Abstract
Background:
There is an international drive towards increasing provision of community-led models of social and practical support for people living with advanced illness.
Aim:
This feasibility project aims to develop, implement and evaluate a model of community volunteers, identified as Compassionate Communities Connectors, to support people living with advanced life limiting illnesses/palliative care needs. The aims also include the development and evaluation of a training programme for volunteers and assessment of the feasibility, acceptability and preliminary effectiveness of this model of care.
Methods:
The approach seeks to map and mobilise people’s personal networks of care through the Connectors enlisting Caring Helpers (community volunteers). Up to 10 Connectors will be trained to work with at least 30 families selected by the palliative care service as requiring support. The primary outcome is the effect of the intervention on social connectedness. Secondary outcomes are the intervention’s effect on unplanned hospital utilisation, caregiver support needs, advance care plans and satisfaction with intervention for patients/carers, volunteers and service providers.
Conclusion:
It is expected that this intervention will enhance patient, carer and family social, psychological and practical support and reduce the need for dying people to be admitted to a hospital.
Keywords: Caring Helpers, Community Connectors, Compassionate Communities, end-of-life care, family carers, palliative care, practical support, social connectedness, social support, volunteers
Background
With the number of Australians dying annually expected to double in the next 25 years, the end-of life sector and Australian communities are looking for alternative, sustainable options for supporting positive end-of-life experiences for dying people, their carers and society more broadly. Many Australians currently die in a way and a place that does not reflect their values or their choice, and their end-of-life journey is interrupted with preventable or unnecessary admissions to hospital.1
Compassionate Communities is an international strategy for implementing the public health palliative care approach to end-of-life care. It recognises that sickness and health, death and loss are a natural part of life, and that care is not only a task for health and social services but is a community responsibility.2,3 While professional services are part of the mix, they need to recognise that their role is to work in partnership with civic and personal networks to support social connections and co-design end-of-life support. Hence, there is an international drive towards increasing provision of community-led models of social, psychological and practical support for people living with advanced illness and their families. These models differ in terms of duration of support, contact time, focus and range of activities, raising questions about their comparative effectiveness. There is limited but growing base of evidence concerning existing public health models in palliative care.
Sallnow and colleagues4 found that engaging communities can lead to improved outcomes for carers, such as decreased fatigue or isolation and increased size of care network, and can influence factors such as place of death and involvement of palliative care services. An evaluation of SAIATU (a program of social intervention in palliative care) project in Spain showed that those who had received home-based social support had fewer unscheduled health service visits, including hospital admissions, when compared to the control group. In addition, both patients and families rated the intervention positively, while the model was also found to be cost-effective.5,6 In the United Kingdom, three studies showed positive benefits. Cronin7 found that a primary care–led model of community support reduced patient isolation and led to fewer unscheduled healthcare visits to primary care and other allied health services, thereby reducing demand on National Health Service (NHS) staff and budgets. The End-of-Life Social Action study8 found that volunteer befriending services may reduce the rate of decline in quality of life and concluded that clinicians can confidently refer to volunteer services at end-of-life. More recently, Abel and colleagues9 found that proactive community involvement within primary care contributed to highly significant reductions in unplanned admissions to hospital resulting in a reduction of healthcare costs. For example, in Frome, a community of 30,000 people in Somerset (UK), there was a decrease of 14% in unplanned hospital admissions during the study period (2013–2017). By contrast, there was a 28.5% increase in admissions per quarter within the rest of the county of Somerset where no intervention was implemented. The Irish INSPIRE (INvestigating Social and PractIcal suppoRts at the End of life) study of the Good Neighbour Partnership developed a robust methodology but was not completed.10
In Australia, individuals, families and communities are already involved in caring for people who are unwell or dying or grieving,11–13 but there is a scarcity of evaluations of Australian community–led initiatives of practical and social support resulting in improved social connectedness. This proposed study presents an opportunity in the Australian context to develop, implement and evaluate a volunteer-led intervention in partnership with the palliative care service within the West Australian Country Health Service (WACHS).
Objectives
The objectives of this feasibility project are to
Design and implement a volunteer-led model of social, psychological and practical support for people living with advanced life limiting illnesses/palliative care needs and their families.
Develop and evaluate a training programme for the Compassionate Communities Connectors model of end-of-life care (the volunteer-led model)
Assess the feasibility, acceptability and preliminary effectiveness of this community model of care.
Methods
Ethics
Ethics approval (RGS3419) was obtained from WACHS Human Research Ethics Committee and La Trobe University Ethics Committee. All participants will receive a participant information sheet and have the opportunity to ask questions about participation before deciding to take part. Participants will sign a consent form and receive a copy for their own records. If participants decide to withdraw from the study, they will be able to do so at any point without providing a reason and without any future care, treatment or employment being affected.
Study design
This is a non-randomised prospective intervention study with a historical control matched just for health service utilisation data. A pre/post design will be used. The duration of the project is limited to 24 months in total with data collection spanning just 10 months.
Setting
This feasibility project will take place in the South West of Western Australia, a region of 24,000 km2 with a population of approximately 170,000. It comprises one regional port town, Bunbury, and many smaller rural towns and communities. Based on the Accessibility/Remoteness Index of Australia, the South West is classified 50% outer regional, 40% inner regional and 10% remote. The age structure of the South West differs from the state with a larger proportion of adults aged 45 years and above. The largest growth is in older age groups.14 The leading causes of death in the South West region are ischaemic heart diseases, cerebrovascular diseases, dementia (including Alzheimer’s disease), lung cancer and chronic obstructive pulmonary disease (COPD).
The South West Palliative care service is comprised of clinical nursing teams, each between one and three staff, located in seven sites across the region. The clinical nurses provide a 24-hour on-call service for patients in the terminal phase only. The nurses have access to two palliative care consultants based in Bunbury, the regional referral centre, and access to allied health staff; however, that access is variable and dependent upon local availability. The Regional Palliative Care team provides governance and support to these services. The region has 10-bed hospice (Palliative Care Unit) based in a private hospital in Bunbury and a four-bed hospice in Busselton (a smaller town).
Over the past year, 37.5% of palliative care patients died in hospital, 32.6% died in a hospice and 25% at home. The gaps in palliative care in the South West region were reported during a project in May 2019, which sought to better understand the South West palliative care system, to inform how access can be improved within existing resources. The summary report highlighted that while Western Australia is recognised ‘for its home-based palliative care service’, this service has generally only been provided in the Perth metropolitan area. Stakeholder and community representatives in the South West highlighted a lack of understanding of palliative care and how to access it; a lack of a 24-hour access to services; poor uptake of Advanced Care Plans; issues with communication, information sharing and poor linkages between agencies; a lack of support for people with a non-cancer diagnosis; and lack of support services for carers and families.15
The South West Compassionate Communities Network (SWCCN) is one of the eight GroundBreaker groups selected to be part of the National Compassionate Communities Forum, which is a learning network of communities across Australia. The SWCCN was established in August 2018 and aims to create opportunities for conversations around death, dying and loss; to identify naturally occurring community connectors and hubs within the community; and to foster a Compassionate Communities model of end-of-life care for practical and social support.13
Participants
The study will involve four groups: patients, their family carers, the Connectors and Caring Helpers. The aim is to train up to 10 Connectors to work with at least 30 families selected by the palliative care service as requiring support. Connectors are community volunteers who will be recruited via expressions of interest advertised through the SWCCN website. The number of Caring Helpers involved will be dictated by the nature and extent of needs of each family.
Patients/family carers
Patients/families that fit the inclusion criteria are screened by the WA Country Health Service palliative care team to enrol in the study, using the Supportive and Palliative Care Indicators Tool (SPICT).16 This tool is used to help identify people whose health is deteriorating and assess them for unmet supportive and palliative care needs. Approval is sought from the patient/carer to pass on contact details to the Project Coordinator.
Inclusion criteria
Patients with Cancer, COPD, Chronic Heart Failure or Renal disease and other chronic conditions such as neurodegenerative conditions;
Patients with an awareness of their advanced illness;
Patients are likely to die within the next 12 months, as advised by the palliative care service;
Patients with frequent hospital usage [>2 times in the past 3 months of hospital admissions or emergency department (ED) visits] or at risk of hospitalisation for palliative care;
Patients must have unmet social, psychological and practical needs;
Patients are socially isolated and rely on just one other person to meet the majority of their everyday needs;
Patients and carers must be 18 years and older;
All participants need to have capacity to provide informed consent.
Connectors
It is anticipated that the Connectors will have an existing, moderate level of death literacy and are aware of the project through attending the educational programmes undertaken by the SWCCN. Attendees were invited to leave their contact details if they were interested to participate in future activities of the SWCCN. The advertisement for Connectors will target these individuals. Those who have attended the SWCCN Death Festival in particular would have self-selected to attend because of their interest or experience in death-related matters, have already been volunteering in end-of-life care situations and they had looked after family members or friends who had a terminal illness and have died. Connectors can provide assistance to the person affected by advanced illness and their family by identifying the additional social and practical support they may require from within their local community and tap into formal and informal sources.
Connector selection will involve an interview process with members of the project team; this enables the interviewers to determine the person’s understanding of the role and the project. The interview questions and interviewers will ascertain that the person has the capacity to deal with the experiences of advanced illness, death and grief with compassion. Connectors will undergo reference checks, then recruitment will follow the health service Volunteer Policy. Insurance will be provided by the health service. The screening requirements include a National Criminal History Record Check.
Caring Helpers
Caring Helpers can be members of the family, friends, neighbours or other people in the community who are willing and able to assist with activities such as walking the dog, doing the shopping, collecting a prescription, going to the library, mowing the lawn, making a snack, tidying up or sitting with a person who needs a break. It does not involve providing personal or physical care, heavy lifting of people/objects or providing help with medical or financial matters. Assistance is provided by Caring Helpers without an expectation of payment or other reward or benefit.
Data collection and outcome measures
The project aims to achieve a set of outcomes related to preliminary effectiveness and feasibility and acceptability. Primary and secondary outcomes for preliminary effectiveness will be measured before and after the intervention.
Outcomes for preliminary effectiveness
Primary outcome
Improvement in patient and carer social connectedness as measured by the Modified Medical Outcomes Study of Social Support (mMOS-SS) survey.17 The mMOS-SS has two subscales covering two domains in social support (emotional and instrumental or tangible) composed of four items each designed to maintain the theoretical structure of the original 19-item Medical Outcomes Study of Social Support (MOS-SS) and identify potentially modifiable social support deficits. The psychometric properties of the eight-item mMOS-SS were reported to be excellent by Moser and colleagues.17
Secondary outcomes
- Reduction in unplanned hospital usage as measured by
- Comparing patient outcomes from the intervention group with those from the matched control group in terms of presentations to EDs, unplanned admissions to hospital and Length of Stay (LoS).
- Comparing costs of presentations to EDs, and unplanned hospital admissions, and LoS between the intervention group and the control group.
- Estimating overall cost-effectiveness for the local health service from programme implementation during the study period.
Reduction in carer unmet support needs by family carers as measured by completing the Carers’ Alert Thermometer (CAT) which identifies and addresses unmet support needs.18 The CAT is evidence-based and has eight domains within two overarching themes of the reported carer experience: the support needed by the carer to provide care and the support needed for the carer’s own health and well-being.
Improvement in death literacy of Connectors as measured by a death literacy tool developed by the project team, which asks about the Connectors’ knowledge and experience of death and dying.
Increase in the number of completed Advance Care Plans: the CAT includes one question to family carers, ‘Do you know the person’s wishes and preferences for end of life care’? If the patient is amenable to having an advance care plan, the palliative care team will be notified to undertake this task.
Other data collection tools include the following:
The Unmet Needs Tool assesses the unmet social/practical needs and support from social networks of patients and their carers, adapted from McLoughlin and colleagues.10 This tool lists needs in several domains such as personal care, home, medical, transport, social, food and pets. For example, to assess needing help at home, the three response categories are by order of increasing need: able to complete home care activities independently, requires some help to complete home care activities and requires another person to complete all home care activities on their behalf. Similarly, for assessing the strength of their support networks, the three response categories are by decreasing order of available support: members of the person’s network provide regular help, members of the person’s network provides ad hoc help or less than desired by the person and person has no one to help them in their network.
The Network Enhancement Tool (NET) is adapted from the tool used by the local aged care assessment team.19 It lists the same domains of needs as the Unmet Needs Tool, but next to each need, the connector can assign who can help the family, the potential helper’s relationship to the family, the frequency of their help and in which specific tasks.
Outcomes for feasibility and acceptability
Assess the experience of participation in this model of care through interviews and focus groups with patients/carers, Connectors and Caring Helpers.
Assess service providers’ experience in terms of improvement in care planning and coordination, improve links between referral pathways and disconnected services for specific cases and develop recommendations for improved service delivery.
Qualitative tools will be used to assess the feasibility and acceptability of this model of care and will be undertaken at the end of the intervention: interviews with patients and family carers and Connectors, a brief questionnaire for Caring Helpers and a focus group for service providers.
Sample size
Given the exploratory nature of the study, our conservative estimate of at least 30 is based on several factors: the size of the study population (about 100), what is feasible within the data collection time frame of 10 months, the reality of finding enough families fitting the inclusion criteria once implementation starts, willing to participate initially and then willing to complete the study. However, if all these conditions are met, we will endeavour to recruit more.
This trial is planned as a pilot in a small geographical area, to test procedures for applicability and acceptability, appraise the likely rates of recruitment and retention of participants and estimate adequate sample size based on the primary outcome measure for future larger studies.
The community intervention model
Connectors will attend a training course of 2-day duration delivered by content experts.
As part of the training, Connectors will be provided with a training resource that will be developed specifically to assist them understand their role and what is expected of them. Their knowledge and skills will be evaluated pre- and post-training. In addition, a community directory will be developed, so Connectors can signpost participants to community resources by knowing what is going on in the community.
Connectors will work with patients and families to co-design a plan on how to mobilise their network of Caring Helpers who will be providing the hands-on assistance. The project coordinator will liaise with the Connectors weekly to share their experiences and work through any arising issues.
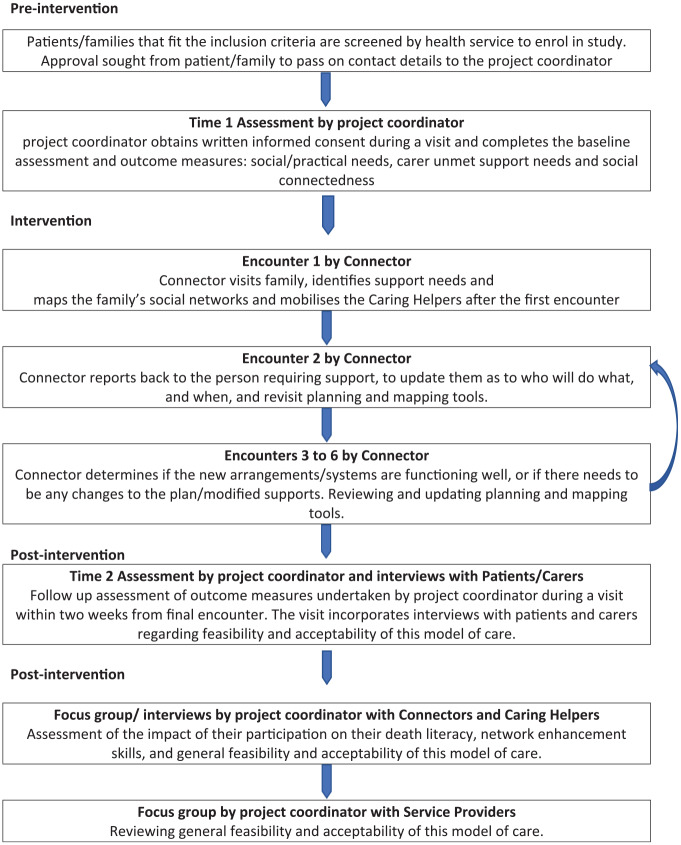
The project coordinator will assign a Connector, taking into account the profile of the person requiring support, their age and gender, geographical location, personality and the Connector’s availability and experience. The flowchart in Figure 1 maps out the sequence of data collection.
Figure 1.
Study protocol flowchart.
Pre-intervention phase
Assessment 1 by project coordinator
The project coordinator will visit the family to provide an explanation of the project, seek written consent and collect baseline information on the demographic and clinical profile of the family, their social and practical needs (using the Unmet Needs Tool), the carers’ support needs (using CAT) and their social connectedness (using mMOS-SS).
Intervention phase
After being trained, the community connectors will visit the person with advanced illness and their family carer or make contact over the phone a minimum of six times over 3 months. Each time they make contact, they will measure how well the patient/carer’s network of care and support is functioning.
The project coordinator will liaise with the Connectors on a weekly basis to discuss any arising issues and keep track of the data collection.
Encounter 1 by Connector
The nominated Connector visits the person with advanced illness and their family carer (with the support of the project coordinator, if required) and identifies their specific social and practical support needs by mapping the patient/carer’s social network using the NET. The connector co-designs a plan with the patient/carer to mobilise Caring Helpers or formal services, if required. This may involve the Connector contacting nominated Caring Helpers or formal services on behalf of the patient/carer. The project coordinator keeps a record of Connectors’ and Caring Helpers’ frequency and duration of visits and types of tasks undertaken throughout all encounters.
Encounter 2 by Connector
The Connector revisits the NET to see who has been mobilised and how well that is working for them. If required, the Connector may accompany the Caring Helper on their first visit, to provide introductions and outline their role. The Connector also identifies whether any further support is needed and once again co-designs a plan to identify informal and formal options to meet the needs of the family.
Encounters 3 to 6 by Connector
The Connector determines how well the network of care and support is functioning. If any further support is needed, they again co-design a plan moving forward with the patient/carer on how best to mobilise support.
Post-intervention phase
Assessment 2 by project coordinator
Follow-up assessment of the same outcome measures of assessment 1 will be undertaken by the project coordinator during a visit within 2 weeks following the Connector’s final encounter with the family. This visit incorporates interviews with patients and carers regarding the feasibility and acceptability of this model of care.
Interviews and focus groups
These will be undertaken with Connectors, Caring Helpers and palliative care providers to assess their experience and the feasibility and acceptability of this model of care.
Additional cycles of support
An additional 12-week cycle of support can be provided if required, subject to the agreement of the person with the advanced illness and their carer. After the death of the person with the advanced illness, a process similar to the above can take place with the carer whereby the Connector helps to mobilise Caring Helpers, if needed. Follow-up during this bereavement phase may extend up to three encounters within a 6-week period, if within the duration of the project.
The Connectors will be prepared during the training on how to deal with situations when the patient dies, and the project coordinator who meets with the connectors on a regular basis will be monitoring such events and addressing challenges as they arise with the connectors and the palliative care team.
Analyses
Quantitative data analysis
Quantitative data will be analysed using the SPSS software version 24. Descriptive statistics will summarise the quantitative data such as frequencies and percentages for categorical variables; means, standard deviations, medians and ranges for variables measured on a continuous scale will be used to describe the demographic (patients and carers) and clinical profile (patients) in the study. A paired t-test will be used to compare pre- versus post-intervention responses to all outcome measurement tools if the data are normally distributed. The Wilcox-signed rank test will be used if the data are not normally distributed. The data will be compared using two-tailed tests.
Qualitative data analysis
The interviews will be audio-recorded and transcribed verbatim. Transcripts will be imported into NVivo version 12 software for data management. Thematic analysis will be utilised to guide the development of themes from responses of the target groups where applicable. Two researchers will work independently and later check coding of data. A third team member will resolve disagreements about coding using the established coding scheme.
Effectiveness evaluation
For the outcome related to reducing hospital admissions, we will have a historical comparison/control group matched on socio-demographics (age, gender), clinical information (type and duration of disease) and hospital and emergency department use. Information on hospital utilisation will be drawn from the administrative database of WACHS. Comparisons will be undertaken regarding heath care costs and the costs of the programme implementation compared to the financial savings on prevented emergency admissions and hospital bed days.
Economic analysis
Costs and outcomes associated with delivering the intervention will be compared using cost-consequence analysis, a variant of cost-effectiveness analysis in which the components of incremental costs and outcomes are computed and listed without aggregating these results into an overall ratio. Cost-outcomes analysis provides a more comprehensive presentation of information than other types of economic evaluation and is appropriate for complex interventions that generate outcomes that cannot meaningfully be expressed using a single metric such as those in this study. Consequences and net costs will be tabulated to allow analysis of incremental cost per net change for each outcome. Decision trees will be used to illustrate the conceptual model of a cost-effectiveness analysis.
Discussion
Compassionate Communities as part of the public health approach to end-of-life care offers the possibility of solving the inequity of the difference in provision of care through enhancing the naturally occurring supportive networks surrounding patient and family and through palliative care services building stronger partnerships with these supportive networks to transform end-of-life care at home.20–22 Therefore, as Abel and colleagues22 stated, ‘if global and local palliative care are to successfully address challenges of unequal access, continuity of care, and health services reductionism, new practice models to address these issues need to be identified, debated and tested’. This feasibility project is about debating and testing one such new practice model by establishing a partnership between the community and the palliative care service in the South West of Western Australia, aiming to improve the capacity of the service to provide the full aspects of palliative care, including the psychosocial, practical and existential care. The unit of care is the patient and their caring network and the emphasis is on the social aspects of care where social relationships have been shown to have a larger impact on reducing mortality than any other existing intervention, over and above giving up smoking, alcohol drinking, exercise, diet and so on.23 It is expected that, by the end of the project, the community will have a sustainable pool of trained and experienced people who can work with the palliative care services to attend to the social and practical needs of dying people, improve their social connectedness and reduce the need for unplanned hospital usage.
Acknowledgments
We also acknowledge colleagues who advised on different aspects of the project: Dr Julieanne Hilbers, Anthea Openshaw, Associate Professor Rachael Moorin, Jan Stiberc, Leanne O’Shea and Dr John Rosenberg.
Footnotes
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by the Western Australian Health Translation Network and the Australian Government’s Medical Research Future Fund (MRFF) as part of the Rapid Applied Research Translation program.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Trial registration: Australian and New Zealand Clinical Trial Registry: ACTRN12620000326998.
ORCID iDs: Samar M. Aoun  https://orcid.org/0000-0002-4073-4805
https://orcid.org/0000-0002-4073-4805
Julian Abel  https://orcid.org/0000-0002-1002-5557
https://orcid.org/0000-0002-1002-5557
Contributor Information
Samar M. Aoun, Public Health Palliative Care Unit, School of Psychology and Public Health, La Trobe University, Melbourne, VIC 3086, Australia; Perron Institute for Neurological and Translational Science, Perth, WA, Australia.
Julian Abel, Director, Compassionate Communities, UK.
Bruce Rumbold, Public Health Palliative Care Unit, Department of Public Health, School of Psychology and Public Health, La Trobe University, Melbourne, VIC, Australia.
Kate Cross, WA Primary Health Alliance, Rivervale, WA, Australia.
Jo Moore, WA Country Health Service, Perth, WA, Australia.
Piari Skeers, WA Country Health Service, Perth, WA, Australia.
Luc Deliens, End-of-Life Care Research Group, Vrije Universiteit Brussel & Ghent University, Belgium; Department of Public Health and Primary Care, Ghent University, Ghent, Belgium.
References
- 1. Productivity Commission. Introducing competition and informed user choice into human services: reforms to human services. Report no. 85, 27 October 2017. Canberra, ACT, Australia: Australian Government. [Google Scholar]
- 2. Kellehear A. Compassionate cities: public health and end-of-life care. London: Routledge, 2005. [Google Scholar]
- 3. Kellehear A. The Compassionate City Charter. Compassionate Communities: Case Studies from Britain and Europe. Abingdon: Routledge, 2015. [Google Scholar]
- 4. Sallnow L, Richardson H, Murray SA, et al. The impact of a new public health approach to end-of-life care: a systematic review. Palliat Med 2016; 30: 200–211. [DOI] [PubMed] [Google Scholar]
- 5. Molina EH, Nuño-Solinis R, Idioaga GE, et al. Impact of a home-based social welfare program on care for palliative patients in the Basque Country (SAIATU Program). BMC Palliat Care 2013; 12: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Solinís RN, Hasson N, Idoiaga GE, et al. Impact of a home-based social program in end of life care in the Basque Country (SAIATU Program). Int J Integr Care 2014; 14: 165–166. [Google Scholar]
- 7. Cronin P. Compassionate Communities in Shropshire, West Midlands, England. In: Wegleitner K, Heimerl K, Kellehear A. (eds) Compassionate Communities: case studies from Britain and Europe. London: Routledge, 2015, pp. 30–45. [Google Scholar]
- 8. Walshe C, Dodd S, Hill M, et al. How effective are volunteers at supporting people in their last year of life? A pragmatic randomised wait-list trial in palliative care (ELSA). BMC Med 2016; 14: 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abel J, Kingston H, Scally A, et al. Reducing emergency hospital admissions: a population health complex intervention of an enhanced model of primary care and Compassionate Communities. Br J Gen Pract 2018; 68: e803–e810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McLoughlin K, Rhatigan J, McGilloway S, et al. INSPIRE (INvestigating Social and PractIcal suppoRts at the End of life): pilot randomised trial of a community social and practical support intervention for adults with life-limiting illness. BMC Palliat Care 2015; 14: 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Horsfall D, Leonard R, Rosenberg JP, et al. Home as a place of caring and wellbeing? A qualitative study of informal carers and caring networks lived experiences of providing in-home end-of-life care. Health Place 2017; 46: 58–64. [DOI] [PubMed] [Google Scholar]
- 12. Aoun S, Breen L, White I, et al. What sources of bereavement support are perceived helpful by bereaved people and why? Empirical evidence for the Compassionate Communities approach. Palliat Med 2018; 32: 1378–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hilbers J, Rankin-Smith H, Horsfall D, et al. ‘We are all in this together’: building capacity for a community-centred approach to caring, dying and grieving in Australia. Eur J Pers Cent Healthc 2018; 6: 685–692. [Google Scholar]
- 14. WA Country Health Service. South West health profile. Report, Planning and Evaluation Unit, Perth, WA, Australia, November 2018. [Google Scholar]
- 15. WA Primary Health Alliance. Palliative care strategy and roadmap: summary report. Perth, WA, Australia: Nous Group, 2019. [Google Scholar]
- 16. The University of Edinburgh. Supportive and Palliative care Indicators Tool (SPICT), www.spict.org.uk (2019, accessed 28 April 2020).
- 17. Moser A, Stuck AE, Silliman RA, et al. The eight-item Modified Medical Outcomes Study Social Support Survey: psychometric evaluation showed excellent performance. J Clin Epidemiol 2012; 65: 1107–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Knighting K, O’Brien MR, Roe B, et al. Development of the Carers’ Alert Thermometer (CAT) to identify family carers struggling with caring for someone dying at home: a mixed method consensus study. BMC Palliat Care 2015; 14: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. WACHS South West, Network Enhancement Tool (NET), 2019. (Unpublished tool). [Google Scholar]
- 20. Abel J, Walter T, Carey L, et al. Circles of care: should community development redefine the practice of palliative care? BMJ Support Palliat Care 2013; 3: 383–388. [DOI] [PubMed] [Google Scholar]
- 21. Abel J, Kellehear A. Palliative care reimagined: a needed shift. BMJ Support Palliat Care 2016; 6: 21–26. [DOI] [PubMed] [Google Scholar]
- 22. Abel J, Kellehear A, Karapliagou A. Palliative care – the new essentials. Ann Palliat Med 2018; 7: S3–S14. [DOI] [PubMed] [Google Scholar]
- 23. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med 2010; 7: e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]