Dear Editors,
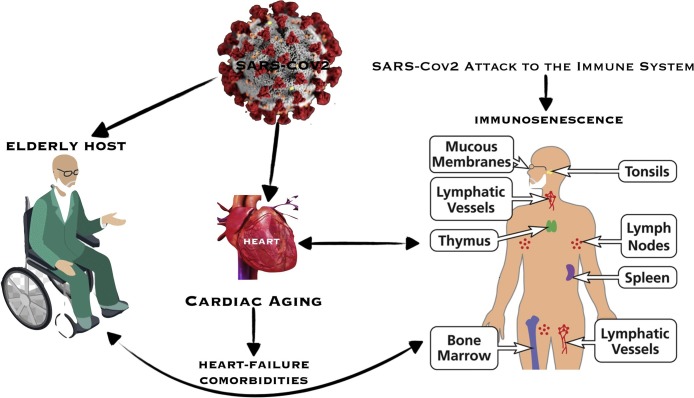
Aging and senescence are complex processes associated with increased frailty (Calimport, Bentley, & Stewart, 2019). Overall, many pathogens are more aggressive and prevalent in the elderly population. SARS-CoV-2 betacoronavirus (large RNA virus) is the virus inducing Corona Virus Disease 2019 (COVID-19), a respiratory infection that has relevant systemic effects on immune and cardiovascular systems (Bonow, Fonarow, O’Gara, & Yancy, 2020; Zhu, Zhang, & Wang, 2020). Typical hallmarks of immunosenescence (Thomas, Wang, & Su, 2020) are the reduction of peripheral blood T cells, an increase in the frequency of CD28 memory T cells, as well as a low-grade of chronic inflammation. Immunosenescence has a direct impact on the development of chronic heart failure and other comorbidities (Lainscak & Vitale, 2016; Moro-García, Echeverría, & Galán-Artímez, 2014) (Fig. 1 ). Lymphopenia occurs in over 80 % of COVID-19 patients with marked reductions in circulating levels of CD4+ and CD8 + T lymphocytes, and relative prevalence of mononuclear cells (monocytes and macrophages) in target injury tissues (Chen, Wu, & Guo, 2020), including the cardiovascular system. However, lymphopenia is based on the PBL test and all the effectors may have been activated and be attracted into the disease area, such as lung tissue, which caused a dramatic reduction of total immune effector number drop. Immune effector data from lung tissue or BALF contains a more reliable T cell number. In addition, the cytokine storm is a pathogenic factor after the infection, which was a result of overwhelmed activation of inflammation, a type activation of innate immunity, Conversely, in the aging immune system, there is a progressive marked lymphopenia with CD4 + T cell attrition and decreased regulatory T-cell function, leading to a partial restore through homeostatic lymphocyte proliferation, with a propensity for autoimmune and excessive inflammatory responses (Thomas et al., 2020). Decreased capacity to phagocytose apoptotic cells by senescent resident macrophages may promote a pro-inflammatory state. Indeed, the imbalanced aged immune system is then exacerbated by an infection such as COVID-19 which further induces the direct depletion of CD4 + T cells and macrophage migration by enhancing cellular apoptosis. Indeed, there is a substantial reduction of the peripheral lymphocyte counts, mainly CD4 T and CD8 T cells in COVID-19 patients, and is associated with a high risk of developing a secondary bacterial infection and viral sepsis. The precise mechanism underlying lymphopenia remains unknown but it is quite clear that SARS-CoV2 might be able to infect T cells directly (Li et al., 2020). Thus, elderly subjects may have a natural tendency to have a reduced virus clearance which in turn generates an inappropriate cytokine storm, with inadequate immune response and immunologic memory. During COVID-19, there is also increasing production of cytokines which can lead to a massive cytokine storm. Besides, the cytokine storm is a pathogenic factor after the infection, which was a result of overwhelmed activation of inflammation, a type activation of innate immunity. Patients with laboratory markers of progressive systemic inflammation, such as rising IL-6 and/or d-dimer levels, should be considered early for antithrombotic drugs (Bikdeli, Madhavan, & Jimenez, 2020). Many of these patients should be considered for full anticoagulation, such as heparin, depending on individual risk versus benefit. After convalescence post-COVID-19, great attention should be devoted to the issue of cardiopulmonary rehabilitation especially in the elderly age since a great bulk of evidence suggests that regular physical exercise may reduce immunosenescence (Duggal, Niemiro, Harridge, Simpson, & Lord, 2019). In elderly patients with dysfunctional immune response, the presence of early warning signals, such as marked lymphopenia, huge troponin release, elevated BNP, CRP, IL-1β, and IL-6 must be carefully detected. Such patients should be followed closely for existing comorbidities and monitored for the prevention of multi-organ failure (Gontijo Guerra, Berbiche, & Vasiliadis, 2019) also with efforts, including nutritional supplementation, made to restore immune balance (Aspinall & Lang, 2018). Remarkably, low-grade of chronic inflammation observed in immunosenescence contributes to excessive inflammation and other detrimental actions of comorbidities (e.g., diabetes, hypertension and heart failure) on the endothelium as a key target organ in COVID-19 patients.
Fig. 1.
Effects of immunosenescence in the elderly host. We thank G.M. Napoli (Sacro Cuore Institute) for assembling the figure.
If viral proliferation is continuing, strategies to attenuate the virus may be critical. Understanding these molecular mechanisms has identified several novel therapeutic targets that are now in development to treat COVID-19. Indeed, the ability to restore immune balance, with carefully controlled therapeutic approaches such as type I interferon, immunoglobulins, and passive immunity with convalescent plasma, may be considered (Valk, Piechotta, & Chai, 2020). Moreover, the efficacy of novel anti-inflammatory drug therapies including IL-1 receptor antagonist (Anakinra) or anti-IL-6 receptor antagonist (such as tocilizumab) will be determined in randomized trials (Salvi & Patankar, 2020). However, these interventions will need to be instituted early, before the irreversible immune amplification process is fully underway. The greatest benefit would be seen when these drugs are administered 30 h before severe symptom onset, especially in elderly individuals (Monto, Rotthoff, & Teich, 2004). Vaccine development is the best successful approach for combating viral diseases, including COVID-19. To date, there are 60 active clinical trials related to a SARS-CoV2 vaccine (see ClinicalTrials.gov). Overall, people who have more than 60 years are believed to have lesser protective effects by vaccines due to age-related declines in immune function (Monto et al., 2004). Thus, even when a vaccine for SARS-CoV2 will become available, particular attention will be due to elderly individuals (Pawelec & Weng, 2020).
Author contributions
Conception and design: C. Napoli.
Drafting of the article: C. Napoli, I. Tritto, G. Mansueto, G. Ambrosio.
Critical revision of the article for important intellectual content: C. Napoli, E. Coscioni, G. Ambrosio.
Final approval of the article: C. Napoli, G. Ambrosio.
Declaration of Competing Interest
There are no conflicts of interest in the connection of this manuscript.
References
- Aspinall R., Lang P.O. Interventions to restore appropriate immune function in the elderly. Immunity & Ageing: I & A. 2018;15:5. doi: 10.1186/s12979-017-0111-6. [PMID: 29416551] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E. COVID-19 and thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy, and follow-up. Journal of the American College of Cardiology. 2020 doi: 10.1016/j.jacc.2020.04.031. S0735-1097(20)35008-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonow R.O., Fonarow G.C., O’Gara P.T., Yancy C.W. Association of Coronavirus Disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiology. 2020 doi: 10.1001/jamacardio.2020.1105. [PMID: 32219362] [DOI] [PubMed] [Google Scholar]
- Calimport S.R.G., Bentley B.L., Stewart C.E., Pawelec G., Scuteri A., Vinciguerra M. To help aging populations, classify organismal senescence. Science. 2019;366:576–578. doi: 10.1126/science.aay7319. [PMID: 31672885] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Wu D., Guo W., Cao Y., Huang D., Wang H. Clinical and immunologic features in severe and moderate Coronavirus Disease 2019. The Journal of Clinical Investigation. 2020 doi: 10.1172/JCI137244. [PMID: 32217835] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggal N.A., Niemiro G., Harridge S.D.R., Simpson R.J., Lord J.M. Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity? Nature Reviews Immunology. 2019;19:563–572. doi: 10.1038/s41577-019-0177-9. [PMID: 31175337] [DOI] [PubMed] [Google Scholar]
- Gontijo Guerra S., Berbiche D., Vasiliadis H.M. Measuring multimorbidity in older adults: Comparing different data sources. BMC Geriatrics. 2019;19:166. doi: 10.1186/s12877-019-1173-4. [PMID: 31200651] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lainscak M., Vitale C. Biological and chronological age in heart failure: Role of immunosenescence. Journal of Cardiovascular Medicine (Hagerstown, Md) 2016;17(12):857–859. doi: 10.2459/JCM.0000000000000448. [DOI] [PubMed] [Google Scholar]
- Li H., Liu L., Zhang D., Xu J., Dai H., Tang N. SARS-CoV-2 and viral sepsis: Observations and hypotheses. Lancet. 2020;395(10235):1517–1520. doi: 10.1016/S0140-6736(20)30920-X. [PMID:32311318] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monto A.S., Rotthoff J., Teich E., Herlocher M.L., Truscon R., Yen H.L. Detection and control of influenza outbreaks in well-vaccinated nursing home populations. Clinical Infectious Diseases. 2004;39:459–464. doi: 10.1086/422646. [PMID: 15356805] [DOI] [PubMed] [Google Scholar]
- Moro-García M.A., Echeverría A., Galán-Artímez M.C., Suárez-García F.M., Solano-Jaurrieta J.J., Avanzas-Fernández P. Immunosenescence and inflammation characterize chronic heart failure patients with more advanced disease. International Journal of Cardiology. 2014;174:590–599. doi: 10.1016/j.ijcard.2014.04.128. [DOI] [PubMed] [Google Scholar]
- Pawelec G., Weng N.P. Can an effective SARS-CoV-2 vaccine be developed for the older population? Immunity & Ageing: I & A. 2020;17:8. doi: 10.1186/s12979-020-00180-2. [PMID: 32300370] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvi R., Patankar P. Emerging pharmacotherapies for COVID-19. Biomedicine & Pharmacotherapy. 2020 doi: 10.1016/j.biopha.2020.110267. [PMID: 32410772] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas R., Wang W., Su D.M. Contributions of age-related thymic involution to immunosenescence and inflammaging. Immunity & Ageing: I & A. 2020;17:2. doi: 10.1186/s12979-020-0173-8. [PMID: 31988649] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valk S.J., Piechotta V., Chai K.L., Doree C., Monsef I., Wood E.M. Convalescent plasma or hyperimmune immunoglobulin for people with COVID-19: A rapid review. The Cochrane Database of Systematic Reviews. 2020;5 doi: 10.1002/14651858. [PMID: 32406927] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. China novel coronavirus I and research t. A novel coronavirus from patients with pneumonia in China, 2019. The New England Journal of Medicine. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [PMID: 31978945] [DOI] [PMC free article] [PubMed] [Google Scholar]