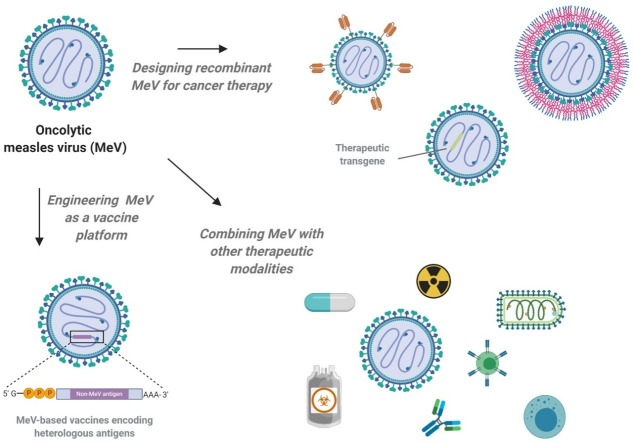
Graphical abstract
Abbreviations: 5-FUMP, 5-fluorouridine monophosphate; Ad, adenovirus; ATP, adenosine triphosphate; BiTE, bi-specific T-cell engager; CCNU, lomustine; CDV, canine distemper virus; CEA, carcinoembryonic antigen; CHIK, chikungunya; CPA, cyclophosphamide; CTLA-4, cytotoxic T-lymphocyte-associated protein 4; DCA, dichloroacetate; EGFR, epidermal growth factor receptor; EMA, European Medicines Agency; F, fusion; FDA, U.S. Food and Drug Administration; FMG, fusogenic membrane glycoprotein; GA, geldanamycin; GM-CSF, granulocyte-macrophage colony-stimulating factor; H, hemagglutinin; HCC, hepatocellular carcinoma; HADC, histone deacetylase; HSV, herpes simplex virus; i.p., intraperitoneal; i.t., intratumoral; ICI, immune checkpoint inhibition; IDO, indoleamine 2,3-dioxygenase; IFN, interferon; IL, interleukin; IRF, interferon regulatory factor; MAVS, mitochondrial antiviral signaling protein; MCP, membrane cofactor protein; MeV, measles virus; MOI, multiplicity of infection; NIS, sodium iodide symporter; NK, natural killer; OV, oncolytic virus; PD, programmed cell death; PNP, purine nucleoside phosphorylase; PVRL4, poliovirus receptor-like 4; RT, radiotherapy; SCD, super cytosine deaminase; scFv, single-chain variable fragment; SCID, severe combined immunodeficient; SLAMF1, signaling lymphocytic activation molecule, family member 1; TIL, tumor infiltrating lymphocyte; TME, tumor microenvironment; TMZ, temozolomide
Keywords: Measles virus, Genetic engineering, Virotherapy, Oncolytic virus, Immunotherapy, Combination therapy
Abstract
Cancer immunotherapy using tumor-selective, oncolytic viruses is an emerging therapeutic option for solid and hematologic malignancies. A considerable variety of viruses ranging from small picornaviruses to large poxviruses are currently being investigated as potential candidates. In the early days of virotherapy, non-engineered wild-type or vaccine-strain viruses were employed. However, these viruses often did not fully satisfy the major criteria of safety and efficacy. Since the advent of reverse genetics systems for manipulating various classes of viruses, the field has shifted to developing genetically engineered viruses with an improved therapeutic index. In this review, we will summarize the concepts and strategies of multi-level genetic engineering of oncolytic measles virus, a prime candidate for cancer immunovirotherapy. Furthermore, we will provide a brief overview of measles virus-based multimodal combination therapies for improved tumor control and clinical efficacy.
1. Introduction
Measles viruses (MeV) are enveloped, pleomorphic particles that belong to the family of Paramyxoviridae [1,2]. They harbor one or more copies of a non-segmented RNA genome of negative polarity and exhibit a natural lymphotropism in humans and primates [[3], [4], [5]]. Wild-type MeV uses CD150/SLAMF1 as an attachment receptor for entering different immune cells (macrophages, dendritic cells, activated or memory B and T cells) and Nectin-4/PVRL4 on cells of the airway epithelium to exit the host via the respiratory route [[6], [7], [8]]. Natural infection with wild-type MeV causes measles, a disease that is still responsible for more than 100,000 deaths per year worldwide, despite the availability of a safe and effective vaccine [9,10]. Attenuated, replication-competent vaccine strains of MeV exhibit a natural oncotropism and have thus been explored as novel anti-tumor therapeutics. Their dual mechanism of action includes direct lysis of infected cancer cells along with the release of tumor-associated antigens and the induction of an immunostimulatory tumor microenvironment. In addition to their excellent safety record and natural oncotropism, the possibility of multi-level genetic engineering makes MeV a promising oncolytic virus (OV) candidate (Fig. 1 ).
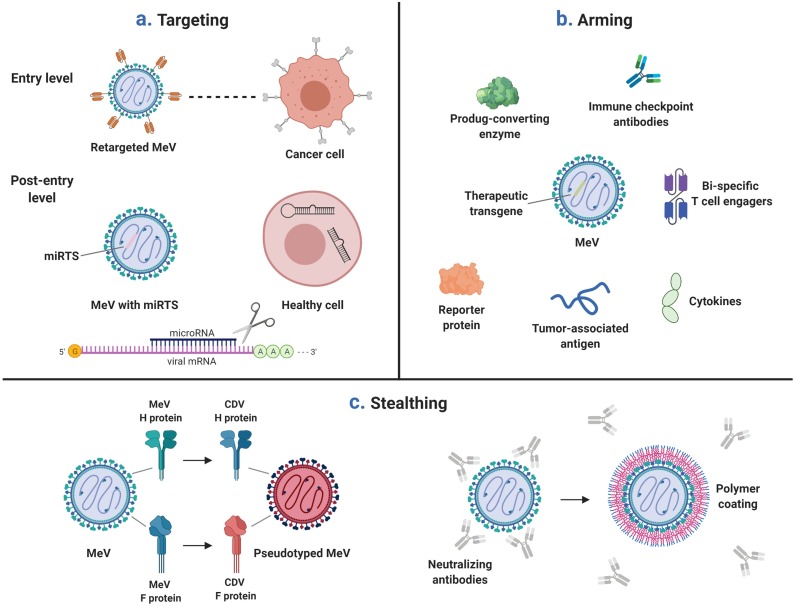
Fig. 1.
Targeting, arming, and stealthing of oncolytic MeV. a) Targeting and tumor-specificity of oncolytic MeV can be engineered on multiple levels. Entry targeting: Shown here is a fully-retargeted MeV that recognizes tumor antigens via scFv fused to the MeV H protein. Post-entry targeting: Displayed is an oncolytic MeV carrying target sites for microRNAs which are present in healthy cells but lost in malignant cells. This microRNA-controlled MeV is strongly attenuated in healthy cells expressing cognate microRNAs, but remains fully effective against tumor cells. b) Oncolytic MeV can be engineered to encode therapeutic transgenes. c) Stealthing of oncolytic MeV. Left: Pseudotyping of MeV with the envelope glycoproteins of a closely related paramyxovirus (canine distemper virus, CDV). Right: To avoid neutralization by pre-existing anti-MeV antibodies, it is possible to shield the individual virions using a polymeric envelope structure.
While next-generation oncolytic MeV are being developed pre-clinically, the first generation of recombinant MeV vaccine strains are already being tested in phase I/II clinical trials [11,12]. Recently reported data from the first trials are promising, with early indications of safety and anti-tumor activity [[13], [14], [15], [16]].
In this review, we will give an overview of genetic engineering strategies and combination therapies with oncolytic MeV. We will use the acronym TASC-MeV to structure this review and will discuss targeting, arming, and stealthing of oncolytic MeV, as well as combination therapies and measles virus as a vaccine platform. For further details on the mechanisms of oncolytic immunotherapy using measles virus, we refer the reader to the review article by Pidelaserra-Martí and Engeland in this special issue on oncolytic immunotherapy.
2. Targeting
When considering the use of replication-competent viruses as therapeutic agents for the treatment of cancer, tumor specificity is of critical importance to ensure both patient safety and therapeutic efficacy. OVs that are highly effective against a given cancer but lack tumor specificity resulting in substantial off-target replication and toxicity have limited to no clinical applicability. Likewise, OVs that may bind to many different cell types or that get sequestered in, for example, the liver might not reach the tumor in sufficient numbers, thus limiting their efficacy, especially when administered systemically. To address the issue of tumor-specificity, two main approaches have been employed: the selection of viruses with natural oncotropism, and the genetic modification of viruses resulting in engineered tumor specificity. A third option, the use of cell carriers with tumor-homing capabilities, will be discussed in the chapter “Stealthing and neutralizing antibodies”.
In MeV-based virotherapy, both natural oncotropism and engineered tumor-specificity come into play. The natural oncotropism of MeV has been first described in a well-known case report of a young boy whose Burkitt’s lymphoma regressed following infection with wild-type MeV [17]. The molecular basis for the natural tumor selectivity of MeV is primarily based on its receptor usage and its sensitivity towards the anti-viral interferon (IFN) response, which is often compromised in cancer cells. It should be noted that most of the pre-clinical and clinical constructs currently used in MeV-based virotherapy are derived from vaccine strains of MeV, which differ from the wild-type viruses not only in terms of pathogenicity but also in terms of receptor usage and ability to antagonize the IFN response. Wild-type strains utilize CD150/SLAM-F1 [8,18] and Nectin-4/PVRL-4 [6,7] as entry receptors, with the vaccine strains additionally using CD46/MCP [19,20]. CD150/SLAM-F1 is overexpressed on many hematological malignancies (including the aforementioned Burkitt’s lymphoma [21]), while CD46/MCP (a negative regulator of complement activity) is constitutively overexpressed on a wide variety of tumor cells [22]. Interestingly, some of the vaccine strains (incl. the Edmonston-B strain, from which MeV currently used in clinical trials are derived) carry mutations in the phosphoprotein (P) gene, which dampens their ability to control the host’s anti-viral IFN response [[23], [24], [25], [26], [27], [28]]. Since the IFN response is frequently dysregulated in malignant cells, this accounts - at least in part - for the preferential replication of vaccine-strain MeV in transformed cells.
Genetically engineered oncolytic MeV have been made possible by the development and refinement of a reverse genetics system allowing virus rescue from cloned DNA [29,30].
Engineered tumor-specificity, also referred to as “targeting”, has been achieved on the entry and post-entry level. In the case of entry-targeting, recognition of the natural receptor is prohibited by altering the amino acids responsible for receptor binding within the hemagglutinin (H) gene. In a second step, a novel tropism is conveyed by genetic fusion of targeting ligands to the “blinded” H gene. A variety of targeting molecules have been successfully tested, including different kinds of antibodies [[31], [32], [33], [34], [35], [36], [37]], DARPins [38,39], or ligands for cytokine/growth factor/cell membrane receptors [40,41]. In the case of post-entry targeting, microRNA target sites and artificial riboswitches have been explored. Global loss of microRNA expression levels in healthy versus malignant cells is an emerging hallmark of cancer and can be exploited by engineering OVs for increased tumor specificity. For this concept, target sequences of microRNAs which are lost in tumor cells, but expressed in healthy tissues, are inserted into the OV genome [[42], [43], [44], [45], [46]]. We have shown that this approach suppresses oncolytic MeV in microRNA-expressing healthy tissues, while replication kinetics and subsequent destruction of cancer cells remains unchanged [[47], [48], [49]].
Finally, it is possible to engineer inactive MeV, to be activated in the tumor microenvironment (TME) before exerting any cytotoxic activity. This can be achieved by the insertion of ectopic protease cleavage sites into the MeV F protein, as described by Springfeld et al. and Muehlebach et al. [50,51] By selecting cleavage motifs recognized by proteases frequently overexpressed and secreted by cancer cells (e.g., matrix metalloproteinase 2), preferential activation of oncolytic MeV in the TME can be achieved. Apart from this distinct activation of MeV in the TME, temporal particle inactivation can be achieved using small molecule-inducible ribozyme switches. These riboswitches can be engineered as RNA-based ON or OFF switches, and have been used by Ketzer et al. to design DNA-based OVs (adenoviruses) and RNA-based OVs (MeV) which are “switched off” by the addition of a small molecule riboswitch activator [52]. This genome modification adds another layer of safety, similarly to entry-targeted or microRNA-controlled oncolytic MeV.
3. Arming
With the development of reverse genetics and rescue system [29,30], MeV vaccine strains have become a powerful tool for transgene delivery. Three different attenuated MeV constructs have been administered to cancer patients in clinical trials, one unmodified, and two encoding reporter transgenes, the sodium iodide symporter (NIS) and carcinoembryonic antigen (CEA) [15,16,53]. A strong argument is to be made that future clinical trials will yield even better patient outcomes with the introduction of therapeutic transgenes. Though only demonstrated in pre-clinical models, NIS has the supplementary function as a therapeutic transgene in radiovirotherapy by driving intracellular uptake of 131I isotopes in infected cells [54]. Synergy between MeV-NIS and 131I radiotherapy has been shown in mice with subcutaneous human xenografts of pancreatic adenocarcinoma, medulloblastoma, prostate cancer, squamous cell carcinoma of the head and neck, and anaplastic thyroid cancer [[54], [55], [56], [57], [58]]. MeV-NIS has also been engineered to co-express IFN-beta, which led to enhanced infiltration of the tumor by innate immune cells as well as superior tumor control and overall survival in murine xenograft models of mesothelioma [59]. This approach leverages the capacity of OVs to express a given protein locally in cancer cells. Similarly, tumor-restricted activation of chemotherapeutics has been explored using prodrug convertases. Early experiments with virally-encoded prodrug convertases used Escherichia coli purine nucleoside phosphorylase (PNP) in conjunction with fludarabine to concentrate toxic ATP analogs in cancer cells [32,33,60]. Due to toxicity concerns from systemic fludarabine administration, the foundation of current chemovirotherapeutic strategies uses super cytosine deaminase (SCD/CD-UPRT), a fusion protein of yeast-derived cytosine deaminase and uracil phosphoribosyltransferase [[61], [62], [63], [64]]. SCD converts the prodrug 5-fluorocystosine into 5-fluorouracil then 5-fluorouridine monophosphate (5-FUMP). This process occurs exclusively in cancer cells due to the tumor-restricted expression of SCD. Cellular enzymes in cancer cells then process 5-FUMP into toxic metabolites that interfere with DNA repair, as well as DNA, RNA, and protein synthesis, leading to enhanced tumoricidal bystander effects [63].
The recent body of pre-clinical transgene research has had an emphasis on immunomodulation. Specifically, transgenes that strengthen the host’s immune response against the tumor are desirable. Following the observation that MeV was a suitable candidate as an OV, Grote et al. suspected that the host inflammatory response, particularly neutrophils, contributed to its therapeutic effect [65]. To address this, the cytokine granulocyte-macrophage colony-stimulating factor (GM-CSF) was encoded into MeV to potentiate neutrophil functions. In a SCID mouse model of human lymphoma, MeV encoding murine GM-CSF outperformed unmodified MeV, and its efficacy correlated with neutrophil infiltration in the tumor [65]. SCID mice lack B- and T-cells; therefore, the adaptive immune response towards the therapy was not analyzed. This was revisited using an immunocompetent murine colon adenocarcinoma model using MC38cea cells permissive to retargeted MeV-antiCEA [66]. In this study, we demonstrated that MeV-antiCEA armed with GM-CSF not only enhanced the median overall survival, but also led to a durable complete remission in one third of the mice. Mice treated with MeV-GM-CSF-antiCEA rejected tumors upon re-challenge, demonstrating an adaptive memory immune response with lasting protection [66]. GM-CSF as an OV transgene has effectively translated into the clinic as it is utilized in the first globally approved oncolytic virus Talimogene laherparepvec.
Immune checkpoint inhibitors are a breakthrough cancer immunotherapy that enable persistent activation of tumor-infiltrating lymphocytes (TILs); for this and other reasons, OVs are an ideal partner for combination therapy. OVs attract cytotoxic T lymphocytes to the tumor and upregulate the expression of PD-L1 on both cancer and immune cells [67,68]. In an attempt to combine MeV with immune checkpoint inhibition (ICI), we have virally-encoded PD-L1 and CTLA-4 antibodies and found that MeV virotherapy was greatly enhanced by ICI in an immunocompetent melanoma mouse model [69]. This demonstrated synergy between the two treatment modalities and showed how they can be engineered into a single, functional monotherapy. Bi-specific T-cell engagers (BiTEs) are another strategy to engage TILs toward cancer cells. BiTEs are covalently linked single-chain variable fragments with dual specificity for T-cells and a desired tumor antigen, thereby bringing them in proximity to form an artificial immunological synapse [70]. We have shown in a B16-CD20-CD46 mouse model that MeV encoding CD3xCD20 BiTEs cause a significant increase in CD8+ TILs and induce a protective anti-tumor immunity [71]. In another study, MeV-encoded IL-12 likewise enhanced the abundance of CD8+ TILs, and depletion experiments showed this T-cell subtype was crucial for its efficacy [72]. When comparing several immunomodulatory transgenes including IL-12, IP-10, a soluble form of CD80, GM-CSF, and PD-L1/CTLA-4 antibodies, the PD-L1 antibody- and IL-12- armed viruses were superior in their respective experiments [72]. MeV encoding IL-12 also showed a superior anti-tumor efficacy in MC38cea and B16-hCD46 tumor models when compared to an IL-15-encoding variant [73]. Finally, MeV encoding tumor-associated antigens have been engineered as an oncolytic vaccine platform, and shown to successfully prime and activate CD8+ T cells [74].
4. Stealthing and neutralizing antibodies
While oncolytic MeV offers many advantages as a therapeutic agent (most notably its excellent safety profile along with the possibility for multi-level genetic engineering), a major hurdle to its use systemically are pre-existing neutralizing antibodies. This is the case since most people in the western population have been previously immunized against this virus to confer immunity towards the pathogenic strain [75,76]. This poses a challenge for systemic administration of the virus since the neutralizing antibodies may bind and neutralize the virus before it reaches the tumor location [77]. A clinical trial of intraperitoneal MeV treatment in ovarian cancer patients that had neutralizing antibodies towards MeV was encouraging; however, it was hypothesised that the results could be improved by removing the pre-existing neutralizing antibodies [14]. This was likely due to the success of a disseminated myeloma clinical trial that utilized systemic administration of MeV in patients with no neutralizing antibodies towards the virus [13]. While these results are promising, as mentioned previously, the majority of the western population is immunized against MeV; therefore, many novel strategies have emerged to circumvent this potential obstacle. One such approach is pseudotyping, the substitution of envelope glycoproteins of one virus with another. Since MeV neutralizing antibodies recognize and achieve neutralization via binding to the F and H glycoproteins of MeV [76], exchanging these proteins with those of a closely related virus which the general population has not been exposed to would confer humoral immune evasion to the administered pseudotyped MeV.
Pseudotyping MeV for the goal of evading neutralizing antibodies has been achieved with several viruses with varying degrees of success. Measles was successfully pseudotyped with the closely related canine distemper virus (CDV) and was able to evade anti-MeV neutralizing antibodies [78,79]. Miest et al. demonstrated that the CDV-pseudotyped MeV had similar oncolytic properties to the original MeV. On the other hand, pseudotyping MeV with the Tupaia virus, also from the Paramyxoviridae family, generated a virus that was too attenuated and was no longer a viable oncolytic therapy [80]. It was also attempted to generate an H glycoprotein that will evade neutralization by inducing point mutations in typical antibody binding sites. While this was successful in stealthing a retargeted version of H, it was not effective for the endogenous form indicating shared epitopes for viral entry and antibody neutralization warranting the need for further insight on the matter [81].
Another approach for stealthing oncolytic MeV from neutralizing antibodies is to employ infected cell carriers. The concept is to infect designated cells with MeV and then administer this complex systemically. Once the infected cells reach the tumor location either passively or actively via cytokine homing [82], MeV spreads to the tumor via heterogeneous cell-cell fusion [83]. The infected cell carriers have been shown to protect its oncolytic cargo from circulating neutralizing antibodies [84]. Many types of cell carriers have been tested with oncolytic MeV, including transformed cells [85], mesenchymal stem cells [84], macrophages [86], dendritic cells [87], and T cells [83]. Apart from the choice of carrier cells, the particulars of the manufacturing process, such as loading dose and time [88], will likely influence the therapeutic efficacy achieved by this strategy.
Moreover, MeV stealthing has been achieved via a chemical modification - coating the virus particle with polyethylene glycol [89]. This was done with layer-by-layer deposition of ionic polymers at the MeV surface. Not only did the coated virus have better oncolytic capacity in the presence of neutralizing antibodies, but it also demonstrated better anti-tumor activity in vivo than the unmodified virus. A similar strategy was employed by Xia et al., where they coated the particle surface with graphene oxide and obtained similar results with the coated virus displaying superior tumor-killing ability in the presence of MeV neutralizing antibodies versus its bare counterpart [90].
Indirect strategies for overcoming MeV neutralizing antibodies have also been explored. Administration of immunosuppressors such as cyclophosphamide (CPA) prior to MeV treatment caused a drastic decrease in anti-MeV neutralizing antibodies in an in vivo mouse model [91] and resulted in enhanced oncolytic activity [60]. CPA acts by killing proliferating lymphocytes, thus ablating the humoral anti-viral response if administered following proper guidelines as outlined by Peng et al. [91]. A second approach that has been investigated in vitro is the use of UV-inactivated MeV prior to administration of the therapeutically active virus [92]. This effectively acts as a decoy for sequestering the pre-existing anti-MeV antibodies and might in turn boost the efficacy of the active virus administered shortly thereafter. While this depletion of anti-MeV antibodies might be an effective strategy in vitro, it remains to be seen if such a regimen can be translated safely into the clinic, especially when administering doses of oncolytic MeV repeatedly.
5. Combination therapies
5.1. MeV in combination with chemotherapy or other OVs
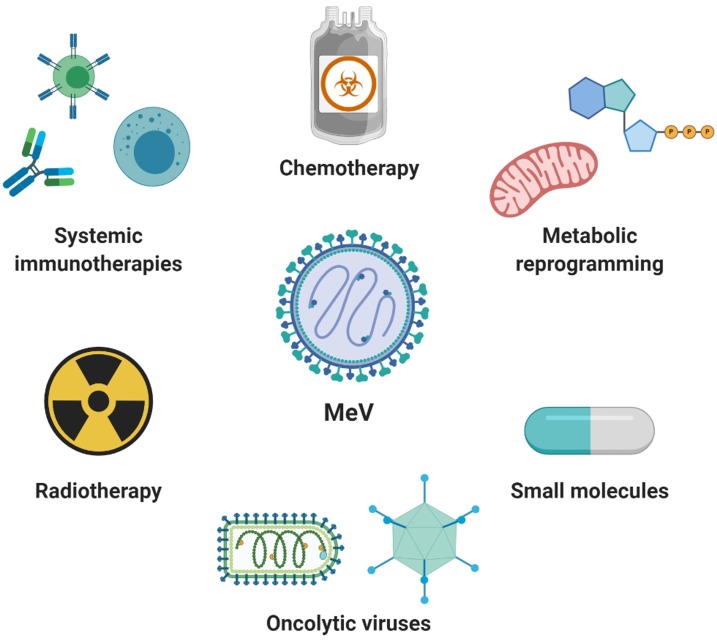
Chemotherapeutics remain at the forefront of cancer therapy. However, their therapeutic potential is limited by considerable toxicity, the occurrence of therapy resistance, and often a lack of durable disease control. With the emergence of MeV as a clinically well-tolerated and promising OV, it is feasible to combine oncolytic MeV with chemotherapy or other treatment modalities to augment tumor clearance (Fig. 2 ). Preliminary studies by Hoffmann et al. analyzed the combination of MeV fusogenic membrane glycoproteins (FMGs) H and F with chemotherapy as a potentially synergistic therapy approach [93]. In this study, pancreatic cancer cells infected with a replication-deficient, FMG-encoding adenovirus (Ad.H/F) in combination with gemcitabine, led to increased apoptotic events and cytotoxicity. Gemcitabine, a pyrimidine nucleoside analog, is frequently used for therapy of various cancers (including pancreatic ductal adenocarcinoma) and has shown synergy with other chemotherapeutics [94]. Mice receiving Ad.H/F and gemcitabine had increased survival as well as significantly reduced tumor volumes compared to single-agent treated animals [93]. In another study using a xenograft model of colorectal cancer, mice were treated with replication-defective, MeV FMG-encoding adenovirus (Ad.H/F) or herpes virus (HSV.H/F). These vectors were given alone or in combination with the chemotherapy regimen FOLFOX (folinic acid, 5-fluorouracil, oxaliplatin) and/or the respective trans-complementing, oncolytic adeno- or HSV vectors (enabling replication and intra-tumoral spread of otherwise replication-deficient Ad.H/F or HSV.H/F) [95]. In this study, triple combination therapy had the highest treatment efficacy compared to either single or double agent regimens. Collectively, intratumoral expression of MeV FMGs can synergize with chemotherapy to improve therapeutic outcomes.
Fig. 2.
Combination therapies involving oncolytic MeV. OVs in general, and MeV in particular, can be combined successfully with a variety of alternative treatment modalities, as displayed here.
More recently, replication-competent MeV has been combined with various therapeutics, including gemcitabine. An enhanced cytotoxic effect was observed in non-small cell lung cancer cells treated (in vitro) with a combination of gemcitabine and MeV, compared to single-agent treatment [96]. A combination of MeV and senescence inducing chemotherapeutics, such as gemcitabine, accelerates lysis of senescent cancer cells in various tumor types [97,98]. Co-treatment of MeV with low-dose camptothecin resulted in enhanced cytotoxicity in breast cancer cells and demonstrated the potential for a less toxic combination therapy [99]. In another study, triple chemo-viro-radiotherapy with MeV, temozolomide, and radiotherapy was shown to exert synergistic anti-glioma activity while inducing a pro-inflammatory phenotype [100]. In this context, we have demonstrated that a triple combination approach of MeV armed with a prodrug convertase (PNP) and delivered with the prodrug fludarabine with the chemotherapeutic cyclophosphamide resulted in complete tumor regression in vivo [60]. The combination of paclitaxel and recombinant MeV encoding BNiP3, a pro-apoptotic gene, was found to increase toxicity and apoptotic activity in breast cancer cells as well [101]. It should be noted that the individual combination of an OV with a chemotherapeutic drug, as well as the timing of their administration, needs to be carefully optimized for synergy. In some cases, however, chemotherapeutics can in fact antagonize the efficacy of immunovirotherapy, as recently described for the combination of IL-12-encoding HSV1 and temozolomide [102].
Synergy of MeV with other OVs has also been observed. For instance, the combination of measles and mumps virus has been found to increase oncolysis in various solid tumors and hematological malignancies in vitro, ex vivo, and in vivo, compared to stand-alone therapies [103,104]. Administration of MeV-CEA and MeV-NIS was found to decrease tumor burden compared to MeV-CEA alone, and also presents the possibility of dual non-invasive monitoring of virus spread via the soluble CEA peptide and NIS-based radioiodine imaging [105].
Altogether, these findings demonstrate that various combinatorial methods can enhance the efficacy of MeV-based virotherapy.
5.2. MeV in combination with radiotherapy
Combination of radiotherapy (RT) and MeV was tested mostly in glioblastoma cell lines [100,106]. The sequence in which RT and MeV are administered is critical to ensure the best outcome, with RT following MeV infection showing the greatest synergistic effect [100,106]. The mechanism underlying the synergy between RT and MeV combined therapy involves increased apoptosis through activation of FAS receptor signaling which in turn activates extrinsic caspase-8 pathways [106]. This synergistic cytotoxic effect was also seen in vivo, with enhanced tumor regression and survival, and, in some cases, complete and durable tumor eradication [106].
Moreover, chemotherapy in conjunction with RT and MeV may improve treatment outcomes even further. In particular, temozolomide (TMZ) and lomustine (CCNU), chemotherapies frequently used against glioblastoma, showed promise in this regard [100]. Maximal synergistic anti-tumor effects were found in a treatment regimen using either TMZ or CCNU first, followed by MeV infection, and then RT [100]. Triple combination therapy boosted anti-tumor effects even with cell lines that are resistant to one of the monotherapies [100]. A strong increase in IFN-β expression, antigen presentation, and the induction of pro-inflammatory cytokines ultimately enhanced the anti-tumor immune response [100].
5.3. MeV in combination with small molecules or metabolic reprograming
There are various mechanisms by which small molecules can enhance the therapeutic efficacy of MeV. These include dampening the cellular anti-viral response, altering metabolic pathways, or boosting the induction of apoptosis. In the following chapter, we will highlight some of these pharmaco-virotherapy approaches.
Epigenetic perturbations, and particularly histone modifications as key regulators of epigenetics, play a critical role in the development of cancer [107,108]. Indeed, resminostat, an inhibitor of class I and IIb histone deacetylase (HDAC) isoenzyme, has shown promising results in phase I/II clinical trials for the treatment of advanced-stage hepatocellular carcinoma (HCC) [109]. The combination of resminostat and MeV in HCC and pancreatic cancer cell lines enhanced anti-tumor activity of MeV and resulted in a 20–50 % reduction in cell viability compared to either monotherapy [110,111]. This enhanced efficacy of the combination therapy occurs through a more pronounced activation of intrinsic apoptotic pathways [111]. Interestingly, resminostat does not boost virus replication or spread but instead enhances the rate of primary infection without altering the MeV-induced IFN response [110,111]. Likewise, MeV did not interfere with the pharmacological function of resminostat as an HDAC inhibitor [110,111].
Pharmacological targeting of direct or indirect regulators of the cytoskeleton and mitotic spindle dynamics with, for instance, geldanamycin (GA), Y27632, or alisertib, is a common approach in cancer therapy. Geldanamycin (GA) is a heat shock protein 90 inhibitor that is ultimately thought to inactivate RhoA, a protein centrally involved in actin cytoskeleton dynamics [112]. Y27632 inhibits the RhoA downstream effector, Rho-associated coiled-coil-forming kinase (ROCK) [113]. Alisertib is a highly selective small-molecule inhibitor of the serine/threonine protein kinase Aurora A kinase [114]. Inhibition of Aurora A kinase results in a dysregulation of the mitotic spindle apparatus and thus chromosome segregation [114]. In breast, ovarian, rhabdomyosarcoma, and glioma cell lines treated with GA or Y27632 in combination with MeV, the number and average size of syncytia were increased [115,116]. In breast and glioma cell lines [116], these effects resulted from the disruption of the actin cytoskeleton and ultimately increased the anti-tumor effect of MeV. GA is known to increase apoptosis through the activation of extrinsic apoptotic pathways [115]. Indeed, the increased efficacy of MeV in combination with GA was not due to increased virus replication; instead, it was caused by GA-induced inactivation of RhoA and the consequent downstream dysregulation of cytoskeletal dynamics, transcriptional processes, and cell cycle progression which ultimately boosts syncytia formation and apoptosis [115]. Y27632 on the other hand, exerts its effect by enhancing MeV replication in a dose-dependent manner in vitro, which was further confirmed in vivo using a breast cancer mouse model [116]. Treating breast cancer cell lines with alisertib before MeV infection was shown to kill 97 % of cells at a low MOI, boosted virus replication 4-fold, and increased IL-24 expression [117]. The combination of alisertib with MeV in vivo led to higher survival rates compared to either monotherapy in a pleural effusion model of advanced breast cancer [117].
Targeting metabolism is another approach to eradicate cancer cells. It is well known that cancer cells alter metabolic processes to increase glucose uptake and promote fermentation of glucose to lactate, resulting in enhanced survival [118]. Selective interference with cellular metabolic processes can be combined with MeV for boosting its anti-tumor efficacy. In this context, alteration of glycolytic pathways with dichloroacetate (DCA) inhibits the conversion of pyruvate to lactate, thereby lowering the lactate level, glucose uptake, and ATP production [119]. DCA and MeV co-treatment resulted in a shortage of bioenergetic supplies, which induced necrosis in the tumor cells [119]. Additionally, DCA enhanced MeV replication by reducing the expression of key players of the anti-viral response, including IFNB1, CXCL10, MAVS, and phosphorylated IRF3, which led to increased tumor control in a glioblastoma model [119]. Similarly, human colorectal cancer cells subjected to long-term low-serum, glucose starvation potentiated the effects of MeV oncolysis compared to non-cancerous cells, suggesting differential stress resistance in healthy and tumor cells [120].
5.4. MeV in combination with systemic immunotherapies
The aim of oncolytic immunotherapy is to increase the immune system’s anti-tumor response, as well as to antagonize the immunosuppressive TME, which hinders therapeutic efficacy [121]. Combination of various immunotherapies with the pro-inflammatory MeV presents the possibility for synergy leading to enhanced therapeutic outcomes. A study by Chen et al. investigated the ability of MeV to improve adoptive CD8+ NKG2D+ cells against hepatocellular carcinoma (HCC) [122]. In HCC cells lines, MeV was found to increase anti-tumor activities of CD8+ NKG2D+ cells. Intratumoral injection of MeV followed by intravenous transfer of CD8+ NKG2D+ cells in HCC-bearing mouse models resulted in increased anti-tumor activity, inhibited HCC growth, and led to a significantly increased survival [122]. A caveat of this combinatorial approach was its capacity to induce expression of large amounts of the immune-suppressive enzyme IDO1. Additional administration of fludarabine, a chemotherapeutic agent, was able to successfully decrease levels of induced IDO1, demonstrating the importance of addressing therapy-induced immune suppression [122]. Another combinatorial approach employed oncolytic MeV with activated human NK cells, which resulted in increased release of NK cell cytolytic enzymes, and enhanced sarcoma cell destruction compared to monotherapies in vitro [123]. The separate administration of systemic checkpoint inhibitors and MeV has also been successful in vitro and in vivo. In the early stages of human glioma cell infection with MeV-NIS, an initial upregulation of PD-L1 was noted, demonstrating the immunosuppressive nature of gliomas and the logical approach of anti-PD-1 therapy. In the later stages of MeV-NIS infection, glioma cells release damage-associated molecular patterns (DAMPs). In mice bearing orthotopic GL261 gliomas, the combination of a MeV retargeted against EGFR (administered i.t.) and anti-PD-1 treatment (administered i.p.) enhanced survival, compared to stand-alone therapy or untreated mice, as a result of increased CD8+ T cell influx to tumor sites [67].
5.5. Measles virus as a vaccine platform
For over half a century, the widespread administration of the live attenuated MeV vaccine has greatly reduced the number of measles-related deaths and has demonstrated lifelong protection against infection accompanied by minimal side effects [124,125]. In addition to this excellent safety profile, the ability to generate recombinant MeV vectors from the various existing measles vaccine strains presents the possibility of generating vectors for immunization against a wide range of viruses. Specifically, MeV vectors have been pre-clinically developed as vaccines against chikungunya virus (CHIKV) [126], dengue virus [[127], [128], [129]], hepatitis B virus (HBV) [[130], [131], [132]], hepatitis C virus (HCV) [133], HIV [[134], [135], [136], [137]], human papillomavirus (HPV) [138,139], MERS [140,141], SARS [142,143], Nipah virus [144], respiratory syncytial virus [[145], [146], [147]], West Nile virus [148,149], and Zika virus [150]. MeV-CHIKV has successfully completed phase I clinical trials and is progressing through phase II testing (NCT03028441, NCT02861586, NCT03635086). Additionally, the therapeutic effects of MeV-ZIKA (NCT02996890, NCT04033068), MeV-Lassa virus (NCT04055454), and recombinant HIV measles vaccine vector (NCT01320176) are being evaluated at various stages of clinical trials. Currently, we and others are working on the development and clinical translation of a MeV-vectored COVID-19 vaccine.
6. Concluding remarks
Oncolytic immunotherapeutics have come a long way from being an unusual concept to being one of the most innovative and promising novel immunotherapeutics in cancer therapy. This shift in perception of OVs from oddities to viable therapeutic modalities has strengthened considerably with the FDA and EMA approval of Talimogene laherparepvec, an engineered oncolytic herpes simplex virus encoding GM-CSF, for the treatment of advanced-stage melanoma. Following this breakthrough for the field, a large variety of OVs based on very different virus families and strains are being developed pre-clinically or are currently being evaluated in clinical trials. As we have discussed here, vaccine strain-derived oncolytic MeV are among the most promising OV candidates. They have an excellent safety record, can be genetically engineered on multiple levels, and have successfully been combined with various established treatment regimens. Multiple phase I-II clinical trials with oncolytic MeV are currently ongoing and the first reported data seem promising. Some of the crucial questions for the next years will be: How can we select the patients who could benefit most from OV therapy? Can we elucidate the molecular principles that are divergent between responding and non-responding patients? Can we exploit this knowledge to engineer next-generation viruses or conceive combination therapies that are successful in patients who do not respond to currently available therapies? We strongly believe that OVs, and oncolytic MeV in particular, can be further developed and translated into a modern immunotherapy for the benefit of cancer patients.
Funding information
Ontario Institute for Cancer Research (OICR) Clinician-Scientist grant (to GU), Terry-Fox New Investigator award (to GU).
CRediT authorship contribution statement
Mathias F. Leber: Conceptualization, Supervision, Writing - original draft, Writing - review & editing, Visualization. Serge Neault: Writing - original draft, Writing - review & editing. Elise Jirovec: Writing - original draft, Writing - review & editing. Russell Barkley: Writing - original draft, Writing - review & editing. Aida Said: Writing - original draft, Writing - review & editing. John C. Bell: Supervision, Funding acquisition, Writing - review & editing. Guy Ungerechts: Conceptualization, Supervision, Funding acquisition, Writing - review & editing.
Declaration of Competing Interest
GU is co-founder, stakeholder, and CMO/CSO of CanVirex AG, a company investigating oncolytic viruses as novel cancer immunotherapeutics. JCB is co-founder and stakeholder of Turnstone Biologics, a company developing viral immunotherapeutics against cancer. The remaining authors declare no conflict of interest.
Acknowledgments
We thank Dr. Tommy Alain (Children’s Hospital of Eastern Ontario, Ottawa, ON, Canada) for his continuous support. All Figures were created with BioRender.com.
Biographies

Mathias F. Leber, MD, PhD, is a clinician-scientist, and currently works as a Senior Research Associate and Head of Laboratory at the Ottawa Hospital Research Institute (Cancer Therapeutics Program). His main research interests are novel immuno-virotherapy approaches and the genetic engineering of oncolytic viruses using small RNAs.

Serge Neault is a Ph.D. student at the University of Ottawa in Ottawa, Canada. His current research interest is in the design of oncolytic viruses for a novel treatment of cancers.

Elise Jirovec recently completed her Bachelor’s degree in Biopharmaceutical Science at the University of Ottawa and is starting her Master’s degree in Innovative Medicine at Heidelberg University. Her current research interest is in the design of a novel virotherapy for cancer treatment.

Russell Barkley is a Master’s student at the University of Ottawa with a deep curiosity for all things unknown. He enjoys creating fresh ideas and being puzzled by new discoveries. Outside of the laboratory he can be found at the local ice hockey rink.

Aida Said obtained her MSc. in Neuroscience from the Faculty of Medicine, University of Ottawa. She is currently pursuing a PhD degree in Microbiology and Immunology at the Faculty of Medicine, University of Ottawa. Her research interest is focused on developing treatments for cancer by combining oncolytic measles virus with kinase inhibitors.

John C. Bell, PhD, is a Senior Scientist in the Cancer Therapeutics Program at the Ottawa Hospital Research Institute and a Professor of Medicine at the University of Ottawa. He is also the Scientific Director of BioCanRx, a network of scientists, clinicians, cancer stakeholders, academic institutions, NGOs and industry partners aiming at the development of leading-edge immune oncology therapies. John is also a co-founder of Turnstone Biologics, a company developing viral immunotherapeutics against cancer. Since 2012, he heads the Terry Fox-funded Canadian Oncolytic Virus Consortium, which is developing virus-based cancer therapeutics, and he is the Director of the Biotherapeutics Program for the Ontario Institute for Cancer Research. In addition, John is the Scientific Director of the National Centre of Excellence for the development of Biotherapeutics for Cancer Therapy and a fellow of the Royal Society of Canada.

Guy Ungerechts, MD, PhD, is the Deputy Director of the Department of Medical Oncology at the Heidelberg University Hospital in Heidelberg, Germany, and Head of the Clinical Cooperation Unit “Virotherapy” at the German Cancer Research Center in Heidelberg, Germany. He is also the co-founder of CanVirex, a spin-off company from the University Hospital Heidelberg, focused on the development of novel immunovirotherapies. Guy is an affiliated investigator at the Ottawa Hospital Research Institute (Cancer Therapeutics Program). His main research interest is the translation of oncolytic immunotherapies from bench to bedside.
References
- 1.Aref S., Bailey K., Fielding A. Measles to the rescue: a review of oncolytic measles virus. Viruses. 2016;8(10) doi: 10.3390/v8100294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daikoku E., Morita C., Kohno T., Sano K. Analysis of morphology and infectivity of measles virus particles. Bull. Osaka Med. Coll. 2007;53:107–114. [Google Scholar]
- 3.Bellini W.J., Rota J.S., Rota P.A. Virology of measles virus. J. Infect. Dis. 1994;170(Suppl 1):S15–23. doi: 10.1093/infdis/170.supplement_1.s15. [DOI] [PubMed] [Google Scholar]
- 4.Cattaneo R., Donohue R.C., Generous A.R., Navaratnarajah C.K., Pfaller C.K. Stronger together: multi-genome transmission of measles virus. Virus Res. 2019;265:74–79. doi: 10.1016/j.virusres.2019.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rima B.K., Duprex W.P. The measles virus replication cycle. Curr. Top. Microbiol. Immunol. 2009;329:77–102. doi: 10.1007/978-3-540-70523-9_5. [DOI] [PubMed] [Google Scholar]
- 6.Noyce R.S., Bondre D.G., Ha M.N., Lin L.T., Sisson G., Tsao M.S., Richardson C.D. Tumor cell marker PVRL4 (nectin 4) is an epithelial cell receptor for measles virus. PLoS Pathog. 2011;7(8) doi: 10.1371/journal.ppat.1002240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muhlebach M.D., Mateo M., Sinn P.L., Prufer S., Uhlig K.M., Leonard V.H., Navaratnarajah C.K., Frenzke M., Wong X.X., Sawatsky B., Ramachandran S., McCray P.B., Jr, Cichutek K., von Messling V., Lopez M., Cattaneo R. Adherens junction protein nectin-4 is the epithelial receptor for measles virus. Nature. 2011;480(7378):530–533. doi: 10.1038/nature10639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tatsuo H., Ono N., Tanaka K., Yanagi Y. SLAM (CDw150) is a cellular receptor for measles virus. Nature. 2000;406(6798):893–897. doi: 10.1038/35022579. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . 2019. Measles.https://www.who.int/news-room/fact-sheets/detail/measles Published May 9, (Accessed November 20, 2019) [Google Scholar]
- 10.Griffin D.E., Lin W.H., Pan C.H. Measles virus, immune control, and persistence. FEMS Microbiol. Rev. 2012;36(3):649–662. doi: 10.1111/j.1574-6976.2012.00330.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pol G.J., Levesque S., Workenhe S.T., Gujar S., Le Boeuf F., R.C. D, Fahrner J.E., Fend L., C.B. J, L.M. K, Fucikova J., Spisek R., Zitvogel L., Kroemer G., Galluzzi L., Watch Trial. Oncolytic viro-immunotherapy of hematologic and solid tumors. Oncoimmunology. 2018;7(12) doi: 10.1080/2162402X.2018.1503032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Msaouel P., Opyrchal M., Dispenzieri A., Peng K.W., Federspiel M.J., Russell S.J., Galanis E. Clinical trials with oncolytic measles virus: current status and future prospects. Curr. Cancer Drug Targets. 2018;18(2):177–187. doi: 10.2174/1568009617666170222125035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russell S.J., Federspiel M.J., Peng K.W., Tong C., Dingli D., Morice W.G., Lowe V., O’Connor M.K., Kyle R.A., Leung N., Buadi F.K., Rajkumar S.V., Gertz M.A., Lacy M.Q., Dispenzieri A. Remission of disseminated cancer after systemic oncolytic virotherapy. Mayo Clin. Proc. 2014;89(7):926–933. doi: 10.1016/j.mayocp.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galanis E., Atherton P.J., Maurer M.J., Knutson K.L., Dowdy S.C., Cliby W.A., Haluska P., Jr, Long H.J., Oberg A., Aderca I., Block M.S., Bakkum-Gamez J., Federspiel M.J., Russell S.J., Kalli K.R., Keeney G., Peng K.W., Hartmann L.C. Oncolytic measles virus expressing the sodium iodide symporter to treat drug-resistant ovarian cancer. Cancer Res. 2015;75(1):22–30. doi: 10.1158/0008-5472.CAN-14-2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galanis E., Hartmann L.C., Cliby W.A., Long H.J., Peethambaram P.P., Barrette B.A., Kaur J.S., Haluska P.J., Jr, Aderca I., Zollman P.J., Sloan J.A., Keeney G., Atherton P.J., Podratz K.C., Dowdy S.C., Stanhope C.R., Wilson T.O., Federspiel M.J., Peng K.W., Russell S.J. Phase I trial of intraperitoneal administration of an oncolytic measles virus strain engineered to express carcinoembryonic antigen for recurrent ovarian cancer. Cancer Res. 2010;70(3):875–882. doi: 10.1158/0008-5472.CAN-09-2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dispenzieri A., Tong C., LaPlant B., Lacy M.Q., Laumann K., Dingli D., Zhou Y., Federspiel M.J., Gertz M.A., Hayman S., Buadi F., O’Connor M., Lowe V.J., Peng K.W., Russell S.J. Phase I trial of systemic administration of Edmonston strain of measles virus genetically engineered to express the sodium iodide symporter in patients with recurrent or refractory multiple myeloma. Leukemia. 2017;31(12):2791–2798. doi: 10.1038/leu.2017.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bluming A.Z., Ziegler J.L. Regression of Burkitt’s lymphoma in association with measles infection. Lancet. 1971;2(7715):105–106. doi: 10.1016/s0140-6736(71)92086-1. [DOI] [PubMed] [Google Scholar]
- 18.Navaratnarajah C.K., Vongpunsawad S., Oezguen N., Stehle T., Braun W., Hashiguchi T., Maenaka K., Yanagi Y., Cattaneo R. Dynamic interaction of the measles virus hemagglutinin with its receptor signaling lymphocytic activation molecule (SLAM, CD150) J. Biol. Chem. 2008;283(17):11763–11771. doi: 10.1074/jbc.M800896200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dorig R.E., Marcil A., Chopra A., Richardson C.D. The human CD46 molecule is a receptor for measles virus (Edmonston strain) Cell. 1993;75(2):295–305. doi: 10.1016/0092-8674(93)80071-l. [DOI] [PubMed] [Google Scholar]
- 20.Naniche D., Varior-Krishnan G., Cervoni F., Wild T.F., Rossi B., Rabourdin-Combe C., Gerlier D. Human membrane cofactor protein (CD46) acts as a cellular receptor for measles virus. J. Virol. 1993;67(10):6025–6032. doi: 10.1128/jvi.67.10.6025-6032.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gordiienko I.M., Shlapatska L.M., Kovalevska L.M., Sidorenko S.P. Differential expression of CD150/SLAMF1 in normal and malignant B cells on the different stages of maturation. Exp. Oncol. 2016;38(2):101–107. [PubMed] [Google Scholar]
- 22.Anderson B.D., Nakamura T., Russell S.J., Peng K.W. High CD46 receptor density determines preferential killing of tumor cells by oncolytic measles virus. Cancer Res. 2004;64(14):4919–4926. doi: 10.1158/0008-5472.CAN-04-0884. [DOI] [PubMed] [Google Scholar]
- 23.Haralambieva I.H., Ovsyannikova I.G., Dhiman N., Vierkant R.A., Jacobson R.M., Poland G.A. Differential cellular immune responses to wild-type and attenuated edmonston tag measles virus strains are primarily defined by the viral phosphoprotein gene. J. Med. Virol. 2010;82(11):1966–1975. doi: 10.1002/jmv.21899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Naniche D. Human immunology of measles virus infection. Curr. Top. Microbiol. Immunol. 2009;330:151–171. doi: 10.1007/978-3-540-70617-5_8. [DOI] [PubMed] [Google Scholar]
- 25.Naniche D., Yeh A., Eto D., Manchester M., Friedman R.M., Oldstone M.B. Evasion of host defenses by measles virus: wild-type measles virus infection interferes with induction of Alpha/Beta interferon production. J. Virol. 2000;74(16):7478–7484. doi: 10.1128/jvi.74.16.7478-7484.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ohno S., Ono N., Takeda M., Takeuchi K., Yanagi Y. Dissection of measles virus V protein in relation to its ability to block alpha/beta interferon signal transduction. J. Gen. Virol. 2004;85(Pt 10):2991–2999. doi: 10.1099/vir.0.80308-0. [DOI] [PubMed] [Google Scholar]
- 27.Devaux P., Hodge G., McChesney M.B., Cattaneo R. Attenuation of V- or C-defective measles viruses: infection control by the inflammatory and interferon responses of rhesus monkeys. J. Virol. 2008;82(11):5359–5367. doi: 10.1128/JVI.00169-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Devaux P., Hudacek A.W., Hodge G., Reyes-Del Valle J., McChesney M.B., Cattaneo R. A recombinant measles virus unable to antagonize STAT1 function cannot control inflammation and is attenuated in rhesus monkeys. J. Virol. 2011;85(1):348–356. doi: 10.1128/JVI.00802-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Radecke F., Spielhofer P., Schneider H., Kaelin K., Huber M., Dotsch C., Christiansen G., Billeter M.A. Rescue of measles viruses from cloned DNA. EMBO J. 1995;14(23):5773–5784. doi: 10.1002/j.1460-2075.1995.tb00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martin A., Staeheli P., Schneider U. RNA polymerase II-controlled expression of antigenomic RNA enhances the rescue efficacies of two different members of the Mononegavirales independently of the site of viral genome replication. J. Virol. 2006;80(12):5708–5715. doi: 10.1128/JVI.02389-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bossow S., Grossardt C., Temme A., Leber M.F., Sawall S., Rieber E.P., Cattaneo R., von Kalle C., Ungerechts G. Armed and targeted measles virus for chemovirotherapy of pancreatic cancer. Cancer Gene Ther. 2011;18(8):598–608. doi: 10.1038/cgt.2011.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ungerechts G., Springfeld C., Frenzke M.E., Lampe J., Johnston P.B., Parker W.B., Sorscher E.J., Cattaneo R. Lymphoma chemovirotherapy: CD20-targeted and convertase-armed measles virus can synergize with fludarabine. Cancer Res. 2007;67(22):10939–10947. doi: 10.1158/0008-5472.CAN-07-1252. [DOI] [PubMed] [Google Scholar]
- 33.Ungerechts G., Springfeld C., Frenzke M.E., Lampe J., Parker W.B., Sorscher E.J., Cattaneo R. An immunocompetent murine model for oncolysis with an armed and targeted measles virus. Mol. Ther. 2007;15(11):1991–1997. doi: 10.1038/sj.mt.6300291. [DOI] [PubMed] [Google Scholar]
- 34.Zaoui K., Bossow S., Grossardt C., Leber M.F., Springfeld C., Plinkert P.K., Kalle C., Ungerechts G. Chemovirotherapy for head and neck squamous cell carcinoma with EGFR-targeted and CD/UPRT-armed oncolytic measles virus. Cancer Gene Ther. 2012;19(3):181–191. doi: 10.1038/cgt.2011.75. [DOI] [PubMed] [Google Scholar]
- 35.Nakamura T., Peng K.W., Harvey M., Greiner S., Lorimer I.A., James C.D., Russell S.J. Rescue and propagation of fully retargeted oncolytic measles viruses. Nat. Biotechnol. 2005;23(2):209–214. doi: 10.1038/nbt1060. [DOI] [PubMed] [Google Scholar]
- 36.Allen C., Vongpunsawad S., Nakamura T., James C.D., Schroeder M., Cattaneo R., Giannini C., Krempski J., Peng K.W., Goble J.M., Uhm J.H., Russell S.J., Galanis E. Retargeted oncolytic measles strains entering via the EGFRvIII receptor maintain significant antitumor activity against gliomas with increased tumor specificity. Cancer Res. 2006;66(24):11840–11850. doi: 10.1158/0008-5472.CAN-06-1200. [DOI] [PubMed] [Google Scholar]
- 37.Bach P., Abel T., Hoffmann C., Gal Z., Braun G., Voelker I., Ball C.R., Johnston I.C., Lauer U.M., Herold-Mende C., Muhlebach M.D., Glimm H., Buchholz C.J. Specific elimination of CD133+ tumor cells with targeted oncolytic measles virus. Cancer Res. 2013;73(2):865–874. doi: 10.1158/0008-5472.CAN-12-2221. [DOI] [PubMed] [Google Scholar]
- 38.Friedrich K., Hanauer J.R., Prufer S., Munch R.C., Volker I., Filippis C., Jost C., Hanschmann K.M., Cattaneo R., Peng K.W., Pluckthun A., Buchholz C.J., Cichutek K., Muhlebach M.D. DARPin-targeting of measles virus: unique bispecificity, effective oncolysis, and enhanced safety. Mol. Ther. 2013;21(4):849–859. doi: 10.1038/mt.2013.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanauer J.R.H., Koch V., Lauer U.M., Muhlebach M.D. High-affinity DARPin allows targeting of MeV to glioblastoma multiforme in combination with protease targeting without loss of potency. Mol. Ther. Oncolytics. 2019;15:186–200. doi: 10.1016/j.omto.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Allen C., Paraskevakou G., Iankov I., Giannini C., Schroeder M., Sarkaria J., Puri R.K., Russell S.J., Galanis E. Interleukin-13 displaying retargeted oncolytic measles virus strains have significant activity against gliomas with improved specificity. Mol. Ther. 2008;16(9):1556–1564. doi: 10.1038/mt.2008.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jing Y., Zaias J., Duncan R., Russell S.J., Merchan J.R. In vivo safety, biodistribution and antitumor effects of uPAR retargeted oncolytic measles virus in syngeneic cancer models. Gene Ther. 2014;21(3):289–297. doi: 10.1038/gt.2013.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ylosmaki E., Hakkarainen T., Hemminki A., Visakorpi T., Andino R., Saksela K. Generation of a conditionally replicating adenovirus based on targeted destruction of E1A mRNA by a cell type-specific MicroRNA. J. Virol. 2008;82(22):11009–11015. doi: 10.1128/JVI.01608-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Edge R.E., Falls T.J., Brown C.W., Lichty B.D., Atkins H., Bell J.C. A let-7 MicroRNA-sensitive vesicular stomatitis virus demonstrates tumor-specific replication. Mol. Ther. 2008;16(8):1437–1443. doi: 10.1038/mt.2008.130. [DOI] [PubMed] [Google Scholar]
- 44.Kelly E.J., Hadac E.M., Cullen B.R., Russell S.J. MicroRNA antagonism of the picornaviral life cycle: alternative mechanisms of interference. PLoS Pathog. 2010;6(3) doi: 10.1371/journal.ppat.1000820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kelly E.J., Hadac E.M., Greiner S., Russell S.J. Engineering microRNA responsiveness to decrease virus pathogenicity. Nat. Med. 2008;14(11):1278–1283. doi: 10.1038/nm.1776. [DOI] [PubMed] [Google Scholar]
- 46.Kelly E.J., Nace R., Barber G.N., Russell S.J. Attenuation of vesicular stomatitis virus encephalitis through microRNA targeting. J. Virol. 2010;84(3):1550–1562. doi: 10.1128/JVI.01788-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leber M.F., Bossow S., Leonard V.H., Zaoui K., Grossardt C., Frenzke M., Miest T., Sawall S., Cattaneo R., von Kalle C., Ungerechts G. MicroRNA-sensitive oncolytic measles viruses for cancer-specific vector tropism. Mol. Ther. 2011;19(6):1097–1106. doi: 10.1038/mt.2011.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baertsch M.A., Leber M.F., Bossow S., Singh M., Engeland C.E., Albert J., Grossardt C., Jager D., von Kalle C., Ungerechts G. MicroRNA-mediated multi-tissue detargeting of oncolytic measles virus. Cancer Gene Ther. 2014;21(9):373–380. doi: 10.1038/cgt.2014.40. [DOI] [PubMed] [Google Scholar]
- 49.Leber M.F., Baertsch M.A., Anker S.C., Henkel L., Singh H.M., Bossow S., Engeland C.E., Barkley R., Hoyler B., Albert J., Springfeld C., Jager D., von Kalle C., Ungerechts G. Enhanced control of oncolytic measles virus using MicroRNA target sites. Mol. Ther. Oncolytics. 2018;9:30–40. doi: 10.1016/j.omto.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Springfeld C., von Messling V., Frenzke M., Ungerechts G., Buchholz C.J., Cattaneo R. Oncolytic efficacy and enhanced safety of measles virus activated by tumor-secreted matrix metalloproteinases. Cancer Res. 2006;66(15):7694–7700. doi: 10.1158/0008-5472.CAN-06-0538. [DOI] [PubMed] [Google Scholar]
- 51.Muhlebach M.D., Schaser T., Zimmermann M., Armeanu S., Hanschmann K.M., Cattaneo R., Bitzer M., Lauer U.M., Cichutek K., Buchholz C.J. Liver cancer protease activity profiles support therapeutic options with matrix metalloproteinase-activatable oncolytic measles virus. Cancer Res. 2010;70(19):7620–7629. doi: 10.1158/0008-5472.CAN-09-4650. [DOI] [PubMed] [Google Scholar]
- 52.Ketzer P., Kaufmann J.K., Engelhardt S., Bossow S., von Kalle C., Hartig J.S., Ungerechts G., Nettelbeck D.M. Artificial riboswitches for gene expression and replication control of DNA and RNA viruses. Proc. Natl. Acad. Sci. U. S. A. 2014;111(5):E554–62. doi: 10.1073/pnas.1318563111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Heinzerling L., Kunzi V., Oberholzer P.A., Kundig T., Naim H., Dummer R. Oncolytic measles virus in cutaneous T-cell lymphomas mounts antitumor immune responses in vivo and targets interferon-resistant tumor cells. Blood. 2005;106(7):2287–2294. doi: 10.1182/blood-2004-11-4558. [DOI] [PubMed] [Google Scholar]
- 54.Msaouel P., Iankov I.D., Allen C., Aderca I., Federspiel M.J., Tindall D.J., Morris J.C., Koutsilieris M., Russell S.J., Galanis E. Noninvasive imaging and radiovirotherapy of prostate cancer using an oncolytic measles virus expressing the sodium iodide symporter. Mol. Ther. 2009;17(12):2041–2048. doi: 10.1038/mt.2009.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hutzen B., Pierson C.R., Russell S.J., Galanis E., Raffel C., Studebaker A.W. Treatment of medulloblastoma using an oncolytic measles virus encoding the thyroidal sodium iodide symporter shows enhanced efficacy with radioiodine. BMC Cancer. 2012;12:508. doi: 10.1186/1471-2407-12-508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li H., Peng K.W., Russell S.J. Oncolytic measles virus encoding thyroidal sodium iodide symporter for squamous cell cancer of the head and neck radiovirotherapy. Hum. Gene Ther. 2012;23(3):295–301. doi: 10.1089/hum.2011.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Penheiter A.R., Wegman T.R., Classic K.L., Dingli D., Bender C.E., Russell S.J., Carlson S.K. Sodium iodide symporter (NIS)-mediated radiovirotherapy for pancreatic cancer. AJR Am. J. Roentgenol. 2010;195(2):341–349. doi: 10.2214/AJR.09.3672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Reddi H.V., Madde P., McDonough S.J., Trujillo M.A., Morris J.C., 3rd, Myers R.M., Peng K.W., Russell S.J., McIver B., Eberhardt N.L. Preclinical efficacy of the oncolytic measles virus expressing the sodium iodide symporter in iodine non-avid anaplastic thyroid cancer: a novel therapeutic agent allowing noninvasive imaging and radioiodine therapy. Cancer Gene Ther. 2012;19(9):659–665. doi: 10.1038/cgt.2012.47. [DOI] [PubMed] [Google Scholar]
- 59.Li H., Peng K.W., Dingli D., Kratzke R.A., Russell S.J. Oncolytic measles viruses encoding interferon beta and the thyroidal sodium iodide symporter gene for mesothelioma virotherapy. Cancer Gene Ther. 2010;17(8):550–558. doi: 10.1038/cgt.2010.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ungerechts G., Frenzke M.E., Yaiw K.C., Miest T., Johnston P.B., Cattaneo R. Mantle cell lymphoma salvage regimen: synergy between a reprogrammed oncolytic virus and two chemotherapeutics. Gene Ther. 2010;17(12):1506–1516. doi: 10.1038/gt.2010.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kaufmann J.K., Bossow S., Grossardt C., Sawall S., Kupsch J., Erbs P., Hassel J.C., von Kalle C., Enk A.H., Nettelbeck D.M., Ungerechts G. Chemovirotherapy of malignant melanoma with a targeted and armed oncolytic measles virus. J. Invest. Dermatol. 2013;133(4):1034–1042. doi: 10.1038/jid.2012.459. [DOI] [PubMed] [Google Scholar]
- 62.Maurer S., Salih H.R., Smirnow I., Lauer U.M., Berchtold S. Suicide genearmed measles vaccine virus for the treatment of AML. Int. J. Oncol. 2019 doi: 10.3892/ijo.2019.4835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lampe J., Bossow S., Weiland T., Smirnow I., Lehmann R., Neubert W., Bitzer M., Lauer U.M. An armed oncolytic measles vaccine virus eliminates human hepatoma cells independently of apoptosis. Gene Ther. 2013;20(11):1033–1041. doi: 10.1038/gt.2013.28. [DOI] [PubMed] [Google Scholar]
- 64.Lange S., Lampe J., Bossow S., Zimmermann M., Neubert W., Bitzer M., Lauer U.M. A novel armed oncolytic measles vaccine virus for the treatment of cholangiocarcinoma. Hum. Gene Ther. 2013;24(5):554–564. doi: 10.1089/hum.2012.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Grote D., Cattaneo R., Fielding A.K. Neutrophils contribute to the measles virus-induced antitumor effect: enhancement by granulocyte macrophage colony-stimulating factor expression. Cancer Res. 2003;63(19):6463–6468. [PubMed] [Google Scholar]
- 66.Grossardt C., Engeland C.E., Bossow S., Halama N., Zaoui K., Leber M.F., Springfeld C., Jaeger D., von Kalle C., Ungerechts G. Granulocyte-macrophage colony-stimulating factor-armed oncolytic measles virus is an effective therapeutic cancer vaccine. Hum. Gene Ther. 2013;24(7):644–654. doi: 10.1089/hum.2012.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hardcastle J., Mills L., Malo C.S., Jin F., Kurokawa C., Geekiyanage H., Schroeder M., Sarkaria J., Johnson A.J., Galanis E. Immunovirotherapy with measles virus strains in combination with anti-PD-1 antibody blockade enhances antitumor activity in glioblastoma treatment. Neuro-Oncology. 2017;19(4):493–502. doi: 10.1093/neuonc/now179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu Z., Ravindranathan R., Kalinski P., Guo Z.S., Bartlett D.L. Rational combination of oncolytic vaccinia virus and PD-L1 blockade works synergistically to enhance therapeutic efficacy. Nat. Commun. 2017;8:14754. doi: 10.1038/ncomms14754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Engeland C.E., Grossardt C., Veinalde R., Bossow S., Lutz D., Kaufmann J.K., Shevchenko I., Umansky V., Nettelbeck D.M., Weichert W., Jager D., von Kalle C., Ungerechts G. CTLA-4 and PD-L1 checkpoint blockade enhances oncolytic measles virus therapy. Mol. Ther. 2014;22(11):1949–1959. doi: 10.1038/mt.2014.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dietz L., Engeland C.E. Immunomodulation in oncolytic measles virotherapy. Methods Mol. Biol. 2020;2058:111–126. doi: 10.1007/978-1-4939-9794-7_7. [DOI] [PubMed] [Google Scholar]
- 71.Speck T., Heidbuechel J.P.W., Veinalde R., Jaeger D., von Kalle C., Ball C.R., Ungerechts G., Engeland C.E. Targeted BiTE expression by an oncolytic vector augments therapeutic efficacy against solid tumors. Clin. Cancer Res. 2018;24(9):2128–2137. doi: 10.1158/1078-0432.CCR-17-2651. [DOI] [PubMed] [Google Scholar]
- 72.Veinalde R., Grossardt C., Hartmann L., Bourgeois-Daigneault M.C., Bell J.C., Jager D., von Kalle C., Ungerechts G., Engeland C.E. Oncolytic measles virus encoding interleukin-12 mediates potent antitumor effects through T cell activation. Oncoimmunology. 2017;6(4) doi: 10.1080/2162402X.2017.1285992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Backhaus Veinalde, Hartmann Dunder, Jeworowski Albert, Hoyler Poth, Jäger, Ungerechts, Engeland Immunological effects and viral gene expression determine the efficacy of oncolytic measles vaccines encoding IL-12 or IL-15 agonists. Viruses. 2019;11(10):914. doi: 10.3390/v11100914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Busch E., Kubon K.D., Mayer J.K.M., Pidelaserra-Martí G., Albert J., Hoyler B., Heidbuechel J.P.W., Stephenson K.B., Lichty B.D., Osen W., Eichmüller S.B., Jäger D., Ungerechts G., Engeland C.E. Measles vaccines designed for enhanced CD8+ T cell activation. Viruses. 2020;12(2):242. doi: 10.3390/v12020242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bankamp B., Takeda M., Zhang Y., Xu W., Rota P.A. Genetic characterization of measles vaccine strains. J. Infect. Dis. 2011;204(Suppl 1):S533–48. doi: 10.1093/infdis/jir097. [DOI] [PubMed] [Google Scholar]
- 76.Polack F.P., Lee S.H., Permar S., Manyara E., Nousari H.G., Jeng Y., Mustafa F., Valsamakis A., Adams R.J., Robinson H.L., Griffin D.E. Successful DNA immunization against measles: neutralizing antibody against either the hemagglutinin or fusion glycoprotein protects rhesus macaques without evidence of atypical measles. Nat. Med. 2000;6(7):776–781. doi: 10.1038/77506. [DOI] [PubMed] [Google Scholar]
- 77.Russell S.J., Peng K.W. Measles virus for cancer therapy. Curr. Top. Microbiol. Immunol. 2009;330:213–241. doi: 10.1007/978-3-540-70617-5_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Miest T.S., Yaiw K.C., Frenzke M., Lampe J., Hudacek A.W., Springfeld C., von Messling V., Ungerechts G., Cattaneo R. Envelope-chimeric entry-targeted measles virus escapes neutralization and achieves oncolysis. Mol. Ther. 2011;19(10):1813–1820. doi: 10.1038/mt.2011.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Muñoz-Alía M.A., Russell S.J. Probing morbillivirus antisera neutralization using functional chimerism between measles virus and canine distemper virus envelope glycoproteins. Viruses. 2019;11(8):688. doi: 10.3390/v11080688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hudacek A.W., Navaratnarajah C.K., Cattaneo R. Development of measles virus-based shielded oncolytic vectors: suitability of other paramyxovirus glycoproteins. Cancer Gene Ther. 2013;20(2):109–116. doi: 10.1038/cgt.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lech P.J., Pappoe R., Nakamura T., Tobin G.J., Nara P.L., Russell S.J. Antibody neutralization of retargeted measles viruses. Virology. 2014;454-455:237–246. doi: 10.1016/j.virol.2014.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hakkarainen T., Sarkioja M., Lehenkari P., Miettinen S., Ylikomi T., Suuronen R., Desmond R.A., Kanerva A., Hemminki A. Human mesenchymal stem cells lack tumor tropism but enhance the antitumor activity of oncolytic adenoviruses in orthotopic lung and breast tumors. Hum. Gene Ther. 2007;18(7):627–641. doi: 10.1089/hum.2007.034. [DOI] [PubMed] [Google Scholar]
- 83.Ong H.T., Hasegawa K., Dietz A.B., Russell S.J., Peng K.W. Evaluation of T cells as carriers for systemic measles virotherapy in the presence of antiviral antibodies. Gene Ther. 2007;14(4):324–333. doi: 10.1038/sj.gt.3302880. [DOI] [PubMed] [Google Scholar]
- 84.Mader E.K., Maeyama Y., Lin Y., Butler G.W., Russell H.M., Galanis E., Russell S.J., Dietz A.B., Peng K.W. Mesenchymal stem cell carriers protect oncolytic measles viruses from antibody neutralization in an orthotopic ovarian cancer therapy model. Clin. Cancer Res. 2009;15(23):7246–7255. doi: 10.1158/1078-0432.CCR-09-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Iankov I.D., Blechacz B., Liu C., Schmeckpeper J.D., Tarara J.E., Federspiel M.J., Caplice N., Russell S.J. Infected cell carriers: a new strategy for systemic delivery of oncolytic measles viruses in cancer virotherapy. Mol. Ther. 2007;15(1):114–122. doi: 10.1038/sj.mt.6300020. [DOI] [PubMed] [Google Scholar]
- 86.Peng K.W., Dogan A., Vrana J., Liu C., Ong H.T., Kumar S., Dispenzieri A., Dietz A.B., Russell S.J. Tumor-associated macrophages infiltrate plasmacytomas and can serve as cell carriers for oncolytic measles virotherapy of disseminated myeloma. Am. J. Hematol. 2009;84(7):401–407. doi: 10.1002/ajh.21444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Iankov I.D., Msaouel P., Allen C., Federspiel M.J., Bulur P.A., Dietz A.B., Gastineau D., Ikeda Y., Ingle J.N., Russell S.J., Galanis E. Demonstration of anti-tumor activity of oncolytic measles virus strains in a malignant pleural effusion breast cancer model. Breast Cancer Res. Treat. 2010;122(3):745–754. doi: 10.1007/s10549-009-0602-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xu C., Xia M., Meng G., Li C., Jiang A., Wei J. Carrier cells for delivery of oncolytic measles virus into tumors: determinants of efficient loading. Virol. Sin. 2018;33(3):234–240. doi: 10.1007/s12250-018-0033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nosaki K., Hamada K., Takashima Y., Sagara M., Matsumura Y., Miyamoto S., Hijikata Y., Okazaki T., Nakanishi Y., Tani K. A novel, polymer-coated oncolytic measles virus overcomes immune suppression and induces robust antitumor activity. Mol. Ther. Oncolytics. 2016;3:16022. doi: 10.1038/mto.2016.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Xia M., Luo D., Dong J., Zheng M., Meng G., Wu J., Wei J. Graphene oxide arms oncolytic measles virus for improved effectiveness of cancer therapy. J. Exp. Clin. Cancer Res. 2019;38(1):408. doi: 10.1186/s13046-019-1410-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Peng K.W., Myers R., Greenslade A., Mader E., Greiner S., Federspiel M.J., Dispenzieri A., Russell S.J. Using clinically approved cyclophosphamide regimens to control the humoral immune response to oncolytic viruses. Gene Ther. 2013;20(3):255–261. doi: 10.1038/gt.2012.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Xu C., Goss A.V., Dorneburg C., Debatin K.M., Wei J., Beltinger C. Proof-of-principle that a decoy virus protects oncolytic measles virus against neutralizing antibodies. Oncolytic Virother. 2018;7:37–41. doi: 10.2147/OV.S150637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hoffmann D., Wildner O. Enhanced killing of pancreatic cancer cells by expression of fusogenic membrane glycoproteins in combination with chemotherapy. Mol. Cancer Ther. 2006;5(8):2013–2022. doi: 10.1158/1535-7163.MCT-06-0128. [DOI] [PubMed] [Google Scholar]
- 94.Toschi L., Finocchiaro G., Bartolini S., Gioia V., Cappuzzo F. Role of gemcitabine in cancer therapy. Future Oncol. 2005;1(1):7–17. doi: 10.1517/14796694.1.1.7. [DOI] [PubMed] [Google Scholar]
- 95.Hoffmann D., Bangen J.M., Bayer W., Wildner O. Synergy between expression of fusogenic membrane proteins, chemotherapy and facultative virotherapy in colorectal cancer. Gene Ther. 2006;13(21):1534–1544. doi: 10.1038/sj.gt.3302806. [DOI] [PubMed] [Google Scholar]
- 96.Patel M.R., Jacobson B.A., Belgum H., Raza A., Sadiq A., Drees J., Wang H., Jay-Dixon J., Etchison R., Federspiel M.J., Russell S.J., Kratzke R.A. Measles vaccine strains for virotherapy of non-small-cell lung carcinoma. J. Thorac. Oncol. 2014;9(8):1101–1110. doi: 10.1097/JTO.0000000000000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.May V., Berchtold S., Berger A., Venturelli S., Burkard M., Leischner C., Malek N.P., Lauer U.M. Chemovirotherapy for pancreatic cancer: gemcitabine plus oncolytic measles vaccine virus. Oncol. Lett. 2019;18(5):5534–5542. doi: 10.3892/ol.2019.10901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Weiland T., Lampe J., Essmann F., Venturelli S., Berger A., Bossow S., Berchtold S., Schulze-Osthoff K., Lauer U.M., Bitzer M. Enhanced killing of therapy-induced senescent tumor cells by oncolytic measles vaccine viruses. Int. J. Cancer. 2014;134(1):235–243. doi: 10.1002/ijc.28350. [DOI] [PubMed] [Google Scholar]
- 99.Tai C.J., Liu C.H., Pan Y.C., Wong S.H., Tai C.J., Richardson C.D., Lin L.T. Chemovirotherapeutic treatment using camptothecin enhances oncolytic measles virus-mediated killing of breast cancer cells. Sci. Rep. 2019;9(1):6767. doi: 10.1038/s41598-019-43047-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rajaraman S., Canjuga D., Ghosh M., Codrea M.C., Sieger R., Wedekink F., Tatagiba M., Koch M., Lauer U.M., Nahnsen S., Rammensee H.G., Muhlebach M.D., Stevanovic S., Tabatabai G. Measles virus-based treatments trigger a pro-inflammatory cascade and a distinctive immunopeptidome in Glioblastoma. Mol. Ther. Oncolytics. 2019;12:147–161. doi: 10.1016/j.omto.2018.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lal G., Rajala M.S. Combination of oncolytic measles virus armed with BNiP3, a pro-apoptotic gene and paclitaxel induces breast cancer cell death. Front. Oncol. 2018;8:676. doi: 10.3389/fonc.2018.00676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Saha D., Rabkin S.D., Martuza R.L. Temozolomide antagonizes oncolytic immunovirotherapy in glioblastoma. J. Immunother. Cancer. 2020;8(1) doi: 10.1136/jitc-2019-000345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Son H.A., Zhang L., Cuong B.K., Van Tong H., Cuong L.D., Hang N.T., Nhung H.T.M., Yamamoto N., Toan N.L. Combination of vaccine-strain measles and mumps viruses enhances oncolytic activity against human solid malignancies. Cancer Invest. 2018;36(2):106–117. doi: 10.1080/07357907.2018.1434539. [DOI] [PubMed] [Google Scholar]
- 104.Zhang L.F., Tan D.Q., Jeyasekharan A.D., Hsieh W.S., Ho A.S., Ichiyama K., Ye M., Pang B., Ohba K., Liu X., de Mel S., Cuong B.K., Chng W.J., Ryo A., Suzuki Y., Yeoh K.G., Toan N.L., Yamamoto N. Combination of vaccine-strain measles and mumps virus synergistically kills a wide range of human hematological cancer cells: special focus on acute myeloid leukemia. Cancer Lett. 2014;354(2):272–280. doi: 10.1016/j.canlet.2014.08.034. [DOI] [PubMed] [Google Scholar]
- 105.Hasegawa K., Pham L., O’Connor M.K., Federspiel M.J., Russell S.J., Peng K.W. Dual therapy of ovarian cancer using measles viruses expressing carcinoembryonic antigen and sodium iodide symporter. Clin. Cancer Res. 2006;12(6):1868–1875. doi: 10.1158/1078-0432.CCR-05-1803. [DOI] [PubMed] [Google Scholar]
- 106.Liu C., Sarkaria J.N., Petell C.A., Paraskevakou G., Zollman P.J., Schroeder M., Carlson B., Decker P.A., Wu W., James C.D., Russell S.J., Galanis E. Combination of measles virus virotherapy and radiation therapy has synergistic activity in the treatment of glioblastoma multiforme. Clin. Cancer Res. 2007;13(23):7155–7165. doi: 10.1158/1078-0432.CCR-07-1306. [DOI] [PubMed] [Google Scholar]
- 107.Kurdistani S.K. Histone modifications as markers of cancer prognosis: a cellular view. Br. J. Cancer. 2007;97(1):1–5. doi: 10.1038/sj.bjc.6603844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Berger S.L., Kouzarides T., Shiekhattar R., Shilatifard A. An operational definition of epigenetics. Genes Dev. 2009;23(7):781–783. doi: 10.1101/gad.1787609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhao J., Gray S.G., Wabitsch M., Greene C.M., Lawless M.W. The therapeutic properties of resminostat for hepatocellular carcinoma. Oncoscience. 2018;5(5-6):196–208. doi: 10.18632/oncoscience.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ellerhoff T.P., Berchtold S., Venturelli S., Burkard M., Smirnow I., Wulff T., Lauer U.M. Novel epi-virotherapeutic treatment of pancreatic cancer combining the oral histone deacetylase inhibitor resminostat with oncolytic measles vaccine virus. Int. J. Oncol. 2016;49(5):1931–1944. doi: 10.3892/ijo.2016.3675. [DOI] [PubMed] [Google Scholar]
- 111.Ruf B., Berchtold S., Venturelli S., Burkard M., Smirnow I., Prenzel T., Henning S.W., Lauer U.M. Combination of the oral histone deacetylase inhibitor resminostat with oncolytic measles vaccine virus as a new option for epi-virotherapeutic treatment of hepatocellular carcinoma. Mol. Ther. Oncolytics. 2015;2:15019. doi: 10.1038/mto.2015.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Amiri A., Noei F., Feroz T., Lee J.M. Geldanamycin anisimycins activate Rho and stimulate Rho- and ROCK-dependent actin stress fiber formation. Mol. Cancer Res. 2007;5(9):933–942. doi: 10.1158/1541-7786.MCR-06-0362. [DOI] [PubMed] [Google Scholar]
- 113.Ishizaki T., Uehata M., Tamechika I., Keel J., Nonomura K., Maekawa M., Narumiya S. Pharmacological properties of Y-27632, a specific inhibitor of rho-associated kinases. Mol. Pharmacol. 2000;57(5):976–983. [PubMed] [Google Scholar]
- 114.Asteriti I.A., Di Cesare E., De Mattia F., Hilsenstein V., Neumann B., Cundari E., Lavia P., Guarguaglini G. The Aurora-A inhibitor MLN8237 affects multiple mitotic processes and induces dose-dependent mitotic abnormalities and aneuploidy. Oncotarget. 2014;5(15):6229–6242. doi: 10.18632/oncotarget.2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Liu C., Erlichman C., McDonald C.J., Ingle J.N., Zollman P., Iankov I., Russell S.J., Galanis E. Heat shock protein inhibitors increase the efficacy of measles virotherapy. Gene Ther. 2008;15(14):1024–1034. doi: 10.1038/gt.2008.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Opyrchal M., Allen C., Msaouel P., Iankov I., Galanis E. Inhibition of Rho-associated coiled-coil-forming kinase increases efficacy of measles virotherapy. Cancer Gene Ther. 2013;20(11):630–637. doi: 10.1038/cgt.2013.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Iankov I.D., Kurokawa C.B., D’Assoro A.B., Ingle J.N., Domingo-Musibay E., Allen C., Crosby C.M., Nair A.A., Liu M.C., Aderca I., Federspiel M.J., Galanis E. Inhibition of the Aurora a kinase augments the anti-tumor efficacy of oncolytic measles virotherapy. Cancer Gene Ther. 2015;22(9):438–444. doi: 10.1038/cgt.2015.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Liberti M.V., Locasale J.W. The Warburg effect: how does it benefit Cancer cells? Trends Biochem. Sci. 2016;41(3):211–218. [Google Scholar]
- 119.Li C., Meng G., Su L., Chen A., Xia M., Xu C., Yu D., Jiang A., Wei J. Dichloroacetate blocks aerobic glycolytic adaptation to attenuated measles virus and promotes viral replication leading to enhanced oncolysis in glioblastoma. Oncotarget. 2015;6(3):1544–1555. doi: 10.18632/oncotarget.2838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Scheubeck G., Berchtold S., Smirnow I., Schenk A., Beil J., Lauer U.M. Starvation-induced differential virotherapy using an oncolytic measles vaccine virus. Viruses. 2019;11(7) doi: 10.3390/v11070614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Achard C., Surendran A., Wedge M.E., Ungerechts G., Bell J., Ilkow C.S. Lighting a fire in the tumor microenvironment using oncolytic immunotherapy. EBioMedicine. 2018;31:17–24. doi: 10.1016/j.ebiom.2018.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chen A., Zhang Y., Meng G., Jiang D., Zhang H., Zheng M., Xia M., Jiang A., Wu J., Beltinger C., Wei J. Oncolytic measles virus enhances antitumour responses of adoptive CD8(+)NKG2D(+) cells in hepatocellular carcinoma treatment. Sci. Rep. 2017;7(1):5170. doi: 10.1038/s41598-017-05500-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Klose C., Berchtold S., Schmidt M., Beil J., Smirnow I., Venturelli S., Burkard M., Handgretinger R., Lauer U.M. Biological treatment of pediatric sarcomas by combined virotherapy and NK cell therapy. BMC Cancer. 2019;19(1):1172. doi: 10.1186/s12885-019-6387-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.McLean H.Q., Fiebelkorn A.P., Temte J.L., Wallace G.S. MMWR Recommendations and Reports. 2013. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP) [PubMed] [Google Scholar]
- 125.W.H. Organization . 2012. GLOBAL MEASLES AND RUBELLA: Strategic Plan 2012-2020. [Google Scholar]
- 126.Brandler S., Ruffié C., Combredet C., Brault J.B., Najburg V., Prevost M.C., Habel A., Tauber E., Desprès P., Tangy F. A recombinant measles vaccine expressing chikungunya virus-like particles is strongly immunogenic and protects mice from lethal challenge with chikungunya virus. Vaccine. 2013 doi: 10.1016/j.vaccine.2013.05.086. [DOI] [PubMed] [Google Scholar]
- 127.Brandler S., Lucas-Hourani M., Moris A., Frenkiel M.P., Combredet C., Février M., Bedouelle H., Schwartz O., Desprès P., Tangy F. Pediatric measles vaccine expressing a dengue antigen induces durable serotype-specific neutralizing antibodies to dengue virus. PLoS Negl. Trop. Dis. 2007 doi: 10.1371/journal.pntd.0000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hu H.M., Chen H.W., Hsiao Y.J., Wu S.H., Chung H.H., Hsieh C.H., Chong P., Leng C.H., Pan C.H. The successful induction of T-cell and antibody responses by a recombinant measles virus-vectored tetravalent dengue vaccine provides partial protection against dengue-2 infection. Hum. Vaccin. Immunother. 2016 doi: 10.1080/21645515.2016.1143576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Brandler S., Ruffie C., Najburg V., Frenkiel M.P., Bedouelle H., Desprès P., Tangy F. Pediatric measles vaccine expressing a dengue tetravalent antigen elicits neutralizing antibodies against all four dengue viruses. Vaccine. 2010 doi: 10.1016/j.vaccine.2010.07.073. [DOI] [PubMed] [Google Scholar]
- 130.Singh M., Cattaneo R., Billeter M.A. A recombinant measles virus expressing hepatitis B virus surface antigen induces humoral immune responses in genetically modified mice. J. Virol. 1999;73(6):4823–4828. doi: 10.1128/jvi.73.6.4823-4828.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.del Valle J.R., Devaux P., Hodge G., Wegner N.J., McChesney M.B., Cattaneo R. A vectored measles virus induces hepatitis B surface antigen antibodies while protecting macaques against measles virus challenge. J. Virol. 2007;81(19):10597–10605. doi: 10.1128/JVI.00923-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Reyes-del Valle J., Hodge G., McChesney M.B., Cattaneo R. Protective anti-hepatitis B virus responses in rhesus monkeys primed with a vectored measles virus and boosted with a single dose of hepatitis B surface antigen. J. Virol. 2009;83(17):9013–9017. doi: 10.1128/JVI.00906-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Reyes-del Valle J., de la Fuente C., Turner M.A., Springfeld C., Apte-Sengupta S., Frenzke M.E., Forest A., Whidby J., Marcotrigiano J., Rice C.M., Cattaneo R. Broadly neutralizing immune responses against hepatitis C virus induced by vectored measles viruses and a recombinant envelope protein booster. J. Virol. 2012;86(21):11558–11566. doi: 10.1128/JVI.01776-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Guerbois M., Moris A., Combredet C., Najburg V., Ruffié C., Février M., Cayet N., Brandler S., Schwartz O., Tangy F. Live attenuated measles vaccine expressing HIV-1 Gag virus like particles covered with gp160ΔV1V2 is strongly immunogenic. Virology. 2009 doi: 10.1016/j.virol.2009.02.047. [DOI] [PubMed] [Google Scholar]
- 135.Liniger M., Zuniga A., Morin T.N.A., Combardiere B., Marty R., Wiegand M., Ilter O., Knuchel M., Naim H.Y. Recombinant measles viruses expressing single or multiple antigens of human immunodeficiency virus (HIV-1) induce cellular and humoral immune responses. Vaccine. 2009 doi: 10.1016/j.vaccine.2009.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lorin C., Segal L., Mols J., Morelle D., Bourguignon P., Rovira O., Mettens P., Silvano J., Dumey N., Le Goff F., Koutsoukos M., Voss G., Tangy F. Toxicology, biodistribution and shedding profile of a recombinant measles vaccine vector expressing HIV-1 antigens, in cynomolgus macaques. Naunyn Schmiedebergs Arch. Pharmacol. 2012 doi: 10.1007/s00210-012-0793-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Stebbings R., Février M., Li B., Lorin C., Koutsoukos M., Mee E., Rose N., Hall J., Page M., Almond N., Voss G., Tangy F. Immunogenicity of a recombinant Measles-HIV-1 clade B candidate vaccine. PLOS ONE. 2012 doi: 10.1371/journal.pone.0050397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Cantarella G., Liniger M., Zuniga A., Schiller J.T., Billeter M., Naim H.Y., Glueck R. Recombinant measles virus-HPV vaccine candidates for prevention of cervical carcinoma. Vaccine. 2009 doi: 10.1016/j.vaccine.2009.01.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Gupta G., Giannino V., Rishi N., Glueck R. Immunogenicity of next-generation HPV vaccines in non-human primates: measles-vectored HPV vaccine versus Pichia pastoris recombinant protein vaccine. Vaccine. 2016 doi: 10.1016/j.vaccine.2016.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bodmer B.S., Fiedler A.H., Hanauer J.R.H., Prüfer S., Mühlebach M.D. Live-attenuated bivalent measles virus-derived vaccines targeting Middle East respiratory syndrome coronavirus induce robust and multifunctional T cell responses against both viruses in an appropriate mouse model. Virology. 2018 doi: 10.1016/j.virol.2018.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Malczyk A.H., Kupke A., Prüfer S., Scheuplein V.A., Hutzler S., Kreuz D., Beissert T., Bauer S., Hubich-Rau S., Tondera C., Eldin H.S., Schmidt J., Vergara-Alert J., Süzer Y., Seifried J., Hanschmann K.-M., Kalinke U., Herold S., Sahin U., Cichutek K., Waibler Z., Eickmann M., Becker S., Mühlebach M.D. A highly immunogenic and protective middle east respiratory syndrome coronavirus vaccine based on a recombinant measles virus vaccine platform. J. Virol. 2015 doi: 10.1128/JVI.01815-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Escriou N., Callendret B., Lorin V., Combredet C., Marianneau P., Février M., Tangy F. Protection from SARS coronavirus conferred by live measles vaccine expressing the spike glycoprotein. Virology. 2014 doi: 10.1016/j.virol.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Liniger M., Zuniga A., Tamin A., Azzouz-Morin T.N., Knuchel M., Marty R.R., Wiegand M., Weibel S., Kelvin D., Rota P.A., Naim H.Y. Induction of neutralising antibodies and cellular immune responses against SARS coronavirus by recombinant measles viruses. Vaccine. 2008 doi: 10.1016/j.vaccine.2008.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Yoneda M., Georges-Courbot M.C., Ikeda F., Ishii M., Nagata N., Jacquot F., Raoul H., Sato H., Kai C. Recombinant measles virus vaccine expressing the Nipah virus glycoprotein protects against lethal Nipah virus challenge. PLOS ONE. 2013 doi: 10.1371/journal.pone.0058414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mok H. Evaluation of measles vaccine virus as a vector to deliver respiratory syncytial virus fusion protein or epstein-barr virus glycoprotein gp350. Open Virol. J. 2012 doi: 10.2174/1874357901206010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sawada A., Yunomae K., Nakayama T. Immunogenicity of recombinant measles vaccine expressing fusion protein of respiratory syncytial virus in cynomolgus monkeys. Microbiol. Immunol. 2018 doi: 10.1111/1348-0421.12559. [DOI] [PubMed] [Google Scholar]
- 147.Yamaji Y., Sawada A., Yasui Y., Ito T., Nakayama T. Simultaneous administration of recombinant measles viruses expressing respiratory syncytial virus fusion (F) and nucleo (N) proteins induced humoral and cellular immune responses in cotton rats. Vaccines. 2019 doi: 10.3390/vaccines7010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Desprès P., Combredet C., Frenkiel M.P., Lorin C., Brahic M., Tangy F. Live measles vaccine expressing the secreted form of the West Nile virus envelope glycoprotein protects against West Nile virus encephalitis. J. Infect. Dis. 2005 doi: 10.1086/426824. [DOI] [PubMed] [Google Scholar]
- 149.Brandler S., Marianneau P., Loth P., Lacôte S., Combredet C., Frenkiel M.P., Desprs P., Contamin H., Tangy F. Measles vaccine expressing the secreted form of West Nile virus envelope glycoprotein induces protective immunity in squirrel monkeys, a new model of West Nile virus infection. J. Infect. Dis. 2012 doi: 10.1093/infdis/jis328. [DOI] [PubMed] [Google Scholar]
- 150.Nürnberger C., Bodmer B.S., Fiedler A.H., Gabriel G., Mühlebach M.D. A measles virus-based vaccine candidate mediates protection against Zika Virus in an allogeneic mouse pregnancy model. J. Virol. 2018 doi: 10.1128/JVI.01485-18. [DOI] [PMC free article] [PubMed] [Google Scholar]