Abstract
The morbidity and mortality of lung cancer are increasing. The Corona Virus Disease 2019 (COVID-19) is caused by novel coronavirus 2019-nCoV-2, leading to subsequent pulmonary interstitial fibrosis with chronic inflammatory changes, e.g., inflammatory factors repeatedly continuously stimulating and attacking the alveolar epithelial cells. Meanwhile, 2019-nCoV-2 can activate PI3K/Akt and ERK signaling pathways, which can play the double roles as both anti-inflammatory and carcinogenic factors. Moreover, hypoxemia may be developed, resulting in the up-regulation of HIF-1 α expression, which can be involved in the occurrence, angiogenesis, invasion and metastasis of lung cancer. Additionally, the immune system in 2019-nCoV-2 infected cases can be suppressed to cause tumor immune evasion. Therefore, we speculate that COVID-19 may be a risk factor of secondary lung cancer.
Keywords: Corona Virus Disease 2019(COVID-19), 2019-nCoV-2, Lung cancer, Risk factor
Lung cancer is one of the most common malignancy with rising morbidity and mortality, as a great threat to public health. Currently, it annually induces nearly 20% of all cancer-related deaths, and become the leading killer among the cancers [1], [2]. Smoking, air pollution, and histories of other bronchial-pulmonary diseases, e.g., chronic bronchitis, asthma, pneumonia and tuberculosis were proved to be the possible risk factors of lung cancer [3]. However, the etiology and epidemiology of lung cancer is still complex and warrants further study.
Currently, an acute respiratory infectious disease(COVID-19) caused by a novel coronavirus (2019-nCoV-2) is spreading and prevailing worldly[4]. With the accumulation of pathological knowledge and treatment experience, the cure rate has been improved greatly, and the mortality has decreased gradually [5]. However, the issues arise regarding management and follow-up of these cured case population. Will COVID-19 induce secondary lung diseases, e.g., LUNG CANCER?
COVID-19 can cause varying degrees of chronic airway inflammation and pulmonary fibrosis which may induce lung cancer
The pathophysiological mechanisms of COVID-19 seemed to be very similar to those of SARS-CoV and MERS-CoV, which can cause acute respiratory distress syndrome and Middle East respiratory syndrome, respectively [6]. Transmitted by droplets, the coronavirus may enter human respiratory tract and infect epithelial cells of trachea, bronchi and alveoli [7]. Furthermore, 2019-nCoV-2 can cause the systemic inflammation and multi-organ injuries, mainly targeting lung. Its main pulmonary pathological features include hyaline membrane consisting of monocytes, multinucleated giant cells and macrophages in the alveolar cavity, hyperplasia and abscission of type II alveolar epithelial cells, congestion and edema of alveolar septum, focal hemorrhage and necrosis of lung tissue, exudation from alveoli, and formation of pulmonary interstitial fibrosis [8].
Following COVID-19 goes through the acute stage, it can be classified as chronic inflammatory changes of trachea, bronchus and alveoli. The essences of chronic inflammation include a variety of inflammatory factors repeatedly and continuously stimulating the alveolar epithelium, leading to damage, shedding, proliferation and repair, and finally the atypical hyperplasia, metaplasia and even canceration of squamous cell epithelium [9]. Furthermore, 2019-nCoV-2 can trigger some inflamed cells, e.g., neutrophils and macrophages, to reach and gather in the infected alveoli, leading to the release of inflammatory mediators, e.g., protease and reactive oxygen free radicals, which can enhance fibroblast migration, proliferation, differentiation, resistance to apoptosis, metaplasia and even canceration of alveoli epithelial cells [10].
Additionally, COVID-19 associated chronic inflammation can stimulate and damage alveolar epithelial tissues leading to pulmonary fibrosis which may eventually induce lung cancer [11]. Actually, pulmonary fibrosis may be the pathological changes associating with end-stage of pulmonary inflammations, e.g., pneumonia, chronic obstructive pulmonary disease and tuberculosis, with a variety of genetic mutations and angiogenesis leading to high risks of lung cancer [12]. Over the past 10 years, the understanding of the inflammatory microenvironment of malignant tissues has supported Virchow's hypothesis on the connections between inflammation and cancer initially recognized by Rudolf Virchow in the nineteenth century [13]. The studies focusing on these abovementioned connections have clinical implications for cancer prevention and treatment [14].
Potential molecular mechanisms caused by COVID-19 may trigger the incidence of lung cancer
The spike protein on capsule surface of 2019-nCoV-2 can bind to angiotensin-converting enzyme 2 (ACE2) on cytomembrane of alveolar epithelial cell II, and thereafter enter the alveolar epithelial cell and replicate substantially, causing excessive inflammatory response and cytokine storm. Normally, ACE2 can degrade AngII in alveolar epithelial cell II into Ang (1–7). AngII can directly bind to NF-κB to promote the expression of inflammatory cytokines, while Ang (1–7) can bind to its specific receptor to up regulate PI3K/Akt and ERK signaling pathway to play an anti-inflammatory effect [15], [16]. The pathological combination of coronavirus and ACE2 results in reduction of free ACE2 and the subsequent accumulation of AngII, which aggravates the inflammatory response and pulmonary fibrosis. Meanwhile, PI3K/Akt and ERK signaling pathways can also be activated and participate in the occurrence and development of tumors, despite of relatively weak anti-inflammatory roles of these carcinogenic pathways [17], [18].
COVID-19 can induce hypoxemia and up regulate the expressions of hypoxia-inducible factor-1α (HIF-1α), vascular cell adhesion molecule-1 (VACM-1), intercellular adhesion molecule-1 (ICAM-1), E-selectin and other adhesion molecules. All these adhesion molecules can increase the adhesion between leukocytes and pulmonary vascular endothelial cells, causing the infiltration of inflammatory cells, secretion of numerous inflammatory factors by alveolar macrophages in lung tissues, up regulation of Toll-like receptor 4 (TLR4) by lipopolysaccharide (LPS) signal pathway, and amplification of inflammatory response[19]. Indeed, the expression of HIF-1α is up-regulated, which may be involved in the genesis, angiogenesis, invasion and metastasis of lung cancer [20].
COVID-19 leads to immune deficiency potentially leading to lung cancer
Based on previous studies regarding SARS, lymphocytes was found to be sensitized after SARS-CoV infection, and likely to enter the infected tissues, rather than lymphocyte circulation pool, leading to increasing of lymphocyte apoptosis and decreasing of peripheral blood lymphocytes. As per autopsy of COVID-19, numerous apoptotic cells was found to be increased significantly in the spleen, lung, lymph nodes and other tissues, e.g., lung cells, lymphocytes and monocytes, resulting in low or suppressed immune system function [21], [22]. Theoretically, immune system has the balance of immune monitoring to recognize and eliminate these “non self” cells in case of appearance of tumor cells. Compromised immune system can allow tumor cells escape immune surveillance [23]. For instance, the incidence of cancer in organ transplant patients will raise 2–4 times as compared with general population. In COVID19 patients, especially those aged and severe cases, the abundance of CD8+ or CD4+ T cells in circulation is lower than healthy controls, however, these T cells are very critical to antigen presentation and anti-tumor immunology. Studies show that a decrease in immune cell count increases the risk of lung cancer and is associated with a later stage of lung cancer at diagnosis [24], [25].
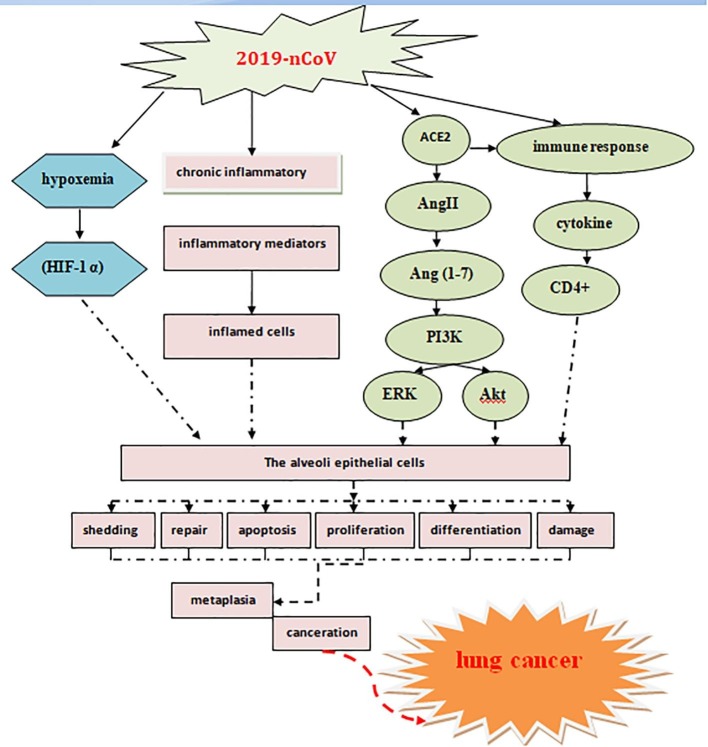
Collectively, the morbidity and mortality of lung cancer are increasing. The causes and risk factors of lung cancer are relatively complex. The COVID-19 is an acute respiratory infectious disease caused by novel coronavirus 2019-nCoV-2. Epithelial cells of trachea, bronchi and alveoli can be infected, leading to the formation of hyaline membrane in alveolar cavity, exudation from alveoli, and subsequent pulmonary interstitial fibrosis. The essence of pulmonary fibrosis is the chronic inflammatory changes with a variety of inflammatory factors repeatedly continuously stimulating and attacking the alveolar epithelial cells and causing proliferation, squamous cell epithelial atypical hyperplasia, metaplasia and possible canceration. Meanwhile, 2019-nCoV-2 can activate PI3K/Akt and ERK signaling pathways by combining with ACE2 on cell membrane. PI3K/Akt and ERK signaling pathways can play the double roles as both anti-inflammatory and carcinogenic factors. Moreover, patients with COVID-19 may develop hypoxemia, resulting in the up-regulation of HIF-1 α expression, which may be involved in the occurrence, angiogenesis, invasion and metastasis of lung cancer. In addition, following 2019-nCoV-2 infection, the immune system of the body can be suppressed, and the incidence of tumor is significantly increased. Therefore, as shown in Fig. 1 , we speculate that COVID-19 may be a risk factor of secondary lung cancer.
Fig. 1.
The possible mechanism that COVID-19 may increase the risk of secondary lung cancer.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This work was supported by grants from the Natural Science Foundation of Chong-qing, China (No. cstc2015jcyjA10073, No. cstc2019jscx-msxmX0252).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mehy.2020.110074.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 2.Wang X., Yang X., Li J., Liu F., Chen J., Liu X. Impact of healthy lifestyles on cancer risk in the chinese population. Cancer. 2019;125(12):2099–2106. doi: 10.1002/cncr.31971. [DOI] [PubMed] [Google Scholar]
- 3.Brody H. Lung cancer. Nature. 2014;513(7517):S1. doi: 10.1038/513S1a. [DOI] [PubMed] [Google Scholar]
- 4.Zhai P., Ding Y., Xia W.u., Long J., Zhong Y., Li Y. The epidemiology, diagnosis and treatment of COVID-19. Int J Antimicrob Agents. 2020;55(5) doi: 10.1016/j.ijantimicag.2020.105955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou F., Ting Y.u., Ronghui D.u., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuntao W.u., Ho W., Huang Y., Jin D.-Y., Li S., Liu S.-L. SARS-CoV-2 is an appropriate name for the new coronavirus. Lancet. 2020;395(10228):949–950. doi: 10.1016/S0140-6736(20)30557-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G. A New coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh N., Baby D., Prasad Rajguru Jagadish, Patil Pankaj B., Thakkannavar Savita S., Bhojaraj Pujari Veena. Inflammation and Cancer. Ann Afr Med. 2019;18(3):121–126. doi: 10.4103/aam.aam_56_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harapan H., Itoh N., Yufika A., Winardi W., Keam S., Te H., Megawati D., Hayati Z., Wagner A.L., Mudatsir M. Coronavirus disease 2019 (COVID-19): a literature review. J Infection Public Health. 2020;13(5) doi: 10.1016/j.jiph.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez Isis E., Eickelberg Oliver. New cellular and molecular mechanisms of lung injury and fibrosis in idiopathic pulmonary fibrosis. Lancet. 2020;380(9842):680–688. doi: 10.1016/S0140-6736(12)61144-1. [DOI] [PubMed] [Google Scholar]
- 12.Alavanja M.C.R. Biologic damage resulting from exposure to tobacco smoke and from radon:implication for preventive interventions[J] Oncogene. 2002;21(48):7365–7375. doi: 10.1038/sj.onc.1205798. [DOI] [PubMed] [Google Scholar]
- 13.Blanca Piazuelo M., Riechelmann R.P., Wilson K.T., Scott Algood H.M. Resolution of gastric cancer-promoting inflammation: a novel strategy for anti-cancer Therapy. Curr Top Microbiol Immunol. 2019;421:319–359. doi: 10.1007/978-3-030-15138-6_13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colotta F., Allavena P., Sica A., Garlanda C., Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: Links to genetic instability. Carcinogenesis. 2009;30:1073–1081. doi: 10.1093/carcin/bgp127. [DOI] [PubMed] [Google Scholar]
- 15.Kuba Keiji, Imai Yumiko, Rao Shuan, Jiang Chengyu, Penninger Josef M. Lessons from SARS:control of acute lung failure by the SARS receptor ACE2. J Mol Med(Berl) 2006;84(10):814–820. doi: 10.1007/s00109-006-0094-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Passos-Silva D.G., Verano-Braga T., Santos R.A. Angiotensin-(1-7): beyond the cardiorenal actions. Clin Sci(Lond) 2013;124(7):443–456. doi: 10.1042/CS20120461. [DOI] [PubMed] [Google Scholar]
- 17.Celec Peter. Nuclear factor kappa B-molecular biomedicine:the next generation. Biomed Pharmacother. 2004;58(6–7):365–371. doi: 10.1016/j.biopha.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 18.Mercer Paul F, Woodcock Hannah V, Eley Jessica D, Platé Manuela, Sulikowski Michal G, Durrenberger Pascal F. Chambers. Exploration of a potent PI3 kinase /mTOR inhibitor as a novel anti- fibrotic agent in IPF.Thorax. Pauline T Lukey, Rachel C. 2016;71(8):701–711. doi: 10.1136/thoraxjnl-2015-207429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gang Wu., Gang Xu., Chen De-Wei, Gao Wen-Xiang, Xiong Jian-Qiong, Shen Hai-Ying. Hypoxia exacerbates inflammatory acute lung injury via the Toll-like receptor 4 signaling pathway. Front Immunol. 2018;9:1667. doi: 10.3389/fimmu.2018.01667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eloy Moreno Roig, Arjan J Groot, Ala Yaromina, Tessa C Hendrickx, Lydie M O Barbeau, Lorena Giuranno, Glenn Dams, Jonathan Ient, Veronica Olivo Pimentel, Marike W van Gisbergen, Ludwig J Dubois, Marc A Vooijs. HIF-1α and HIF-2α Differently Regulate the Radiation Sensitivity of NSCLC Cells. Cells, 2019;8 (1): pii: E45. [DOI] [PMC free article] [PubMed]
- 21.Li G., Fan Y., Lai Y., Han T., Li Z., Zhou P. Coronavirus Infections and Immune Responses. J Med Virol. 2020;92(4):424–432. doi: 10.1002/jmv.25685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ou X, Liu Y, Lei X, Li P, Mi D, Ren L, Guo L, Guo R, Chen T, Hu J, Xiang Z, Mu Z, Chen X, Chen J, Hu K, Jin Q, Wang J, Qian Z. Characterization of Spike Glycoprotein of SARS-CoV-2 on Virus Entry and Its Immune Cross-Reactivity With SARS-CoV. Nat Commun,2020,11 (1):1620 2020 . [DOI] [PMC free article] [PubMed]
- 23.Menachery V.D., Yount B.L., Jr, Debbink K., Agnihothram S., Gralinski L.E., Plante J.A. A SARS-like Cluster of Circulating Bat Coronaviruses Shows Potential for Human Emergence. Nat Med. 2015;21(12):1508–1513. doi: 10.1038/nm.3985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lambrechts Diether, Wauters Els, Boeckx Bram, Aibar Sara, Nittner David, Burton Oliver. Phenotype molding of stromal cells in the lung tumor microenvironment. Nat Med. 2018;24(8):1277–1289. doi: 10.1038/s41591-018-0096-5. [DOI] [PubMed] [Google Scholar]
- 25.Chiappelli Francesco, Khakshooy Allen, Greenberg Gillian. CoViD-19 Immunopathology and Immunotherapy. Bioinformation. 2020;16(3):219–222. doi: 10.6026/97320630016219. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.