Abstract
Background and Aims
EUS-guided gallbladder drainage has been increasingly applied for acute cholecystitis in high-risk surgical patients. In cases of EUS-guided gallbladder drainage with lumen-apposing metal stents (LAMSs), endoscopic retrieval of gallstones becomes feasible. However, retrieval of giant gallstones is still difficult because of the limited space in the saddle section of the LAMS. In this study, we aimed to evaluate the efficacy and safety of endoscopic laser lithotripsy and lithotomy through LAMSs for the removal of giant gallstones.
Methods
Five consecutive patients with recurrent cholecystitis due to giant gallstones were enrolled. We proceeded with EUS-guided LAMS implantation. Endoscopic laser lithotripsy and lithotomy then was performed through the LAMSs, and the stents were removed after all stones were extracted. The patients were followed up at scheduled times.
Results
EUS-guided LAMS implantation was successfully performed, and target gallstones were completely removed in all 5 patients. There was no severe bleeding, perforation, or stent migration during the operation. No recurrence of gallstones was found at late follow-up.
Conclusions
Endoscopic laser lithotripsy and lithotomy through LAMSs could be a safe and effective approach for removal of giant gallstones.
Abbreviations: ELLL, endoscopic laser lithotripsy and lithotomy; LAMSs, lumen-apposing metal stents
Cholecystectomy is the main treatment method for gallstones but is not always suitable for all patients. Some serious adverse events and secondary problems after cholecystectomy have attracted increasing concern among both doctors and patients.1, 2, 3, 4 Thus, some new endoscopic gallbladder-sparing surgeries have been tentatively applied in clinical cases.5,6 Of these natural orifice transluminal endoscopic surgery techniques, EUS-guided gallbladder drainage has been increasingly applied for acute cholecystitis in high-risk surgical patients.7, 8, 9 In case of EUS-guided gallbladder drainage with lumen-apposing metal stents (LAMSs), endoscopic retrieval of gallstones through LAMSs becomes feasible, especially for small stones.10 The LAMS provides both a passage of drainage and a bridge that allows the endoscope into the gallbladder. However, larger stones cannot be extracted directly because of the limited space in the saddle section of the LAMS. Endoscopic laser lithotripsy and lithotomy (ELLL) may be a good method and has been performed successfully in our practice.11 In this study, we aimed to evaluate the efficacy and safety of the new approach.
Patients and methods
Patients
Five consecutive patients in Changhai Hospital were enrolled in this study between February 2016 and October 2017. The inclusion criteria were as follows: (1) symptomatic gallstones were diagnosed by ultrasound, CT, or magnetic resonance imaging; (2) the maximum diameter of the gallstone was greater than 1.5 cm; (3) the gallbladder contraction function was fine; and (4) the patients rejected surgery and desired preservation of the gallbladder. The exclusion criteria were (1) atrophy of the gallbladder and/or thickening of the gallbladder wall; (2) coagulopathy; (3) ascites; and (4) poor general condition and intolerance of endoscopic treatment. All patients provided informed consent before the procedure.
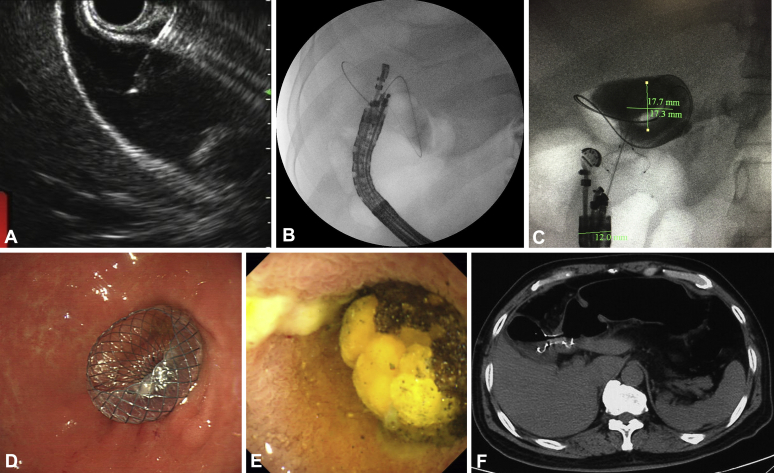
EUS-guided LAMS implantation
Patients were placed in a horizontal position while under single-lumen intubated anesthesia. All patients received prophylactic antibiotic treatment before the procedure. EUS-guided interventional procedures were performed using a linear-array echoendoscope (GIF-UCT260; Olympus Medical, Tokyo, Japan) under fluoroscopic guidance. The optimum puncture site was chosen as per the distance between the gallbladder and digestive tract and operability of the endoscope—either the antrum of the stomach or the bulb of the duodenum. EUS-guided transmural puncture was performed with a 19-gauge needle (EchoTip Access Needle; Cook Medical, Bloomington, Ind, USA) under color Doppler guidance. After the needle was inserted into the gallbladder, sterile normal saline solution was used for gallbladder aspiration and lavage to avoid bile leakage into the peritoneal cavity if necessary. Next, a 0.035-inch guidewire (Jagwire; Boston Scientific, Natick, Mass, USA) was advanced into the gallbladder through the needle. The guidewire was coiled into 2 to 3 circles in the gallbladder to ensure stability. The needle then was removed, and a cystotome (CST-10; Cook Medical) was applied to establish a passage into the gallbladder. Afterward, the stent delivery system was inserted over the guidewire and advanced into the gallbladder. Deployment of the stent proceeded under EUS and fluoroscopic guidance until the distal and proximal flanges were both expanded and in good position (Fig. 1).
Figure 1.
EUS-guided lumen-apposing metal stent implantation. A, EUS-guided puncture and irrigation of the gallbladder. B, A guidewire was advanced into the gallbladder through the needle. C, Imaging showed the gallstone. D, Successful deployment of the stent under EUS and fluoroscopic guidance. E, Gastroscopy showing the gallstone through the stent. F, CT image showing the stent in good position.
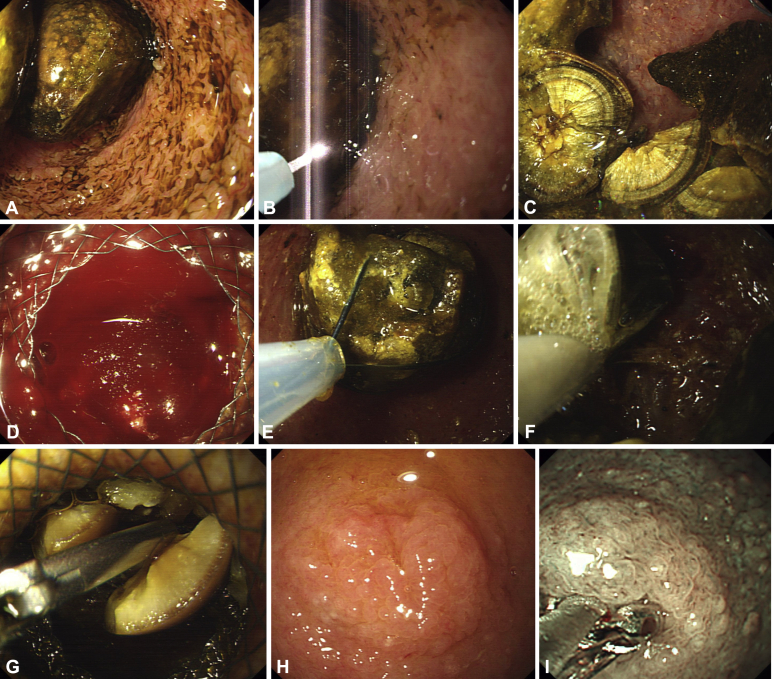
ELLL through the LAMS
U-100 plus frequency-doubled double-pulse laser (FREDDY; World of Medicine, Berlin, Germany) was used to break down large stones. After a gastroscope with a 2.8-mm work channel (GIF-H-260; Olympus Medical) was advanced into the gallbladder, the laser fiber passed through the channel and contacted the stones immersed in water. Laser lithotripsy proceeded in work mode 120 mJ and 5/10 Hz until all stone fragments were smaller than 1 cm. Various devices were selected to remove the fragments according to the stone shape and size. Larger pieces were extracted by basket or trielcon, and smaller pieces were extracted by rat-tooth forceps. Washing and suction was effective for sand grains and stones that had fallen into the cystic duct. All visible pieces were extracted, and no retained stones were found by antegrade cholangiography (Fig. 2). The LAMS then was removed, and gastroscopy and histopathologic examinations for potential mucosal lesions proceeded. Finally, the artificial fistula was handled properly according to actual conditions (Fig. 3).
Figure 2.
Endoscopic laser lithotripsy and lithotomy through the lumen-apposing metal stents. A-C, The giant gallstones were broken into fragments by laser. D, Minor hemorrhage occurred during laser lithotripsy. E-G, The fragments were extracted by baskets, disposable bags, and rat-tooth forceps, respectively. H, I, Gastroscopy and biopsy were performed for potential mucosal lesions.
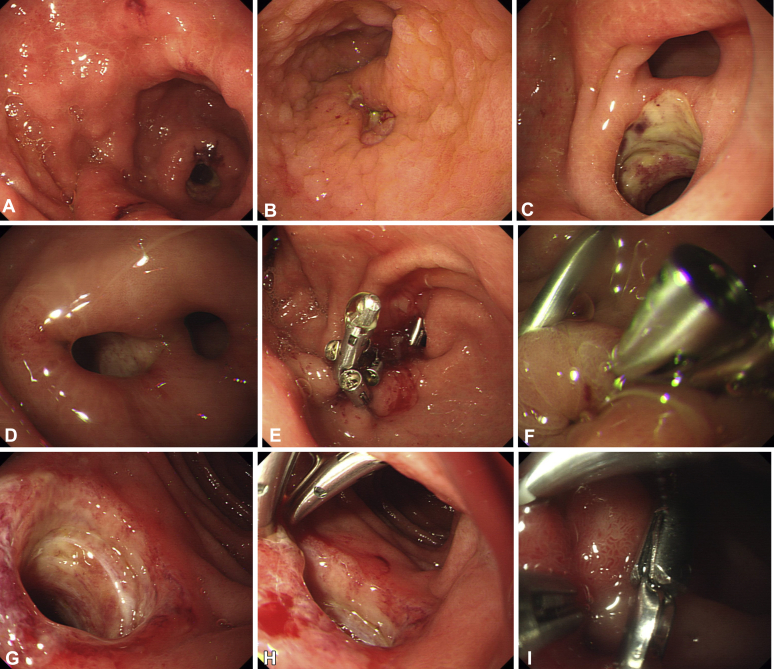
Figure 3.
Healing condition of the artificial fistulas after stent removal. A, B, The fistula closed 3 days after stent removal in case 2. C-E, The fistula had not closed spontaneously 3 days after stent removal, and endoclips were used to promote closure in case 3. F, The fistula nearly closed 11 days after stent removal in case 3. G-I, The fistula was closed with endoclips immediately after stent removal and nearly closed 10 days later in case 4.
Main outcome measurements
The main outcome parameters include technique success rate, clinical success rate, and adverse events. Technique success is defined as the implantation of the LAMS. Clinical success is defined as complete removal of gallstones. Adverse events include bleeding, peritonitis, perforation, failed stent deployment, and stent migration. Procedure-related parameters include puncture sites, operation time of stent implantation, interval time between ELLL and stent implantation, operation time of ELLL, and healing time of fistula.
Follow-up
Regular US and CT examination was performed at 3, 6, and 12 months after surgery in the first year and every 6 months in the following years. Gastroscopy and MRCP were performed if necessary.
Results
Five patients (1 male and 4 female) were enrolled in the study. A total of 6 large stones were found. The size of gallstones ranged from 12.5 × 16.7 mm to 23.8 × 28.8 mm. EUS-guided LAMS implantation was successfully performed via a transgastric approach (n = 2) and transduodenal approach (n = 3). The mean operation time of stent implantation was 33 minutes, ranging from 25 to 42 minutes. One patient had 5 days of postoperative fever and upper abdominal pain because of localized peritonitis. For the 5 patients, the interval between ELLL and stent implantation was 28, 14, 2, 2, and 7 days, respectively. ELLL was successfully performed in all 5 patients through the LAMSs. The mean time of ELLL is 2.5 hours, ranging from 0.5 to 5 hours. There was no pneumoperitoneum, subcutaneous emphysema, or stent migration in any of the 5 cases, except a minor hemorrhage that occurred in 1 case during laser lithotripsy. No stone pieces fell into the common bile duct, as confirmed by antegrade cholangiography. ERCP proceeded in 1 case for retrieval of stone fragments retained in the neck of the gallbladder. All LAMSs were removed immediately after complete retrieval of gallstones. The artificial fistula was completely self-closed in the first 2 patients, and endoclips were used to promote the closure of fistulas in the last 3 cases. The mean healing time of the fistula was 6.6 days, ranging from 2 to 11 days. No recurrence of gallstones was found after a mean follow-up of 27.8 months (range 24-36 months) (Table 1).
Table 1.
Clinical and technical characteristics
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Sex | Female | Male | Female | Female | Female |
| Age, y | 65 | 60 | 49 | 45 | 33 |
| Acute cholecystitis | Yes | No | No | No | No |
| Size of gallbladder, mm | 69.2 × 24.5 | 52.2 × 34.4 | 39.3 × 23.5 | 49.4 × 16.3 | 56.0 × 24.0 |
| Number of gallstones | 1 | 1 | 1 | 2 | 1 |
| Size of gallstones, mm | 26.2 × 19.0 | 23.8 × 28.8 | 24.5 × 11.4 | 18.6 × 12.6 23.6 × 18.3 |
16.7 × 12.5 |
| Puncture sites | Duodenal bulb | Gastric antrum | Gastric antrum | Duodenal bulb | Duodenal bulb |
| Technique success | Yes | Yes | Yes | Yes | Yes |
| Time of stents implantation, min | 30 | 42 | 33 | 25 | 35 |
| Peritonitis | No | No | No | No | Yes |
| Interval time between ELLL and stent implantation, days | 28 | 14 | 2 | 2 | 7 |
| Clinical success | Yes | Yes | Yes | Yes | Yes |
| Time of ELLL, hours | 5 | 4 | 1.5 | 1.5 | 0.5 |
| Hemorrhage | No | Yes | No | No | No |
| Subcutaneous emphysema | No | No | No | No | No |
| Pneumoperitoneum | No | No | No | No | No |
| Stent immigration | No | No | No | No | No |
| Combined ERCP | No | No | No | Yes | No |
| Gastroscopic biopsy in gallbladder | No | Yes | No | No | No |
| Fistulas handling method | Putting aside | Putting aside | Putting aside + endoclips | Endoclips | Endoclips |
| Healing time of fistula, days | 2 | 3 | 11 | 10 | 7 |
| Recurrence of gallstones | No | No | No | No | No |
| Duration of follow-up, months | 36 | 28 | 27 | 24 | 24 |
ELLL, Endoscopic laser lithotripsy and lithotomy.
Discussion
In recent years, endoscopic transgastric and transrectal gallbladder-preserving cholecystolithotomy have been tentatively applied in the clinic.12 The gallbladder incision should be closed with endoclips after stone removal in this type of surgery. Residual endoclips in the abdominal cavity will influence not only the gallbladder contraction function but also subsequent US and magnetic resonance examinations. Moreover, they may lead to recurrence of gallstones. With the rapid development of endoscopic instruments and techniques, EUS-guided interventional procedures have been applied more extensively.13 As a typical example of EUS-guided natural orifice transluminal endoscopic surgery, EUS-guided gallbladder drainage with LAMSs has showed merit, such as safety, effectivity, and less injury to the gallbladder.13,14 The LAMS has bilateral anchor flanges and a saddle section and is fully covered. Theoretically, a LAMS allows adhesion between 2 organs via bilateral anchor flanges, as is done with a surgical anastomosis. In addition, the fully covered metal stent could prevent side leakage. All of these advantages make LAMSs an ideal device for endoscopic treatment of gallbladder diseases.
The diameter of the saddle section of LAMSs is approximately 1.5 cm. Stones measuring less than 1 cm can be removed easily through the LAMS, but larger stones should be broken into smaller fragments to facilitate retrieval. ELLL may be an effective method for giant stones, as established in our previous report.11 To further validate the effectivity and safety, we prospectively treated 5 consecutive patients. Although the sample size is small, the results could provide some good suggestions.
First, the body of the gallbladder may be the optimal puncture site, although the neck of the gallbladder is more advised because it is less mobile as compared with the body of the gallbladder. However, the narrow space will make the deployment of the stent challenging and create difficulties in the treatment of residual stones in the gallbladder neck.7,15 In the fourth case, the stone fragments retained in the neck of the gallbladder could not be removed because of the blockage caused by the anchor flanges. After repeated failure, the residual stones were removed with the method of endoscopic transpapillary retrograde flush and suction (Video 1, available online at www.VideoGIE.org).
Second, the optimal timing for endoscopic laser lithotripsy and lithotomy should be no less than 2 weeks after LAMS implantation. To ensure safety, the interval between laser lithotripsy and stent implantation in the first case was 4 weeks, which was enough for the fistula tract to mature. All subsequent procedures were safe and successful. The fistula closed completely 2 days after stent removal. On the basis of the first case, the interval was compressed to 2 weeks for the second case, and the fistula closed completely 3 days after stent removal. As a minimally invasive procedure, we expected this method to be an effective and safe procedure as compared with laparoscopic cholecystectomy and to be successfully completed within 1 week. Thus, we compressed the whole operation time of the last 3 cases. The interval between laser lithotripsy and stent implantation of the last 3 cases was 2, 2, and 7 days, respectively. Although no adverse events occurred during ELLL, the fistulas did not heal quickly after stent removal. Endoclips were used to promote the closure of fistulas in all of the last 3 cases. The healing time of the fistulas was 11, 10, and 7 days. This suggests that the healing time of the defects depends on the maturity of the fistulas, and 2 weeks may be an optimal time.
Third, the stone fragments should be within 1 cm in diameter to allow extraction through the stent. However, pieces should not be too small because this may increase rather than decrease the difficulty of retrieval. Overly small pieces could not be grasped by the baskets or forceps, and retrieval may be more difficult if some fall into the cystic duct or behind the stent. Moreover, some overly small pieces will most likely fall into the common bile duct during the operation, but fortunately this did not happen in any of the 5 cases.
Fourth, what is considered success for this novel approach to the treatment of gallstones? Success will be measured not merely by no evidence of residual stones in the gallbladder and no pieces falling into the cystic duct or common bile duct, but also by no evidence of precancerous or neoplastic lesions found in the gallbladder wall, which is a potential risk for patients. It is essential that gastroscopic and histopathologic examinations proceed after complete removal of stones. If necessary, endoscopic mucosal resection or endoscopic submucosal dissection should be performed—after all, the LAMSs supply the passage and chance for repeat operations.
Fifth, it is crucial to prevent the recurrence of gallstones after the operation. Although the causes are varied, it is confirmed that ursodeoxycholic acid may play a role in preventing the relapse of lithiasis after gallbladder-protecting lithotomy. The patients were all administrated ursodeoxycholic acid except keeping regular meals, especially breakfast. All patients were followed up every 6 months after the operation, and no recurrence occurred.
In conclusion, we show that ELLL is safe and feasible for gallstones through LAMSs, especially for giant gallstones. This could be an effective alternative treatment for patients who are not suitable for open surgery. However, further studies are needed to evaluate the long-term results and effectiveness.
Disclosure
All authors disclosed no financial relationships.
Supplementary data
Successful removal of residual stones in the neck of gallbladder with the method of ERCP and endoscopic laser lithotripsy and lithotomy for gallstones through the lumen-apposing metal stent.
References
- 1.Mori Y., Itoi T., Baron T.H. Tokyo Guidelines 2018: management strategies for gallbladder drainage in patients with acute cholecystitis (with videos) J Hepatobiliary Pancreat Sci. 2018;25:87–95. doi: 10.1002/jhbp.504. [DOI] [PubMed] [Google Scholar]
- 2.Kim H., Han I.W., Heo J.S. Postcholecystectomy syndrome: symptom clusters after laparoscopic cholecystectomy. Ann Surg Treat Res. 2018;95:135–140. doi: 10.4174/astr.2018.95.3.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thurley P.D., Dhingsa R. Laparoscopic cholecystectomy: postoperative imaging. AJR Am J Roentgenol. 2008;191:794–801. doi: 10.2214/AJR.07.3485. [DOI] [PubMed] [Google Scholar]
- 4.Morvay K., Nawroth R., Szentleleki K. Effects of fecal bile acids on experimental colon carcinogenesis. Zentralbl Chir. 1991;116:1359–1367. [PubMed] [Google Scholar]
- 5.Tan Y.Y., Zhao G., Wang D. A new strategy of minimally invasive surgery for cholecystolithiasis: calculi removal and gallbladder preservation. Dig Surg. 2013;30:466–471. doi: 10.1159/000357823. [DOI] [PubMed] [Google Scholar]
- 6.Lin X., Cai J., Wang J. Minimally invasive cholecystolithotomy to treat cholecystolithiasis in children: a single-center experience with 23 cases. Surg Laparosc Endosc Percutan Tech. 2017;27:e108–e110. doi: 10.1097/SLE.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 7.Cho D.H., Jo S.J., Lee J.H. Feasibility and safety of endoscopic ultrasound-guided gallbladder drainage using a newly designed lumen-apposing metal stent. Surg Endosc. 2019;33:2135–2141. doi: 10.1007/s00464-018-6485-5. [DOI] [PubMed] [Google Scholar]
- 8.Manta R., Mutignani M., Galloro G. Endoscopic ultrasound-guided gallbladder drainage for acute cholecystitis with a lumen-apposing metal stent: a systematic review of case series. Eur J Gastroenterol Hepatol. 2018;30:695–698. doi: 10.1097/MEG.0000000000001112. [DOI] [PubMed] [Google Scholar]
- 9.Larghi A., Rimbas M., Attili F. Endoscopic holmium laser lithotripsy of symptomatic gallstones through a lumen-apposing self-expandable metal stent. Am J Gastroenterol. 2016;111:1516. doi: 10.1038/ajg.2016.258. [DOI] [PubMed] [Google Scholar]
- 10.Minaga K., Yamashita Y., Ogura T. Clinical efficacy and safety of endoscopic ultrasound-guided gallbladder drainage replacement of percutaneous drainage: a multicenter retrospective study. Dig Endosc. 2019;31:180–187. doi: 10.1111/den.13242. [DOI] [PubMed] [Google Scholar]
- 11.Wang W., Shi X., Jin Z. Endoscopic laser lithotripsy and lithotomy through the lumen-apposing metal stent for a giant gallstone after EUS gallbladder drainage. VideoGIE. 2017;2:112–115. doi: 10.1016/j.vgie.2017.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cho S.H., Oh D., Song T.J. Comparison of the effectiveness and safety of lumen-apposing metal stent and antimigrating tubular self-expandable metal stent for EUS-guided gallbladder drainage in high surgical risk patients with acute cholecystitis. Gastrointest Endosc. 2020;91:543–550. doi: 10.1016/j.gie.2019.09.042. [DOI] [PubMed] [Google Scholar]
- 13.Ogura T., Higuchi K. Endoscopic ultrasound-guided gallbladder drainage: current status and future prospects. Dig Endosc. 2019;31(Suppl 1):55–64. doi: 10.1111/den.13334. [DOI] [PubMed] [Google Scholar]
- 14.Yuste R.T., Garcia-Alonso F.J., Sanchez-Ocana R. Safety and clinical outcomes of endoscopic ultrasound-guided gallbladder drainage with lumen-apposing metal stents in patients with dwell time over one year. Ann Gastroenterol. 2019;32:514–521. doi: 10.20524/aog.2019.0395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takagi W., Ogura T., Sano T. EUS-guided cholecystoduodenostomy for acute cholecystitis with an anti-stent migration and anti-food impaction system; a pilot study. Therap Adv Gastroenterol. 2016;9:19–25. doi: 10.1177/1756283X15609285. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Successful removal of residual stones in the neck of gallbladder with the method of ERCP and endoscopic laser lithotripsy and lithotomy for gallstones through the lumen-apposing metal stent.