Dear Editor,
Coronavirus disease (COVID-19) caused by the new coronavirus SARS-CoV-2 has hit the world as a global pandemic of an unprecedented scale. COVID-19 has become one of the major causes of death worldwide. It is estimated that around 5% of cases are critically ill, requiring intensive care unit (ICU) admission. As of June 29, 2020, United Arab Emirates counts 47,797 cases, with 313 deaths [1].
The observed ICU mortality rate of COVID-19 is highly variable [2], [3], [4], [5]. Also, no studies have reported the ICU outcomes of COVID-19 critically ill patients in the United Arab Emirates. The aim was to compare the published ICU case series [2], [3], [4], [5], [6], including ours, to understand the reasons for the differences in ICU mortality and if it is related to different ICU management of these patients (different rates of mechanical ventilation).
The institutional Ethics Committee of Cleveland Clinic Abu Dhabi approved the study (number: A-2020-035), and a waiver of informed consent was obtained. Series of ICU patients with confirmed COVID-19 infection from published cohorts were included [2], [3], [4], [5], [6]. Regarding our study, all consecutive adult patients admitted to our ICU between March 31 and May 10, 2020, with confirmed SARS-CoV-2 infection (virus detected by a real time reverse transcriptase-polymerase chain reaction assay of a nasopharyngeal sample) were included. De-identified data from the electronic medical record were collected. Continuous variables are expressed as mean ± SD or as median [interquartile range], and proportions were used for categorical variables.
Five ICU cohorts from four different countries (China, USA, Italy, and Spain) [2], [3], [4], [5], [6] were included along with our case series. The mean/median age was comparable between all these reported cohorts (60–64 years) except for our report, which was lower (51 ± 13 years) (Table 1 ). SOFA score was similar in Atlanta and Vitoria cohorts, but was higher than observed in our study. APACHE II score was comparable between the different reports (Table 1).
Table 1.
Intensive care management and clinical outcomes compared with case series from different countries.
| Abu Dhabi (UAE) (n = 55) | Seattle (USA) (n = 24) [3] | Atlanta (USA) (n = 217) [4] | Wuhan (China) (n = 52) [2] | Lombardy (Italy) (n = 1591) [5] | Vitoria (Spain) (n = 48) [6] | |
|---|---|---|---|---|---|---|
| Age, mean ± SD or median [IQR], yr | 51 ± 13 | 64 ± 18 | 64 [54–73] | 60 ± 13 | 63 [57–70] | 63 [51–75] |
| SOFA score, mean ± SD or median [IQR] | 4 [3–7] | – | 7 [5–11] | – | – | 7 ± 3 |
| APACHE II score, median [IQR] | 15 [12–20] | – | – | 17 [14–19] | – | 15 [12–19] |
| Intensive care therapy, n (%) | ||||||
| High-flow nasal cannula | 32 (58) | 10 (42) | – | 33 (63) | 0 (0) | 3 (6) |
| Non-invasive ventilation | 25 (45) | 0 (0) | – | 29 (56) | 137 (11) | 0 (0) |
| Invasive mechanical ventilation | 40 (73) | 18 (75) | 165 (76) | 22 (42) | 1150 (89) | 45 (94) |
| Hospital days prior to intubation, median (range), d | 0 (0-8) | – | - | – | – | – |
| Neuromuscular blockade | 34/40 (85) | 7/18 (39) | – | – | – | – |
| Prone position (PP) | 28/40 (70) | 5/18 (28) | – | 6/22 (27) | 240/875 (27) | 22/45 (49) |
| Days from intubation to PP, median (range) | 0 (0-8) | – | – | – | – | – |
| Number of PP sessions/patient, median (range) | 4 (1-13) | – | – | – | – | – |
| Longest duration of PP, median (range), hour | 23 (14-38) | – | – | – | – | – |
| Inhaled pulmonary vasodilators | 11 (20) | 5 (21) | 22 (10) | – | – | 0 (0) |
| ECMO | 6 (11) | 0 (0) | 4 (1.8) | 6 (11) | 5/498 (1) | 1 (2) |
| ICU days prior to ECMO, median (range) | 4 (0-7) | – | – | – | – | – |
| Vasopressors | 38 (69) | 17 (71) | 143 (66) | 18 (35) | – | – |
| ICU days prior to vasopressors use, median (range) | 1 (0-8) | – | – | – | – | – |
| Renal replacement therapy (RRT) | 11 (20) | – | 63 (29) | 9 (17) | – | – |
| ICU days prior to RRT, median (range) | 2 (0-16) | – | – | – | – | – |
| Outcomes | ||||||
| Length of follow-up, median (range), d | 26 (4-61) | – | – | – | – | – |
| Median length of stay, median [IQR], d | ||||||
| Overall, in ICU | 17 [8–34] | 9 [4–14] | 9 [5–15] | 9 [6–13] | ||
| In patients still in ICU | 52 [47–54] | – | 32 [28–41] | – | 10 [8–14] | – |
| In patients discharged from ICU | 14.5 [7–27] | – | – | 8 [5–12] | – | |
| In patients discharged from hospital | 22 [15–29] | – | – | – | – | |
| Duration of IMV, median [IQR], d | ||||||
| Overall | 18.5 [9–41] | 10 [7–12] | 9 [4–13] | |||
| In patients who were extubated | 12.5 [7–16] | 11 [7–12] | – | – | – | |
| Extubated, n/total n (%) | 20/40 (50) | 6/18 (33) | 101/165 (61) | 0/22 (0) | - | 10/45 (22) |
| Died in ICU, n (%) | 12 (22) | 12 (50) | 67 (31) | 32 (61) | 405/1581 (26) | 16 (33) |
| Death among patients with MV, n (%) | 11/40 (27) | – | 56/165 (34) | 30/37 (81) | - | 16/45 (36) |
| Time from ICU admission to death, median [IQR], d | 23 [7–35] | – | 9 [5–14] | – | 7 [5–11] | – |
| Discharged alive from ICU, n (%) | 38 (69) | – | 147 (68) | 14 (27) | 256 (16) | 13 (27) |
| Remains critically ill and requiring MV, n (%) | 4 (7) | 7 (29) | 8 (4) | 3(6) | - | 21 (44) |
| Discharged alive from hospital, n (%) | 34 (62) | 5 (21) | 131 (60) | – | – | – |
SOFA: Sequential Organ Failure Assessment; APACHE: Acute Physiology And Chronic Health Evaluation; PP: prone position; ECMO: extracorporeal membrane oxygenation; RRT: renal replacement therapy; MV: invasive mechanical ventilation; IQR: interquartile range.
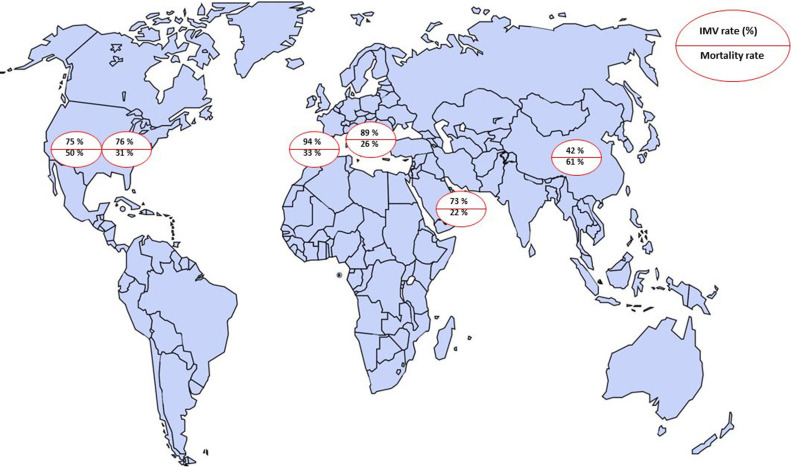
Mechanical ventilation (MV) rate in our patients was the same as in Seattle and Atlanta reports (75% and 76%, respectively), but higher than in the Wuhan series (42%), and lower than in Lombardy and Vitoria series (89% and 94%, respectively) (Table 1). Prone position rate was comparable in the USA, China, and Italy cohorts (∼27%), higher in the Spain report (49%), but much higher in our study (79%). The use of extracorporeal membrane oxygenation (ECMO) was similar in our and Wuhan reports (11%), but much higher than in the other cohorts (Table 1).
The mortality rate in Wuhan and Seattle were much higher (61% and 50%, respectively) compared with the other reported ICU cohorts ranging from 26% to 33% (Table 1 and Fig. 1 ). The mortality rate among patients who required MV was not reported in the Lombardy, and Seattle cohorts. The mortality rate among mechanically ventilated patients was much higher in the Wuhan study (81%) than in the other case series (34% to 36%) (Table 1). As of June 20, 2020, our overall mortality rate was 22% and 27% among mechanically ventilated patients.
Fig. 1.
Percentages of invasive mechanical ventilation (IMV) and ICU mortality in different countries (USA, Italy, Spain, China, and UAE).
The median duration of MV was comparable between the Seattle and Atlanta cohorts, but lower than in our study, which was 18.5 days [9–41] (Table 1). The median ICU length of stay (LOS) was also similar in the different reports, but much shorter than in our cohort (17 [8–34] days) (Table 1).
Table 1 compares our findings with ICU COVID-19 series from China [1], USA [3], [4], Italy [5], and Spain [6]. The rate of MV varied between the different cohorts [2], [3], [4], [5], [6] (Table 1). Various rates of intubation might be due to different strategies of managing COVID-19 acute respiratory failure. Some ICUs might be in favour of the early intubation approach in patients with high oxygen requirements [6]. Another explanation could be due to practice variation between centres. In some countries, high-flow oxygen therapy or non-invasive ventilation might be delivered mainly in hospital wards [5], whereas only patients at high risk of intubation were admitted to the ICU.
Our rates of prone position and ECMO use were markedly higher than the other cohorts [3], [4], [5], [6], reflecting the severity of our patients.
In the earliest reports from Wuhan [2] and Seattle [3], the MR of ICU COVID-19 patients were very high, raising concerns about the unfortunate outcome of these patients, especially among those who required MV. However, in the recent reports from Atlanta [4], Italy [5] and Spain [6], the mortality rate was much lower, ranged from 26% to 33% (Fig. 1). The use of MV cannot explain the difference in mortality rate between the earliest [2], [3] and recent cohorts [4], [5], [6]. Indeed, the observed mortality rate among patients requiring MV were 34% to 36% in the latest reports, even with higher rates of MV [4], [6]. In more recent data from the United Kingdom, 37% of those who received MV died [7]. The later arrival of the COVID-19 pandemic in different countries or regions might have provided time to establish organisational structures, prepare personnel, and create clinical protocols, which might explain the difference in mortality rate between cohorts [2], [3], [4], [5], [6].
A lower mortality rate (22%) was reported in our patients, even among those who received MV (27%). The younger age, lower SOFA score, and a higher rate of prone position might explain the mortality difference between our and the reported studies (Table 1).
Our data, along with the recent findings, suggest that the mortality rate in ICU COVID-19 patients are comparable and might be lower than those observed with acute respiratory distress syndrome (ARDS) caused by other viral infections [6].
The longer duration of MV and ICU LOS, in our study, is due to the longer follow-up period (median 26 [15–41] days) compared with the other cohorts [2], [3], [4], [5], [6].
This study has several limitations. First, the retrospective and descriptive design of all the included cohorts. Second, data from other countries are not represented in our study. Third, outcome data should be interpreted with caution as most patients were still hospitalised in ICU in many of the included cohorts. However, in our case series, only nine patients (16%) remained in hospital at the time of data censoring on June 20, 2020. Among them, only five patients were still in ICU. As a result, our reported MR would not change too much.
In conclusion, ICU mortality of COVID-19 patients is highly variable between the different cohorts and not explained by the MV's different rates. In the recent reports, the observed mortality rate for patients who required MV ranged from 27% to 36%, which are comparable to those seen with ARDS from other origins.
Disclosure of interest
The authors declare that they have no competing interest.
Funding
None.
Compliance with ethical standards
The study was approved by the Clinical Research Ethics Committee of Cleveland Clinic Abu Dhabi (number: A-2020-035) and consent was waived due to the observational nature of the study.
Consent for publication
Not applicable.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to privacy (patients’ data) but are available from the corresponding author on reasonable request.
Authors’ contributions
The study was designed by JM. JM enrolled patients and it is responsible for the integrity of data. JM, AN, KS, and BA collected data. Data analysis was performed by JM, FH. JM wrote the first draft of the manuscript. All authors contributed scientifically in the subsequent versions. All authors read and approved the final manuscript.
References
- 1.https://www.worldometers.info/coronavirus/
- 2.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhatraju P.K., Ghassemieh B.J., Nichols M., Kim R., Jerome K.R., Nalla A.K. Covid-19 in critically ill patients in the Seattle region — case series. N Engl J Med. 2020;382:2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Auld S.C., Caridi-Scheible M., Blum J.M., Robichaux C., Kraft C., Jacob J.T. ICU and ventilator mortality among critically ill adults with Coronavirus Disease 2019. Crit Care Med. 2020;26 doi: 10.1097/CCM.0000000000004457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barrasa H., Rello J., Tejada S., Martín A., Balziskueta G., Vinuesa C. SARS-CoV-2 in Spanish intensive care units: early experience with 15-day survival in Vitoria. Anaesth Crit Care Pain Med. 2020 doi: 10.1016/j.accpm.2020.04.001. [S2352-5568(20)30064-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to privacy (patients’ data) but are available from the corresponding author on reasonable request.