man aged 64 years with 2 days of cough and fever presented following a fall; on day 9 of hospital admission, developed paraesthesia in hands and feet and progressive weakness in all limbs, with areflexia and loss of vibration sense; then developed dysphagia and respiratory insufficiency | RT-PCR was positive in nasopharyngeal swab on admission, 9 days before onset of neurological symptoms | Negative for Campylobacter jejuni, M pneumoniae, Salmonella enterica, CMV, EBV, HSV-1, HSV-2, VZV, influenza virus A and B, HIV, and hepatitis E; serum: antiganglioside antibodies not detected | Chest CT: 10% to 25% ground glass opacities | CSF: normal cell count and raised protein (166 mg/dL); nerve conduction study and electromyography: acute inflammatory demyelinating polyneuropathy | Had initially needed 2L to 3L oxygen via nasal cannula but had been weaned off it before onset of neurological symptoms; given lopinavir–ritonavir; treated with intravenous immunoglobulin for 5 days; developed respiratory insufficiency and required admission to ICU for intubation and mechanical ventilation; no other details given | |
| Toscano et al;44 five cases, Italy | Five patients (four men and one woman), aged 23 to 77 years; four patients had flaccid, areflexic limb weakness (three with quadriparesis and one with paraparesis), three of whom had facial weakness, two had dysphagia, and three developed respiratory failure; one had facial diplegia, areflexia, limb paraesthesia, and ataxia; patients presented a median of 7 (range 5 to 10) days after respiratory symptoms; four had cough, three had fever, three had hyposmia, anosmia, or ageusia, and one had pharyngitis | RT-PCR was positive in nasopharyngeal swab of four patients; one patient was positive by serological test; RT-PCR in CSF was negative in all patients | One patient (patient 5) was negative for C jejuni, EBV, CMV, HSV, VZV, influenza, and HIV; three patients were tested for antiganglioside antibodies, but none was detected | Patient 1: CT scan of thorax showed interstitial bilateral pneumonia; patient 2: no details; patient 3: CT scan of thorax showed multiple bilateral, ground glass opacities compatible with interstitial pneumonia; patient 4: chest imaging was negative; patient 5: x-ray and CT showed interstitial pneumonia, without parenchymal opacities or alveolar damage | CSF analysis: all patients had normal white cell counts, three had elevated protein; MRI: enhancement of caudal nerve roots in two patients and of facial nerve in one, and no signal change in two patients; nerve conduction study: axonal pattern in three patients and demyelinating in two | All treated with intravenous immunoglobulin; two had two cycles, and one also had plasma exchange; three required mechanical ventilation; at 4 weeks, two patients were still ventilated in intensive care, two were having physiotherapy, and one was discharged | |
| Zhao et al;45 one case, China | Woman aged 61 years with progressive weakness of lower and then upper limbs and severe fatigue; areflexia in lower limbs and decreased sensation distally; 7 days after neurological symptoms, she developed dry cough and fever | RT-PCR was positive in oropharyngeal swab | NR | Laboratory results on admission were clinically significant for lymphopenia and thrombocytopenia; chest CT: ground glass opacities bilaterally | CSF: normal cell count and raised protein (124 mg/dL); nerve conduction study: acute inflammatory demyelinating polyneuropathy | Treated with intravenous immunoglobulin for 5 days; given arbidol, lopinavir, and ritonavir; improved neurologically; had normal power and reflexes on discharge at day 30 | |
| GBS variants and other neuropathies | |||||||
| Gutiérrez-Ortiz et al;46 one Miller Fisher Syndrome, Spain | Man aged 50 years with 5 days of cough, fever, malaise, headache, back pain, anosmia, and ageusia, who developed right internuclear opthalmoparesis with right fascicular oculomotor palsy, ataxia, and areflexia (preserved plantar responses) | RT-PCR was positive in oropharyngeal swab, negative in CSF | Antiganglioside antibody GD1b-IgG detected in serum; normal CSF cytology, sterile cultures, and negative antibody tests | Lymphopenia; elevated CRP; chest x-ray: normal | CSF: normal opening pressure, cell count, raised protein (80 mg/dL), and normal glucose; brain CT with contrast: normal | Treated with intravenous immunoglobulin for 5 days; complete recovery at 2 weeks except for residual anosmia and ageusia | |
| Dinkin et al;47 one ophthalmoplegia, USA | Woman aged 71 years with isolated ophthalmoplegia after a few days of cough and fever; unable to abduct her right eye (right abducens palsy) | RT-PCR was positive in nasal swab | NR | Leucopenia; chest x-ray: bilateral opacities | CSF: normal opening pressure; brain MRI: enhancement of optic nerve sheaths and posterior Tenon capsules | Treated with hydroxychloroquine and oxygen; discharged after 6 days; symptoms improving, although ongoing at 2 weeks after discharge | |
| Gutiérrez-Ortiz et al;46 one bilateral ophthalmoplegia, Spain | Man aged 39 years, with 3 days of fever and diarrhoea, developed diplopia; abduction deficits in both eyes and fixation nystagmus consistent with bilateral abducens palsy; global areflexia and ageusia | RT-PCR was positive in oropharyngeal swab and negative in CSF | Normal CSF cytology, sterile cultures, and negative anti-pathogen antibody tests | Leucopenia, but blood tests otherwise normal; chest x-ray: normal | CSF: normal cell count, but raised protein (62 mg/dL); brain CT: normal | No specific treatment; complete recovery in 2 weeks | |
| Escalada Pellitero et al;48 one acute vestibular dysfunction, USA | Woman aged 30 years had nausea, unsteadiness, and disequilibrium that was worse on standing; 3 weeks before, she had 10 days of anosmia and ageusia; horizontal nystagmus with rapid phase to the right, oscillopsia, and Romberg positive | RT-PCR was positive on admission; sample tested not reported | NR | Lymphopenia, and raised D-dimer, fibrinogen, and CRP; chest CT angiogram: normal | Brain MRI with contrast: normal | Treated with antiemetics and vestibular suppressants; improved | |
| Rhabdomyolysis and other muscle disease | |||||||
| Jin et al,49 one case of rhabdomyolysis, China | Man aged 60 years admitted with COVID-19 developed weakness and tenderness in lower limbs 15 days after onset of fever and cough | RT-PCR was positive in throat swab | Urine: blood and protein detected | Leucopenia, and raised CRP and LDH; normal urea, electrolytes, liver function tests, and creatine kinase initially; then raised creatine kinase (11 842 U/L), myoglobin (12 000 mg/L), aspartate aminotransferase and alanine aminotransferase; chest CT: ground glass opacities | NR | Worsening respiratory status following admission; received antibiotics and supportive therapy; neuromuscular symptoms improved over several days | |
| Taste and smell dysfunction | |||||||
| Lechien et al;50 357 cases, Belgium, France, Italy, Spain, and Switzerland | 357 (86%) of 417 patients had smell dysfunction; 342 (82%) had taste dysfunction | All RT-PCR were positive in respiratory samples | NR | NR | NR | Treated with nasal corticosteroids (8%), oral corticosteroids (3%), and nasal irrigation (17%) | |
| Cerebrovascular disease | |||||||
| Ischaemic stroke | |||||||
| Avula et al;51 four cases, USA | Four patients (aged 73 to 88 years) with hypertension; three had dyslipidaemia, one diabetes and neuropathy, one carotid stenosis, and one chronic kidney disease; three presented with acute new focal neurological deficit (facial droop, slurred speech; left-sided weakness; and right-arm weakness and word finding difficulty), and one with altered mental status; one had fever, respiratory distress, nausea, and vomiting; one had fever only; one had mild shortness of breath with dry cough; one had no respiratory symptoms or fever | All four had positive RT-PCR (presumed to be upper respiratory samples); no mention of CSF studies | Negative blood and urine cultures in the two patients for whom results were reported | Three patients had lymphopenia, one with leucopenia and two with leucocytosis; two had elevated D-dimer and inflammatory markers; three had patchy changes bilaterally on chest x-ray or CT | All four had evidence of unifocal infarcts: three on CT, one on brain MRI | All were treated with antiplatelet therapy; none had thrombolysis or thrombectomy; three required intubation and ventilation, all of whom died; fourth patient discharged to rehabilitation facility | |
| Beyrouti et al;52 six cases, UK | Six patients (aged 53 to 83 years; five male and one female), three of whom had hypertension, two ischaemic heart disease, two atrial fibrillation, one a previous stroke and high body-mass index, and one was a smoker with heavy alcohol consumption and diabetes; three had dysarthria, one expressive dysphasia, one aphasia; four had hemiparesis and two had incoordination; one had reduced consciousness, and all had respiratory symptoms at a median of 13 days (range −2 to 24) before or after neurological symptom onset | All six had positive RT-PCR (presumed to be upper respiratory samples); no mention of CSF studies | One had a medium titre IgM anti-cardiolipin antibody and low titre IgG and IgM aβ2GP1 antibody | One had leucocytosis and three had lymphopenia; all had raised D-dimer and LDH; five had raised ferritin and five had raised CRP; all had bilateral patchy changes on chest x-ray or CT, and two had pulmonary emboli (one in a segmental artery and one with bilateral emboli in segmental and subsegmental arteries) | Initial scans (CT and brain MRI) showed unifocal infarcts in four patients, one of whom had bilateral infarcts on a follow-up brain MRI; two had bilateral infarcts on initial scans | One treated with dual antiplatelet and therapeutic low-molecular weight heparin therapy; one had external ventricular drain placement and therapeutic low-molecular-weight heparin; one had apixaban; one had therapeutic low-molecular weight heparin; two had intravenous thrombolysis; three required oxygen therapy; two were admitted to ICU; one died secondary to COVID-19 pneumonia following cardiorespiratory deterioration | |
| Li et al;53 11 cases, China | 11 patients (aged 57 to 91 years; six female and five male), nine of whom had hypertension, six diabetes, three cardiovascular disease, three were smokers, and one with malignancy; five had large-vessel stenosis, three cardioembolic, and three small-vessel disease; all had respiratory symptoms a median of 11 days (range 0 to 30) before neurological symptoms onset | All RT-PCRs were positive on throat swab | NR | No specific detail given on the 11 patients with ischaemic stroke; all patients had evidence of COVID-19 pneumonia on chest CT | NR | Nine had severe disease; six were treated with antiplatelets (aspirin or clopidogrel); five were given anticoagulant therapy (clexane); four died and seven survived | |
| Morassi et al;54 four cases, Italy | Four patients (aged 64 to 82 years), three of whom had hypertension, two had a previous stroke or transient ischaemic attack and aortic valve disease, and one was a smoker with a previous myocardial infarction; all presented with severe acute respiratory illness; three developed neurological manifestations during hospitalisation (two hemiparesis and one inability to rouse when sedation held); one presented with episodes of transient loss of consciousness and confusion | All RT-PCRs were positive on nasopharyngeal swab | NR | All had raised CRP levels, two each had raised D-dimer, raised LDH, and abnormal renal and liver function tests; chest CT on all patients: bilateral ground glass opacities (one patient also had bilateral pleural effusions and a pulmonary embolism) | One had CSF: normal leukocyte count, protein, and IgG index; all had multifocal infarcts on brain CT or MRI; the patient presenting with transient loss of consciousness and ensuing confusion had EEG: normal background in the alpha range (8 Hz), associated with recurrent sharp slow waves over left temporal region, which occasionally were seen also on the right homologous regions | One patient treated with aspirin, clopidogrel, and enoxaparin; one given levetiracetam; treatment not reported for the remaining two; two were intubated and mechanically ventilated; two died; of the two survivors, one had coma (GCS 3/15) and one was severely disabled with modified Rankin score of 4 | |
| Oxley et al;55 five cases, USA | Five patients (aged 33 to 49 years; four male and one female); all had hemiplegia; four had reduced consciousness; three had dysarthria, one global dysphasia, two had a sensory deficit, and three had systemic or respiratory symptoms | All five had positive RT-PCR (presumed to be upper respiratory samples); no mention of CSF studies | NR | One had thrombocytopenia, one prolonged prothrombin time, one prolonged activated partial thromboplastin time, and three each had raised fibrinogen, increased D-dimer, and raised ferritin; CT angiography reported in one patient: patchy ground glass opacities in lung apices | All had single-territory infarcts on brain CT or MRI | Four had clot retrieval, one of whom had intravenous thrombolysis and hemicraniectomy and one had stent insertion; two had apixaban, two aspirin alone, and one dual antiplatelets; one discharged home; two discharged to rehabilitation facilities; two remain in hospital (one in ICU and one in stroke unit) | |
| Intracerebral haemorrhage | |||||||
| Al Saiegh et al;56 one case, USA | Man aged 31 years with one week of malaise, mild fever, cough, and arthralgia had sudden onset of headache and loss of consciousness; confused after first operation | RT-PCR was positive in nasal swab; CSF RT-PCR was negative on two samples | NR | NR | Head CT: subarachnoid haemorrhage in posterior fossa; subsequent CT showed hydrocephalus; cerebral angiogram showed ruptured dissecting right posterior–inferior cerebellar artery aneurysm | External ventricular drain inserted initially; then flow-diverting stent placed to treat ruptured aneurysm; intubated for surgery but did not require ongoing ventilator support; postoperative confusion resolved; discharged for rehabilitation | |
| Morassi et al;54 two cases, Italy | Two men aged 57 years admitted to hospital with critical COVID-19; at 7 and 11 days later (14 and 17 days after onset of cough and fever, one with dyspnoea), they had bilaterally fixed dilated pupils and coma (GCS 3/15) | Both RT-PCRs were positive on nasopharyngeal swab | NR | Both had raised CRP, LDH, aspartate aminotransferase and gamma-glutamyl transpeptidase; chest CT showed diffuse bilateral ground glass opacities in both patients | One patient had bilateral cerebellar haemorrhages on brain CT with hydrocephalus; the other had a large frontal haemorrhage with displaced ventricles and multiple smaller haemorrhages | Both patients developed respiratory failure requiring intubation, ventilation, and admission to ICU; both deteriorated neurologically, and imaging confirmed cerebral haemmorhage; both died | |
| Cerebral venous sinus thrombosis | |||||||
| Li et al;53 one case, China | Man aged 32 years with history of smoking developed neurological features 14 days after initial presentation with COVID-19 | RT-PCR was positive on throat swab | NR | NR | NR | Treated with anticoagulation; survived but remains in hospital | |
A full version of this table is provided in the appendix (pp 13–23); the studies included here are those that more comprehensively reported patient data or reported novel findings. SARS-CoV-2=severe acute respiratory syndrome coronavirus 2. HSV=herpes simplex virus. VZV=varicella zoster virus. CRP=C-reactive protein. ICU=intensive care unit. PaO2=partial pressure of oxygen. PCO2=partial pressure of carbon dioxide. LDH=lactate dehydrogenase. MOG=myelin oligodendrocyte glycoprotein. NR=not reported. WNV=West Nile virus. FLAIR=fluid-attenuated inversion recovery. HHV=human herpes virus. EBV=Epstein-Barr virus. CMV=cytomegalovirus. RSV=respiratory syncytial virus. LDH=lactate dehydrogenase. GCS=Glasgow Coma Scale.
Encephalitis
Encephalitis is the inflammation of the brain parenchyma, usually caused by an infection or the body's immune defences. Although it is strictly speaking a pathological diagnosis, for practical purposes, clinical evidence of brain inflammation is accepted, such as a CSF pleiocytosis, imaging changes, or focal abnormalities on EEG. Detection of virus in the CSF per se does not provide a diagnosis of encephalitis if there is no evidence of brain inflammation (panel; appendix p 6).57
As of May 19, 2020, eight adults aged 24–78 years (median 62 [IQR 40–70]), including four women, have been described with encephalitis associated with COVID-19, mostly diagnosed through a nasal or nasopharyngeal swab (table 2; appendix pp 13–14).31, 32, 33, 58, 59, 60, 61 Neurological features mostly started from the time of respiratory symptom onset to 17 days afterwards, although in one man aged 60 years, confusion preceded cough and fever by two days (figure 1 ).58 Two patients had fever only, with no respiratory features.59, 60 The neurological manifestations were typical for encephalitis, with irritability, confusion, and reduced consciousness, sometimes associated with seizures; three patients also had neck stiffness31, 58, 59 and another had psychotic symptoms.61 A man aged 40 years developed ataxia, oscillopsia, hiccups, and bilateral facial weakness.33 CSF analysis was reported for six patients; it showed a pleiocytosis in five, mostly lymphocytic, and was normal in one patient. Four patients had CSF PCR done for SARS-CoV-2, of whom one was positive: a man aged 24 years with encephalitis, minor respiratory symptoms, and ground glass changes on chest CT, who had a PCR negative respiratory sample.31 Few publications reported comprehensive investigation for other causes of encephalitis (table 2; appendix pp 13–14). Brain imaging was normal or had no acute changes for six patients, and showed high signal intensity in two, including temporal lobe changes in one (figure 2A, B );31 the patient with ataxia had a cerebellar lesion that extended into the spinal cord.33 EEG was done in five patients.32, 58, 59, 60, 61 Two had generalised slowing, two had focal abnormalities, and one patient, who presented with psychotic symptoms followed by a seizure, was found to be in non-convulsive status epilepticus.61 One patient responded quickly to high dose steroids,58 but for the other seven no specific treatment was reported beyond anticonvulsants, antiviral, and antibiotic medication.
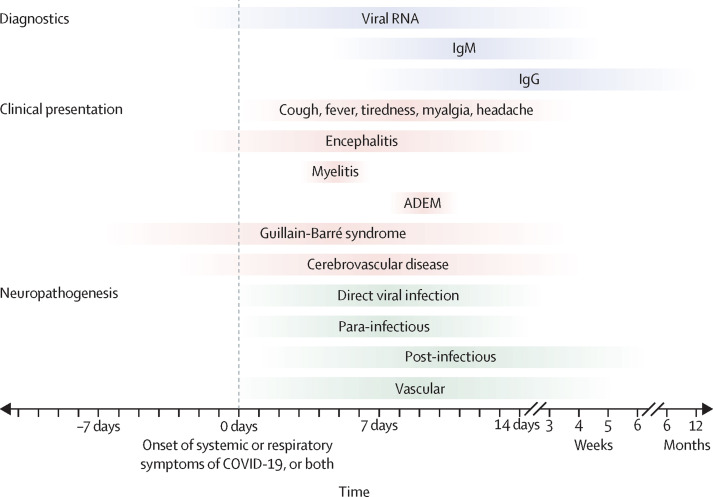
Figure 1.
Approximate timeline for positive diagnostic tests, clinical presentation, and pathogenesis in COVID-19-associated neurological disease
Approximate values are based on currently published data. Bars are faded to indicate uncertainty about specific ranges. Blue bars represent the period in which SARS-CoV-2 viral RNA and anti-SARS-CoV-2 IgM or IgG antibodies are detectable on either RT-PCR or antibody testing.62, 63, 64, 65, 66, 67 Red bars represent the time of clinical presentation, including the duration of systemic or respiratory symptoms of COVID-19 and the time interval between onset of COVID-19 symptoms and symptoms of encephalitis,31, 32, 33, 58, 59, 60, 61 myelitis,42 acute disseminated encephalomyelitis,40, 41 Guillain-Barré syndrome,43, 44, 45, 46, 47, 48, 68, 69, 70, 71, 72, 73, 74, 75 or cerebrovascular disease.52, 53, 54, 76, 77, 78, 79 A small number of patients who presented with neurological disease and never had respiratory features of COVID-19 are not represented in the figure. Green bars represent pathological mechanisms that might result in neurological disease in COVID-19, as in other viruses (appendix p 4). The dynamics of anti-SARS-CoV-2 IgG antibody production are not known beyond a few weeks, although by analogy with other viruses, it might be expected to persist for months to years. ADEM=acute disseminated encephalomyelitis. SARS-CoV-2=severe acute respiratory syndrome coronoavirus 2.
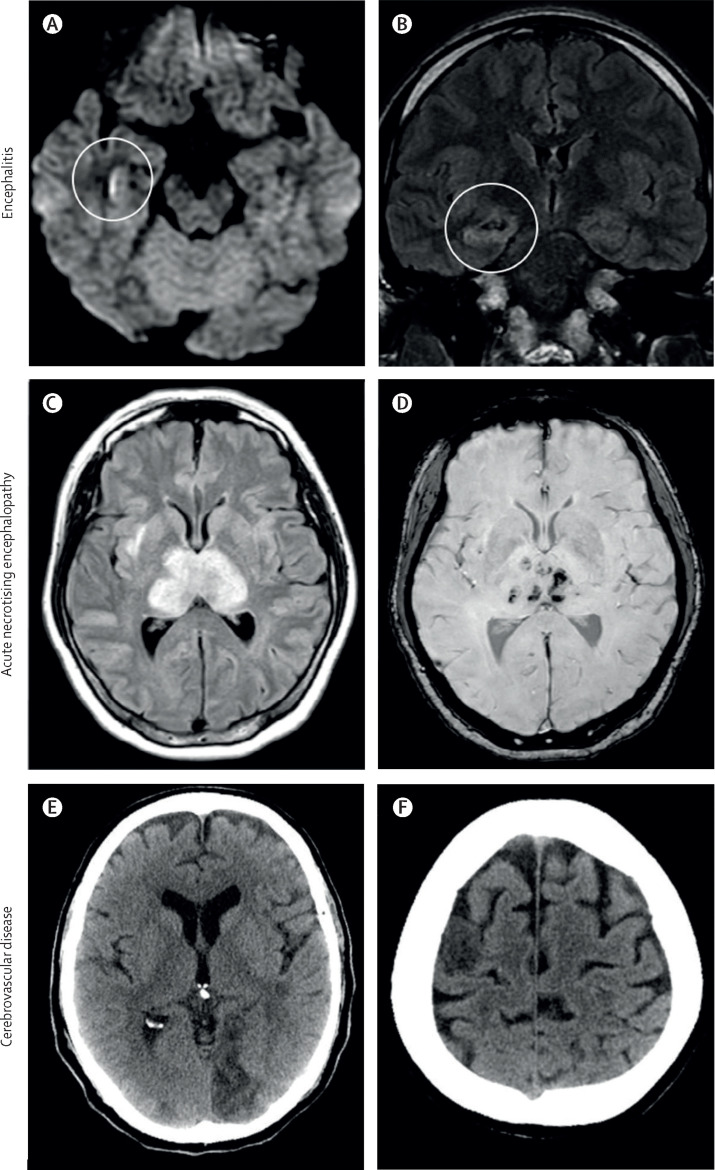
Figure 2.
Brain imaging in patients with neurological disease associated with COVID-19
(A) Hyperintensity along the wall of inferior horn of right lateral ventricle on diffusion-weighted imaging, indicating ventriculitis. (B) hyperintense signal changes in the right mesial temporal lobe and hippocampus with slight hippocampal atrophy on FLAIR MRI, consistent with encephalitis, in a patient with COVID-19.31 (C) Hyperintensity within the bilateral medial temporal lobes and thalami on T2/FLAIR MRI. (D) Evidence of haemorrhage, indicated by hypointense signal on susceptibility-weighted images, consistent with acute necrotising encephalopathy in a patient with confirmed COVID-19.37 (E) CT showing ischaemic lesions involving the left occipital lobe. (F) Right frontal precentral gyrus of the brain in a man aged 64 years who deteriorated neurologically after admission to hospital with COVID-19 and was diagnosed with acute stroke.54 FLAIR=fluid-attenuated inversion recovery. Panels A and B reproduced from Moriguchi et al31 with permission from Elsevier under a creative commons CC BY-NC-ND license; panels C and D reproduced from Poyiadji et al37 with permission from The Radiological Society of North America; and panels E and F reproduced from Morassi et al54 with permission from Springer Nature.
No specific treatment exists for SARS-CoV-2 encephalitis. As for other forms of encephalitis, questions will emerge concerning the relative contributions of viral damage and host inflammatory response, and whether corticosteroids might be useful. Clinical trials seem unlikely, given the current low number of cases.
Other encephalopathies
Encephalopathy is a pathobiological process in the brain that usually develops over hours to days and can manifest as changed personality, behaviour, cognition, or consciousness (including clinical presentations of delirium or coma).80 In patients with encephalopathy and COVID-19, in whom brain inflammation has not been proven, the wide range of other causes to consider includes hypoxia, drugs, toxins, and metabolic derangements (appendix pp 2–3).57
The largest study to date,36 from Wuhan, China, retrospectively described 214 patients with COVID-19, of whom 53 (25%) had CNS symptoms, including dizziness (36 [17%] patients), headache (28 [13%]), and impaired consciousness (16 [7%]). 27 (51%) of the patients with CNS symptoms had severe respiratory disease, but there was little further detail (table 2; appendix pp 14–15).36 In a French series of 58 intensive care patients with COVID-19,35 49 (84%) had neurological complications, including 40 (69%) with encephalopathy and 39 (67%) with corticospinal tract signs. MRI in 13 patients showed leptomeningeal enhancement for eight and acute ischaemic change for two; CSF examination for seven patients showed no pleiocytosis. 15 (33%) of 45 patients who had been discharged had a dysexecutive syndrome. Additionally, some case reports have appeared, including a woman with encephalopathy with imaging changes consistent with acute necrotising encephalopathy (figure 2C, D)37 and a fatal case in which viral particles were found in endothelial cells and neural tissue, although there was no indication of whether this was associated with inflammation.38
Several reports have described seizures in children with SARS-CoV-2 infection. Paroxysmal episodes consistent with seizures were described in two infants with no respiratory symptoms but SARS-CoV-2 on nasopharyngeal swab;34, 81 both made a good recovery. In one series of 168 children hospitalised with COVID-19,82 seizures were described for five (3%) children, of whom three had pre-existing epilepsy and one had previous febrile seizures.
Acute disseminated encephalomyelitis and myelitis
Acute disseminated encephalomyelitis is a syndrome of multifocal demyelination, typically occurring weeks after an infection, which generally presents with focal neurological symptoms, often with encephalopathy (appendix p 7).83 Two case reports40, 41 describe middle-aged women with acute disseminated encephalomyelitis and SARS-CoV-2 detected on respiratory swabs (table 2; appendix p 16). One developed dysphagia, dysarthria, and encephalopathy 9 days after the onset of headache and myalgia (figure 1).41 The other presented with seizures and reduced consciousness, and required intubation for respiratory failure.40 Both patients had normal CSF and high signal intensities on MRI, typical of acute disseminated encephalomyelitis. They both improved after treatment, one with intravenous immunoglobulin and one with steroids. To date, a single report exists of myelitis (inflammation of the spinal cord; appendix p 8) associated with COVID-19. A man aged 66 years in Wuhan, China, developed fever, fatigue, and then acute flaccid paraparesis with incontinence. Examination showed hyporeflexia and a sensory level at T10. He was treated with dexamethasone and intravenous immunoglobulin, and was discharged for rehabilitation.42
Acute disseminated encephalomyelitis and myelitis, usually considered post-infectious diseases, are treated typically with corticosteroids or other immunotherapies. In these para-infectious cases, with SARS-CoV-2 detectable at presentation, clinicians might need to be more cautious, especially if the virus is detected in the CSF, because such treatment might diminish the patient's immune response to the virus.
Peripheral nervous system and muscle disease
Guillain-Barré syndrome is an acute polyradiculopathy characterised by rapidly progressive, symmetrical limb weakness, areflexia on examination, sensory symptoms, and, in some patients, facial weakness, although several variants exist (appendix p 9). To date, 19 patients (six female) with Guillain-Barré syndrome or its variants and COVID-19 have been reported, with a median age of 63 years (range 23 to 77; table 2; appendix pp 16–18). Given the number of SARS-CoV-2 infections worldwide, the incidence is not particularly higher than what might be expected.84 Neurological symptoms started at a median of 7 days (range −7 to 24) after respiratory or systemic features (figure 1), although two patients developed febrile illness 7 days after the onset of Guillain-Barré syndrome;45, 68 on hospital admission, one had a positive swab for SARS-CoV-2 and the other had lymphocytopenia and thrombocytopenia, which are characteristic for SARS-CoV-2 infection. Three patients had diarrhoea before the onset of neurological disease.
11 patients had Guillain-Barré syndrome with weakness of all four limbs with or without sensory loss,43, 44, 45, 69, 70, 71, 72, 73, 74 three had a paraparetic variant with leg weakness only,44, 68, 75 and one had lower limb paraesthesia.44 Four of these patients had facial nerve involvement, five had dysphagia, and eight developed respiratory failure. Three had autonomic complications, one with hypertension and two with sphincter dysfunction. Electrophysiological studies were done in 12 patients and were consistent with demyelinating disease in eight and axonal disease in four patients.
Two patients had the Miller Fisher variant of Guillain-Barré syndrome, with ophthalmoplegia, ataxia, and areflexia;46, 47 one also had loss of smell and taste, and was positive for anti-GD1b-IgG. One patient had bilateral and one patient unilateral abducens palsy,46, 47 and another had an acute vestibular syndrome with horizontal nystagmus and oscillopsia.48
For 16 patients, SARS-CoV-2 was detected in a respiratory swab, and for two, the sample was not specified; one patient was also positive for rhinovirus. One patient was diagnosed by a blood antibody test. Lumbar puncture was done in 13 patients and showed albuminocytological dissociation in 11. SARS-CoV-2 was not detected in any CSF samples. Testing for other pathogens commonly associated with Guillain-Barré syndrome was reported for only four patients.43, 44, 73, 75 15 patients were treated with intravenous immunoglobulin, and eight (all with classical Guillain-Barré syndrome) were admitted to intensive care for ventilatory support, two of whom died.70, 71 12 improved, and five had ongoing disability at discharge.
Muscle injury associated with raised creatine kinase affected 23 (11%) of 214 patients in the Wuhan series.57 Rhabdomyolysis due to COVID-19 has also been reported.85, 86
Loss of smell (anosmia) and taste (ageusia) have emerged as common symptoms of COVID-19, either with other features or in isolation, suggesting that they might be useful diagnostic markers (appendix p 19).87 A study of 259 patients,88 including 68 who were positive for SARS-CoV-2, found that abnormal smell and taste were both strongly associated with COVID-19. In a European study,50 olfactory dysfunction was reported for 357 (86%) of 417 COVID-19 patients; 342 (82%) reported gustatory disorders. These symptoms were reported more frequently for COVID-19 patients than for a historical cohort of influenza patients.89 Subclinical deficits in smell, taste, or both have also been detected.90, 91 Although these symptoms can occur in any respiratory infection because of coryza, the fact they occur in isolation of other symptoms suggest that there is involvement of the olfactory nerve.
Cerebrovascular manifestations
As COVID-19 has spread around the world, evidence has grown for an association with cerebrovascular disease, as well as with other forms of vascular disease. Cerebrovascular manifestations were reported for 13 (6%) of 221 COVID-19 patients in an early retrospective case series from Wuhan:53 11 (5%) patients developed ischaemic stroke, one (<1%) had intracerebral haemorrhage, and one (<1%) had cerebral venous sinus thrombosis. In Milan, Italy, nine (2%) of 388 retrospectively identified hospital patients with laboratory-confirmed COVID-19 had a stroke.92 Another centre in Italy reported that 43 (77%) of 56 SARS-CoV-2-positive patients admitted to one neurology unit had cerebrovascular disease; 35 had ischaemic stroke and three haemorrhagic stroke, and five had transient ischaemic attacks.93 In the Netherlands, three (2%) of 184 patients in intensive care with COVID-19 had ischaemic strokes.94 In total, 88 patients with ischaemic stroke and eight with haemorrhagic stroke53, 54, 56, 77, 93 have been reported, 18 (19%) of whom died (table 2; appendix pp 20–23).
Most patients were older than 60 years, and many had known risk factors for cerebrovascular disease, especially hypertension, diabetes, hyperlipidaemia, and vascular disease.51, 52, 53, 54, 77, 78 Younger stroke patients have also been reported.52, 55, 56, 92, 95 In one hospital in New York, NY, USA, five patients younger than 50 years with stroke and SARS-CoV2 were admitted in just 2 weeks, whereas the average number of admissions for young patients with stroke per 2 weeks in the preceding year was 0·73.55 Two patients had no other symptoms of COVID-19. All had large vessel ischaemic strokes.
Cerebrovascular symptoms began at a median of 10 days (range 0–33) after the onset of respiratory illness (figure 1), although in one patient the stroke preceded respiratory features36 and five had only cerebrovascular symptoms.51, 55, 56, 95
In two patients, ischaemic stroke has been associated with thrombus in the aorta,95, 96 and indeed multiple infarcts have been reported in these and other patients (figure 2E, F),52, 77, 79 sometimes associated with arterial thrombosis and limb ischaemia.77, 79 Concurrent deep vein thrombosis and pulmonary embolism have been found in other stroke patients.52, 95 Arterial and venous imaging is clearly essential for COVID-19 patients with acute cerebrovascular events. Small asymptomatic infarcts identified on MRI only have also been described.35 Blood D-dimer concentration was raised in many patients with COVID-19, consistent with a pro-inflammatory, coagulopathic state in the setting of critical illness.51, 52, 53, 54, 55, 77, 92, 95, 96 Positive lupus anticoagulant, anticardiolipin, and anti-β2-glycoprotein-1 antibodies have also been reported in COVID-19-associated stroke,52, 77 although these can be raised in other critical illnesses, including infections.
Immediate anticoagulation with low-molecular-weight heparin has been recommended for patients with COVID-19, to reduce the risk of thrombotic disease.97 This approach might also reduce COVID-19-associated ischaemic stroke, but it must be balanced against the risk of intracranial haemorrhage, including haemorrhagic transformation of an acute infarct. Several randomised trials are looking at the role of anticoagulation in patients with COVID-19 (NCT04362085, NCT04345848, NCT04406389), including the effect on stroke incidence.
Disease mechanisms
Infection and inflammation of the central and peripheral nervous systems
As with other neurotropic viruses, key questions for SARS-CoV-2 infection concern the routes of entry into the nervous system and the relative contribution of viral infection versus host response to the subsequent damage (appendix p 12).
Viral entry to the brain through the olfactory bulb—the only part of the CNS not protected by dura—is one plausible route for SARS-CoV-2, especially given the anosmia in COVID-19. This entry route is thought to be used by the herpes simplex virus, the most common cause of sporadic viral encephalitis.98 In mouse models, following intranasal injection, human coronavirus OC43 invades the CNS by the olfactory route.99 Alternative entry routes include carriage across the blood–brain barrier, following viraemia, or through infected leukocytes.3 The angiotensin converting enzyme 2 receptor, to which SARS-CoV-2 binds for entry into cells,100 is found in brain vascular endothelium and smooth muscle.101 SARS-CoV-2 replicates in neuronal cells in vitro.102
Damage within the CNS or PNS might be caused directly by the virus or by the body's innate and adaptive immune responses to infection. Data so far do not suggest that SARS-CoV-2 or related coronaviruses are highly neurovirulent, unlike herpes simplex virus, some enteroviruses, and some arthropod-borne viruses, which can cause rampant destruction of neurons.98
Autopsy material from a patient who developed encephalopathy weeks after presenting with SARS showed oedema, neuronal necrosis, and broad gliocyte hyperplasia.8 Immunohistochemical staining showed that SARS-CoV in the brain was associated with elevated expression of the cytokine, monokine induced by gamma interferon (known as MIG or CXCL9), and with infiltration of monocytes and macrophages plus T cells. These findings are consistent with viral CNS entry triggering the infiltration of immune cells and the release of cytokines and chemokines, which contribute to tissue damage.
Little work has been done on disease mechanisms for coronavirus PNS disease. By comparison with other viruses, it would not be surprising to see immune-mediated disease, such as Guillain-Barré syndrome, and direct anterior horn cell viral damage, which causes acute flaccid myelitis, might also be expected.103
Cerebrovascular disease
Early indicators suggest that cerebrovascular disease in COVID-19 might be due to a coagulopathy. SARS-CoV-2 can cause damage to endothelial cells, activating inflammatory and thrombotic pathways.104 Endothelial cell infection or monocyte activation, upregulation of tissue factors, and the release of microparticles, which activate the thrombotic pathway and cause microangiopathy, might occur for SARS-CoV-2 as for other viruses.105, 106 Monocyte activation is postulated to constitute part of the secondary haemophagocytic lymphohistiocytosis described in severe COVID-19.107 Thrombocytopenia with elevated D-dimer and C-reactive protein in severe COVID-19 and stroke are consistent with a virus-associated microangiopathic process.53 Endothelial dysfunction can potentially lead to microvascular and macrovascular complications in the brain, as described systemically.94
Acute ischaemic stroke might also occur through the early inflammatory process, following acute infection, destabilising a carotid plaque or triggering atrial fibrillation.108 A vasculitis process similar to that for varicella zoster virus, in which viral replication in the cerebral arterial wall triggers local inflammation,109 is also plausible; endothelial infection by SARS-CoV-2 with inflammation and apoptosis of endothelial cells has been shown in kidney, heart, bowel, and lung at autopsy,104 but cerebral vessels have not yet been investigated.
Investigating for neurological disease
As SARS-CoV-2 continues to spread and patients with neurological symptoms are seen increasingly, it is essential that the desire to publish quickly is balanced with the need for careful clinical, diagnostic, and epidemiological studies. Clinicians must adopt a methodical approach to investigating patients with possible COVID-19-associated neurological disease, and must systematically consider the evidence for viral infection and the presenting clinical diagnosis, using definitions that distinguish confirmed, probable, and possible cases (panel; appendix pp 5–12).
Given that SARS-CoV-2 causes a large number of asymptomatic or mildly symptomatic infections, it is crucial to remember that patients with neurological disease from other causes might be infected coincidentally with the virus, including in hospital through nosocomial transmission. A full investigation, which is absent in many reports to date, is needed to rule out other established causes of brain infections before attributing disease to COVID-19.57, 110 Distinguishing between nasopharyngeal SARS-CoV-2 infection and nervous system infection is also key.
For patients with altered consciousness or agitation, all causes of encephalopathy must be considered, including hypoxia, drugs, toxins, and metabolic derangement; encephalitis should be diagnosed only if clinical evidence exists of brain inflammation, such as a CSF pleiocytosis, imaging changes, focal seizures, or histological changes (appendix p 6).57 Even if virus is detected in the CSF, encephalitis should not be diagnosed unless evidence exists of brain inflammation. For patients with possible peripheral nerve disease, clinicians should aim to do CSF examination, looking for evidence of albuminocytological dissociation (an elevated CSF protein level with a normal CSF cell count), nerve conduction studies, and electromyography during recovery, even if they cannot be done acutely.
In patients with neuropathy, cerebrovascular disease, or acute disseminated encephalomyelitis, in whom the damage is probably caused by the host's response to viral infection, establishing causality is even more challenging, especially if patients present after the virus has been cleared from the nasopharynx. Clinical case definitions for COVID-19 that are based on the history and typical findings for chest imaging and blood investigations will be useful (panel). For patients with stroke, clinicians should consider cerebral angiography, intracranial vessel wall imaging, and, if necessary, brain biopsy, looking for vasculitis. The apparently high incidence of cerebrovascular disease in patients with COVID-19, with predominantly large vessel disease and markers of a highly prothrombotic state, suggest a causal relationship. However, the high prevalence of the virus during the pandemic, and the fact that most stroke patients have other risk factors, mean that it is hard to be sure about causation. The link with SARS-CoV-2 will ultimately need to be proven by careful case-control studies.
In investigating patients with limb weakness and sensory change, it is crucial to distinguish between disease of the peripheral nerves (eg, Guillain-Barré syndrome) and inflammation of the spinal cord, which can present with flaccid paralysis if the anterior horn cells are involved.103 CSF examination, neurophysiological studies, and spinal imaging are essential.
For patients on intensive care, determining whether neuropathy, myopathy, encephalopathy, or cerebrovascular disease are non-specific manifestations of critical illness or are specific to the virus itself might be particularly challenging; no reliable markers exist for neurological disease caused by critical illness, although it tends to occur after several weeks.10 Up to 70% of patients with sepsis might develop encephalopathy or polyneuropathy.111 In the Wuhan series, neurological complications were more common in those with severe disease, suggesting that some of the neurological manifestations were related to critical illness.36, 112
Conclusion and future directions
Given existing knowledge of other coronaviruses and respiratory viruses, the wide range of CNS and PNS associations with COVID-19 is not surprising, and this is the focus of most current reports. However, neurological disease is also likely to be seen increasingly in patients who are SARS-CoV-2-positive but with few or no typical features of COVID-19, based on knowledge of other epidemic viral infections and cases reported so far.28 Case-control studies will be needed to help establish whether SARS-CoV-2 is causal or coincidental in such patients. Hypercoagulable states and cerebrovascular disease, which have been seen rarely for some acute viral infections, are an important neurological complication of COVID-19.
Overall, the proportion of patients with neurological manifestations is small compared with that with respiratory disease. However, the continuing pandemic, and the expectation that 50–80% of the world's population might be infected before herd immunity develops, suggest that the overall number of patients with neurological disease could become large. Neurological complications, particularly encephalitis and stroke, can cause lifelong disability, with associated long-term care needs and potentially large health, social, and economic costs. Health-care planners and policy makers need to be aware of the growing burden.
Careful clinical, diagnostic, and epidemiological studies are needed to help define the neurological disease manifestations and burden. This work will involve the collaboration of a range of clinical and research expertise, and harmonised approaches across regions; smaller case series and registries should be combined into meta-analyses such as that of the COVID-19 Neuro Network run through Brain Infections Global, which is also providing standardised case record forms and case definitions.
Search strategy and selection criteria
We searched PubMed and Scopus for articles on COVID-19 from database inception to May 19, 2020, without language restrictions, using the terms “COVID-19”, “novel coronavirus”, “SARS-CoV-2”, or “coronavirus” in combination with “neurological”, “nervous system”, “encephalitis”, “encephalopathy”, “seizure”, “ataxia”, “myelopathy”, “Guillain-Barré syndrome”, “myopathy”, “peripheral neuropathy”, “neuritis”, “cerebrovascular”, “stroke”, “neuromuscular”, or “brain”, modified as per requirements for the search tool of each database. We reviewed the references of relevant studies for additional articles and consulted experts in the field to ensure that we did not miss important preprints and unpublished studies. Articles were included on the basis of relevance and originality with regards to the topics covered in this Rapid Review.
Acknowledgments
Acknowledgments
MAE, SL, and TS are supported by the European Union's Horizon 2020 research and innovation programme, ZikaPLAN (Preparedness Latin America Network; grant 734584). Additionally, MAE is supported by the Association of British Neurologists though a Clinical Research Training Fellowship. BS, SL, BDM, and TS are supported by the National Institute for Health Research (NIHR) Global Health Research Group on Brain Infections (17/63/110) and the NIHR Health Protection Research Unit in Emerging and Zoonotic Infections at University of Liverpool in partnership with Public Health England, in collaboration with Liverpool School of Tropical Medicine and the University of Oxford (NIHR200907). The views expressed are those of the authors and not necessarily those of the National Health Service, the NIHR, the Department of Health, or Public Health England. BDM has received funding from the Medical Research Council, Wellcome Trust, and Academy of Medical Sciences. We are also grateful for the support of Liverpool Health Partners and the Centre of Excellence in Infectious Disease Research, Liverpool.
Contributors
MAE, BDM, JS, and TS devised the idea for this Rapid Review. MAE, LB, BS, SL, BDM, RK, SD, JS, and TS contributed to the literature search. MAE, LB, BS, SL, BDM, and TS designed and drafted the figures. MAE, LB, BS, SL, BDM, RK, SD, JS, and TS prepared the initial manuscript draft. All authors contributed to, reviewed, and approved the final draft of the paper.
Declaration of interests
TS was an adviser to the GlaxoSmithKline Ebola Vaccine programme, chaired a Siemens Diagnostics clinical advisory board, and advises the WHO Brain Health Unit Forum on Neurology and COVID-19; TS has also previously filed a patent for a test for bacterial meningitis based on a blood test (GB 1606537.7, April 14, 2016). All other authors declare no competing interests.
Footnotes
Definitions for the different neurological diseases and syndromes are in the appendix (pp 5–12).
Detection in CSF or brain tissue by PCR, culture, or immunohistochemistry, as appropriate.
Serological evidence of acute infection can be defined as detection of IgM, IgG seroconversion, or an increase of four times in antibody titres in paired acute and convalescent serum samples.
Detection in non-CNS sample by PCR or culture.
These include infection with one of Campylobacter jejuni, Mycoplasma pneumoniae, Cytomegalovirus, Epstein–Barr virus, hepatitis E virus, Zika virus, or HIV; or vaccination in the last 6 weeks. Associated causes might differ depending on geographical location.
Traditional cardiovascular risk factors include hypertension, current smoker, diabetes, hypercholesterolaemia, and atrial fibrillation.
Supplementary Material
References
- 1.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taubenberger JK, Morens DM. 1918 influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12:15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desforges M, Le Coupanec A, Dubeau P, et al. Human coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? Viruses. 2019;12:12. doi: 10.3390/v12010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ksiazek TG, Erdman D, Goldsmith CS, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 5.Saad M, Omrani AS, Baig K, et al. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis. 2014;29:301–306. doi: 10.1016/j.ijid.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hung EWC, Chim SSC, Chan PKS, et al. Detection of SARS coronavirus RNA in the cerebrospinal fluid of a patient with severe acute respiratory syndrome. Clin Chem. 2003;49:2108–2109. doi: 10.1373/clinchem.2003.025437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lau KK, Yu WC, Chu CM, Lau ST, Sheng B, Yuen KY. Possible central nervous system infection by SARS coronavirus. Emerg Infect Dis. 2004;10:342–344. doi: 10.3201/eid1002.030638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu J, Zhong S, Liu J, et al. Detection of severe acute respiratory syndrome coronavirus in the brain: potential role of the chemokine mig in pathogenesis. Clin Infect Dis. 2005;41:1089–1096. doi: 10.1086/444461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsai LK, Hsieh ST, Chao CC, et al. Neuromuscular disorders in severe acute respiratory syndrome. Arch Neurol. 2004;61:1669–1673. doi: 10.1001/archneur.61.11.1669. [DOI] [PubMed] [Google Scholar]
- 10.Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive Care Med. 2020;46:637–653. doi: 10.1007/s00134-020-05944-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Algahtani H, Subahi A, Shirah B. Neurological complications of Middle East respiratory syndrome coronavirus: a report of two cases and review of the literature. Case Rep Neurol Med. 2016;2016 doi: 10.1155/2016/3502683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arabi YM, Harthi A, Hussein J, et al. Severe neurologic syndrome associated with Middle East respiratory syndrome corona virus (MERS-CoV) Infection. 2015;43:495–501. doi: 10.1007/s15010-015-0720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim JE, Heo JH, Kim HO, et al. Neurological complications during treatment of Middle East respiratory syndrome. J Clin Neurol. 2017;13:227–233. doi: 10.3988/jcn.2017.13.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morfopoulou S, Brown JR, Davies EG, et al. Human coronavirus OC43 associated with fatal encephalitis. N Engl J Med. 2016;375:497–498. doi: 10.1056/NEJMc1509458. [DOI] [PubMed] [Google Scholar]
- 15.Yeh EA, Collins A, Cohen ME, Duffner PK, Faden H. Detection of coronavirus in the central nervous system of a child with acute disseminated encephalomyelitis. Pediatrics. 2004;113:e73–e76. doi: 10.1542/peds.113.1.e73. [DOI] [PubMed] [Google Scholar]
- 16.Li Y, Li H, Fan R, et al. Coronavirus infections in the central nervous system and respiratory tract show distinct features in hospitalized children. Intervirology. 2016;59:163–169. doi: 10.1159/000453066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goenka A, Michael BD, Ledger E, et al. Neurological manifestations of influenza infection in children and adults: results of a National British Surveillance Study. Clin Infect Dis. 2014;58:775–784. doi: 10.1093/cid/cit922. [DOI] [PubMed] [Google Scholar]
- 18.Studahl M. Influenza virus and CNS manifestations. J Clin Virol. 2003;28:225–232. doi: 10.1016/s1386-6532(03)00119-7. [DOI] [PubMed] [Google Scholar]
- 19.Gu Y, Shimada T, Yasui Y, Tada Y, Kaku M, Okabe N. National surveillance of influenza-associated encephalopathy in Japan over six years, before and during the 2009–2010 influenza pandemic. PLoS One. 2013;8 doi: 10.1371/journal.pone.0054786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kwon S, Kim S, Cho M, Seo H. Cho M Hyun, Seo H. Neurologic complications and outcomes of pandemic (H1N1) 2009 in Korean children. J Korean Med Sci. 2012;27:402. doi: 10.3346/jkms.2012.27.4.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khandaker G, Zurynski Y, Buttery J, et al. Neurologic complications of influenza A(H1N1)pdm09: surveillance in 6 pediatric hospitals. Neurology. 2012;79:1474–1481. doi: 10.1212/WNL.0b013e31826d5ea7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glaser CA, Winter K, DuBray K, et al. A population-based study of neurologic manifestations of severe influenza A(H1N1)pdm09 in California. Clin Infect Dis. 2012;55:514–520. doi: 10.1093/cid/cis454. [DOI] [PubMed] [Google Scholar]
- 23.Foley PB. Encephalitis lethargica and influenza. I. The role of the influenza virus in the influenza pandemic of 1918/1919. J Neural Transm (Vienna) 2009;116:143–150. doi: 10.1007/s00702-008-0161-1. [DOI] [PubMed] [Google Scholar]
- 24.Tobi H, van den Berg PB, de Jong-van den Berg LTW. Small proportions: what to report for confidence intervals? Pharmacoepidemiol Drug Saf. 2005;14:239–247. doi: 10.1002/pds.1081. [DOI] [PubMed] [Google Scholar]
- 25.Varatharaj A, Thomas N, Ellul M, et al. UK-wide surveillance of neurological and neuropsychiatric complications of COVID-19: the first 153 patients. SSRN. 2020 doi: 10.1016/S2215-0366(20)30287-X. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3601761 published online May 22. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.WHO . World Health Organization; Geneva: 2020. Coronavirus disease 2019 (COVID-19): situation report, 61. [Google Scholar]
- 27.WHO . World Health Organization; Geneva: 2020. Laboratory testing for coronavirus disease 2019 (2019-nCoV) in suspected human cases. [Google Scholar]
- 28.Solomon T, Dung NM, Vaughn DW, et al. Neurological manifestations of dengue infection. Lancet. 2000;355:1053–1059. doi: 10.1016/S0140-6736(00)02036-5. [DOI] [PubMed] [Google Scholar]
- 29.Granerod J, Cunningham R, Zuckerman M, et al. Causality in acute encephalitis: defining aetiologies. Epidemiol Infect. 2010;138:783–800. doi: 10.1017/S0950268810000725. [DOI] [PubMed] [Google Scholar]
- 30.Mehta R, Soares CN, Medialdea-Carrera R, et al. The spectrum of neurological disease associated with Zika and chikungunya viruses in adults in Rio de Janeiro, Brazil: a case series. PLoS Negl Trop Dis. 2018;12 doi: 10.1371/journal.pntd.0006212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moriguchi T, Harii N, Goto J, et al. A first case of meningitis/encephalitis associated with SARS-coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sohal S, Mossammat M. COVID-19 presenting with seizures. IDCases. 2020;20 doi: 10.1016/j.idcr.2020.e00782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong PF, Craik S, Newman P, et al. Lessons of the month 1: a case of rhombencephalitis as a rare complication of acute COVID-19 infection. Clin Med (Lond) 2020 doi: 10.7861/clinmed.2020-0182. https://doi.org.10.7861/clinmed.2020-0182 published online May 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dugue R, Cay-Martínez KC, Thakur KT, et al. Neurologic manifestations in an infant with COVID-19. Neurology. 2020 doi: 10.1212/WNL.0000000000009653. https://doi.org.10.1212/WNL.0000000000009653 published online April 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. https://doi.org.10.1001/jamaneurol.2020.1127 published online April 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020 doi: 10.1148/radiol.2020201187. https://doi.org.10.1148/radiol.2020201187 published online March 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paniz-Mondolfi A, Bryce C, Grimes Z, et al. Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) J Med Virol. 2020;92:699–702. doi: 10.1002/jmv.25915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou L, Zhang M, Wang J, Gao J. Sars-Cov-2: underestimated damage to nervous system. Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101642. published online March 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zanin L, Saraceno G, Panciani PP, et al. SARS-CoV-2 can induce brain and spine demyelinating lesions. Acta Neurochir (Wien) 2020 doi: 10.1007/s00701-020-04374-x. https://doi.org.10.1007/s00701-020-04374-x published online May 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang T, Rodricks MB, Hirsh E. COVID-19-associated acute disseminated encephalomyelitis: a case report. medRxiv. 2020 https://doi.org.2020.04.16.20068148 (preprint). [Google Scholar]
- 42.Zhao K, Huang J, Dai D, Feng Y, Liu L, Nie S. Acute myelitis after SARS-CoV-2 infection: a case report. medRxiv. 2020 https://doi.org.2020.03.16.20035105 (preprint). [Google Scholar]
- 43.Camdessanche J-P, Morel J, Pozzetto B, Paul S, Tholance Y, Botelho-Nevers E. COVID-19 may induce Guillain-Barré syndrome. Rev Neurol (Paris) 2020;176:516–518. doi: 10.1016/j.neurol.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Toscano G, Palmerini F, Ravaglia S, et al. Guillain-Barré syndrome associated with SARS-CoV-2. N Engl J Med. 2020 doi: 10.1056/NEJMc2009191. published online April 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhao H, Shen D, Zhou H, Liu J, Chen S. Guillain-Barre syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19:383–384. doi: 10.1016/S1474-4422(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gutiérrez-Ortiz C, Méndez A, Rodrigo-Rey S, et al. Miller Fisher Syndrome and polyneuritis cranialis in COVID-19. Neurology. 2020 doi: 10.1212/WNL.0000000000009619. https://doi.org.10.1212/WNL.0000000000009619 published online April 17. [DOI] [PubMed] [Google Scholar]
- 47.Dinkin M, Gao V, Kahan J, et al. COVID-19 presenting with ophthalmoparesis from cranial nerve palsy. Neurology. 2020 doi: 10.1212/WNL.0000000000009700. https://doi.org.10.1212/WNL.0000000000009700 published online May 1. [DOI] [PubMed] [Google Scholar]
- 48.Escalada Pellitero S, Garriga Ferrer-Bergua L. Report of a patient with neurological symptoms as the sole manifestation of SARS-CoV-2 infection. Neurologia. 2020;35:271. doi: 10.1016/j.nrl.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jin M, Tong Q. Rhabdomyolysis as potential late complication associated with COVID-19. Emerg Infect Dis. 2020 doi: 10.3201/eid2607.200445. https://doi.org.10.3201/eid2607.200445 published online March 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol. 2020 doi: 10.1007/s00405-020-05965-1. https://doi.org.10.1007/s00405-020-05965-1 published online April 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Avula A, Nalleballe K, Narula N, et al. COVID-19 presenting as stroke. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.077. https://doi.org.10.1016/j.bbi.2020.04.077 published online April 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Beyrouti R, Adams ME, Benjamin L, et al. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry. 2020 doi: 10.1136/jnnp-2020-323586. published online April 30. jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li Y, Wang M, Zhou Y, et al. Acute cerebrovascular disease following COVID-19: a single center, retrospective, observational study. 2020. https://media.tghn.org/medialibrary/2020/06/Li_2020_Preprint_Acute_cerebrovascular_disease_COVID19.pdf (preprint). [DOI] [PMC free article] [PubMed]
- 54.Morassi M, Bagatto D, Cobelli M, et al. Stroke in patients with SARS-CoV-2 infection: case series. J Neurol. 2020 doi: 10.1007/s00415-020-09885-2. https://doi.org.10.1007/s00415-020-09885-2 published online May 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oxley TJ, Mocco J, Majidi S, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Al Saiegh F, Ghosh R, Leibold A, et al. Status of SARS-CoV-2 in cerebrospinal fluid of patients with COVID-19 and stroke. J Neurol Neurosurg Psychiatry. 2020 doi: 10.1136/jnnp-2020-323522. https://doi.org.jnnp-2020-323522 published online April 30. [DOI] [PubMed] [Google Scholar]
- 57.Solomon T, Michael BD, Smith PE, et al. Management of suspected viral encephalitis in adults—Association of British Neurologists and British Infection Association National Guidelines. J Infect. 2012;64:347–373. doi: 10.1016/j.jinf.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 58.Pilotto A, Odolini S, Stefano Masciocchi S, et al. Steroid-responsive encephalitis in Coronoavirus disease 2019. Ann Neurol. 2020 doi: 10.1002/ana.25783. https://doi.org.10.1002/ana.25783 published online May 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Duong L, Xu P, Liu A. Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in downtown Los Angeles, early April 2020. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.024. https://doi.org.10.1016/j.bbi.2020.04.024 published online April 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vollono C, Rollo E, Romozzi M, et al. Focal status epilepticus as unique clinical feature of COVID-19: a case report. Seizure. 2020;78:109–112. doi: 10.1016/j.seizure.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bernard-Valnet R, Pizzarotti B, Anichini A, et al. Two patients with acute meningo-encephalitis concomitant to SARS-CoV-2 infection. Eur J Neurol. 2020 doi: 10.1111/ene.14298. https://doi.org.10.1111/ene.14298 published online May 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 63.Lee Y-L, Liao C-H, Liu P-Y, et al. Dynamics of anti-SARS-Cov-2 IgM and IgG antibodies among COVID-19 patients. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.019. https://doi.org.10.1016/j.jinf.2020.04.019 published online April 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jin Y, Wang M, Zuo Z, et al. Diagnostic value and dynamic variance of serum antibody in coronavirus disease 2019. Int J Infect Dis. 2020;94:49–52. doi: 10.1016/j.ijid.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu Y, Yan L-M, Wan L, et al. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020;20:656–657. doi: 10.1016/S1473-3099(20)30232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672–675. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- 67.Xiang F, Wang X, He X, et al. Antibody detection and dynamic characteristics in patients with COVID-19. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa461. https://doi.org.10.1093/cid/ciaa461 published online April 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Abdelnour L, Eltahir Abdalla M, Babiker S. COVID 19 infection presenting as motor peripheral neuropathy. J Formos Med Assoc. 2020;119:1119–1120. doi: 10.1016/j.jfma.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Galán AV, del Saz Saucedo P, Postigo FP, Paniagua EB. Guillain-Barré syndrome associated with SARS-CoV-2 infection. Neurologia. 2020;35:268–269. doi: 10.1016/j.nrl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marta-Enguita J, Rubio-Baines I, Gastón-Zubimendi I. Fatal Guillain-Barre syndrome after infection with SARS-CoV-2. Neurologia. 2020;35:265–267. doi: 10.1016/j.nrl.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Alberti P, Beretta S, Piatti M, et al. Guillain-Barré syndrome related to COVID-19 infection. Neurol Neuroimmunol Neuroinflamm. 2020;7:e741. doi: 10.1212/NXI.0000000000000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Virani A, Rabold E, Hanson T, et al. Guillain-Barré Syndrome associated with SARS-CoV-2 infection. IDCases. 2020;20 doi: 10.1016/j.idcr.2020.e00771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Padroni M, Mastrangelo V, Asioli GM, et al. Guillain-Barré syndrome following COVID-19: new infection, old complication? J Neurol. 2020 doi: 10.1007/s00415-020-09849-6. https://doi.org.10.1007/s00415-020-09849-6 published online April 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.El Otmani H, El Moutawakil B, Rafai M-A, et al. Covid-19 and Guillain-Barré syndrome: more than a coincidence! Rev Neurol (Paris) 2020;176:518–519. doi: 10.1016/j.neurol.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Coen M, Jeanson G, Culebras Almeida LA, et al. Guillain-Barré syndrome as a complication of SARS-CoV-2 infection. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.074. https://doi.org.10.1016/j.bbi.2020.04.074 published online April 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sharifi-Razavi A, Karimi N, Rouhani N. COVID-19 and intracerebral haemorrhage: causative or coincidental? New Microbes New Infect. 2020;35 doi: 10.1016/j.nmni.2020.100669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhai P, Ding Y, Li Y. The impact of COVID-19 on ischemic stroke: a case report. Research Square. 2020 doi: 10.21203/rs.3.rs-20393/v1. published online March 31. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moshayedi P, Ryan TE, Mejia LLP, Nour M, Liebeskind DS. Triage of acute ischemic stroke in confirmed COVID-19: large vessel occlusion associated with coronavirus infection. Front Neurol. 2020;11:353. doi: 10.3389/fneur.2020.00353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Slooter AJ, Otte WM, Devlin JW, et al. Updated nomenclature of delirium and acute encephalopathy: statement of ten Societies. Intensive Care Med. 2020;46:1020–1022. doi: 10.1007/s00134-019-05907-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chacón-Aguilar R, Osorio-Cámara JM, Sanjurjo-Jimenez I, González-González C, López-Carnero J, Pérez-Moneo-Agapito B. COVID-19: fever syndrome and neurological symptoms in a neonate. An Pediatr. 2020 doi: 10.1016/j.anpede.2020.04.001. https://doi.org.10.1016/j.anpede.2020.04.001 published online April 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Garazzino S, Montagnani C, Donà D, et al. Multicentre Italian study of SARS-CoV-2 infection in children and adolescents, preliminary data as at 10 April 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.18.2000600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pohl D, Alper G, Van Haren K, et al. Acute disseminated encephalomyelitis. Neurology. 2016;87(9 Suppl 2):S38–S45. doi: 10.1212/WNL.0000000000002825. [DOI] [PubMed] [Google Scholar]
- 84.Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barré syndrome. Lancet. 2016;388:717–727. doi: 10.1016/S0140-6736(16)00339-1. [DOI] [PubMed] [Google Scholar]
- 85.Jin M, Tong Q. Rhabdomyolysis as potential late complication associated with COVID-19. Emerg Infect Dis. 2020 doi: 10.3201/eid2607.200445. https://doi.org.10.3201/eid2607.200445 published online March 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Suwanwongse K, Shabarek N. Rhabdomyolysis as a presentation of 2019 novel coronavirus disease. Cureus. 2020;12 doi: 10.7759/cureus.7561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Luers JC, Klussmann JP, Guntinas-Lichius O. The Covid-19 pandemic and otolaryngology: what it comes down to? Laryngorhinootologie. 2020;99:287–291. doi: 10.1055/a-1095-2344. [DOI] [PubMed] [Google Scholar]
- 88.Bénézit F, Le Turnier P, Declerck C, et al. Utility of hyposmia and hypogeusia for the diagnosis of COVID-19. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30297-8. published online April 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Beltrán-Corbellini Á, Chico-García JL, Martínez-Poles J, et al. Acute-onset smell and taste disorders in the context of COVID-19: a pilot multicentre polymerase chain reaction based case-control study. Eur J Neurol. 2020 doi: 10.1111/ene.14359. https://doi.org.10.1111/ene.14273 published online April 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Moein ST, Hashemian SMR, Mansourafshar B, Khorram-Tousi A, Tabarsi P, Doty RL. Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol. 2020 doi: 10.1002/alr.22587. https://doi.org.10.1002/alr.22587 published online April 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hornuss D, Lange B, Schröter N, Rieg S, Kern WV, Wagner D. Anosmia in COVID-19 patients. Clin Microbiol Infect. 2020 doi: 10.1016/j.cmi.2020.05.017. https://doi.org.10.1016/j.cmi.2020.05.017 published online May 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;19:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Benussi A, Pilotto A, Premi E, et al. Clinical characteristics and outcomes of inpatients with neurologic disease and COVID-19 in Brescia, Lombardy, Italy. Neurology. 2020 doi: 10.1212/WNL.0000000000009848. https://doi.org.10.1212/WNL.0000000000009848 published online May 22. [DOI] [PubMed] [Google Scholar]
- 94.Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.González-Pinto T, Luna-Rodríguez A, Moreno-Estébanez A, Agirre-Beitia G, Rodríguez-Antigüedad A, Ruiz-Lopez M. Emergency room neurology in times of COVID-19: malignant ischaemic stroke and SARS-CoV-2 infection. Eur J Neurol. 2020 doi: 10.1111/ene.14286. https://doi.org.10.1111/ene.14286 published online April 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lushina N, Kuo JS, Shaikh HA. Pulmonary, cerebral, and renal thromboembolic disease associated with COVID-19 infection. Radiology. 2020 doi: 10.1148/radiol.2020201623. https://doi.org.10.1148/radiol.2020201623 published online April 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Thachil J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–1026. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Solomon T. In: Brain's diseases of the nervous system. 12th edn. Donaghy M, editor. Oxford University Press; Oxford: 2009. Encephalitis, and infectious encephalopathies. [Google Scholar]
- 99.Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82:7264–7275. doi: 10.1128/JVI.00737-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367:1444–1448. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chu H, Chan JF-W, Yuen TT-T, et al. Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study. Lancet Microbe. 2020 doi: 10.1016/S2666-5247(20)30004-5. published April 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Solomon T, Willison H. Infectious causes of acute flaccid paralysis. Curr Opin Infect Dis. 2003;16:375–381. doi: 10.1097/00001432-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 104.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lopes da Silva R. Viral-associated thrombotic microangiopathies. Hematol Oncol Stem Cell Ther. 2011;4:51–59. doi: 10.5144/1658-3876.2011.51. [DOI] [PubMed] [Google Scholar]
- 106.Brisse E, Wouters CH, Andrei G, Matthys P. How viruses contribute to the pathogenesis of hemophagocytic lymphohistiocytosis. Front Immunol. 2017;8 doi: 10.3389/fimmu.2017.01102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Emsley HC, Hopkins SJ. Acute ischaemic stroke and infection: recent and emerging concepts. Lancet Neurol. 2008;7:341–353. doi: 10.1016/S1474-4422(08)70061-9. [DOI] [PubMed] [Google Scholar]
- 109.Gilden D, Cohrs RJ, Mahalingam R, Nagel MA. Varicella zoster virus vasculopathies: diverse clinical manifestations, laboratory features, pathogenesis, and treatment. Lancet Neurol. 2009;8:731–740. doi: 10.1016/S1474-4422(09)70134-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Venkatesan A, Tunkel AR, Bloch KC, et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis. 2013;57:1114–1128. doi: 10.1093/cid/cit458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bolton CF, Young GB, Zochodne DW. The neurological complications of sepsis. Ann Neurol. 1993;33:94–100. doi: 10.1002/ana.410330115. [DOI] [PubMed] [Google Scholar]
- 112.Turtle L. Respiratory failure alone does not suggest central nervous system invasion by SARS-CoV-2. J Med Virol. 2020;92:705–706. doi: 10.1002/jmv.25828. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.