Bile leaks are an uncommon adverse event after biliary surgery. Iatrogenic common bile duct (CBD) injuries are particularly uncommon. However, they lead to substantial morbidity and often require surgical intervention, possibly with the creation of Roux-en-Y hepaticojejunostomy. We describe a case demonstrating the successful combination of endoscopic and percutaneous methods to recanalize the bile duct after iatrogenic injury.
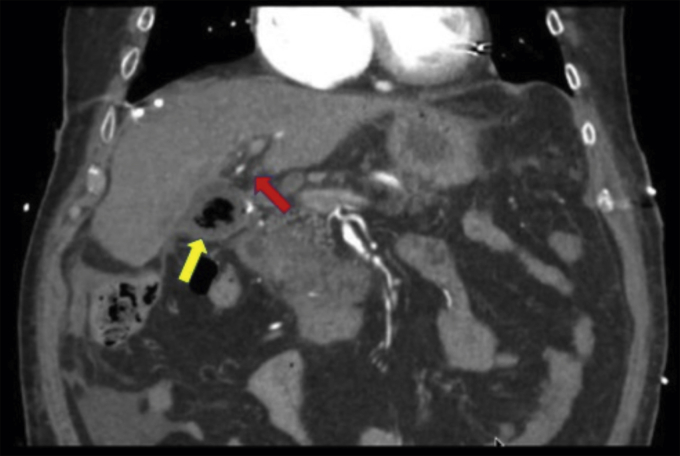
An 87-year-old man who had undergone laparoscopic cholecystectomy 4 weeks earlier presented for treatment of an iatrogenic common hepatic duct (CHD) leak due to a Bergman type D complete CBD transection. The output from a previously placed percutaneous subhepatic drain had ceased. A CT scan identified a 5-cm subhepatic debris-filled and air-filled collection (Fig. 1, yellow arrow). The bile duct could be visualized to the level of the surgical clips (Fig. 1, red arrow) without visualization of the CHD or presence of intrahepatic biliary dilation. ERCP was attempted locally but was unsuccessful because of an abrupt cutoff at the CHD resulting in inability to access the intrahepatic bile ducts.
Figure 1.
CT scan revealed a 5-cm subhepatic debris-filled and air-filled collection (yellow arrow). The bile duct was visualized to the level of the surgical clips (red arrow) without visualization of the common hepatic duct.
The patient was transferred to our institution. A multidisciplinary approach was used to achieve biliary recanalization. Given the patient’s prior CT and ERCP findings, the patient was referred to interventional radiology for placement of a right-sided percutaneous transhepatic biliary drain (PTBD) into the subhepatic space adjacent to the CHD injury. A repeat ERCP was performed, and an angled guidewire was manipulated through the site of CHD obstruction from the malpositioned surgical clips (Video 1, available online at www.VideoGIE.org). The wire was coiled in the subhepatic collection (Fig. 2). Contrast injection confirmed wire placement in the collection. The tract was dilated (Fig. 3). Digital single-operator cholangioscopy was performed over the guidewire. The cholangioscope was advanced through the CBD and across the site of CHD transection. The subhepatic space was entered, and the PTBD was visualized (Fig. 4). Eventually, an angled guidewire accessed the PTBD side hole and advanced through the looped portion of PTBD catheter (Fig. 5).
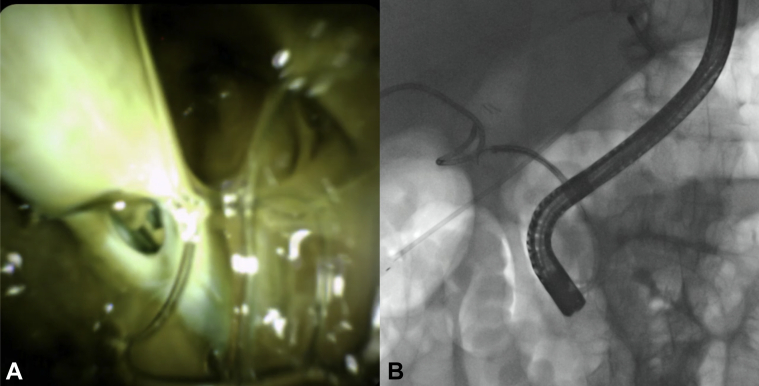
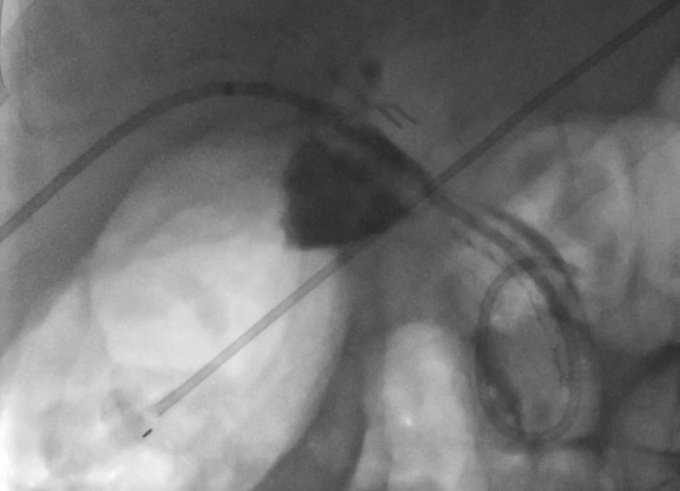
Figure 2.
The endoscopically placed wire was coiled in the subhepatic collection.
Figure 3.
The endoscopic tract into the collection was balloon dilated.
Figure 4.
A, Cholangioscopy facilitated successful entry into the subhepatic space, and the percutaneous transhepatic biliary drain was visualized. B, Fluoroscopy confirmed entry into the subhepatic space.
Figure 5.
The guidewire was advanced through the percutaneous transhepatic biliary drain side hole and through the looped portion of the percutaneous transhepatic biliary drain catheter.
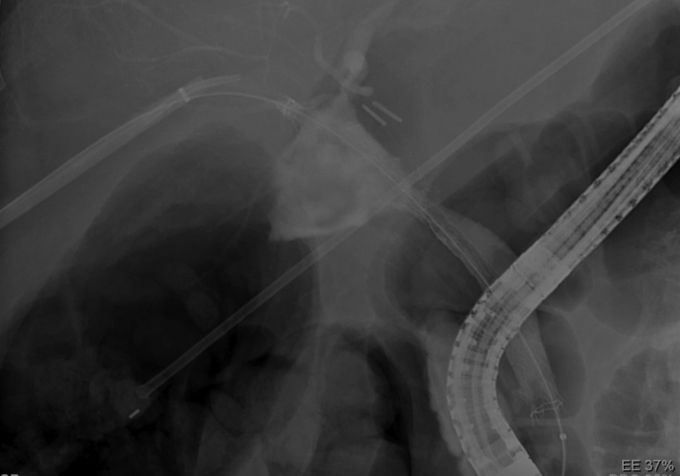
During PTBD removal over a second safety guidewire, the endoscopically placed wire was retracted into the PTBD tract and ultimately out of the percutaneous site. A 10 mm × 10 cm biliary fully covered self-expanding metal stent (FCSEMS) was deployed across the site of the CHD transection such that the proximal extent was in the right main hepatic duct and the distal extent was intraductal in the distal CBD (Fig. 6).
Figure 6.
Fluoroscopy confirmed successful placement of a 10-mm × 10-cm fully covered self-expanding metal stent across the site of common hepatic duct transection.
Contrast from the bilateral intrahepatic ducts drained spontaneously. The stent was secured with an 8.5F internal/external biliary drain placed through the FCSEMS and terminating in the duodenal lumen (Fig. 7). A repeat percutaneous cholangiogram performed 48 hours later demonstrated no left-sided intrahepatic biliary dilation suggestive of obstruction from the FCSEMS. The patient was discharged home 3 days later. The percutaneous drain was removed 4 weeks after the procedure. The patient was able to return to his baseline activities, and his liver chemistries have remained normal. The FCSEMS will remain in place indefinitely, given the unclear risk of stricture formation.
Figure 7.
The fully covered self-expanding metal stent was secured with an 8.5-Fr internal/external biliary drain placed through the fully covered self-expanding metal stent and terminating in the duodenal lumen.
In conclusion, iatrogenic bile duct injuries are uncommon, especially complete transection. Although they lead to substantial morbidity and anatomy-altering surgery is often required, our case demonstrates that, in select cases, recanalization of the bile duct is technically possible and safe using a multidisciplinary percutaneous and endoscopic approach.
Disclosure
Dr Pomerantz is a consultant for Olympus America. Dr Kazanjian is a consultant for Medtronic. Dr Law is a consultant for Olympus America. All other authors disclosed no financial relationships. There was no funding source for this case report.
Supplementary data
Recanalization of the bile duct using percutaneous and endoscopic methods after iatrogenic injury.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Recanalization of the bile duct using percutaneous and endoscopic methods after iatrogenic injury.