Abstract
Aims
The present observational study aims to describe political actions in place to combat COVID-19 in the South and Central America region (SACA) while protecting individuals with diabetes.
Methods
A survey with 12 questions was shared with all IDF-SACA member organizations, in 18 countries. A descriptive analysis was performed and a multivariate cluster analysis technique pam (partitioning around medoids) was applied.
Results
Two groups of countries were identified. The first group, mostly countries with stricter measures to contain the spread of the virus, reported more difficulties (limitations in accessing basic or health needs) and fears (concerns regarding the impact of the pandemic); whereas most of the second group consisted of countries with less restrictive measures, and reported fewer difficulties. Only 37% responded that a policy was put into place to protect individuals with diabetes, either delivering their medicines and supplies at home (16%) or providing them at once enough for 2–3 months (21%). All respondents reported that one of the main fear was to “be infected and not to receive adequate treatment” and/or “getting infected if going to the hospital or medical appointments”.
Conclusion
Most of the SACA countries failed to implement timely measures to protect individuals with diabetes, which may severely impact individuals, health systems and economies.
Keywords: COVID-19, Diabetes, Pandemic, SARS-CoV-2, South America, Central America
1. Introduction
The COVID-19 pandemic has been testing the capacity to respond and adapt of populations, governments and health systems worldwide. A highly contagious disease that emerged in China, in December 2019, spread unprecedentedly throughout the world in a few months and collapsed health systems of regions and countries considered well prepared [1], [2], [3], [4], [5]. Data show that the time to respond and measures adopted predict outcomes [4], [6], [7], [8]. In the South and Central America region (SACA), Brazil presented the first suspected and the first confirmed cases on January 27th and February 26th, respectively [9]. Notwithstanding, in a region where differences in time and measures to respond were astonishing [10], Brazil did not take advantage of the early alerts and, as a consequence, quickly climbed to one of the highest global position in number of cases, deaths, and case fatality rates [11], [12], [13]. Neighboring countries responded much faster and in a stringent manner, with lockdowns starting in Peru on March 15th [10], followed by many of the other SACA nations, and lasting much longer than initially planned [13], [14].
The first publications about the pandemic in China and Italy revealed that people with diabetes and other noncommunicable diseases were at higher risk for COVID-19 severity and mortality [4], [15], [16], [17], [18], which was shown to be especially associated with hyperglycemia [15], [19]. SACA presents a prevalence of diabetes of 9.4%, which surpasses 31.6 million people with diabetes [20]. The region is also known for its active vector-borne diseases; malaria, dengue and yellow fever should be highlighted because of the current outbreaks in some of the countries and added uncertainty to recommendations and diagnosis where COVID-19 tests are insufficient [13], [21], [22], [23]. Despite all local and global alerts [17], [24], it is unclear whether governments were taking specific measures to protect people with DM that, if infected, would quickly occupy the limited number of ICU beds available, in a region where health systems are already considered fragile [13], [21], [22].
The present study aimed to identify the main public policies in place to fight COVID-19 in the SACA region while protecting individuals with diabetes, and in addition to exploring the main challenges and worries faced by this population during this global health crisis.
2. Method
A survey in Spanish, with 12 questions, was shared through e-mail and WhatsApp group with representatives of 40 diabetes organizations, in 18 countries, all members of the International Diabetes Federation (IDF), in the SACA region. The 4 initial questions were related to the identification of the organization, the representative responding, the country and the type of town (coastal, capital or inland). The 4 subsequent questions enquired about policies including: the presence of policies to fight COVID-19, social distancing orientations, specific policies to protect people with diabetes and potential changes in terms of subsidies to medicines, supplies and exams for people with diabetes. One question pertained to the presence of official data on infection and mortality of people with diabetes during the pandemic and the following two were about main challenges and fears of people with diabetes due to COVID-19 (respondents could select more than one fear and challenge). The last was a placeholder for detailing country information on how the pandemic was affecting individuals with diabetes.
A database was built by aggregating answers of respondents from the same country regions (i.e. since all answers from Argentina were from the capital, they were aggregated in one final answer; from Ecuador there were two answers from the capital, one from the coast and one from inland, with differences between them, reason why Ecuador-capital, Ecuador-coast and Ecuador-inland were created). As a result, from the total number of 26 responding organizations, from 16 different countries, the processing led to 19 different final analyzed reports (Table 1 ). A multivariate cluster analysis technique pam (partitioning around medoids) was applied using the silhouette method to identify group of countries.
Table 1.
Demographic and government policies during COVID-19 pandemic.
| Geographic distribution of respondents (n = 26) | n | % |
|---|---|---|
| South America | 17 | 65,38% |
| Central America | 7 | 26,92% |
| Caribbean/North America (Cuba and Puerto Rico) | 2 | 7,69% |
| Social Distancing Policies (n = 19) | n | % |
| Social distancing recommended, only essencial shops open | 9 | 47,37% |
| Lockdown, with fines or prison | 9 | 47,37% |
| No recommendations | 1 | 5,26% |
| ProtectivePolicies for PwD* (n = 19) | n | % |
| PwD are advised to stay at home | 8 | 42,11% |
| Medicines provided for 2–3 months | 4 | 21,05% |
| Medicines are delivered to PwD | 3 | 15,79% |
| No policies | 4 | 21,05% |
| Official Data (n = 19) | n | % |
| No official data available | 6 | 31,58% |
| No official data, but it seems that PwD are more affected | 6 | 31,58% |
| No official data, but it seems that PwD are affected the same way | 2 | 10,53% |
| Yes, official data show higher mortality of PwD | 3 | 15,79% |
| Yes, official data show that PwD are more infected | 1 | 5,26% |
| Yes, official data show that PwD are affected in the same way | 1 | 5,26% |
*PwD = people with diabetes.
3. Results
The multivariate cluster analysis determined the ideal number of groups, identifying similarities in relation to the reported challenges and fears, which resulted in 2 groups. Countries reporting greater number of difficulties and fears: Argentina, Chile, Costa Rica, Ecuador, Ecuador-inland, Ecuador-coast, Nicaragua, Puerto Rico, Dominican Republic and Venezuela were in the group 1. In group 2 were: Bolivia, Brazil, Brazil-inland, Cuba, Guatemala, Honduras, Paraguay, Peru and Uruguay.
Nicaragua was the only country reporting neither public policies to deal with the pandemic, nor recommendations for social isolation. Brazil-inland, Cuba and Honduras were the only ones that did not report one or more of the challenges or fears related to shortage or lack of medicines and medical supplies, or difficulties to access health services. The countries that reported shortage or lack of medicines and medical supplies included: Argentina, Ecuador-inland, Ecuador-coast, Guatemala, Nicaragua, Uruguay, and Venezuela (most of them in the group 1). Difficulties to access health services were reported by Argentina, Bolivia, Brazil, Chile, all three Ecuador (capital, coast and inland), Nicaragua, Paraguay, Peru, Puerto Rico, Uruguay, and Venezuela. Concerns about the consequences on the economy were reported by most respondents, with increase in price of first necessity products as most cited (Fig. 1 ).
Fig. 1.
Frequencies of challenges selected by respondents.
4. Discussion
Although the responses unveil the presence of COVID-19 policies in most of the countries (95%), only one of them (5%) lacked policies, half reported partial lockdowns, where “stay-at-home” recommendation was ordered, but no mobility restrictions enforced by law (which is the case of the other half). Although Asian and European countries experimented different tactics and experts alerted SACA countries on the potential consequences of not adopting certain restrictive measures [3], [12], [22], most of our findings were aligned with previous reports [10], [13], however we were also interested in understanding specific policies to protect people with diabetes.
Unfortunately, only 37% responded that a policy was put into place to protect individuals with diabetes delivering their medicines and supplies at home (16%) or receiving them at once enough for 2 or 3 months (21%). This means that the other 63% were just being advised to stay at home (42%) or not even that (21%). For the reasons presented in the introduction, higher risk of poor outcome for people with diabetes when infected by SARS-CoV-2 [4], [15], [16], [17], [18], [25], it would be wise for governments to implement early strategies on this matter aiming to prevent the spread of the virus and, this way protect their hospitals and health services from unsustainable high demand.
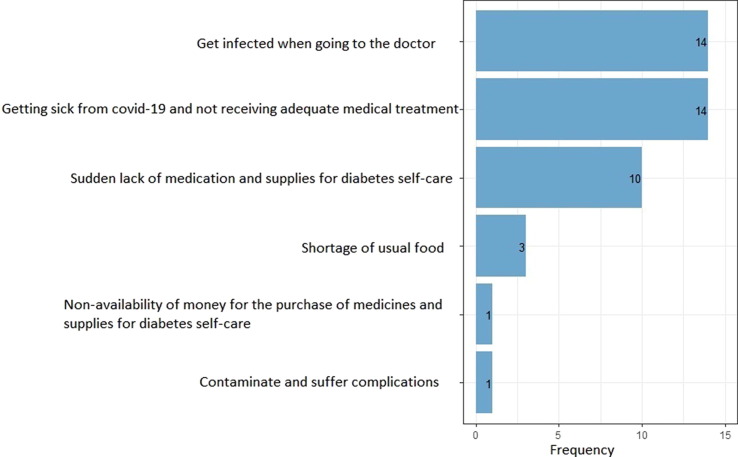
The absence or weakness of protective policies creates fear, reason why all respondents reported as one of the main fear is to “be infected and not receive adequate treatment” and/or “getting infected whilst going to the hospital or to appointment with a physician” (Fig. 2 ). Consequently, a survey in Brazil [24] revealed that 38.4% of the individuals with diabetes are postponing their medical appointments or laboratory exams and 5.8% stopped reclaiming their medicines and medical supplies for diabetes self-care. The potential consequences of these fears on populations with diabetes can be catastrophic, increasing the already high incidence of chronic complications and exacerbating them to get in an even more risky metabolic situation if infected by SARS-CoV-2 [15], [19]. Thus, among the protective measures to be promptly implemented, we recommend telehealth, teleconsultation and other online strategies to overcome the challenges of healthcare professionals’ shortage, while keeping individuals with diabetes protected and assisted [24], [26], [27], [28].
Fig. 2.
Frequencies of fears selected by respondents.
Successful measures implemented by different nations included monitoring, testing, tracing, isolating and treating, which work especially within a well-organized and integrated health structure and data system, with availability of COVID-19 tests, and trained healthcare professionals. In SACA and other developing regions, these components have constraints [3], [13], [21], a probable reason why only 26% reported that official data on COVID-19 in people with diabetes is available in their countries.
The multivariate cluster analysis revealed that, in general, countries with more restrictive measures reported more challenges and fears, the exceptions were Bolivia, Nicaragua and Venezuela. Bolivia, even reporting among the most restrictive measures, listed few challenges and fears (compatible with group 2, where countries that adopted less stringent measures were found). In Nicaragua, no social distancing policy was reported, while Venezuela reported policies and measures of the same level as Honduras and Brazil, but both still listed many challenges and fears (equivalent to group 1). We hypothesize that, independently of objective measures, the perceived challenges during the pandemic is associated also with the trust in the country’s health system and potential to respond.
It is also clear that the unfortunate prediction of lack of medication and supplies - such as syringes, needles and glucose strips - and difficulties to access health services - especially consultation with a physician and lab exams - were reported by most of the respondents, 68.4% and 57.9%, respectively [29]. These findings play against the recommendation of maintaining or even improving blood sugar levels and diabetes selfcare during the pandemic [25], [26], [28], [30], since diabetes is a known risk factor for severity and mortality by SARS-CoV-2 infection [4], [15], [16], [25], which is especially increased when associated with hyperglycemia [15], [19].
An aspect that must not be disregarded, highlighted by other authors [13], [21], [31] is the socioeconomic harm caused by the pandemic, reported by 12 out of the 16 respondent countries, 78.9% of the answers (Fig. 1: increase in costs, unemployment and lack of economic support from the government). Universal health coverage has not been implemented in the entire SACA region. In some countries, coverage by the public health system has to be complemented with additional private plans by populations and those who seek care [24], [32], this economic crises may severely impact the individuals' capacity to sustain their diabetes management and control in short, mid and long term. The consequences of reduced access to healthcare and medicines because of impoverishment would be disastrous, with dramatic increase in the prevalence of chronic complications. While four countries did not report these challenges, it is worth emphasizing that they reported other severe experiences; two of them (Bolivia and Paraguay) experiencing challenges to access health services, Cuba experiencing lack of fresh fruits and vegetables, and Honduras experiencing lack of food in general.
Among the limitations of the present study is the lack of response from members of all the 40 diabetes organizations that are IDF SACA members. We received responses from 26 of them, representing 16 out of the 18 countries and regions that form the IDF SACA group. The survey was not conducted in a representative sample of the population with diabetes in this region and, therefore, no generalization can be made for these people with diabetes. Meanwhile, it was answered by the organizations who represent them, and are likely to be aware of the adopted policies and measures, as well as main challenges and fears. Therefore, as such, reported perceptions were built by the experiences of each respondent, and may not necessarily reflect the general opinion of the population that they represent. We would also highlight the fact that, since most diabetes organizations are based in the capital cities, the inland and coastal areas of the region may be experiencing situations that were not captured. Another limitation, intrinsic to surveys, is the absence of all answers that the respondents would like to find, reason why we found the following comments “question 9 is not well formulated” or “not all questions reflect precisely the situation in our country”.
5. Conclusion
Although SACA region was not among the first to be infected by SARS-CoV-2 and, theoretically, it would have benefited from more time to prepare compared to nations in Asia or Europe for example, several of its countries experienced great and/or prolonged consequences. Aspescts that would differentiate countries in this unexpected battle include: preparedness for disasters, presence of a consistent universal health system and coverage, effective communication channels and means to invest in new priorities. Notwithstanding, diabetes organizations of “better prepared countries” not necessarily reported less perceived challenges or fears. Thus, in the present study we identified that, according to the respondent organizations, individuals with diabetes, known to be in higher risk for poor prognosis if infected by the new coronavirus, did not feel protected, and most suffered socio-economic restrains and/or limitations to access healthcare and/or supplies as consequences of this pandemic.
We understand that, as shown in countries where the SARS-CoV-2 spread started earlier, measures must be swiftly implemented to protect populations, with potential to reduce time in quarantine or lockdown. Moreover, specifically about individuals with diabetes, knowing about their higher risk, especially when presenting glycemic levels out of target, protective measures and strategies to facilitate optimum self-care must be adopted. In the present study, more than 68% of the respondents reported current shortage or lack of medicines and almost 58% difficulties in accessing health services. Therefore, we advise SACA governments to quickly act to revert this situation, implementing measures to guarantee access to medicines and health services, offering telehealth, teleconsultations and medicines delivery options whenever possible. These are not only strategies to reduce the burden on individuals, communities, and entire populations, but also a way to prevent health systems collapse.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
The authors acknowledge the non-governmental organizations ADJ Diabetes Brasil (ADJ), Asociación Costarricense Lucha Contra la Diabetes, Asociación de Diabetes Juvenil del Perú (ADJ), Asociación de Diabéticos del Uruguay, Asociación de Padres de Niños y Jóvenes Diabéticos de Nicaragua (APNJDN), Asociación Diabetes Argentina (A.D.A.), Asociación Nacional de Diabetes de Honduras, Asociación Nacional pró Estudio de la Diabetes Endocrinología y Metabolismo (ANPEDEM), Asociación para el Cuidado de la Diabetes en Argentina (CUI.D.AR), Federación Ecuatoriana de Diabetes, Federación Nacional de Diabetes (FENADIABETES), Fundación Aprendiendo a Vivir con Diabetes (FUVIDA), Fundación de Diabetes Juvenil del Ecuador, Fundación Los Fresnos “Casa de la Diabetes”, Fundación Nicaragüense para la Diabetes, Instituto da Criança com Diabetes (ICD), Instituto Nacional de Diabetes, Patronato de Pacientes Diabéticos de Guatemala, Sociedad Argentina de Diabetes, Sociedad Boliviana de Endocrinología Metabolismo y Nutrición, Sociedade Brasileira de Diabetes (SBD), Sociedad Cubana de Endocrinología y Diabetes, Sociedad de Diabetología y Nutrición del Uruguay, Sociedad Paraguaya de Diabetología; Sociedad Puertorriqueña de Endocrinología y Diabetología for their partnership in this study; and Belinda Ngongo for her contributions reviewing the article and bringing valuable suggestions.
Formatting of funding sources
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Yang X., Yu Y., Xu J., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet. 2020 doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez-Morales A.J., Sánchez-Duque J.A., Hernández Botero S., Pérez-Díaz C.E., Villamil-Gómez W.E., Méndez C.A., Verbanaz S., Cimerman S., Rodriguez-Enciso H.D., Escalera-Antezana J.P., Balbin-Ramon G.J., Arteaga-Livias K., Cvetkovic-Vega A., Orduna T., Savio-Larrea E., Paniz-Mondolfi A., LANCOVID-19 Preparación y control de la enfermedad por coronavirus 2019 (COVID-19) en América Latina. Acta Med Peru. 2020;37(1):3–7. doi: 10.35663/amp.2020.371.909. http://amp.cmp.org.pe/index.php/AMP/article/view/909 [DOI] [Google Scholar]
- 3.Sánchez-Duque J.A., Arce-Villalobos L.R., Rodríguez-Morales A.J. Enfermedad por coronavirus 2019 (COVID-19) en América Latina: papel de la atención primaria en la preparación y respuesta. Aten Primaria. 2020;S0212–6567(20):30117–30127. doi: 10.1016/j.aprim.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu Z., McGoogan J. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China. JAMA Network. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 5.Ferrari R, Maggioni AP, Tavazzi L, Rapezzi C. The battle against COVID-19: mortality in Italy. Eur Heart J ehaa326, 10.1093/eurheartj/ehaa326. [DOI] [PMC free article] [PubMed]
- 6.Hale T, Angrist N, Kira B et al. Variation in Government Responses to COVID-19” Version 5.0. Blavatnik School of Government Working Paper; 2020. https://www.bsg.ox.ac.uk/sites/default/files/2020-05/BSG-WP-2020-032-v5.0_0.pdf [accessed 15 May 2020].
- 7.Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in Low- and Middle-Income Countries. JAMA. 2020;323(16):1549–1550. doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
- 8.Inglesby T.V. Public Health Measures and the Reproduction Number of SARS-CoV-2. JAMA. 2020;323(21):2186. doi: 10.1001/jama.2020.7878. [DOI] [PubMed] [Google Scholar]
- 9.Croda J., Oliveira W., Frutuoso R., et al. COVID-19 in Brazil: advantages of a socialized unified health system and preparation to contain cases. Sociedade Brasileira de Medicina Tropical. 2020;53 doi: 10.1590/0037-8682-0167-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coronavirus Impact Dashboard Team. The Coronavirus Impact Dashboard: Measuring the Effects of Social Distancing on Mobility in Latin America and the Caribbean; 2020. https://blogs.iadb.org/efectividad-desarrollo/en/the-coronavirus-impact-dashboard-measuring-the-effects-of-social-distancing-on-mobility-in-latin-america-and-the-caribbean/ [accessed 15 May 2020].
- 11.The Lancet COVID-19 in Brazil: “So what?”. Lancet. 2020;395(10235):1461. doi: 10.1016/S0140-6736(20)31095-3. https://linkinghub.elsevier.com/retrieve/pii/S0140673620310953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mellan T., Hoeltgebaum H., Mishra S., et al. Imperial College London; 2020. Report 21: Estimating COVID-19 cases and reproduction number in Brazil. [Google Scholar]
- 13.Kirby T. South America prepares for the impact of COVID-19. Lancet. 2020 doi: 10.1016/S2213-2600(20)30218-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koh D. COVID-19 lockdowns throughout the world. Occupational Medicine, kqaa073. 10.1093/occmed/kqaa073. [DOI]
- 15.Gentile S., Strollo F., Ceriello A. Ceriello, COVID-19 Infection in italian people with diabetes:lessons learned for our future (an experience to be used) Diabetes Res Clin Pract. 2020;162 doi: 10.1016/j.diabres.2020.108137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang W., Lu J., Gu W., Zhang Y., Liu J., Ning G. Care for diabetes with COVID‐19: Advice from China. J Diabetes. 2020;12(5):417–419. doi: 10.1111/jdb.v12.510.1111/1753-0407.13036. https://onlinelibrary.wiley.com/toc/17530407/12/5 https://onlinelibrary.wiley.com/doi/abs/10.1111/1753-0407.13036 [DOI] [PubMed] [Google Scholar]
- 17.Kluge H., Wickramasinghe K., Rippin H., et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020 doi: 10.1016/S0140-6736(20)31067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu L., She Z., Cheng X., et al. Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes. Cell Metab. 2020 doi: 10.1016/j.cmet.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.International Diabetes Federation (IDF). IDF Diabetes Atlas, 9th ed. Brussels, Belgium: International Diabetes Federation; 2019.
- 21.Rodriguez-Morales A.J., Gallego V., Escalera-Antezana J.P., Méndez C.A., Zambrano L.I., Franco-Paredes C., Suárez J.A., Rodriguez-Enciso H.D., Balbin-Ramon G.J., Savio-Larriera E., Risquez A., Cimerman S. COVID-19 in Latin America: The implications of the first confirmed case in Brazil. Travel Med Infect Dis. 2020;35:101613. doi: 10.1016/j.tmaid.2020.101613. https://linkinghub.elsevier.com/retrieve/pii/S1477893920300806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cimerman S., Chebabo A., da Cunha C.A., et al. Deep impact of COVID-19 in the healthcare of Latin America: the case of Brazil. Braz J Infect Dis. 2020 doi: 10.1016/j.bjid.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Navarro J., Arrivillaga-Henríquez J., Salazar-Loor J., et al. COVID-19 and dengue, co-epidemics Ecuador and other countries in Latin America: Pushing strained health care systems over the edge. Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barone MTUB, Harnik SB, de Luca PV et al. The Impact of COVID-19 on People with Diabetes in Brazil. Diab Res Clin Pract 2020 [submitted for publication]. 10.1016/j.diabres.2020.108304. [DOI] [PMC free article] [PubMed]
- 25.Hussain A., Bhowmik B., Vale Moreira N.C. COVID-19 and diabetes: Knowledge in progress. Diabetes Res Clin Pract. 2020;162 doi: 10.1016/j.diabres.2020.108142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katulanda P., Dissanayake H., Ranathunga I. Prevention and management of COVID-19 among patients with diabetes: an appraisal of the literature. Diabetologia. 2020 doi: 10.1007/s00125-020-05164-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sarti T, Lazarini W, Fontenelle L, et al. What is the role of Primary Health Care in the COVID-19 pandemic? Epidemiol. Serv. Saude, Brasília 2020;29(2):e2020166. 10.5123/S1679-49742020000200024. [DOI] [PubMed]
- 28.Bornstein S., Rubino F., Khunti K., et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet. 2020 doi: 10.1016/S2213-8587(20)30152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ma R.C.W., Holt R.I.G. COVID-19 and diabetes. Diabet Med. 2020;37:723–725. doi: 10.1111/dme.14300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gupta R., Ghosh A., Singh A.K., et al. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diab Metab Syndr Clin Res Rev. 2020;14(3):211–212. doi: 10.1016/j.dsx.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rafael R., Neto M., Carvalho M., et al. Epidemiology, public policies and Covid-19 pandemics in Brazil: what can we expect? Revista de Enfermagem Uerj. 2020;28 [Google Scholar]
- 32.Báscolo E., Houghton N., Del Riego A. Lógicas de transformación de los sistemas de salud en América Latina y resultado en acceso y cobertura de salud. Rev Panam Salud Publica. 2018;42 doi: 10.26633/RPSP.2018.126. [DOI] [PMC free article] [PubMed] [Google Scholar]